Research Article - (2022) Volume 16, Issue 1
Prevalence of Bed-Sore and its Associated Factors among Hospitalized Patients in Medical and Surgical Wards at Yekatit 12 Hospital Medical College, Addis Ababa, Ethiopia 2018
Cheru Kore Sifir*
Department of Public Health and Nursing, Rift Valley University, Addis Ababa,, Ethiopia
Received: 24-Nov-2021, Manuscript No. iphsj-21-11684;
Editor assigned: 28-Nov-2021, Pre QC No. P-11684;
Reviewed: 14-Jan-2022, QC No. Q-11684;
Revised: 19-Jan-2022, Manuscript No. iphsj-21-11684 (R);
Published:
27-Jan-2022, DOI: 10.36648/1791-809X.16.1.907
Abstract
Background: Bed sore (BS) (also known as pressure sore (Ps), pressure injury (PI), decubitus ulcer (du), pressure ulcer (Pu), defined as an area of localized damage to the skin and subordinate tissue caused by pressure. PU leads to ischemia, cell death and tissue necrosis, capillaries are compressed, and the blood rush is limited, the cutaneous tissue turned broken or destroyed, leading to progressive destruction and necrosis of underling soft apkins.
Objective: To assess frequency of bed sore and its associated factors among rehabilitated cases in medical and surgical wards at yekatit 12 hospital medical college, Addis Ababa, Ethiopia 2018.
Method: Institution- grounded, cross-sectional quantitative study design was conducted on a representative sample of 94 rehabilitated cases in the study area from March15, 2018 to May 13, 2018.
Result: A aggregate of 7 beds sore were detected from 226 cases, with the frequency rate of3.0. Maturity of replier 6 (2.65) developed bed sore who came from the civic area and 3 (1.32) cases developed ulcer wasn't educated, and actors who had been veritably poor in nutrition was 2 (0.88) cases.
Conclusion and Recommendation: Frequency of the pressure ulcer was low among rehabilitated cases in this study, age, bedridden, position change, humidity, and nutrition were significant associated with the frequency of pressure ulcer so the frequency of pressure ulcer was low because the cases and health care professionals have knowledge about bed sore and they rehearsed it.
Keywords
Bed sore; Frequency and associated factors; Hospitalized patients; Surgical wards; Rehabilitated cases
Background
Bed sore (BS) (also referred to as bedsore (Ps), pressure injury (PI), decubitus ulcer(du), pressure ulcer (Pu), defined as a neighborhood of localized damage to the skin and underling tissue caused by pressure [1]. PU results in ischemia, necrobiosis and tissue necrosis, capillaries are compressed and therefore the blood flow is restricted, the cutaneous tissue became broken or destroyed, resulting in progressive destruction and necrosis of underling soft tissues. This process results in a pain full and slow healing of pressure ulcer [2]. Pressure ulcers remain a big problem in hospitals also as domestic and community settings. They have been described by both the national pressure ulcer advisory panel (NPUAP) and the European pressure ulcer advisory panel (EPUAP) as localized injury to the skin and or underling tissue usually over a bony prominence as a result of pressure combined with shear and it has been recognized as a major cause of morbidity. Mortality and health care burden globally [3].
Development of bed sore ulcer is complex and multi-factorial. In critical care patient, bed sore are an additional co-morbid threat in patients who are already physiologically compromised. In fact, pressure ulcers are one among the foremost underrated medical problems in critical care patients. Despite advances in medical technology and the use of formalized prevention programs based on clinical practice guidelines, the prevalence of pressure ulcers during hospitalization continues to increase (80%). Among all hospitalized patients, prevalence rates of acquired pressure ulcers was the very best in patients within the medical care unit (ICU), from 14% to 42%. Mortality is also associated with pressure ulcer. Several studies noted deathrate as high as 60% for older persons with pressure ulcers within 1 year of hospital discharge [4,5].
