Keywords
Antenatal care; Home delivery; Practice
Introduction
Maternal health refers to the health of women during pregnancy, childbirth and the postpartum period. Maternal health has emerged as global priority because of a great gap in the status of mothers’ wellbeing between rich and the poor countries [1].
The world health organization defines a maternal death as the “death of women while pregnant or within 42 days of termination of pregnancy, irrespective of the duration and sites of the pregnancy, from any cause related to or aggravated by pregnancy and its management but not from accidental causes [2]. There are many factors that affect place of delivery in developing countries including Ethiopia. Some of the majors ones are, lack of information and adequate knowledge about danger signs during pregnancy and labor; cultural/ traditional practices, quality of services, site service utilized and previous experience [1,3]. Improving in maternal health services are current sensitive issue.
Home delivery in Amhara region is also not far from the national figure although antenatal care attendance has reached 100% [4].
Government of Ethiopia is committed to improve maternal health, with a target of reducing the maternal mortality ratio by three-quarters over the period 1990 to 2015. Improving access to and strengthening facility-based maternal and newborn services is one such approach, and is also a health sector development plan (HSDP) strategic objective [5].
The main aim of this study is to assess the prevalence and determinants for home delivery among parturient that received antenatal care but delivered at home. Findings from this study will help to show the magnitude of the problem and the main determinant factors, thereby it will help as an input for intervention at local level.
Methods
Study design
Community based cross-sectional study design was used.
Study area and period
The study was conducted in Gozamin district Amhara regional state, from March 15/2014 to April15/2014. Amhara is one of the nine ethnic divisions of Ethiopia, containing the homeland of the Amhara people. It‘s capital is Bahir Dar and located here is Ethiopia's largest inland body of water, Lake Tana, which is the source of the Blue Nile river. The region is divided in to 11 administrative areas (zones) of wich the study area is located in East Gojjam administrative zone.
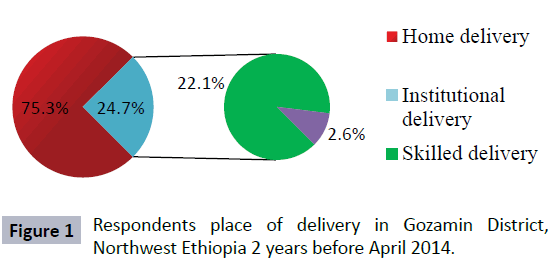
The district where the study tookplace has an estimated total population of 141,717 in 2013/14. Of this 71,142 (50.2%) are females, 34,012 are reproductive age women. Ninety seven percent of the population is estimated to be rural and about 97% of the populations are farmers. The district has 6 health centers, 26 health posts and 4 private clinics. The antenatal care coverage indicators for the last two years (2011/12 and 2012/13) are 99% and 100% respectively [6]. ANC follow up and delivery services in Ethiopia including this destrict provided free of charge. Reports showed that deliveries in the district at health facility level are assisted by health care professionals like nurses, midwiferies, public health officers’ and community health workers. But majority of births are at home and traditional birth attendants assist them (Figure 1).
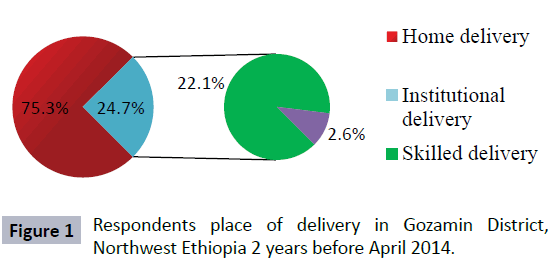
Figure 1: Respondents place of delivery in Gozamin District, Northwest Ethiopia 2 years before April 2014.
Population
The source population was all women who give birth within the last two years after ante natal care follow up in Gozamin district. The study population was all women who give birth within the last two years after ante natal care follow up in the selected kebeles.
Sample size determination
The sample size was determined using single population proportion formula;
n = Number of women’s who gave birth in the last two years recruited for the study.s
P = Proportion of home delivery from previous study_ 84 % [7]
Zα/2 = Level of statistical significant at 95% confidence interval 1.96.
d = Maximum acceptable marginal error_ 5%.
Using the above assumptions and considering design effect of 2 and 10% non respondent rate, the total sample size was 456.
