Perspective - (2024) Volume 14, Issue 3
Pharmacology of the Heart: A Comprehensive Overview
Gokhan Zengin*
Department of Pharmacology, University of Tocaeli, Izmit, Turkey
*Correspondence:
Gokhan Zengin, Department of Pharmacology, University of Tocaeli, Izmit,
Turkey,
Email:
Received: 04-May-2024, Manuscript No. IPFT-24-14766;
Editor assigned: 08-May-2024, Pre QC No. IPFT-24-14766 (PQ);
Reviewed: 22-May-2024, QC No. IPFT-24-14766;
Revised: 04-Jun-2024, Manuscript No. IPFT-24-14766 (R);
Published:
14-Jun-2024
Introduction
The heart is a marvel of biological engineering, tirelessly
pumping blood throughout the body to sustain life. However, its
intricate functionality can be compromised by various
cardiovascular diseases. Pharmacology plays a crucial role in
managing these conditions, offering a wide array of drugs
designed to regulate cardiac function and treat cardiovascular
disorders. In this comprehensive overview, we delve into the
pharmacology of the heart, exploring the mechanisms of action
of key drugs and their clinical implications.
Description
Anatomy and physiology of the heart
Before delving into pharmacology, it's essential to understand
the anatomy and physiology of the heart. The heart comprises
four chambers: Two atria and two ventricles, which contract
rhythmically to pump blood throughout the circulatory system.
Cardiac muscle cells or cardiomyocytes, generate electrical
impulses that coordinate the heart's contractions, regulated by
the autonomic nervous system. The heartbeat is regulated by
electrical impulses generated by the Sinoatrial (SA) node, which
serves as the heart's natural pacemaker. This electrical activity
coordinates the contraction and relaxation of cardiac muscles,
maintaining a steady rhythm essential for efficient pumping.
Pharmacodynamics and pharmacokinetics
Pharmacodynamics refers to how drugs exert their effects on
the body, while pharmacokinetics deals with how the body
processes drugs. In the context of cardiac pharmacology,
understanding these concepts is crucial for optimizing drug
therapy.
Pharmacodynamics of cardiac drugs
Pharmacodynamics refers to how drugs interact with the body
to produce their effects. Several classes of cardiac drugs target
different aspects of cardiac function:
Beta-blockers: These drugs inhibit the action of adrenaline
and noradrenaline on beta-adrenergic receptors, thereby
reducing heart rate and blood pressure. They are commonly
used to manage hypertension, angina and heart failure.
Calcium channel blockers: These drugs inhibit the influx of
calcium ions into cardiac muscle cells, resulting in relaxation of
blood vessels and decreased heart rate. They are prescribed for
hypertension, angina and certain arrhythmias.
ACE inhibitors and ARBs: These drugs block the reninangiotensin-
aldosterone system, leading to vasodilation and
reduced blood pressure. They are indicated for hypertension,
heart failure and post-myocardial infarction management.
Diuretics: Diuretics increase the excretion of sodium and
water by the kidneys, reducing blood volume and blood
pressure. They are used to treat hypertension, heart failure and
edema.
Antiarrhythmic drugs: These drugs stabilize the heart's
electrical activity and prevent or control abnormal heart
rhythms. They are classified into different classes based on their
mechanisms of action.
Pharmacokinetics of cardiac drugs
Pharmacokinetics refers to how drugs are absorbed,
distributed, metabolized and excreted by the body. Factors such
as bioavailability, half-life and drug interactions influence the
pharmacokinetics of cardiac drugs. For example, some drugs are
administered orally, while others are given intravenously.
Clearance of cardiac drugs may be affected by liver or kidney
function, requiring dose adjustments in patients with hepatic or
renal impairment.
Therapeutic applications
Pharmacotherapy in cardiology encompasses a broad
spectrum of conditions, each requiring tailored interventions.
Some common therapeutic applications include:
Hypertension: Antihypertensive drugs like ACE inhibitors,
Angiotensin Receptor Blockers (ARBs), diuretics and calcium
channel blockers are used to lower blood pressure, reducing the
workload on the heart and preventing complications like heart
failure and stroke.
Arrhythmias: Antiarrhythmic drugs are employed to restore
normal cardiac rhythm and prevent recurrence of arrhythmias.
These drugs are classified into multiple classes based on their
mechanism of action and are selected based on the specific type
of arrhythmia and individual patient characteristics.
Heart failure: Pharmacological management of heart failure
aims to improve cardiac function, alleviate symptoms and
prolong survival. Drugs such as Angiotensin-Converting Enzyme
(ACE) inhibitors, beta-blockers, aldosterone antagonists and
Angiotensin Receptor-Neprilysin Inhibitors (ARNIs) are
cornerstones of heart failure therapy, targeting various
neurohormonal pathways implicated in disease progression.
