Abstract
Background: The number of elderly people expected to grow from 524 million in 2010 to 1.5 billion in 2050, predominantly in developing countries. Older people are prone to age-related disease comorbidity, and poly pharmacy, which made medication prescription often inappropriate and inaccurate. Therefor prescribing medication appropriately is concerning issues in older adults. This study was aimed to determine the prevalence of potentially inappropriate medication use and associated factors in an Ethiopian hospital.
Methods: A facility-based cross-sectional study design was employed for patients aged 65 and above years. American geriatrics society Beers 2019 evidence-based criteria were used to collect data and to identify Potential inappropriate medications. Descriptive statistics and binary logistic regression were used to describe and identify potential predictors of PIMs use. Statistical analyses were done by using the Statistical package for social science Software version 23 (SPSS ® 23).
Results: From 675 older patients visited during the study period, 236 patients were included in the study. The magnitude was 47% with 131 PIMs giving a mean ± SD of 1.2 ± 0.5 were identified during the study period. Most of the patients 95 ( 40.3%) had only one PIM and Glibenclamide was the most common inappropriately prescribed drugs. Patients with cardiovascular disorder (AOR=4.0, 95% CI; 2.0, 8.4) and endocrine disorder (AOR=2.6; 95% CI, 1.5, 4.6) had significant association with PIM use.
Conclusion: Prescribing of PIM is common among Ethiopian elderly patients. The patient's having cardiovascular disorders or endocrine disorders were more likely to have increased use of PIMs among older patients.
Keywords
Elderly; Potential inappropriate medication; Beer’s criteria; Comorbidity
Background
The number of people aged 65 and above expected to grow from 524 million in 2010 to 1.5 billion in 2050, predominantly in developing countries [1]. Drug therapy in the elderly needs an emphasis on age-related changes in drug pharmacokinetics and sensitivity profile [2]. Older people are prone to age-related disease comorbidity, and more number of drug use, which made medication prescription often inappropriate and inaccurate. Inappropriate prescriptions are a major health problem affecting elderly persons [3]. Older adults are at high risk for inappropriate medication use given their myriad medical conditions and medications [4]. Certain drugs may cause an increased risk of adverse drug events in geriatrics population groups, which classified as Potentially Inappropriate Medications (PIMs) for the elderly [5]. Medication appropriateness is a concerning issue in older adults as if they are more vulnerable to medication-related problems. Focused screening and intervention to improve medication appropriateness can be accomplished using readily available tools that can be integrated into clinical processes and, in some cases, into the electronic medical record [4]. Among nursing home resident geriatrics, 50% exposed to PIMs and suggests an increasing prevalence over time [6]. Inappropriate prescribing to have significant association with number of drugs prescribed to an elderly patient [7]. PIMs prevalence is vary in different countries, for example Saudi Arabia 52.5%, 11% USA, 66% India, 88 % in Germany of patients received at least one PIMs in the geriatrics age group [5,8-10]. A retrospective study in the USA in cardiovascular patients have a high prevalence of PIMs in geriatrics observed [11]. A retrospective study done in northwest Ethiopia with a total sample of 1252 patients were used in the study, of whom 347 (27.7%) were received at least one potentially inappropriate medication and immediate-release nifedipine (53.9%) is highly prescribed inappropriately followed by diclofenac (22.2%), ibuprofen (7.8%) and indomethacin (5.2) [12]. An observational study in India shows that there is a high prevalence of potentially inappropriate prescribing and adverse drug reactions among hospitalized older adults. The prevalence of PIM revealed a significant association with adverse outcomes in terms of hospitalizations. So further development of interventional strategies is crucial component to prevent PIM use for patients with multiple chronic conditions [13,14]. The utilization of PIMs listed in Beers criteria among the geriatric population can cause unplanned hospitalization. As the patients receiving polypharmacy are at high risk of unplanned hospitalization, so caution must be exercised in prescribing PIMs for older people [15]. Potentially inappropriate medications carry the risk of causing adverse drug events in the elderly [5]. PIM use was an important issue because of higher resource utilization in annual emergency care [16]. Decreased utilization of PIMs will reduce the occurrence of Adverse drug reactions, cost of treatment, and increase compliance in older patients [7] lower risk of hospitalization in the elderly [17].