Sampling technique and procedure
Stratified cluster sampling technique was carried out. First the kebeles stratified in to 6 clusters, stratification was done based on traditional difference and geographic area between kebeles and unequal performance with in health centers and health posts regarding instiututional delivery. Then, one Kebele from each cluster was randomly selected.
The selected kebeles were Kebie, Woyinema, Chimet, Wuger, Yebokla-01 and Chimbored. Then in the selected kebeles each households were checked for having the study units and all women who gave birth in the last two years after ANC follow up were included in the study.
Study variables
The dependent Variable is delivery outcome (home delivery or institutional) and the independent variables include; sociodemographic factors (age of mother, marital status, education, previous bad obstetric history, gravidity, parity, and family size), reinforcing factors (husband’s attitude, TBAs, family influence.), health service experience: sex of birth attendant, previous experience, place of ANC service, lack of privacy and confidentiality), health service access (distance, number of ANC visits, knowledge about free charge of the service), health service quality: women’s opinion about the quality of care, written plan for delivery, follow up care, traditional beliefs and cultural practice (placenta disposal, care of new born, birth assistance, cultural ceremony following delivery)
Eligibility criteria
Inclusion criteria: All women who gave birth within the last two years preceding the study and have been living within the catchment area for at least six months prior the study
Exclusion criteria: All women who gave birth within the last two years without attending ANC and women who were critically ill during data collection time.
Data collection procedures
Data was collected by using 12 trained nurses who were not working in the study area, and the data collection was strictly supervised by three bachlore health professionals. The interviewers and supervisors were given two days training before starting the actual work. Semi-structured questionnaire was used for interviews. The English version interview questions were translated into Amharic (local language) to obtain data from the study participants.
Operational definitions
Home delivery: Delivery that was not taken place at health institutions (hospitals, health centers, health posts and any private health institutions)
Antenatal care attended: Pregnant women who had attended antenatal clinics during the recent pregnancy and have got antenatal care at least once.
Skilled attendance: To people with midwifery skills (doctors, health officers, midwifes, nurses) who have been trained in the skills necessary to manage normal delivery, diagnose and refer obstetric complications.
Clean delivery: Delivery attended by health extension workers.
Traditional birth attendants: A birth attendant who initially acquired the ability by delivering babies herself or through apprenticeship to other TBAs.
Mothers satisfied in ANC service: Mothers who answered more than the average 12.5 from five liker scale questions.
Mothers not satisfied in ANC service: Mothers who answered less than the average 12.5 from five liker scale questions.
Kebele: The lowest Government administrative hierarchy that exists next to district
Data quality assurance
The quality of data was assured by properly designed and pre tested questionnaire and the English version questionnaire was developed by the investigator, translated to local language Every day, 10% of the computed questionnaires were reviewed and checked for completeness and relevance by the supervisors and principal investigator and the necessary feedbacks had been given to data collectors in the next morning before the actual procedure.
Data processing and analysis
Data entry was done using Epi data 3.1 and analysis was carried out by using SPSS version 20. Backward logistic regression was used to see the association between the outcome variable and the explanatory variables.
The dependent Variable entered to outcome category is delivery outcome (home delivery or institutional) and the independent variables entered to covariate category include; socio-demographic factors (age of mother, marital status, education, previous bad obstetric history, gravidity, parity, and family size), reinforcing factors (husband’s attitude, TBAs, family influence.), health service experience: sex of birth attendant, previous experience, place of ANC service, lack of privacy and confidentiality), health service access (distance, number of ANC visits, knowledge about free charge of the service ), health service quality: women’s opinion about the quality of care, written plan for delivery, follow up care, traditional beliefs and cultural practice (placenta disposal, care of new born, birth assistance, cultural ceremony following delivery)
Ethical clearance
Ethical clearance was obtained from the Ethical Clearance Committee of Debre Markos University College of medicine and health science. The study participants were informed about the objective, rationale and expected outcomes of the study and oral consent was obtained either to participate or refuse for the interview. All the informations from the respondents were kept confidential.
