Research Article - (2023) Volume 11, Issue 5
Prevalence of Common Mental Disorder and Associated Factors among Patients Admitted to Medical and Surgical Ward of Dilla University Referal Hospital, South Ethiopia, 2019
Yetayale Berhanu*
Department of Health Science, Dilla University, Dilla, Ethiopia
*Correspondence:
Yetayale Berhanu, Department of Health Science, Dilla University, Dilla,
Ethiopia,
Email:
Received: 31-Dec-2021, Manuscript No. IPACLR-23-12224;
Editor assigned: 05-Jan-2022, Pre QC No. IPACLR-23-12224 (PQ);
Reviewed: 19-Jan-2022, QC No. IPACLR-23-12224;
Revised: 01-Sep-2023, Manuscript No. IPACLR-23-12224 (R);
Published:
29-Sep-2023, DOI: 10.36648/2386-5180.23.11.484
Abstract
Background: The American psychiatric association's manual
of diagnosis and statistics of psychiatric disorders, 4th
edition (DSM-IV), refers to the clinically important term
"mental disorders" for people associated with current
distress (painful symptoms). I am. It is conceptualized as a
behavioral or psychological syndrome or pattern. Or, the risk
of suffering from a disorder (disorder of one or more
important functional areas) or a significant loss of pain,
disability or freedom is greatly increased.
Objectives: To assess the prevalence of common mental
disorder and associated factors among patients admitted in
the medical and surgical wards in Dilla university referral
hospital, Dilla town and South Ethiopia, February 2019.
Materials and methods: Institutional based cross-sectional
descriptive study design was conducted by using
quantitative data collection methods. The study was
conducted at Dilla University Referral Hospital (DURH) from
December to May, 2019, which is found in Dilla town,
Gedeo zone, SNNPR, Ethiopia.
Results: 176 respondents participated in the study and the
response rate was 100%. Studies have shown that the
prevalence of common mental disorders in DURH medical
and surgical wards is 32.4%. It was found that factors such
as gender, age, financial pressure, interpersonal problems
and chronic physical diseases were significantly related to
the common mental disorders of these patients.
Conclusion and recommendations: The prevalence of
common mental disorders in DURH is high. Women, old age,
financial stress, relationship problems and chronic medical
conditions are all risk factors for a general mental disorder.
Thus, patients undergoing treatment in the therapeutic and
surgical departments should be screened for general mental
disorders.
Keywords
Common mental disorders; Prevalence; Mental
illness; Hospital patent; Self reporting questionnaire
Abbreviations
CMD: Common Mental Disorder; COPD: Chronic
Obstructive Pulmonary Disease; CVD: Cardio Vascular
Disease; DSM: Diagnostic Statistical Manual; DURH: Dilla
University Referral Hospital; GHQ: General Health Question;
HADS: Hospitalized Anxiety and Depression Symptoms; LSAD:
Legal Professionals with Stress, Anxiety and Depression;
SRQ: Self-Reporting Questionnaires
Introduction
Background
Mental health is defined as the successful performance of the
mental function related to thinking, mood and behavior that
leads to productive activities and satisfying relationships with
others; the ability to adapt to change and adversity. The
American psychiatric association's diagnostic and statistical
manual of mental disorders (DSM-IV) describes the term
"mental disorder" as a clinically significant behavioral or
psychiatric syndrome or pattern that occurs in a person who has
pre-existing ailments (painful symptoms) or disability (weakness
in one or more important functional areas) or with a significantly
increased risk of pain, disability or loss of freedom. A common
mental illness is a group of conditions of anxiety, depression and
unexplained physical symptoms that are commonly encountered
in the community and medical setting. They are a highly
prevalent mental illness that affects people of all ages and
causes distress to individuals, families and communities. Mental
illnesses are more common in the healthcare sector than in the
community and some studies have shown that up to 40% of
patients in the general medical and surgical wards were
depressed and needed treatment. Nearly 450 million people
worldwide suffer from mental disorders and neuropathies.