In Ethiopia, there are no specific guidelines for the management of medications used in geriatrics, so this study may use as impute for the appropriateness of medication used in geriatrics medication use and to develop the special guideline. Moreover, to my knowledge, this is the first study to identify PIMs use by using the most recently updated 2019 AGS Beers criteria among older patients and evaluate predicting factors associated with PIMs use in Ethiopia. Therefore, this study used to understand PIM and factors for an increment of PIMs. In addition it can be used to establish strategies to avoid use of PIMs and to optimize drug therapy for elders. Besides, it can be used as impute for the institution to update their medication list and to incorporate include alternative drugs for the PIMs.
Methods
Study area and study period
The study was conducted from July 20/2020 to December 20/2020 in the medical referral clinic of Menelik II Referral Hospital, which is located in the center of Addis Ababa. Menelik II Referral Hospital is one of the hospitals under Addis Ababa City Administration Health Bureau and it has been giving routine health care services for the city community and other referral cases from different regional states of Ethiopia. It is a referral and teaching hospital in Addis Ababa, which serves a large number of people from the surrounding zones and nearby regions both for inpatient and outpatient treatment.
Study design and study population
The facility-based cross-sectional study design was employed for patients aged 65 and above years who attended the medical referral clinic during the study period. Patients with incomplete medical and medication information such as missing of dose and frequency, patients on follow up but without any medications were excluded from the study.
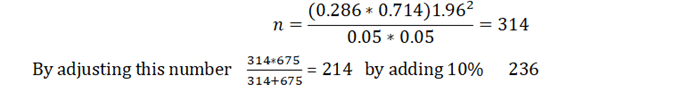
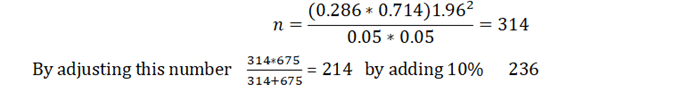
Sample size determination
The sample size was determined using single proportion formula, based on the previous study PIMs proportions of 28.6%, 5% margin of error at 95% confidence level. Six hundred seventy five elderly patients were visited to MIIRH during the study period and adjusting for finite population correction a sample of 236 patients were selected. Study participants were selected by simple random sampling techniques.
Data Collection, Procedure and Instrument
American Geriatrics Society (AGS) Beers criteria 2019 is evidence-based criteria and developed by AGS intended for use in all ambulatory, acute, and institutionalized settings of care for populations aged 65 and older in the United States, except those hospice and palliative care. AGS beers criteria 2019 criteria classified into five categories as medications should be avoided in geriatrics, medications with drug-drug interaction, medications having drug-disease interaction, medications should be administered cautiously and should be adjusted based on creatinin clearance level (AGS, 2019). Structured questionnaire for data abstraction tool used to extract all the necessary information. Patient demographic information, patients' medical conditions, medication-related information's an investigation related information collected by using pre-designed data abstraction tool by using AGS beers criteria 2019.
Variables of the Study
Dependentvariable:
Themainoutcomeofinterestinthisstudywastoestimatetheprevalence of PIMs in older adults. The PIMs were identified according to the American Geriatric Society (AGS) 2019 updated Beers criteria.
Independent variables:
Independent variables included were demographics (age in years, gender); the number of comorbidities: the presence of comorbidity, and the number of drugs prescribed. Patient chronic disease conditions, which were categorized into cardiovascular disease; endocrine disorder; respiratory disorder neurologic disorder; ophthalmic disorder; infectious disorder also considered as independent variables.
Data entry and analysis:
Data were coded, cleaned, and entered, and analyzed using SPSS version 23. Descriptive statistics were used to calculate (mean, median, and percentage) and results were presented using tables, charts. Binary logistic regression analysis was computed, those variables with a p-value <0.05 were considered as significant in multivariate analysis. Odds Ratio (OR) with a 95% confidence interval was also computed for each variable for the corresponding P-value to see the strength of association.
