Keywords
Prevalence, Caesarean section (cephalopelvic disproportion, malpresentation and malposition)
Introduction
Cesarean section refers to the delivery of a fetus, placenta and membrane through the abdominal and uterine incision after 28 weeks of gestation [1].
Cesarean delivery has played a major role in lowering both maternal and perinatal morbidity and mortality rates during the past century. The initial purpose of the surgery was to preserve the life of the mother with obstructed labor, but indications have expanded over the years to include delivery for a variety of more subtle dangers to the mother or fetus. Contributing to its more frequent use is its increased safety, which is largely a result of better surgical technique, improved anesthesia, effective antibiotics, and availability of blood transfusions [2].
Rates of cesarean section are of concern both in developed and developing countries. The global cesarean section rate is distributed very unevenly and results 15% of abdominal delivery. Latin America and Caribbean shows the highest rate (29.2%) and Africa shows the lowest (3.5%). In developed countries the proportion of cesarean birth is 21.1% whereas in least developed countries only 2% of deliveries are by cesarean section. The analysis suggests a strong inverse association between cesarean section rates and maternal, infant and neonatal mortality in countries with high mortality levels. In many developed countries, cesarean sections are increased and attention has focused on strategies to reduce its use do to the concern that higher cesarean section rates do not confer additional health gain but may increase maternal risk, have implications for future pregnancies and have resource implications for health service [3-5].
In Ethiopia the cesarean section rate of the country based on 2010 report is only 1% [6]. The Cs rate in some specified hospitals of the country such as Black Lion Teaching Hospital is around 10% in 1992 [7]. The reason for undertaking this research study is based on the fact that in areas with a high rate of maternal mortality and morbidity from poor access to CEMOC, knowing the prevalence, indications and pregnancy outcomes of operative delivery particularly Cs is crucial. Therefore this study is aimed at providing information on the prevalence, indications and outcomes of CD in Attat Hospital that plays a vital role in reducing maternal mortality and morbidity resulting from complications related with pregnancy that needs urgent surgical intervention. In addition to this the shortage of complete and adequate data on prevalence, indication and outcome of cesarean section at this Hospital as well as in the country level makes me to study on this topic at this specific Hospital. As a result the information on this issue will help the hospital Staff to know the trends, common indications and outcomes of pregnancy after Cs as well as the managers to allocate their resources on the most common priority areas. The study result will also help other stakeholders (NGO’s) working in this line. The best practices in the Hospital may also help other researchers, Zonal health departments, SNNPR and the country at large. This study conducted to investigate the prevalence and outcome of Cesarean delivery.
Materials and Methods
Study area
The study was conducted at Attat hospital. Attat Hospital integrated service is located 187 km south west of Addis Ababa along the Jimma road in the Southern region of Ethiopia. The service has been operative since 1969. The Hospital has 65 beds. In addition, there are 48 beds in the Maternity Waiting Area, 13 beds in the Nutrition Rehabilitation Unit, 3 Labour Beds and 2 Delivery Beds that are often used as overflow beds. Normal deliveries return home within 24 hours or stay in the Postnatal Room of the MWA when necessary. The obstetric/gynecology post-operative cases go to the Surgical Ward. Maternity and Gynecological services are the main surgical procedures done. Elective and emergency surgical services are performed. There are 1 obstetrician/gynecologist, 1 surgeon, 3 GPs, 2 Health officer, 1 health coordinator, 2 pharmacists, 4 druggists, 44 nurses, 7 lab technicians and 14 other health professionals. There are 87 support staff members.
Study design
Hospital based cross-sectional retrospective study was conducted from January 2011 – December 2013 GC.
Inclusion criteria
All cesarean deliveries performed after period of viability (28 weeks) including elective, emergency, primary and repeat cases are included in the study.
Exclusion criteria
Cesarean deliveries which lack full information.
Data collection procedure
The data for the study was collected using pre-tested structured questionnaire which have socio-demographic variables, obstetric history and outcome of cesarean section. The questionnaire was prepared in English. Information obtained from theatre records, labor ward records, and neonatal ward records using structured questionnaire.
Statistical analysis
After data collection was completed, the data were entered into SPSS software version 20. It was checked for its completeness, cleaned and analyzed accordingly. Frequencies and graphs were used to describe some variables. Bivariate analysis and chi- square test were used to examine association between dependent and independent variables. A 95% CI and p-value of <0.05 were considered to be statistically significant. In addition crude/adjusted odd ratios were calculated. To assess the effects of each independent variable on the outcome variables multivariate logistic analysis was carried out and fit to the final model.