Lifetime prevalence ranges from 12.2% to 48.6% and the annual
prevalence ranges from 8.4% to 29.1%. Neuropsychiatric
disorders account for 14% of the global burden of disease, 75%
of which occurs in developing countries.
Due to a lack of understanding of the relationship between
mental illness and other health conditions, the burden of mental disorders can be underestimated and increase the risk of
communicable and non-communicable diseases, as well as lead
to unintentional or intentional injury. Many studies, contrary to
doctors' beliefs, indicate that most patients who are considered
worried only on arrival usually suffer from anxiety and
depression and 30%-60% of inpatients can be diagnosed. It
indicates that you may have a mental disorder. The most
common psychiatric disorder among patients admitted to the
emergency room is anxiety and most admitted patients suffer
from depression. In addition, some illnesses, especially chronic
ones, can cause mental problems due to painful experiences and
side effects. The most common diagnoses of psychiatric
disorders in a typical hospital environment are depression,
substance abuse, neurosis-related and anxiety disorders. These
are often associated with chronic medical conditions.
Statement of the problem
The term general mental illness (CMD) is a broad diagnostic
category of non-psychiatric disorders, depression and anxiety
disorders, covering most mental illnesses in the general
population. The impact of common mental health problems
worldwide is increasing. The World Health Organization has
been concerned about the growing global burden of mental
illness. It is currently estimated to account for 12% of the
world's disease burden and is expected to rise to 15% by 2020,
making it the second largest health problem in the world. This
burden is considered more severe in low-income countries
where poverty and other infectious diseases are prevalent. Not
only in developed and developing countries around the world,
mental illness is gradually being recognized as a public health
problem. Compared with the community, the prevalence of
mental illness among inpatients in general medicine and surgery
is higher, ranging from 16% to 61%. Depression, anxiety and
somatic symptom disorders are the most common psychiatric
disorders in general hospitals. Depression is a common mental
illness with a lifetime prevalence of 12% to 25% in females and
5% to 12% in males [1]. WHO emphasized that depression is the
fourth most common illness and causes physical, emotional,
social and financial problems. Depression can cause dysfunction,
poor quality of life, adverse effects on physical recovery,
increased suicide rates, increased access to medical services and
costs, leading to premature death and general health problems.
There is a possibility. Depression co occurs with a variety of
medical conditions, including pancreatic and bronchial cancer,
hypothyroidism, Cushing's syndrome and Cardiovascular Disease
(CVD).
Depression is thought to complicate the care of patients in
general hospitals in internal and surgical wards. Depressed
patients are twice as likely to use emergency department
services as non-depressed patients. In diabetes, the total health
expenditure of depressed patients is four and one-half times the
health expenditure of non-depressed patients. In chronic heart
disease, depressed patients have a higher incidence of
complications and are more likely to undergo invasive surgery.
People with COPD who also have depression spend longer in the
hospital and the burden of symptoms will increase. In Ethiopia,
based on a WHO study, 2020, it will be the second debilitating
disease of all medical and psychiatric disorders after traffic accidents, cerebrovascular accidents and obstructive pulmonary
disease. Estimated it would be. Depression is widespread
worldwide, but about 50% of patients are untreated and do not
receive treatment. Failure to diagnose and treat depression
leads to disease resistance and recurrence. In a study by the
national center of neurology and psychiatry (NIMH-ECA), anxiety
disorders were more common than any other psychiatric
disorder (8.3% of the home population surveyed). Studies have
shown that the prevalence of anxiety and depression in
hospitalized medical and surgical patients, mostly women, is
relatively high and has nothing to do with the severity of the
disease. Anxiety and depression are associated with more severe
illness perception and less improvement. Another study showed
that the prevalence of clinically significant symptoms of
depression and anxiety in patients with Chronic Obstructive
Pulmonary Disease (COPD) is around 50%, while the prevalence
of depression is high in hospitalized patients with Congestive
Heart Failure (CHF).