Operational definition
AGS 2019 updated beers criteria
2019 Updated Beer's Criteria refers to an explicit list of medications prepared by the American Geriatric Society to be avoided, adjusted, or cautiously used in older adults in 2015 because the risk outweighs benefits.
Geriatrics
Populations aged 65 and older.
PIMs
PIMs refers to any medication listed in updated 2019 Beers criteria to be avoided, adjusted, or cautiously used in older patients.
Results
Socio-demographic and clinical characteristics of patients
From 675 elderly patients vested during the study period, 236 patients were included in the study. The mean age was 70.5 ± 5.9 years and male patients represented 50.4% of the study participants. More than two-thirds (71.6%) of the participants had comorbid disease conditions. The sum of the number of medications prescribed was 743, giving an average of 3.2 ± 1.7 drugs per patient. One hundred eighty-nine (79.2%) patients received less than five drugs with a maximum of nine drugs. In this study, 184 (78.0%) patients had at least one Cardio Vascular Disease (CVD). Whereas infectious disease was identified in eight (3.4%) patients (Table 1).
| Characteristics |
Frequency |
Percent |
| Gender |
| Male |
119 |
50.4 |
| Female |
117 |
49.6 |
| Age (mean ± SD) |
70.51 ± 5.892 |
| 65- 69 |
124 |
52.6 |
| 70-74 |
65 |
27.5 |
| >=75 |
74 |
19.9 |
| Comorbidity |
| Yes |
169 |
71.6 |
| No |
67 |
28.4 |
| Number of comorbidities |
2.67 ± 1.869 |
| One |
67 |
28.4 |
| Two |
108 |
45.8 |
| Three and above |
61 |
25.8 |
| Number of drugs (mean ± SD) |
3.15 ± 1.66 |
| 0-4 |
187 |
79.2 |
| >=5 |
49 |
20.8 |
| Disease |
| Cardio vascular disease |
184 |
78.0 |
| Endocrine disorder |
140 |
59.3 |
| Respiratory disorder |
11 |
4.7 |
| Neurologic disorder |
19 |
8.1 |
| Ophthalmic disorder |
12 |
5.1 |
| Infectious disorder |
8 |
3.4 |
Table 1: Demographic and clinical characteristics of study participants in the medical referral clinic of MIIRH, Addis Ababa, Ethiopia (N=236).
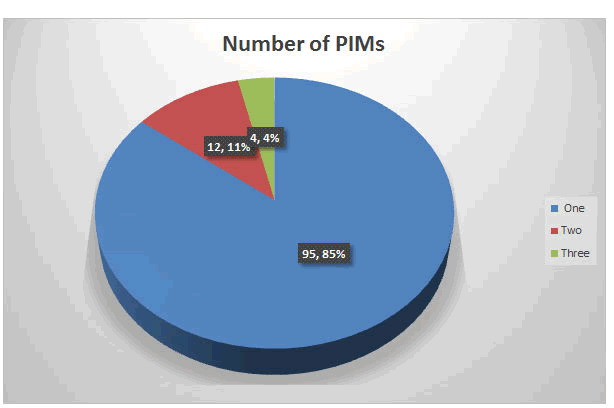
Potentially Inappropriate Medication
Evaluating of the prescribed medications using the 2019 Updated Beer’s Criteria revealed that 111 older patients encountered at least one PIM, encountered 47 % (95% CI: 40.3, 53.8). From total patients, 131 PIMs giving mean ± SD of 1.2 ± 0.5 were identified during the study period. Most of the patients 95(40.3%) had only one PIMs (Figure 1). Glibenclamide was the most commonly prescribed PIMs 74 followed by Diclofenac 14 while Spironolactone and Enalapril were implicated in one patient each (Table 2).