Results
Sample description
Total of 499 women who gave birth after antenatal care follow up within the last two years prior to the survey were initiated to be included in the survey and 497(99.6%) of them were responded to the interview properly. About 31% of respondents were in the age group of 24-29years, 25.4% were in the age group of 30-34 years, and the mean age of the respondents was 29.41(SD ± 6) years. Most of the respondents 424(85.3%) were farmers and 402(80.9%) of the respondents were unable to read and write.
About 72.2% of the respondents were gravida four or less and 27.8% of the respondents were gravida five and more. Among the respondents 29.8% have two and below number of children, 42.7% had three to four children, and 27.3% have five and more children.
About 25.4% of the respondents attended ANC once, 31.6% attended two twice, and 18.5% attended four and more times at health facilities during their pregnancy.
Regarding the reason for choosing ANC attendance in that particular health institution were, 277 (55.7%) of the respondents choose for closer distance to where they live, and 29.8% of the respondents choose for good service. Among the respondents, 409 (82.3%) had received advice where to gave birth. Only 81 (16.3%) of the respondents who attended ANC had written plan for delivery. Four hundred fifty nine (92.4%) of the respondents heard that the ANC and delivery services are given free of any charge, and 443(89.1%) of the respondents heard about availability of free ambulance service when labour started.
Antenatal care and delivery practice
The prevalence of home delivery after ante natal care follow up among mothers who gave birth in the last two years was 75.3%. This prevalence after four and more ANC follow up was 52.2%, and 80.5% among those who attend ANC three times.
Among mothers who gave birth at home, 256 were assisted during child birth by TBAs, and 73 of the respondents were assisted by their mothers. Concerning the decision making related to home delivery, 149(39.8%) of the respondents said that TBAs were the decision maker, 80(21.4%) of the respondents decided together with their husbands and 76(20.3%) of the respondents decided themselves.
Among the study participants who gave birth at health institution 18(14.6%) said institutional delivery was pain full compared to home delivery, 110(89.4) of the respondents were comfortable with both male and female birth attendants. Regarding the position of labor in health institutions, 56(44.8%) of the respondents reported the position of labor was not comfortable.
Cultural and traditional practice of respondents
Regarding husbands preferred place to give birth for their wife’s, 297(59.7%) of the husbands preferred home delivery, 104(20.9%) of the husbands preferred institutional delivery and the rest of the respondents didn’t know their husbands place preference for delivery.
In relation to religion, cultural, and traditional practice during pregnancy and child birth from the study participants, 454(91.3%) of the respondents had religious, cultural, and traditional practice during pregnancy and child birth. Regarding traditional medicine that taken orally or rubbed over the abdomen during labor, three hundred thirty seven (67.8%) of the respondents had trust on traditional medicine that taken orally or rubbed over the abdomen during labor, the preferred position to gave birth during labor from mothers who participated in the study, four hundred seven (81.9%) of the respondents were choose squatting position, and from the respondents three hundred forty four (69.2%) were said the next delivery place preferred home delivery.
Factors associated with home delivery
Binary logistic regression using the stepwise backward likelihood ratio method was used on multivariate analysis. The multivariate analysis showed that educational status had significant association with home delivery, respondents with educational status of unable to read and write were six times more likely to practice home delivery compared to respondents with primary education and above [AOR = 6.91, 95% CI 1.99, 15.10]. Regarding respondent’s occupation being farmer was significantly associated with home delivery compared to daily laborer and other jobs. [AOR = 9.42 95% CI 3.29, 26.94]. Respondents with family size of seven and above were four times more likely to practice home delivery than those respondents with family size of three and less than three. Regarding respondents obstetric history mothers who had five and more children alive were two times more likely to practice home delivery than respondents with two and below two children [AOR =2.51]. In respondents recent ANC history one interesting finding that had significant association with home delivery was that as WHO recommended every pregnant mothers during ANC shall have written plan for birth preparedness and complication readiness, so that respondents who didn’t have written plan for birth preparedness and complication readiness during ANC visit were twelve times more likely to practice home delivery than those respondents with written plan for birth preparedness and complication readiness during ANC visit [AOR= 12.93, 95% CI 4.86, 31.76] and respondents who were not visited in their absence during ANC follow up were two times more likely to practice home delivery compared to mothers who were visited in their absence during ANC follow up [AOR= 2.12] (Table 1).