Ethical consideration
Ethical clearance was obtained from Research Ethics Committee of Jimma University. And Letter of permission was obtained from Attat hospital administration office, Obstetrics and Gynecology department. After information was provided, informed consent was taken from study participants (laboring mothers), anonymity and confidentiality of respondents was kept.
Results
During the period of study, there were 5,611 deliveries at Attat Hospital, of which 1,547 were by C/S, an incidence of 27.6%. The age of the patients ranged between 16-45 years with a mean age of 28.12 years with SD ± 5.14. Majority of the patients were between 20-35 years 236 (84%), the rest were younger than 20 age years 27 (9.6%) and older than 35 years 18 (6.4%), 87 (31%) of the mothers were primipara, 179 (63.7%) were between Para one and Para four and 15 (5.3%) were grand multipara. Table 1 shows patients who had Cs were categorized according to age, parity and residence. 32 (11.4%) of mothers with C/s did not have ANC follow up in any health institution. 59 (21%) and 260 (79%) of the women were from urban and rural respectively (Table 1).
| Variables |
NO of CS |
Percentage |
| Age (Years) |
| <19 |
8 |
2.8 |
| 20-34 |
218 |
76.6 |
| ≥35 |
55 |
19.6 |
| Total |
281 |
100 |
| Parity |
| Primigravida |
88 |
31.3 |
| Para (1-4) |
178 |
63.3 |
| Grandmulti |
15 |
5.4 |
| Total |
281 |
100 |
| LNMP |
| Yes |
114 |
40.6 |
| No |
167 |
59.4 |
| Total |
281 |
100 |
| ANC Follow up |
| Yes |
249 |
88.6 |
| No |
32 |
11.4 |
| Total |
281 |
100 |
| Residence |
|
|
| Urban |
59 |
21 |
| Rural |
222 |
79 |
| Total |
281 |
100 |
| Marital status |
|
|
| Married |
277 |
98.6 |
| Single |
4 |
1.4 |
| Total |
281 |
100 |
Table 1: Distribution of cesarean section cases by socio-demographic characteristics, parity and ANC follow up in Attat Hospital.
193 (68.7%) of the mothers had primary Cs while 88 (31.3%) had repeat cs. The majority of Cs were emergencies-254 (90.4%), whereas 27 (9.6%) were elective. All of uterine incisions were lower uterine segment transverse cs. Bilateral Tubal Ligation (BTL) was done for 36 (12.8%) of the mothers. Out of the total BTL cases, 19 (52.8%) of BTL was done for repeat C/s cases while 17 (47.2) was done for primary C/s cases. Preoperative hemoglobin was done for the majority of Cs cases 270 (96.1%). Most Cs cases were done under Spinal anesthesia 225 (80.1%). Out of the 281 Cs cases 244 (86.8%) were term pregnancies, 28 (10%) were preterm and 9 (3.2%) were posterm (Table 2).
| Variables |
No. of CS |
Percentage |
| Type of CS |
| Elective |
27 |
9.6 |
| Emergency |
254 |
90.4 |
| Total |
281 |
100 |
| Primary |
193 |
68.7 |
| Repeat |
88 |
31.3 |
| Total |
281 |
100 |
| Bilateral tubal ligation |
| Yes |
36 |
12.8 |
| No |
245 |
87.2 |
| Total |
281 |
100 |
| PREOP HGB |
|
|
| 7-11gm/dl |
22 |
7.8 |
| >11gm/dl |
248 |
88.3 |
| Not done |
11 |
3.9 |
| Total |
281 |
100 |
| Type of anesthesia |
| General anesthesia |
56 |
19.9 |
| Spinal anesthesia |
225 |
80.1 |
| Total |
281 |
100 |
| Gestational Age in weeks |
| <37 |
28 |
10 |
| 37-42 |
244 |
86.8 |
| ≥42 |
9 |
3.2 |
| Total |
281 |
100 |
| Duration of labour |
| <12 |
99 |
35.2 |
| 24-Dec |
100 |
35.6 |
| >24 |
50 |
17.8 |
| Not in labour |
32 |
12.4 |
| Total |
281 |
100 |
Table 2: Type of Cs, anesthesia and preoperative hemoglobin status of cesarean sectioned cases in Attat Hospital.