| S. No |
Drugs In PIM |
Frequency |
Potential risk |
| 1 |
Glibenclamide |
74 |
Higher risk of severe prolonged hypoglycemia in the elderly. |
| 2 |
Diclofenac |
12 |
Increased risk of gastrointestinal bleeding or peptic ulcer disease in high-risk groups.Potential to promote fluid retention and/or exacerbate heart failure with reduced ejection fraction (NSAIDs) |
| 3 |
Omeprazole |
10 |
Risk of Clostridium difficile infection and bone loss andFractures, avoid scheduled use for >8 weeks unless for high-risk patients |
| 4 |
Amytrypthylin |
7 |
Highly anticholinergic, sedating, and cause orthostatic hypotension |
| 5 |
Warfarin |
7 |
When it prescribed with aspirin and ciprofloxcillin increased the risk of bleeding.When it prescribed with ciprofloxcillin increased risk of bleeding |
| 6 |
Aspirin |
5 |
When it prescribed with Warfarin, Increased risk of bleedingAspirin in peptic ulcer patients without anti-acidAspirin for primary prevention of cardiac events |
| 7 |
Methyldopa |
4 |
High risk of adverse CNS effects; may cause bradycardia and orthostatic hypotension; not recommended as routine treatment for hypertension |
| 8 |
Ciprofloxacillin |
3 |
Increased risk of CNS effects (eg, seizures, confusion) and tendon rupture when CrCl <30 mL/minIncreased risk of bleeding if used with warfarin |
| 9 |
Indomethacin |
3 |
Increased risk of gastrointestinal bleeding/peptic ulcerdisease and acute kidney injury in older adults |
| 10 |
Diphenhydramine |
2 |
Highly anticholinergic, sedating, and cause orthostatic hypotension |
| 11 |
Ibuprofen |
2 |
Potential to promote fluid retention and/or exacerbate heart failure (NSAIDs) |
| 12 |
Enalapril |
1 |
When it prescribed with Spironolactone Increased risk of hyperkalemia, in those with chronic kidney disease stage 3a or higher |
| 13 |
Spironolactone |
1 |
When it prescribed with Enalapril Increased risk of hyperkalemia, in those with chronic kidney disease stage 3a or higher |
|
Total
|
131
|
Table 2: Prescribed drugs in elderlies that should be avoided based on Beer’s criteria.
Figure 1: Number of PIMs among elder patients attending a medical referral clinic MIIRH, Addis Ababa, Ethiopia.
Factors associated with PIMs
Binary logistic regression analysis was performed to determine risk factors associated with PIMs. Sex, age, presence of comorbidity, number of drugs, and types of disorder were analyzed by binary logistic regression. Patients with a cardiovascular disorder associated with PIM use (adjusted odds ratio (AOR), 4.0; 95% CI; 2.0, 8.412). Moreover having endocrine disorder (AOR, 2.6; 95% CI, 1.5, 4.6) was strongly associated with PIM use (Table 3).
| Variable |
|
PIM |
PIM present |
| |
|
Present |
Absent |
AOR (95% CI) |
P-value |
| Sex |
Male |
54 |
65 |
1.00 |
Reference |
| female |
57 |
60 |
0.928 (0.539, 1.599) |
0.789 |
| Age |
65- 69 |
58 |
66 |
1.00 |
Reference |
| 70-74 |
33 |
32 |
0.959 (0.507, 1.814) |
0.898 |
| >=75 |
20 |
27 |
1.108 (0.527, 2.329) |
0.787 |
| Comorbidity |
Present |
80 |
89 |
1.08 (0.462, 2.526) |
0.859 |
| Absent |
31 |
36 |
1.00 |
Reference |
| Number of drugs |
0-4 |
86 |
101 |
1.00 |
Reference |
| >=5 |
25 |
24 |
1.204 (0.586, 1.693) |
0.613 |
| CVD |
Yes |
79 |
105 |
4.011 (2.013, 8.412) |
0.015* |
| No |
32 |
20 |
1.00 |
Reference |
| Endocrine Disorder |
Yes |
84 |
56 |
2.618 (1.495, 4.583) |
0.001* |
| No |
27 |
69 |
1.00 |
Reference |
| Respiratory Disorder |
Yes |
4 |
7 |
0.693 (0.169, 2.839) |
0.611 |
| No |
107 |
118 |
1.00 |
Reference |
| Neurologic Disorder |
Yes |
6 |
13 |
0.789 (0.257, 2.424) |
0.679 |
| No |
105 |
112 |
1.00 |
Reference |
| Ophthalmic Disorder |
Yes |
6 |
6 |
0.750 (0.218, 2.580) |
0.648 |
| No |
119 |
105 |
1.00 |
Reference |
| Infectious Disorder |
Yes |
4 |
4 |
1.801 (0 .392 8.274) |
0.450 |
| No |
107 |
121 |
1.00 |
Reference |
Table 3: Number and raw percentage of characteristics by PIM use adjusted odds ratios and 95% confidence intervals from binary logistic regression on PIM use among older patients.