In a study conducted through the Hospitalized Anxiety and
Depression Scale (HADS) questionnaire in musculoskeletal
patients, the high levels of anxiety and depression detected in
this sample were psychological comorbidities in a
musculoskeletal rehabilitation environment. It shows that it is
important to screen for. Unexplained physical symptoms such as
pain, discomfort and dizziness are common in primary care and
general medical practice. Frequently changing terms for this
type of illness include functional, psychogenic, non-organic,
somatic, idiopathic and medically unexplained illnesses, as well
as a number of historical terms (twenty-five). Females report
more somatization symptoms than males, but are more
associated with mental distress than gender [2]. In situations
where physical symptoms are more tolerable than emotional or
psychological symptoms or where physical illness is more easily
treated, somatization may increase. Medically unexplainable
physical symptoms pose unique challenges for healthcare
providers. It is difficult for clinicians to understand the patient’s
symptoms; suspicion of the patient often leads to conflicts
between the patient and the provider; healthcare utilization and
related costs are high; although treatment is usually possible, it
takes time and between the patient and the provider close
cooperation.
Materials and Methods
Study design, area and period
A facility-based cross-sectional descriptive study design was
conducted from December to May 2016 at the Dilla University
Referral Hospital (DURH) in Dilla town, Gedeo zone, Southern
Nations, Nationalities, Ethiopia. DURH was established in 1977
EC/1985 GC as a zone hospital in the Gedeo zone and EC was
changed to DURH until June 11, 2001. It is 360 km from Addis
Ababa, the capital of Ethiopia and 90 km from Hawassa, the
capital of SNNPRE. At the time of establishment, about 154 staff
members were hired, 104 of whom were medical professionals
and the rest were support staff. Currently, the hospital has five
wards. That is, medical care (39 beds), surgery (26 beds), obi/gin
(9 beds), pediatrics (18 beds) and psychiatry (12 beds) [3].
Nowadays, the hospital serves around 3 million peoples from
which 95% belongs to Gedeo ethnic group. Concerning mental
health, there are 625 schizophrenia patients annually.
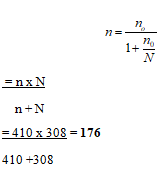
Sample size determination
The sample size was determined using a single population
proportion formula. It was calculated with the assumption of
58% prevalence of common mental disorder from the study
done in Gondar university. 0.58 P, 1.96 Z (standard normal
distribution), 95% CI, α=0.05. Considering the design effect and
adding a 10% nonresponse rate, the final sample size was 410.
Since our study population is less than 10,000, it is finite, we can
use a correction formula. The average number of patients
admitted in both wards within one month is 308 (total
population).
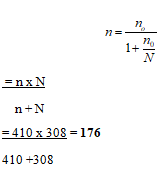
Sample techniques
Using systematic sampling techniques, 176 medical and
surgical patients were randomly assigned. The sampling period
was determined by dividing the total number of study
participants who were admitted to the medical and surgical
wards during the month of data collection by the total sample
size [4]. Relatively speaking, 77 and 99 patients were admitted
from the inpatient medical and surgical wards, respectively; the
first people from the admission record were selected by lottery.
Data collection instruments and procedures
Data were collected through face-to-face interviews, using
semi structured questionnaires, including socio-demographic
factors, clinical characteristics, Oslo 3 items, social support scale,
substance-related factors and Self-Report Questionnaire
(SRQ-20). SRQ-20 was used to evaluate the outcome variables
(common mental disorders). SRQ was originally designed by the
WHO as a self-managed scale. Due to the low literacy rate in
developing countries, SRQ-20 has also been found to be suitable
for interviewer-managed questionnaires. Each of the 20 items is
recorded as 0 or 1. A score of 1 means that the symptom has
appeared in the past month; a score of 0 means that the
symptom does not exist, participants who scored 8 or more in
the SRQ-20 in the past 4 weeks were considered to have CMD.
SRQ-20 has been validated in low- and middle-income countries.
Social support was measured using the 3-point social support
scale in Oslo. People with 3-8, 9-11 and 12-14 points were
viewed as people with little, moderate or strong social support.
The magnitude of substances such as lifelong alcohol
consumption, nicotine consumption and khat chewing was
recorded using a structured questionnaire that was developed.