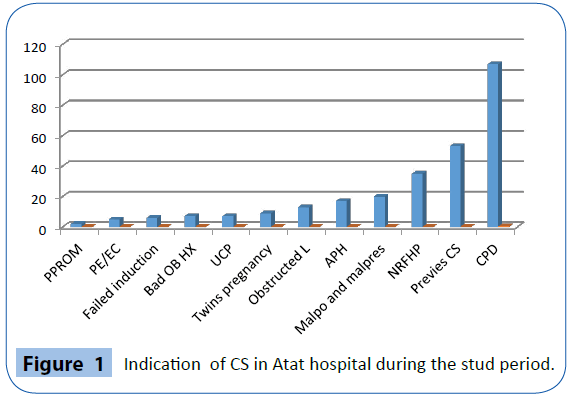
The leading indications for cesarean birth were, Cephalopelvic Disproportion (CPD) 107 (38.1%), previous Cs 53 (18.9%), fetal distress 35 (12.5%), mal-presentation and malposition 20 (7.1%), and Antepartum Hemorrhage (APH) 17 (6%) accounting for 82.6% of the indications for cesarean section. Figure 1 below shows graphical representation of indications of cesarean section.
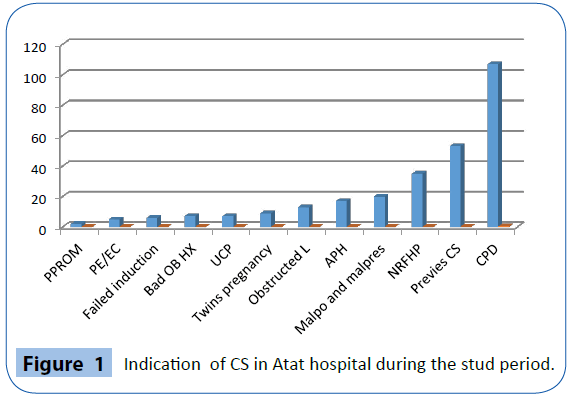
Figure 1: Indication of CS in Atat hospital during the stud period.
From Table 3 observe that post-operative maternal complications, the most common of which was respiratory tract infection 7 (2.5%), followed by post op fever 6 (2.1%). Mothers with ANC follow up have good postoperative outcome than those who didn’t have follow up (P-value=0.024, AOR=0.295, 95%CI =0.102, 0.849) and those mothers whose pre operation hemoglobin ≥ 11 have good post op outcome than mothers with pre operation hemoglobin <11 (P-value=0.034, COR=3.168, 95%CI=1.06, 9.41).
| Variables |
Maternal Outcomes |
COR 95%CI |
P-value |
AOR 95%CI |
P-value |
| Good |
Bad |
| ANC Follow Up |
| No |
22 |
10 |
|
|
|
|
| Yes |
232 |
17 |
0.16(.06,0.935) |
<0.001 |
0.343(0.102,1.15) |
0.082 |
| Labour duration |
| >24hrs |
42 |
8 |
|
|
|
|
| <24Hr or not in labour |
212 |
19 |
0.47(0.19,1.14) |
0.097 |
0.8(0.26,2.39) |
0.68 |
| Type of anesthesia |
| GA |
46 |
10 |
|
|
|
|
| SPA |
208 |
17 |
2.66(1.14,6.18) |
0.023 |
1.35(0.51,3.61) |
0.546 |
Table 3: Binary logistic regression performed to show the association between dependent variables with maternal outcome in Attat Hospital.
Unfavorable neonatal outcomes, 7 (2.5%) still births and 10 (3.6%) early neonatal deaths, only were reported from cases with emergency C/D except 1 (0.4) case reported from elective c/d. But the association was not statistically significant between type of C/s and neonatal outcome.
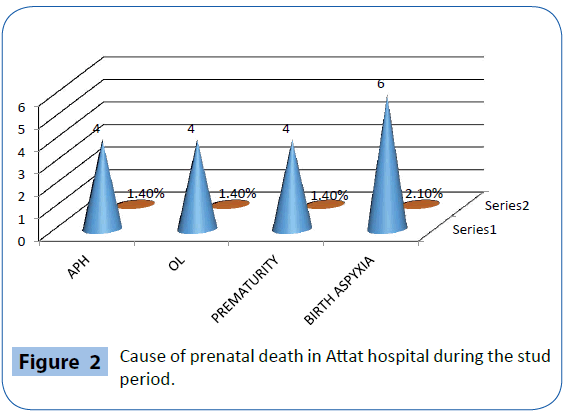
The cause of prenatal death was, birth asphyxia 6 (2.1%), obstructed labour 4 (1.4%), APH 4 (1.4), and prematurity 4 (1.4%) (Figure 2).