Discussion
Optimal drug therapy is an essential component of the health care delivery of older patients. Use of medication that may have more risk than benefit considered as potentially inappropriate. Older patients were more vulnerable for use of such medications since they are more likely to receive several medications due to chronic disease. This study revealed that 47% of participants encountered at least one PIM. Patients' cardiovascular and endocrine disorders were at risk of using PIMs.
In this study, the PIMs were present 47% by using the 2019 Updated Beer’s Criteria. This finding was comparative with other findings in different countries ranges from 44% to (52%) [18–20]. This is slightly lower than in previous studies [9,21–24]. This slight variation might be a difference in the study setting variation, short study period and using different Beers criteria to identify PIMs. Being a long study period in admitted patients, findings might be a reason for a higher rate. Besides, the updated 2019 AGS Beer Criteria® update had nearly 70 modifications to 2015. This study also lower than in the USA (73%) at admission and during discharge (50%) [25]. A possible justification for the discrepancy might be due to the availability of Beers list medications in the USA, being multi-centered study, using of 2015 Beers list and sample size difference (more number of elderly patients) included in the USA study.
This figure was higher than in previous studies [15,26,27]. This higher ;prevalence might be starting of medication before confirming of specific diagnosis with objective findings, inclusion criteria included multi morbid patients, available medications, and prescribing patterns, only DM patients were enrolled in Inamdar & Kulkarni whereas in Lim et al. older patients irrespective of disease condition were included. Meanwhile, the figure is much higher as compared with other Ethiopian hospital studies, in northern Ethiopia 28.6% [28], and in northwest Ethiopia (27.7%) [12]. This discrepancy might be a difference in prescribing patterns, study setting, and study population. For instance admitted patients in different wards were included in the northern Ethiopia study and more than half of patients had an infectious disease, so the highest percentage of antibiotics were prescribed since the Beers list contains more non-antibiotics drugs.
Glibenclamide followed by diclofenac was the most common inappropriately prescribed drugs. Long-acting sulfonylureas (Chlorpropamide, glimepiride, and glibenclamide) can cause prolonged hypoglycemia, so these drugs should be voided in older adults [29]. However, glibenclamide was the most frequently prescribed drugs. Guide lines recommend that short acting sulfonylureas such as glipizide for elder patients to prevent prolonged hypoglycemia. In addition scientific geriatric organisations recommend physicians against prescribing of oral hypoglycaemic drugs to elderly with serious concern of hypoglycaemic effect. The reason for the high prescribing pattern of glibenclamide might be a concern of the availability of short-acting sulfonylureas such as glipizide.
Unlike other studies [11,27,28] having a comorbid disease and prescribing more drugs have no association with the occurrence of PIMs. In this study, the presence of some chronic disease conditions increased the probability of PIMs. Patients were with cardiovascular disorders 4.011 times more likely to have PIMs whereas patients with endocrine disorder 2.6 times more prone to PIMs. The high prevalence of PIMs in cardiovascular and endocrine disorders was due to prescribed drugs not safe for elders. While other studies reported that there is an increased prevalence of PIM on older patients who had diabetes, Ischemic heart disease, heart failure, chronic kidney disease, cancer, osteoarthritis, osteoporosis, and anxiety [21].