Table 1: Socio Demographic, Obstetric and Recent ANC Follow up factors of Home Delivery in Gozamin District Northwest Ethiopia, March to April 2014.
| Variable |
Home Delivery |
COR 95% CI |
AOR 95% CI |
Over all p-value |
| Yes |
No |
Age
15-24years
25-34years
35 and above years |
65
224
85 |
48
56
19 |
1.00
2.95[1.84, 4.75]
3.30[1.77, 6.15] |
1.00
0.67[0.24, 1.87]
0.63[0.146, 2.72] |
0.736 |
Women’s Education
Unable to read & write
Able to read & write rimary school and above |
316
40
18 |
86
21
16 |
3.26[1.59, 6.67]
1.69[0.72, 3.98]
1.00 |
6.91[1.99, 15.10]
3.17[0.92, 9.12]
1.00 |
0.009 |
Women’s Occupation
Farmer
Daily labourer and other |
319
55 |
50
73 |
8.46[5.34, 13.41]
1.00 |
9.42[3.29, 26.94]
1.00 |
P<0.001 |
Number of ANC Visit
One to Two
Three
Four and More |
234
92
48 |
49
30
44 |
1.00
0.64[0.38, 1.07]
0.23[0.14, 0.38] |
1.00
1.16[0.41, 3.28]
2.12[0.45, 6.76] |
0.347 |
Place ANC Attendance
Hospital
Health Center
Health Post and Other |
20
197
157 |
17
88
18 |
1.00
1.90[0.95, 3.80]
7.40[3.29, 16.66] |
1.00
0.59[0.14, 2.52]
1.64[0.67, 3.98] |
0.264 |
Written Plan
for Birth Preparedness
Yes
No |
28
346 |
53
70 |
1.00
9.35[5.53, 15.82] |
1.00
12.93[4.86, 31.7] |
P<0.001 |
Visited in Absence
from ANC
Yes
No |
29
345 |
54
69 |
1.00
9.31[5.53, 15.66] |
1.00
2.19[0.35, 12.16] |
0.424 |
Time Spent in waiting area
Satisfied
Fair
Unsatisfied |
100
165
109 |
56
52
15 |
1.00
1.77[1.13, 2.79]
4.06[2.16, 7.64] |
1.00
2.76[1.18, 6.44]
6.19[2.15, 17.86] |
0.003 |
Husband preference
to place of birth
Home
Health institution and
don’t know |
271 103 |
26 97 |
9.82[6.02, 16.00] 1.00 |
5.84[2.36, 14.42] 1.00 |
P<0.001 |
Cultural and
Traditional Practice
Yes
No |
359
15 |
95
28 |
7.05[3.62, 13.73]
1.00 |
5.74[1.82, 18.07]
1.00 |
0.003 |
Preferred Position
During Child Birth
Squatting
Lithotomic |
338
36 |
69
54 |
7.34[4.48, 12.05]
1.00 |
3.76[1.60, 8.83]
1.00 |
0.002 |
Another important associated factor that had significant association with home delivery was respondents view on the quality of ANC; in this regard respondents were asked for the waiting time, those who spent for fair and unsatisfied waiting time were three and seven times more likely to gave birth at home than those respondents who spent for a satisfied waiting time [AOR = 2.76, 95% CI 1.16, 6.44 and AOR = 6.19, 95% CI 2.15, 17.86] respectively. Concerning respondents trust and confidence on the services provided at ANC, those respondents who didn’t have trust and confidence on the ANC service were four times to gave birth at home compared to those who had trust and confidence on the ANC service[AOR = 3.76, 95% CI 1.72, 8.24]. Lack of privacy and confidentiality also had influence on home delivery; respondents who perceive lack of privacy and confidentiality was a problem at ANC service were significant association with home delivery [AOR = 6.16]. In this study respondents were asked five questions about ANC service satisfaction, by taking the mean, respondents who were not satisfied at ANC service were nearly five times more likely to gave birth at home than those satisfied [AOR = 4.94, 95% CI 2.26, 10.77].
The other associated factor which had significant association with home delivery was reinforcing and enabling factors, respondent’s husbands place preference to their wife’s and husbands preference to birth attendants were significant association with home delivery [AOR = 5.84, 95% CI 2.36, 14.42 and AOR =3.32, 95% CI 1.20, 9.18] respectively.