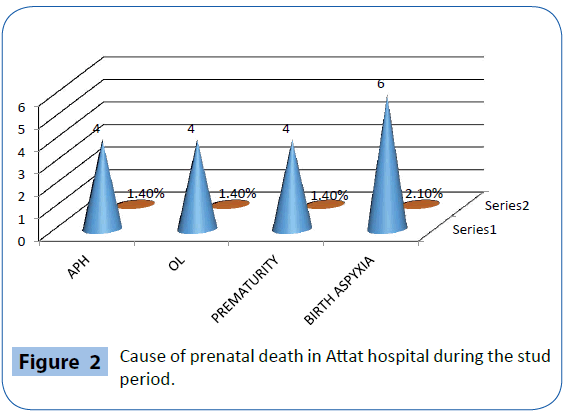
Figure 2: Cause of prenatal death in Attat hospital during the stud period.
Discussion
The cesarean section rate of 27.6% in this study was approximately similar to 23.1% reported from Sagamu, Southern Nigeria, 24.1% reported from Pakistan and 27.1% from Brazil, developing countries like Ethiopia. But the figure is lower than the rate of cesarean section in Chile (40.5%) and most developed countries like USA 32% [8-12]. This cesarean section rate was significantly higher as compared with cesarean section rates in other parts of the country like 10% in Tikur Anbessa Hospital, 8% in Jimma Hospital and 18% reported from the national review of cesarean delivery in Ethiopia but similar to 26.2% reported from another study in Ethiopia [7,13-18]. This rate was above 15% recommended by the World Health Organization. The frequency of cesarean section depends on the inherent characteristics of the obstetrics population, socio-demographic pattern, referral role of the hospital, departmental policies regarding management of cases of dystocia, breech, fetal distress, and previous cesarean section, physician factor and medico legal aspects, and consideration of maternal choice and wishes [19-26]. The higher rate of cesarean section in this study might be because of use of electronic fetal heart rate monitoring devices, less time given for conservative management of fetal distress (intervention with a single episode of fetal distress), increased number of repeat cesarean section with limited number of VBAC, more than three scars were allowed without BTL and acceptance of mothers at risk referred mainly from health institution. Each case should be thoroughly evaluated to determine the possibility for vaginal delivery [27- 31].
Similar to an earlier study from other parts of Ethiopia (Tikur Anbessa Hospital) and other developing countries (Ilorin, Nigeria) the majority of Cs in this study (90.4%) were performed as an emergency. Surprisingly 88.6% of the patients had ANC follow up. One hundred ninety three (68.7%) of the mothers had primary cesarean section which was similar to study done in Tikur Anbessa Hospital, Ethiopia (67.6%) [7,15,32].
The indications for cesarean section can be maternal or fetal, Maternal indications constituted 68% of the caesarean section in this review, the most common of which is cephalopelvic disproportion (38.1%) which is similar to the reports from other parts of the country [7,10,32,33] and other developing countries [32,33]. Because nutritional factors have dominant influence on pelvic size and shape and malnutrition especially during childhood result in pelvic contraction and general growth stunting; this high incidence of cephalopelvic disproportion may be related to the malnutrition that is still rampant in developing countries including Ethiopia. Previous caesarean section was the other most common maternal indication [15].
Fetal distress was the leading fetal indication and it accounted for 12.5% of all cesarean sections performed in this study. This was higher than 6% reported from Jimma Hospital, Ethiopia [14] and lower than 26.6% reported from a comparative study in Tikur Anbessa Hospital, Ethiopia [18]. This variation might be attributed to less priority given for conservative management of fetal distress in Attat Hospital.
Even though the risk of maternal death after cesarean section is 5 times higher than normal vaginal delivery, there was only one death (0.4%) which is low, compared to study done in tikur anbesa (1.6%) [18]. But, the overall maternal morbidity rate was 27 (9.7%) which is slightly lower than 20% reported from Jimma Hospital, Ethiopia. Mothers with ANC follow up have good postoperative outcome as compared with ladies with no DNC follow up (P<0.001, COR=0.16, 95% CI=(0.06, 0.935) which is similar to other studies [14].