Ischemic heart disease: Drugs like nitrates, beta-blockers,
calcium channel blockers and antiplatelet agents are used in the
management of ischemic heart disease to relieve angina,
prevent myocardial ischemia and reduce the risk of thrombotic
events.
Clinical applications and considerations
Understanding the pharmacology of the heart is crucial for
managing various cardiovascular conditions effectively.
Healthcare professionals must consider several factors when
prescribing cardiac drugs:
Patient-specific factors such as age, comorbidities
and concomitant medications influence drug selection and
dosing. Monitoring parameters such as blood pressure, heart
rate, electrolytes and renal function help assess the drug's
efficacy and safety. Adverse effects such as hypotension,
bradycardia, electrolyte imbalances and drug interactions
should be carefully monitored and managed. Patient education
is essential to ensure adherence to medication regimens
and recognize signs of drug toxicity or worsening symptoms.
Future perspectives and advancements
Advancements in pharmacology continue to drive innovation
in cardiovascular medicine. Research efforts focus on
developing novel drug targets, improving drug delivery systems and personalizing treatment approaches based on
genetic and molecular characteristics. Emerging therapies such
as gene editing, stem cell therapy and precision medicine hold
promise for revolutionizing the management of cardiovascular
diseases in the future. While cardiovascular drugs have
revolutionized the management of heart disease, challenges
remain. Adverse effects, drug interactions and patient adherence
are common concerns that clinicians must address to optimize
therapeutic outcomes. Additionally, the emergence of
personalized medicine, genetic testing and novel drug delivery
systems holds promise for advancing cardiac pharmacology.
Conclusion
The pharmacology of the heart encompasses a diverse array
of drugs aimed at maintaining cardiac function and treating
cardiovascular disorders. Understanding the mechanisms of
action, pharmacokinetics and clinical applications of these drugs
is essential for healthcare professionals involved in the
management of cardiovascular diseases. With ongoing research
and technological advancements, the future of cardiac
pharmacology holds exciting possibilities for improving patient
outcomes and quality of life. The pharmacodynamics and
pharmacokinetics of these drugs, healthcare professionals can
tailor therapy to individual patient needs, optimizing
cardiovascular outcomes and enhancing quality of life. As
research continues to unravel the complexities of cardiac
pharmacology, the future holds exciting prospects for improving
cardiovascular care and reducing the global burden of heart
disease.
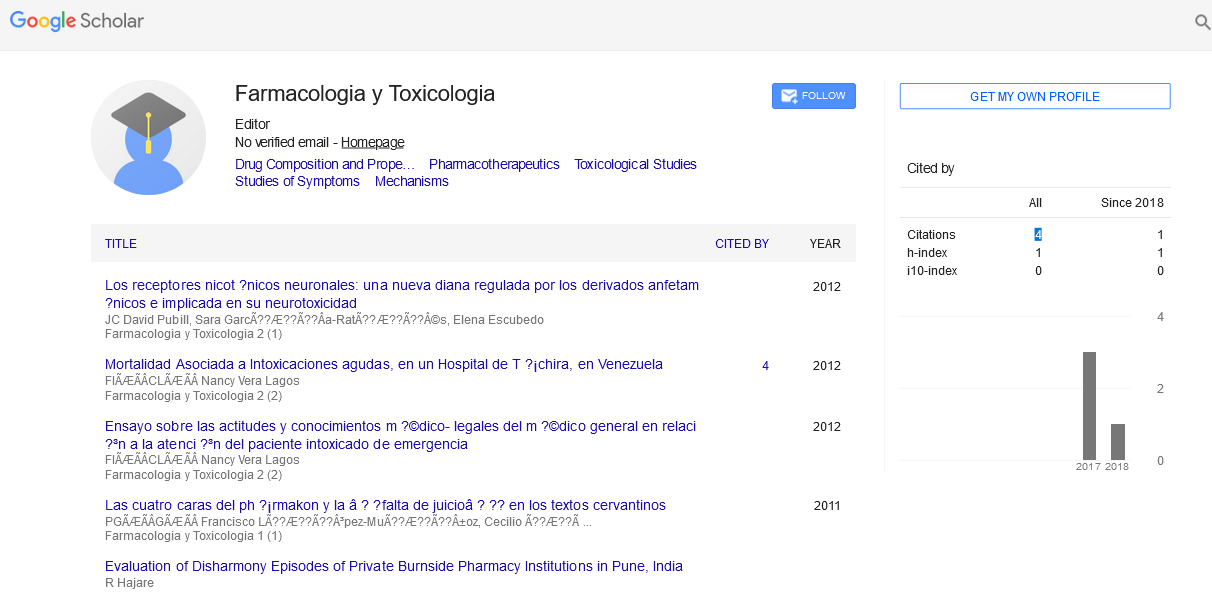
Citation: Zengin G (2024) Pharmacology of the Heart: A Comprehensive Overview. Farmacologia Toxicologia Vol.14 No.3: 023