People are in danger of developing bedsore if they need difficulty moving and are unable to simply change position in bed. Immobility may be due to generally poor health, paralysis sedation recovery after surgery, coma, injury or wheelchair use. Other factors that increase the risk of bedsore include age, lack of sensory perception, weight loss, poor nutrition and hydration, excess moisture or dryness (Medical Group Soft). Some researchers see a parallel risk of an increasing number of pressure ulcers, usually in collection with the growing number of hip fractures which are seen as having the greatest risk association with the development of pressure ulcer [6].
Studies shows that when nurses have an acceptable knowledge and control of patient’s pressure ulcer heal well [7]. However, nutrition is a problem in practice. 25% of elderly hospitalized patients suffer from malnutrition and an albumin value below the accepted reference value (3.5 g/l).
Statement of the problem
PU represents a widespread, painful, and expensive health care problem directly associated with increased morbidity, mortality, and length of hospital stay and several risk factors, including malnutrition, are associated with the development of PU, in the literature, there have been several studies assessing the prevalence of pressure ulcers, but most are restricted to specific regions and cities, and some hospitals, clinics and specific patient groups [8].
Impacts of Pressure ulcer: pressure ulcers affect millions of people worldwide, and remain a major health problem, but the burden and incidence rate of pressure ulcers very greatly with the health care setting [3]. Studies indicated that 1 to 3 million people in the US develop pressure ulcers each year, indeed according to the joint commission, more than 2.5 million patients in US acute care facilities suffer from pressure ulcers, and 60,000 die from pressure ulcer complications each year [9].
Bed sore in Nigeria also a medical health problem with a prevalence of 3.22% studied in all adult hospital wards in the six-university hospital located in the south- western geopolitical zone of Nigeria [3].
In Ethiopia the prevalence of bed sore was high (16.8%) among hospitalized patients, prolonged length of stay in hospital, problem of friction and shearing were liable to develop bed sore [2].
Social impacts: was represented in 10 studies in terms of restricted social activity, social isolation, and impact of personal lives. Patients reported that the physical restrictions imposed by the PU treatment, restricted their social life. The need for PU treatment restricted interaction, resulting in feeling socially isolated and confined a missing family and friends. PUs and hospitalization for PU treatment affected personal relationships due to limitations in intimacy and sexual relations [10].
The main incite to conduct this study was, in our first hospital practice we saw3rd stage bed sore in female client, she was >50 years and she died lastly due to this, then we are interested to investigate more about PU (pressure ulcer) and other associated factors.
Significance of the study
The information generated from the study will benefit both service providers and client. In improving the prevalence of bed sore, particularly the quality of information provided to a hospitalized patient who develop bed sore. The findings will also provide information to health care practitioners regarding to the prevalence and associated factors of bed sore among patient who admitted in yekatit 12 hospital medical colleges.
Objectives
General objective
To assess prevalence of bed sore and its associated factors among hospitalized patients in medical and surgical wards at Yekatit 12 hospital medical college, Addis Ababa, Ethiopia 2018.
Specific objectives:
• To describe prevalence of bed sore among hospitalized patients at Yekatit 12 hospital medical college.
• To identify associated factors of bed sore among hospitalized patients at Yekatit 12 hospital medical college.
Methods and Materials
Study area
Addis Ababa is the capital city of Ethiopia, which is located in the central part of Ethiopia, with a total population of 3,384,569 and covers a geographical coverage of 540 square kilometers. The study will conduct in Addis Ababa, arada sub city around 6 kilos. The specific area was the study will conduct in Yekatit12 hospital medical college [11].
Study design and period
A facility based cross-sectional study design employing quantitative data collection method was conducted and the study period was from Jun 1-10, 2018. Pretest was conducted at zewditu memorial hospital to improve our questionnaires.
Source and study population
Source population: All hospitalized patients at yekatit12 hospital medical college.
Study population: Patients who have been admitted in medical and surgical, wards atyekatit 12 hospital medical colleges during the study period.
Inclusion and exclusion criteria
Inclusion criteria: All patients who admitted in yekatit 12 hospital medical college during the study.