The data were collected in personal interviews with a previously
tested questioner. We employed thirteen health advisors
(registered nurses) and two psychologists (MSc in integrated
clinical and community mental health) as data collectors and
supervisors, respectively [5]. The data collectors were trained
over two days for research purposes, the content of the data
collection tools, ethical issues and how to deal with study
participants. Supervisors have been trained to oversee
participant recruitment, data collection and data quality review
and control. The data-collection process was closely followed up
by the supervisors.
Data quality control issues
The questionnaire was translated into Amharic (the local
language) by a linguist who speaks Amharic and back-translated
into English by a mental health professional. The Amharic
version of the questionnaire was pretested in 5% of the total
study participants in Chefe to check the consistency and
duration of each questioner. Before accepting the interview with
the data collector, the prepared questionnaire was thoroughly
checked for completeness, objectives and variables.
Data processing and analysis
Check the integrity and consistency of the collected data,
enter the epi data 3.1 statistical software and then export it to
the SPSS windows 23 program for analysis. Calculate descriptive
statistics to explain socio-demographic characteristics, clinical
variables, psychosocial characteristics and CMD. Perform
bivariate and multivariate logistic regression analysis to
determine the relationship between the dependent variable and
the independent variable [6].
Results
Socio-demographic characteristics
A total of 176 participants were selected for the study. The
response rate was 100%. Of all the participants, 104 (59.1%)
were men. The average age of the participants was 34.53 years
and the standard deviation was ± 12.34. The majority are
Muslims by religion, with 137 (77.8%) and 33 Orthodox
Christians (18.8%) married, a total of 140 (79.5%) married, 20
(11.4%) single and 5 (11.4%). 11.4% were divorced and 11 (6.2%)
were widowed. Most of them are Gedeo 137 (77.8%), followed
by Oromo 31 (17.6%), Amharic and Grage 5 (2.8%) and 3 (1.8),
respectively [7]. Regarding the educational background of all
respondents, 88 (50%) who cannot read and write, 43 (24.4%)
who can read and write, 17 (9.7%) who studied up to
elementary school, 20 (11.4%) and 8 in junior high school. 4.5%
had higher education (Table 1).
| Variables |
Frequency |
Percentage |
| Age |
15-24 |
14 |
8 |
| 25-34 |
50 |
28.4 |
| 35-44 |
63 |
35.8 |
| 45-54 |
28 |
15.9 |
| 55-64 |
10 |
5.7 |
| 65 and above |
11 |
6.2 |
| Gender |
Male |
104 |
59.1 |
| Female |
72 |
40.9 |
| Marital status |
Single |
51 |
29 |
| Married |
105 |
59.7 |
| Divorced |
10 |
5.7 |
| Widowed |
10 |
5.7 |
| Religion |
Orthodox |
58 |
33 |
| Protestant |
84 |
47.7 |
| Muslim |
34 |
19.3 |
| Ethnicity |
Gedeo |
142 |
80.7 |
| Oromo |
13 |
7.4 |
| Amhara |
10 |
5.7 |
| Gurage |
11 |
6.3 |
| Educational status |
Unable to read and write |
84 |
47.7 |
| Able to read and write |
60 |
34.1 |
| 1-8 grade |
21 |
11.9 |
| 9-12, 9-10, grade, 10+/++ and above |
11 |
6.3 |
| Occupational states |
Unemployed |
2 |
1.1 |
| Daily laborer |
8 |
4.5 |
| Student |
10 |
5.7 |
| House wife |
31 |
17.6 |
| Merchant |
17 |
9.7 |
| Farmer |
63 |
35.8 |
| Employed |
45 |
25.6 |
| Monthly income |
<750 |
40 |
22.7 |
| 750-1199 |
84 |
47.7 |
| >1200 |
52 |
29.5 |
Table 1: Socio-demographic characteristics of respondents (n=176).