Older patients are benefited by applying special consideration before and after prescribing of drugs. To achieve these, physicians should be assisted by pharmacists and ideally by patients [30]. All health professionals should know about basic changes in drug pharmacokinetics and pharmacodynamics during aging, especially those prescribing drugs should always consider this, to prevent compromising the health of the elderly through inappropriate prescriptions. Pharmacists are also key professionals in avoiding the use of PIMs since all drugs dispensed by them, they can identify possible contraindications for the elderly [31]. In Ethiopia, current hospital reform implementation guidelines included clinical pharmacy service in inpatient, outpatient and emergency departments of hospitals. The service should be well organized recorded, documented and reported [32].
An important aspect of this study is that it provided insight into the magnitude of PIMs in ambulatory older chronically ill patients in developing set-up. It enables physicians to give attention in prescribing of drugs in chronically ill patients, spicily for specific medications in CVDs endocrine disorders. Being prospective study, using the most updated criteria for PIM use identification and discussion was made with the physician during data collection is the strong side of the study. This study provided a chance to clinical pharmacists to optimize their role for patient care by identifying, preventing, and resolving problems. This study had some limitations. Firstly, over-the-counter medicines not considered, only prescribed medications from patient charts were collected. This might decreases the generalizability of these findings. Secondly, general health status and co-morbidities of the patients were only assessed based on available documents so the PIMs might be wrongly estimated. Thirdly this study could not dugout the consequence of PIMs due to incomplete recorded data.
Conclusions
This study revealed that PIM prescribing is common among Ethiopian older chronically refill patients. The patient's having cardiovascular disorders or endocrine disorders were more likely to have increased use of PIMs among older patients. With the current rapid growth of the older population, future studies with a strong study design should be done to dig out the adverse health outcome use, and economic burden associated with PIMs.
Acknowledgment
The author would like to acknowledge the Addis Ababa health office and Menelik II Referral Hospital.
Competing Interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- WHO (2011) Global health and aging. National Institute on Aging, National Institute of Health U.S. Department of Health and Human Services: 4
- Olsen CG, Tindall WN (2007) Book reviews. Am J Pharm Educ :71
- Fialová D, Onder G (2009) Medication errors in elderly peopleâ?¯: contributing factors and future perspectives. Br J Clin Pharmacol 67:641–645
- Zullo AR, Gray SL, Holmes HM, Marcum ZA (2017) Screenig for Medication Appropriateness in Older Adults Elderly. Clin Geriatr Med: 1–16
- Holt S, Schmiedl S, Thürmann PA (2010) Potentially Inappropriate Medications in the Elderlyâ?¯: The PRISCUS List. Dtsch Ärzteblatt Int 107:543–551
- Morin L, Laroche M, Texier G, Mscpharm KJ (2016) Prevalence of potentially inappropriate medication use in older adults living in nursing homesâ?¯: a systematic review. J Am Med Dir Assoc 17:862-863
- Pradhan S, Panda A, Mohanty M, Behera JP, Ramani YR, et al. (2015) A study of the prevalence of potentially inappropriate medication in elderly in a tertiary care teaching hospital in the state of Odisha. Int J Med Public Health:5
- Lichtman SM, Boparai M (2008) Potentially inappropriate medication use in elderly cancer patients. Crit Rev Oncol Hematol 68:40
- Narvekar RS, Bhandare NN, Gouveia JJ, Bhandare PN (2017) Utilization Pattern of Potentially Inappropriate Medications in Geriatric Patients in a Tertiary Care Hospitalâ?¯: A Retrospective Observational Study. J Clin Diagnostic Res :11