The most common post-operative complications were respiratory tract infection 7(2.5%) and post op fever 6(2.1%) which were also the leading complications reported from a study done in Sultan Qaboos University [32], Oman. The reduction of post-operative complication might be because of routine use of prophylactic antibiotics associated with clinically important reduction in postpartum febrile morbidity, wound infection and other serious infections. The patients with postpartum hemorrhage were successfully managed with uterotonics. And there was 4(1.4%) mothers transfused with cross-mated blood in this study which is relatively very much low when compared to study done in Tikur Anbesa (19%) [14]. Low morbidity from anesthesia could be due to the use of spinal anesthesia for the majority of Cs cases. The gross Perinatal Mortality Rate (PNMR) of 64/1000 live births was not statistically higher than the rate for all deliveries, which was 73/1000 live births. This figure is lower than 120/1000 live births reported from Jimma University, but similar to 62.4/1000 live births from Tikur Anbessa Hospital, Ethiopia [14,18]. The common causes of perinatal mortality were, birth asphyxia (2.1%), APH (1.4) and prematurity (1.4%), obstructed labor (1.4) which are in similar with other studies [18].
Conclusion
Although the cesarean section rate of 27.6% observed in this review is above the 15% recommended by World Health Organization (WHO) for developing countries, the perinatal outcome is not improved. If unchecked, the rate might reach unacceptable levels. Cesarean sections performed for appropriate medical or obstetric indications are life saving for both the mother as well as the new born. But the high prevalence of Cs is not associated with improved perinatal outcome and it has risks for the mother and the neonate. Therefore to reduce the high prevalence of Cs, each case should be thoroughly evaluated to determine the possibility for vaginal delivery. As a result, this study confirms that even though the cesarean is of the most commonly performed surgical procedures today; it is not without risks. The result of this study agrees with the other authors that the routine use of prophylactic antibiotics helps reduce the morbidity associated with cesarean sections.
Recommendation
Because the previous cesarean section was the major maternal indication, it is recommended that trial of vaginal birth after cesarean section should be encouraged in appropriate cases. In addition, for those cases with more than three scars, Bilateral Tubal Ligation (BTL) should be done after appropriate counseling. Use of cardio topography for continuous fetal heart rate monitoring in labor with confirmation of suspected fetal distress through fetal acid-base study is also recommended if resource is available.
Furthermore, time has to be given for conservative management of fetal distress rather than rushing to operation theatre with a single episode of fetal heart rate abnormality. There is a need for a prospective study to evaluate the reasons for the increasing cesarean section rate in this Hospital. Since cephalopelvic disproportion is the common indication associated with increased Cs rate, the woreda, Zonal and National management bodies are responsible to prevent this problem through avoidance of malnutrition and poverty by enhancing food security.
Authors' Contributions
Authors carried out the study and participated in the design of the study, statistical analysis and the drafting of the manuscript. All authors read and approved the final version.
Acknowledgement
We would like to extend our thanks to Jimma University for financial support to carry out this research and to Attat hospital administrative body for their permission to conduct this research in their hospital.
6742
References
- Decherney AH, Nathan L, Goodwin TM (2007) Current diagnosis and treatment obstetrics and gynecology.
- Thomas J, Paranjothys (2001) Royal College of obstetricians and gynecologists clinical effectiveness support unit. The national sentinel cesarean section audit report. RCOG Press, London, United Kingdom.
- (2001) National collaborating center for women`s and children’s health. Cesarean section:clinical guide line. ROCG Press, London, United Kingdom.
- Betrán AP, Merialdi M, Lauer JA, Bing-Shun W, Thomas J, et al. (2007) Rates of caesarean section: analysis of global, regional and national estimates. PaediatrPerinatEpidemiol 21: 98-113.
- Gibbons L, Belizan JM, Jeremy A L (2010) The global numbers and costs of additionally needed and unnecessary cesarean section performed per year , over use as a barrier to universal coverage. World health report 30: 1-4
- Tadesse E, Adane M, Abiyou M (1996) Caesarean section deliveries at TikurAnbessa Teaching Hospital, Ethiopia. East Afr Med J 73: 619-622.
- Althabe F, Belizán JM (2006) Caesarean section: the paradox. Lancet 368: 1472-1473.