Substance use history and clinical characteristics and
stressful life event and related factors of the
participants
Among the total study participants, 112 (63.6%) had a history
of current substance use, among those 62 (35.2%) using a khat,
41 (23.3%) drinking alcohol and 9 (5.1%) used tobacco. Among
the respondents, 47 (26.7%), 25 (14.2%) and 6 (3.4%) had chronic physical illness, family history of mental illness and
history of any psychiatric illness respectively. Regarding stressful
life events, 41 (23.3%), 24 (13.6%), 23 (13.1%) and 14 (8.0%) had
financial stress, loss of loved one, relationship related and legal
related problems respectively (Table 2) [8].
| Variables response |
Frequency |
Percentage |
| Family history of mental illness |
Yes |
25 |
14.2 |
| No |
151 |
85.8 |
| Chronic physical Illness |
Yes |
47 |
26.7 |
| No |
129 |
73.3 |
| Any psychiatric Illness |
Yes |
6 |
3.4 |
| No |
170 |
96.6 |
| Stress full life event |
| Financial stress |
Yes |
41 |
23.3 |
| No |
135 |
76.7 |
| Loss of loved one |
Yes |
24 |
13.6 |
| No |
152 |
86.4 |
| Relationship stress |
Yes |
23 |
13.1 |
| No |
153 |
86.9 |
| Legal issues |
Yes |
14 |
8 |
| No |
162 |
92 |
Table 2: Clinical characteristics and stressful life event related factors of the respondents (n=176).
Prevalence of CMDS and distribustion of symptoms
Among the studies, participants who scored six and above in
SRQ-20 were considered having CMDs as follow. Prevalence of
common mental disorders was 32.4%. (11.4% males and 21%
females). In majority of the study participants, out of the total
twenty symptoms consisted in SRQ, the most commonly reported symptom during the last 30 days were feeling unhappy,
poor appetite, sleep badly, di iculty in decision, poor digestion,
di iculty to enjoy and loss of interest (Table 3) [9].
| Symptoms |
Frequency |
Percent |
| Feel unhappy |
63 |
35.8 |
| Poor appetite |
59 |
33.5 |
| Sleep badly |
57 |
32.4 |
| Difficulty to enjoy |
56 |
31.8 |
| Easy tired |
52 |
29.5 |
| Feel nervous, tens or worried |
48 |
27.3 |
| Lost interest in things |
45 |
25.6 |
| Unable to play a useful part in life |
44 |
25 |
| Easily frightened |
44 |
25 |
| Feel tired all the time |
43 |
24.4 |
| Daily work suffering |
39 |
22.2 |
| Difficulty in decision making |
31 |
17.6 |
| Feel worthless person |
27 |
15.3 |
| Headache |
27 |
15.3 |
| Poor digestion |
26 |
14.8 |
| Trouble in thinking |
25 |
14.2 |
| Thought of ending life |
23 |
13.1 |
| Crying |
22 |
12.5 |
| Uncomfortable feeling in stomach |
21 |
11.9 |
| Hand shake |
11 |
6.2 |
Table 3: Distribution of SRQ symptoms among the study participants (n=176).
Factors associated with common mental disorders
Associations were based on age, gender, marital status,
education, profession, income, financial stress, relationship
problems, traumatic stress, current substance use, family history
of mental and chronic physical illness. Gender, age, financial
stress, relationship problems and chronic medical conditions
have been found to be significantly associated with common
mental disorders. General mental disorders and female gender
had significant associations. Women admitted to DURH were
twice as likely to have AMD as men. In persons aged 25-34 years,
the likelihood of developing an IUD was approximately 3.37
times higher than in persons under the age of 25, the age of
35-44 increased 3 times, 45-54 years increased 4.5 times, 55-64
years increased by 2.57 times and at the age of 65 and over 5
several times increase the likelihood of AMD compared with
people under 25 years of age. Those who reported financial
stress, relationship problems and living with chronic physical illness were 2.6, 2.3 and 2 times more likely to develop CMDs
when compared to those who did not report, respectively [10].
Discussion
This study tried to use SRQ-20 to determine the prevalence of
common mental disorders among patients admitted to medical
and surgical wards, as well as the association of certain sociodemographic
characteristics, clinical and substance use
variables. The overall prevalence of CMD was found to be 32.4%.