Exclusion criteria: A patient who was be critically ill, was not be talk or listen at the time of interview, medical professions would be exclude from the study.
Sample size and sampling procedures
Sample size determination: The Sample size computed based on a simple proportion population formula with the prevalence (p) of pressure ulcer is 16.8%, taken from previous study in Feleghiwot referral hospital,bahir dare [2]. we used to calculate the sample size with assumptions of 95% level of confidence and 5% margin of error and 10% non- response rate [12].
Sampling procedure: The data was collected by using simple random sampling technique and the maximum sample size was 226. The average number patient coming to the study area was identified by conducting preliminary survey. Then the total sample size was distributed according with the study period.
Variables of the study:
• Dependent variable
• Pressure ulcer.
• Independent variable
• Socio demographic factors (sex, age, marital status, educational status).
Braden scales of bedsore risk assessment tools:
• sensory perception
• friction
• mobility
• nutrition
• moisture
• activity
Operational definition: Pressure ulcers are injuries to skin and underlining tissue resulting from prolonged pressure on the skin.
Braden scale source: in this study, patents were to pressure ulcer development when score <17 or with a pressure ulcer and no risk of pressure ulcer at Braden score ≤ 17.
Data collection procedure (instruments, personnel, measurements)
Data concerning prevalence and determining factors of PU (pressure ulcer) well collected through standard questioner with interview approach and physical examination techniques. The Braden scale risk assessment tool was used to assess the risk of PU and the following items: sensory perception, skin moisture, physical activity, mobility, nutrition and fraction. The Braden scale is a summit rating scale made up of six sub scales scored from 1-3 or 4 for total scores that range from 6-22. A lower Braden scale score indicates a lower level of functioning and, therefore, a higher level of risk for PU development. The standard questionnaires has prepare in English language and translate in to local/Amharic language in order to standardize the way questions was asked [13].
Data processing and analysis
Data was entered, cleaned and analyzed by using scientific calculator, frequencies, percentage in order to describe the study population in relation to relevant variables.
Ethical consideration
Ethical clearance was obtained and a formal letter of cooperation was write to yekatit 12 hospital medical college from rift valley university. The purposes and the importance of the study has to explain and oral consent was obtain from each study participants. Information was given to study participant had full right not to participant in the study if they were not willing to ensure confidentiality was explain clearly to the participants. Nursing care was given for those patients who develop bed sore during study period [14].
Result
Socio demographic characteristics of hospitalized patents
A total 226 patients was interviewed. Their socio demographic character tics are shown in (Figure 1). The majority 32% of clients were in the age range 20-30. Regarding to sex there was 123 (54.4%) female and 103 (45.5%) was male. Regarding the place of residence 198 (87.6%) from Urban and 28 (12.3%) patients was from rural area with respect to educational status majority (27.8%) of the client had grade 11 & above. In their marital status was 60(26.5%) was single, 116(51.3%) was married, 20 (8.8%) was divorced and 30 (13.3%) was windowed [15].
Prevalence of bed sore
Prevalence of bed sore with socio demographic variables: A total of 7 bed sore was detected from 226 patients, with the prevalence rate of 3%. Majority of the respondents 3(1.32%) developed bed sore was greater than 50 years, then 2(0.88%) patients were 31-40 years the rest was 20-30 and 41-50 years (0.44%) each. 6 (2.6%) developed bed sore came from the urban area because the hospital was not referral so the patients who came from rural area was 1(0.44%), and 5(2.21%) patients develop bed sore were female and the rest 2(0.88%) was male. Related to marital status 4 (1.76%) was married, 2(0.88%) was single, 1(0.44%) was divorced.
Association factors to develop bed sore: Almost half 120 (53%) admitted patients at Yekatit 12 hospital medical college had 16-30 days length of stay in hospital and 71(31.4%) patients discharged ≤ 15 days. 35(16.6%) patients stay in hospital more than 30 days.5 (2.21%) of respondents who developed bed sore were admitted ≥ 30 days.