Religious, cultural and traditional practices done by the mothers during child birth was also another important determinant factor for home delivery, respondents who practiced cultural and traditional practices during child birth were six times more likely to gave birth at home than who didn’t practiced [AOR = 5.74, 95% CI 1.82, 18.07].
Mothers who gave birth after ante natal care follow up were asked about their preferred position during labor and those who preferred squatting position during labor were three times more likely to gave birth compared those respondents who preferred lithotomic position [AOR =3.76 95% CI 1.60, 8.83].
Discussion
In this study the percentage of home delivery after ante natal care follows up was 75.3% this finding is higher than findings of previously studies in Adigrat and Holeta which are 35% and 61% respectively. It might be sdue to area difference because the previous studies were conducted in urban kebeles so that mothers in these areas might be more likely to have awareness towards institutional. On the other hand, the current finding was lower than previously community based conducted studies on determinants of antenatal care and institutional delivery care utilization in Tigray, Metekel and Sekela 95.9%, 88% and 87.9% respectively [8-10]. The reason for the difference could be maternal health is one of the millennium development goal so that currently the country is practicing provision of transport access (free ambulance service), and exempted ANC and delivery services were given to those mothers who are pregnant.
In addition this finding was lower than the latest EDHS 2011finding and specifically, the percentage of home delivery in this study after the fourth and one to three ANC follow up were 52.2% and 80.5% respectively, which is lower than EDHS 2011 findings 65.6% and 85.6% respectively [5]. The difference might be due to the given emphasis on maternal health by the government of Ethiopia and increased awareness.
Similarly a study done in western Kenya on ANC and delivery care, from the respondents 80% delivered in their house, this was higher than the present study; the possible reason for this discrepancy could be cultural difference, cost of the services and accessibility of services differences between the two countries affect mother’s place of delivery.
The finding showed that most of the mothers who delivered at home were assisted by TBAs (68.4%) this finding was lower than the study finding done on why do women prefer home births in Ethiopia (78%) and higher in similar studies done in Tigray region [7,8,11].
This study also revealed that cultural and traditional believes, more home delivery history and easy birth were main reasons for home delivery, this finding is in line with different studies in Ethiopia and some African countries [8,12].
This study demonstrates that socio demographic factors like respondents’ occupation and educational status had significant association with home delivery, those mothers with occupational status of house wife’s were nine times more likely to gave birth at home compared with mothers occupation of daily labrourer. Those respondents with educational status of unable to read and write were six times more likely to gave birth at home compared to respondents with primary education and above the reason might be this group of mothers have less awareness regarding complication of pregnancy and unaware of dangerous situations during child birth and also they were less autonomous to decide their place of delivery. The findings from different related previous studies showed that respondents’ educational status had influence on mothers’ choice of delivery place [13-17].
Another important finding from this study factors affecting home delivery were that religious, cultural and traditional practices done during child birth had significantly influence mothers place of delivery. Those mothers who practiced religious, cultural and traditional practice during child birth had six times more likely to give birth at home compared to those who didn’t practiced. On the other hand, mothers preferred position to give child birth had strong association with home delivery, mothers who preferred squatting position during child birth were four times more likely to gave birth at home compared with who preferred lithotomic position. This study finding was in agreement with others related studies showed that cultural and traditional practices had influence on mother’s choice of delivery [17,18].
Conclusions
This study showed that the prevalence of home delivery after ante natal care follow up in Gozamin district was still very high. Traditional beliefs and cultural activities of the community practiced during child birth were influencing mothers on the choice of delivery place.
Waiting time to get health services, lack of privacy, trust and confidence on the services provided lack of respect and friendly treatment during ANC followup and previous delivery in health facilities affect selection of place of delivery.
Decision making power within the household, husbands’ preference to wife’s birth attendants and those husbands’ who preferred to wife’s birth place was positively influence home delivery. Mothers who practice traditional and cultural beliefs, mother’s preference position to gave birth, occupation and educational status of mothers were also important predictors for home delivery.
Recommendation
Health care providers should strive to increase customer’s satisfaction regarding waiting time, respecting culturally sensitive issues and practices during labour and ANC visit so as to increase the attraction of institutional dlivery.
The health care providers should consider squatting position during labour as this is mostly preferred by laboring mothers.