11.4% males and 21% females, the prevalence of common
mental disorders in this study is lower than studies conducted in
other parts of the country. According to a cross-sectional study
conducted at the Kuwait general hospital, 122 (41.4%) of the
295 medical and surgical inpatients studied were found to have
manifestations of one or more mental illnesses. In addition, a
study by the general medical institution in Kenya showed that
out of a total of 2770 male and female hospitalized patients, 42.3% were screened for CMD. This difference may be due to
differences in population, study area and socio-culturally
between the two study populations. Similarly, the results of this
study were lower than those conducted elsewhere in Ethiopia.
Cross-sectional studies conducted on patients admitted to
government hospitals, Mek'ele, Tigray and Ethiopia showed
about half (54.6%) of the study participants. In an intuitive
cross-sectional study from the internal medicine and surgery
department of depressive Gondar university hospital, the
prevalence of AMD among inpatients was 58.6%. Differences in
the equipment (screening and diagnostic tools) they used
((HAADS), (SRQ-25)), socio-cultural characteristics, time
duration, sample size, economic differences and the prevalence
of the surveyed population may explain the inequality. While
this study was heavily related to gender differences, women are
twice as likely to develop an IUD as men. This is consistent with
other studies done in Kuwait and Gondar. The increase in the
prevalence of female CMD may be due to more responsibilities,
such as taking care of children, caring for other family members,
other hormones or biological mechanisms, women’s traditional
role in society, which puts women under greater pressure and
prevents them from changing their stressful environment, high
levels of domestic violence and sexual violence suffered by
women. The positive correlation between the age group and
CMD seen in this study has also been reported in different
previous studies in Kuwait, Mekle and Gondar. This finding may
be because people over 60 are five times more likely to develop
CMD than people under 25 [11-13].
The possible reasons may be that the elderly are at increased
risk of chronic diseases, facing social isolation, economic
difficulties and other related social problems, which may
increase the incidence of mental illness. In this study, there is a
correlation between stressful life events and CMD. Among
people who have experienced financial stress and interpersonal
relationship problems in the past 6 months, the likelihood of
suffering from common mental disorders is about The latter is
twice and a half, stress and relationship problems. A study
conducted in other areas also supports a significant association
between financial stress and interpersonal problems and
common mental disorders. Among people who report chronic
physical illnesses, the prevalence of CMD is higher. Compared
with people who have not reported, people with chronic
physical diseases are about twice as likely to suffer from
common mental disorders. There are other hospital-based
studies that report a positive correlation between chronic
physical illness and CMD in Ethiopia. A possible explanation may
be that people with chronic physical diseases may be restricted
in their daily activities and feel dissatisfied with life, which may
make them feel depressed and anxious; therefore, it may
increase the risk of acquiring CMD [14,15]. Among the variables
that entered the multivariate analysis, marital status, education
level, interviewee's job, health risk, loss of relatives, traumatic
stress, family history of mental illness and current substance use
were not related to CMD.
Limitations of the Study
Some of the patients admitted in surgical wards are refused to
give information and withdraw the interview because of the
pain of illness.
Conclusion
Prevalence of common mental disorders in DURH is high.
Being female, older age, financial stress, relationship problems
and chronic physical illness are risk factors for the development
of common mental disorder. Patients who are treated in medical
and surgical wards should be screened for common mental
disorders.
Ethical Consideration
To carry out this research project, the ethical approval of the
department of psychiatry, department of health sciences, Dilla
university, will be submitted to DURH. A more formal consent
form was obtained from the research only used for research and
kept confidential. During the study period, the participant has
informed him of the right to withdraw from the study at any
time. Interviewees were informed of the purpose of the
procedure, the risks and benefits and the privacy and
confidentiality of the research.
Consent for Publication
Not applicable.
Availability of Data and Materials
The data that support the findings of this study has a sort of
identifier of individual participants and researcherreserved to
send it.
Competing of Interest
All of the authors declare they have no conflict of interest.
Funding
Not applicable.