- Betrán AP, Merialdi M, Lauer JA, Bing-Shun W, Thomas J, et al. (2007) Rates of caesarean section: analysis of global, regional and national estimates. PaediatrPerinatEpidemiol 21: 98-113.
- Souza JP, Gülmezoglu A, Lumbiganon P, Laopaiboon M, Carroli G, et al. (2010) Caesarean section without medical indications is associated with an increased risk of adverse short-term maternal outcomes: the 2004-2008 WHO Global Survey on Maternal and Perinatal Health. BMC Med 8: 71.
- [No authors listed] (1985) Appropriate technology for birth. Lancet 2: 436-437.
- Althabe F, Sosa C, Belizán JM, Gibbons L, Jacquerioz F, et al. (2006) Cesarean section rates and maternal and neonatal mortality in low-, medium-, and high-income countries: an ecological study. Birth 33: 270-277.
- Fisseha N, Getachew A, Hailu M, Hiwot Y, Bailey PA. National review of cesarean delivery in Ethiopia.
- Ali Y1 (1995) Analysis of caesarean delivery in Jimma Hospital, south-western Ethiopia. East Afr Med J 72: 60-63.
- Geidam AD, Audu BM, Kawuwa BM, Obed JY (2009) Rising trend and indications of caesarean section at the university of Maiduguri teaching hospital, Nigeria. Ann Afr Med 8: 127-132.
- Samil F, Hofmayer GJ (2002) Antibiotic prophylaxis for CS. Cochrane Database of systematic Reviews 10: 1465-1858.
- Olumusola A, Sasha R, Ibrahim IB (1998) Risks of Cesarean section. BMJ 317: 462-465.
- YifruBirhan, Ahmed Al (2004) Emergency obstetrics performance with emphasis on a operative delivery outcome. Ethiopian Journal of Health Development 18: 96- 106.
- (2011) Ethiopian Demographic and Health survey, Central Statistical Agency AA, Ethiopia.
- (2006) Ethiopian Demographic and Health Survey 2005 Central Statistical Agency Addis Ababa, Ethiopia ORC Macro Calverton, Maryland, USA.
- (2009) Addressing Community Maternal and Neonatal Health in Ethiopia. Report from National Scoping Exercise and National Workshop to Increase Demand, Accesses and Use of Community Maternal and Neonatal Health Services.
- Betrán AP, Merialdi M, Lauer JA, Bing-Shun W, Thomas J, et al. (2007) Rates of caesarean section: analysis of global, regional and national estimates. PaediatrPerinatEpidemiol 21: 98-113.
- Beena D, Kamath, James K, Todd, Judith E, et al. (2006) Neonatal Outcomes After Elective Cesarean Delivery
- Wanyonyi S, Sequeira E, Obura T (2006) Caesarian section rates and perinatal outcome at the Aga Khan University Hospital, Nairobi.EAMJ 83: 12.
- Geidam AD, Audu BM, Kawuwa BM, Obed JY (2009) Rising trend and indications of caesarean section at the university of Maiduguri teaching hospital, Nigeria. Ann Afr Med 8: 127-132.
- Pembe AB, Othman MK. Pregnancy outcome after one previous caesarean section at a tertiary university teaching hospital in Tanzania. Tanzania Journal of Health Research 12: 3.
- Mekbib TA, Teferi B (1994) Caesarean section and fetal outcome at Yekatit 12 Hospital, Addis Ababa,Ethiopia, 1987-1992.Ethiop Med J32: 173-179.
- Menacker F, Hamilton BE (2010) Recent trends in cesarean delivery in the United States. NCHS Data Brief: 1-8.
- Mariam M, Radha K, Vlasta V, Andrzej K (2002) Cesarean section at Sultan Qaboos University Hospital: A three year review. J Sci Res Med Sci 4: 29-32.
- Ljaiya MA, Aboyeji PA (2001)The trends of CS over a ten-Year period at Ilorin, Nigeria. The Nigerian Journal of Surgical Research 3: 12-18.
- Penn Z, Ghaem-Maghami S (2001) Indications for caesarean section. Best Pract Res ClinObstetGynaecol 15: 1-15.
- Maaike APC , Van H, Pieter WJ, Van D, Jan M (1997) Maternal consequences of CS. A retrospective study of intraoperative and postoperative complication of CS during a 10- year period. European Journal of Obstetrics Gynecology and Reproductive biology 74: 1-6.