- Anne S (2016) Potentially inappropriate medication use in multimorbid elderly inpatients: differences between the FORTA, PRISCUS and STOPP ratings. Drugs - Real World Outcomes 3:317–325
- Sheikh-taha M (2017) Potentially inappropriate home medications among older patients with cardiovascular disease admitted to a cardiology service in USA. BMC Cardiovasc Disord 17:1–6
- Mekonnen AB, Bhagavathula AS (2014) Inappropriate medication use in the elderly Population attending Gondar University Hospital. Int J Pharm Pharm Sci 6:540–543
- Reich O, Rosemann T, Rapold R, Blozik E, Senn O (2014) Potentially Inappropriate Medication Use in Older Patients in Swiss Managed Care Plansâ?¯: Prevalence , Determinants and Association with Hospitalization. PLOS 9:23–25
- Rawat RS (2018) Evaluation of potentially inappropriate medication use and risk of adverse drug reactions in hospitalized older adultsâ?¯: an observational study in a Tertiary Care Hospital. 11:79–85
- Sarwar M rehan, Dar A, Mahar saad Y, Riaz T, Danish U, et al. (2018) Assessment of prescribing potentially inappropriate medications listed in Beers criteria and its association with the unplanned hospitalizationâ?¯: a cross-sectional study in Lahore , Pakistan. Clin Interv Aging 13:1485–1495
- Chang C, Lai H, Hwa S, Yang S, Wu R, et al. (2018) Prescription of potentially inappropriate medication to older patients presenting to the emergency departmentâ?¯: a nationally representative population study. Sci Rep:1–8
- Henschel F, Redaelli M, Siegel M, Stock S (2015) Correlation of Incident Potentially Inappropriate Medication Prescriptions and Hospitalizationâ?¯: An Analysis Based on the PRISCUS List. Drugs - Real World Outcomes 2:249–259
- Bazargan M, Smith JL, King EO (2018) Potentially inappropriate medication use among hypertensive older African-American adults. BMC Geriatr 18:1–9
- Lopes L (2016) Use of potentially inappropriate medications by the elderly at home. Ciência & Saúde Coletiva 21:3429–3438
- Odhayani AAl, Tourkmani A, Alshehri M, Alqahtani H, Mishriky A (2017) Potentially inappropriate medications prescribed for elderly patients through family physicians. Saudi J Biol Sci 24:200–207
- Alhawassi TM, Alatawi W, Alwhaibi M (2019) Prevalence of potentially inappropriate medications use among older adults and risk factors using the 2015 American Geriatrics Society Beers criteria. BMC Geriatr 19:1–8
- Al-Azayzih A, Alamoori R, Shoroq MA (2019) Potentially inappropriate medications prescribing according to Beers criteria among elderly outpatients in Jordanâ?¯: a cross sectional study. Pharm Pract (Granada) 17:1–7
- Simões PA, Santiago LM (2019) Prevalence of potentially inappropriate medication in the older adult population within primary care in Portugalâ?¯: A nationwide cross-sectional study. Patient Prefer Adherence 13:1569–1576
- Alturki A, Alaama T, Alomran Y, Almudaiheem H (2020) Potentially inappropriate medications in older patients based on Beers criteriaâ?¯: a sectional study of a family medicine practice in Saudi Arabia. BJGP: 4
- Osei EK, Berry-cabán CS, Haley CL, Rhodes-pope H (2016) Prevalence of beers criteria medications among elderly patients in a Military Hospital. Gerontol Geriatr Med 2:1 –6
- Inamdar SZ, Kulkarni RV (2016) Drug-related problems in elderly patients with type 2 diabetes mellitus. J Diabetol 1:1–12
- Lim Y, Kim H, Choi J, Lee JS, Ahn A, et al. (2016) Potentially inappropriate medications by beers criteria in older outpatientsâ?¯: Prevalence and risk factors. Korean J Fam Med37:329–333
- Dinkashe FT, Ayalew E, Kassa TT (2016) Prevalence of potentially inappropriate medications. J Drug Deliv Ther 6:16–21.
- AGS (2019) American geriatrics society updated beers criteria. Clin Investig (Lond):1–21
- Bressler R, Bahl JJ (2003) Principles of drug therapy for the elderly patient. Mayo Clin Proc78:1564–1577
- Baldoni ADO, Maria F, Chequer D, Raquel E, Ferraz A, et al. (2010) Elderly and drugsâ?¯: risks and necessity of rational use. Brazilian J Pharm Sci 46:617–632