Author Contributions
YB has contributed in idea conception, topic selection and
writes up of proposal for funding, contributed idea generation in
title selection and AE contributed in organizing literatures
important to the study, commented both proposal draft and
result.
References
- Sim K, Rajasoorya C, Lam KN, Chew LS, Chan YH (2001) High prevalence of psychiatric morbidity in a medical intensive care unit. Singap Med J 42: 522-525.
[Google Scholar] [PubMed]
- Marchesi C, Brusamonti E, Borghi C, Giannini A, Di Ruvo R, et al. (2004) Anxiety and depressive disorders in an emergency department ward of a general hospital: A control study. Emerg Med J 21: 175-179.
- Himelhoch S, Weller WE, Wu AW, Anderson GF, Cooper LA (2004) Chronic medical illness, depression and use of acute medical services among medicare beneficiaries. Med Care 42: 512-21.
[Crossref] [Google Scholar] [PubMed]
- Egede LE, Zheng D, Simpson K (2002) Comorbid depression is associated with increased health care use and expenditures in individuals with diabetes. Diabetes Care 25: 464-470.
[Crossref] [Google Scholar] [PubMed]
- Lauzon C, Beck CA, Huynh T, Dion D, Racine N, et al. (2003) Depression and prognosis following hospital admission because of acute myocardial infarction. CMAJ 168: 547-552.
[Google Scholar] [PubMed]
- van Melle JP, de Jonge P, Spijkerman TA, Tijssen JG, Ormel J, et al. (2004) Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: A meta-analysis. Psychos Med 66: 814-822.
[Crossref] [Goolge Scholar] [PubMed]
- Ng TP, Niti M, Tan WC, Cao Z, Ong KC, et al. (2007) Depressive symptoms and chronic obstructive pulmonary disease: Effect on mortality, hospital readmission, symptom burden, functional status and quality of life. Arch Int Med 167: 60-67.
[Crossref] [Google Scholar] [PubMed]
- Jefferies K, Owino A, Rickards H, Agarwal N (2007) Psychiatric disorders in inpatients on a neurology ward: Estimate of prevalence and usefulness of screening questionnaires. J Neurol Neurosurg Psychiatr 78: 414-416.
[Crossref] [Google Scholar] [PubMed]
- von Ammon Cavanaugh S (1983) The prevalence of emotional and cognitive dysfunction in a general medical population: Using the MMSE, GHQ and BDI. Gen Hosp Psych 5: 15-24.
[Crossref] [Google Scholar] [PubMed]
- Mayou R, Hawton K, Feldman E, Ardern M (1991) Psychiatric problems among medical admissions. Int J Psych Med 21: 71-84.
[Crossref] [Google Scholar] [PubMed]
- Mikkelsen RL, Middelboe T, Pisinger C, Stage KB (2004) Anxiety and depression in patients with Chronic Obstructive Pulmonary Disease (COPD). A review. Nord J Psych 58: 65-70.
[Crossref] [Google Scholar] [PubMed]
- Gureje O, Simon GE, Ustun TB, Goldberg DP (1997) Somatization in cross-cultural perspective: A World Health Organization study in primary care. Am J Psych 154: 989-995.
[Crossref] [Google Scholar] [PubMed]
- Russo J, Katon W, Sullivan M, Clark M, Clark M, et al. (1994) Severity of somatization and its relationship to psychiatric disorders and personality. Psychos 35: 546-556.
[Crossref] [Google Scholar] [PubMed]
- Piccinelli M, Simon G (1997) Gender and cross-cultural differences in somatic symptoms associated with emotional distress. Int Stud Prim Care Psychol Med 27: 433-444.
[Crossref] [Google Scholar] [PubMed]
- Richardson RD, Engel Jr CC (2004) Evaluation and management of medically unexplained physical symptoms. Neurol 10: 18-30.
[Crossref] [Google Scholar] [PubMed]
Citation: Berhanu Y (2023) Prevalence of Common Mental Disorder and Associated Factors among Patients Admitted to Medical and Surgical Ward
of Dilla University Referal Hospital, South Ethiopia, 2019. Ann Clin Lab Res. Vol.11 No.5: 484.