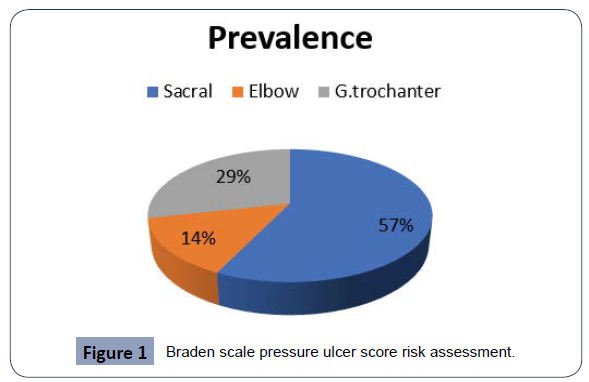
Bed sore related to different anatomical location: A patient those who developed bed sore, most of the participants 4 (1.76%) developed ulcer on sacral area. Majority of respondents 214(94.7%) had no impairment in sensory perception. From the total respondents 17(7.5%) of the patients were probable in adequate in nutrition and 5(2.2%) of the patient had potential problem in friction.
Discussion
Prevalence of pressure ulcer
Overall prevalence of pressure ulcer: In this study, the overall prevalence of pressure ulcer was 3%, this result was not higher than studies conducted in china & Nigeria with prevalence of 1.58%, 3.22% respectively. Higher prevalence in this study might be due to inappropriate nursing care, inadequate & very poor feeding habit & limited resource of pressure reliving devices. It was also found that the prevalence rate was lower than a study conducted in felegehiwote hospital (bahir dare) 16.8% brazil 16.9%, Germany 26.5%, Sweden 22.9%, Canada 25.7%, this discrepancy might be due to different characteristics of participants, disease condition of patients & also the variation of study period & length of study in hospital [16].
Prevalence of pressure ulcer with anatomical location: In this study, prevalence of pressure ulcer due to anatomical location was low (sacral, G. trochanter & elbow 1.76%, 0.88%, 0.44%) than a study conducted in china (sacral, G.trochanter & elbow 60.52%, 6-34 % & 0.79) in brazil (sacral, g. trochanter & elbow 70.4%, & 7%). This difference might be due to the disease condition of patient & variation of study area & length of study in hospital.
Prevalence of pressure ulcer with stage: In this study prevalence of pressure ulcer in stages I, II, III, IV were (32%, 0.44, 0.88, 0.44 respectively this finding was lower than the study conducted in Feleghiwot hospital (Bahirdar) 62%, 26%, 2.8% in china 28.68%, 35.82%, 12.99%, in brazil 33.3% 13.9%, in Ahmdu Bello university (Nigeria). This discrepancy might be due to different characteristics of participants, disease condition of patients & sample size the participants [17].
Conclusions
Prevalence of the pressure ulcer was low among hospitalized patients in this study, age, bedridden, position change, moisture, and nutrition where significant associated with the prevalence of pressure ulcer so the prevalence of pressure ulcer was low because the patients and health care professional have the knowledge about bed sore and they practice it.
Recommendations
Based on the finding the following recommendation for those health care providers and also the patient itself
• Health care provider should give appropriate nursing care for hospitalized patients
• Health care provider should mobilize the patient or change position two times per hour.
• Health care providing should teach to the attendants and the patients about bed sore.
• Attendant should apply the procedure
Acknowledgment
In the very beginning we would like to thank God who gives us life, health and allow as getting this chance and helps us to arrive at this stage. Secondly, would like to acknowledge Sr Bersumihret Terefe (BA, MPH) (our advisor) for her significant input to organize different aspects of this study and gives wellmeaning full about research. Finally, to our teachers, family and our friends for sharing problems while we were passing such difficulties and complicated long time.
Conflicts of Interest
The authors have no conflicts of interest to declare for this study.
REFERENCES
- Gillespie BM, Chaboyer WP, McInnes E, Kent B, Whitty JA, et al. (2014) Repositioning for pressure ulcer prevention in adults. Cochrane Database Syst Rev 2014: CD009958.