The government health system should make strong bond with TBAs and should systematically use TBAs power by engaging them to the formal health system and they play the role of advice, encourage and early referral of pregnant women. It is important to hold regular support and training on their role as TBAs and the cost of home delivery.
The district health office should consider and implement WHO recommendation that all pregnant mothers should have a written plan for their birth preparedness and should be visited if they miss the next appointment in ANC follow up care.
Even though practicing female or women education to improve maternal health plays a large role, the present study also emphasized that the role of husband‘s on maternal health was very significant, so health care provider and health extension workers should make effort to encourage husband’s feeling in the direction of maternal health services and they should be included in the counseling and should participate in pregnant mothers conferences.
Acknowledgements
We would like to thank Debre Markos University and GAMBY College of medical sciences for their material and technical supports.
We are also greatful for all the study participants.
Competing Interests
The authors declare that they have no competing interests.
Authors’ Contribution
The first author drafted the proposal, did the analysis and writes the results. The second and third authors participate in editing the drafting of the proposal, analysis and writing of the results. The third author also prepared the manuscript.
7904
References
- WHO UNICEF, UNFPA, and The World Bank estimates (2012) Trends in Maternal Mortality:1990 to 2010.
- Khan KS, Wojdyla D, Say L, Gülmezoglu AM, Van Look PF (2006) WHO analysis of causes of maternal death: a systematic review.Lancet 367: 1066-1074.
- Fund UNCs (2010) Maternal Health Care in Egypt 2010. United Nations Children's Fund (UNICEF) 87, MisrHelwan Agricultural Road, Maadi, Cairo, Egypt.
- Amhara regional state health berio BD (2013) First anniversary report, Ethiopia.
- Central Statistical Agency [Ethiopia] andICF International Calverton M USA (2012) Ethiopia Demographic and Health Survey 2011.
- Administration Gwh. annual plan performance report. 2011-2012 and 2012-2013.
- Shiferaw S, Spigt M, Godefrooij M, Melkamu Y, Tekie M (2013) Why do women prefer home births in Ethiopia-BMC Pregnancy Childbirth 13: 5.
- Tsegay Y, Gebrehiwot T, Goicolea I, Edin K, Lemma H, et al. (2013) Determinants of antenatal and delivery care utilization in Tigray region, Ethiopia: a cross-sectional study.Int J Equity Health 12: 30.
- Tura G, Gebremariam A (2008) Safe delivery service utilization in metekel zone northwestethiopia. Ethiopia J Health Sci 17: 4.
- Shimeka A, Mazengia F, Meseret S (2012) Institutional delivery service utilization and associated factors among mothers who gave birth in the last 12 months in Sekela District, North West of Ethiopia. BMC Pregnancy Childbirth. 12: 74.
- Godefay H (2009) The importance of antenatal care risk scoring in predicting delivery outcomes in Tigray. Ethiopian J Reprod Health 3:15-26.
- Wanjira C, Mwangi M, Mathenge E, Mbugua G, Ng’ang’a Z (2011) Delivery Practices and Associated Factors among Mothers Seeking Child Welfare Services in Selected Health Facilities in Nyandarua South District, Kenya. BMC Public Health. 11: 360.
- Abeje G, Azage M, Setegn T (2014) Factors associated with Institutional delivery service utilization among mothers in Bahir Dar City administration, Amhara region. Reprod Health 11: 22.
- Esena RK, Kombian B (2013) Factors Associated with Choice of Place for Delivery In Builsa North District Of Ghana. IJPSR 3: 4.
- Abebe F, Berhane Y, Girma B (2012) Factors associated with home delivery in Bahirdar, Ethiopia: a case control study.BMC Res Notes 5: 653.
- Chowdhury AH, Hasan M, Ahmed S, Darwin C, Hasan MS, et al. (2013) Socio-demographic Factors Associated with Home Delivery Assisted by Untrained Traditional Birth Attendant in Rural Bangladesh. Am J Public Health Res. 1:226-230.
- Simfukwe ME (2011)Factors contributing to home delivery in Kongwa District, Dodoma Tanzania. DMSJ18: 13-22
- Mumbare SS, Rege R (2011) Ante natal care services utilization, delivery practices and factors affecting them in tribal area of north maharashtra.Indian J Community Med 36: 287-290.