Indexedat Google Scholar Crossref
- Gedamu H, Hailu M, Amano A (2014) Prevalence and Associated Factors of Pressure Ulcer among Hospitalized Patients at Felegehiwot Referral Hospital, Bahir Dar, Ethiopia. Advances in Nursing 2014: 767358.
Indexedat Google Scholar Crossref
- Adegoke BOA, Odole AC, Akindele LO, Akinpelu AO (2013) Pressure ulcer Prevalence among hospitalized adult in University hospitals in South-west Nigeria. Wound Pract Research 21: 128-134.
Google Scholar Crossref
- Shahin ESM, Dassen T, Halfens RJG (2009) Incidence, prevention and treatment of pressure ulcers in intensive care patients: a longitudinal study. Int J Nurs Stud 46: 413-421.
Indexedat Google Scholar Crossref
- Vangilder C, Amlung S, Harrison P, Meyer S (2009) Results of the 2008-2009 International Pressure Ulcer Prevalence Survey and a 3-year, acute care, unit-specific analysis. Ostomy Wound Manage 55: 39-45.
Indexedat Google Scholar Crossref
- Mathaus-Vliegen EMH (2004) Old age, malnutrition and pressure sores; an ill–fated alliance. J Gerontol A Biol Sci Med Sci 59: 355-360.
Indexedat Google Scholar Crossref
- Brito PA, Generoso SV, Correia MITD (2013) Prevalence of pressure ulcers in hospitals in Brazil and association with nutritional status A multicenter, cross- sectional study part. Nutri 29: 646-649.
Indexedat Google Scholar Crossref
- Dorner B, Posthauer ME, Thomas D, National Pressure Ulcer Advisory Panel (2009) The Role of Nutrition in pressure Ulcer prevention and Treatment: National Pressure Ulcer Advisory Panel white paper. Adv Skin Wound Care 22: 1-15.
Indexedat Google Scholar Crossref
- Prentice JL, Stacey MC (2001) Pressure ulcers: the case for improving prevention and management in Austrelian health care settings. Prim Intent 9: 111-120.
Indexedat Google Scholar Crossref
- Jiang Q, Li X, Qu X, Liu Y, Zhang L, et al. (2014) The incidence, risk factors and characteristics of pressure ulcers in hospitalized patients in China. Int J Clin Exp Pathol 7: 2587-2594.
Google Scholar Crossref
- Houghton PE (2004) Prevalence of pressure ulcers in Canadian Health care setting. Ostomy Wound Manage 50: 22-24.
Indexedat Google Scholar Crossref
- Awwal ML, Ngaski GS, Khalid S, Muhammad SH, Farouk MA (2014) PressureUlcer stages among Bed-Ridden parients in Ahmadu Bello University Teaching Hospital (ABUTH), Zaria-Nigeria. IOSR Journal of Nursing and Health Science 3: 61-68.
Google Scholar Crossref
- Lahmann NA, Tannen A, Kuntz S, Raeder K, Schmitz G, et al. (2015) Mobility is the key! Trends and association of common care problems in German Long-term care facilities from 2008 to 2012. Int J Nurs Stud 52: 167-174.
Indexedat Google Scholar Crossref
- Petzoid T, Eberlein- gonska M, Schmitt J (2014) Which factors predict incident pressure ulcers in hospitalized patients? Br J Dermatol 170: 1285-1290.
Indexedat Google Scholar Crossref
- Lyder CH, Ayello EA (2005) Chapter 12 Pressure Ulcers: A patient Safety Issue. In: Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Hughes RG (editor). Rockville, USA.
Indexedat Google Scholar Crossref
Citation: Sifir CK (2021) Prevalence of
Bed-Sore and its Associated Factors among
Hospitalized Patients in Medical and Surgical
Wards at Yekatit 12 Hospital Medical
College, Addis Ababa, Ethiopia 2018. Health
Sci J. 15 No. 12: 907.