Keywords
Institutional delivery; Prevalence; Antenatal care; Mizan-aman
Background
Institutional delivery is a delivery that has taken place in any medical facility owned by skilled delivery assistance [1]. Appropriate delivery care is crucial for both maternal and prenatal health and increasing skilled attendants at birth is a central goal of the safe motherhood (SMH) and child survival movement. Skilled attendance at delivery is an important indicator in monitoring progress towards millennium development goals (MDGs) to reduce the maternal mortality ratio by three quarter (75%) between1990-2015 [2].
In one of the sub-Saharan Africa countries, Uganda, proportion of mothers delivering at health facilities has been persistently low. But the rates are even lower in rural areas [3]. In Ethiopia where 85% of the population lives in rural area availability of heath service, especially maternal health care service is extremely difficult. Over all access to maternity care is on average 23% for rural and 52% for urban area. These findings clearly indicate that there is high need and much should be done in collaboration with partners in order to achieve Millennium Development Goals (MDG). Most of the deaths occur in the rural parts of the country and most are avoidable. The prevention of maternal and neonatal mortality is a priority for the Ethiopian Government, the UN(United Nations) and WHO (World Health Organization) with MDG 4 and 5 calling for a two-thirds decrease in neonatal mortality and three-fourths decrease in maternal mortality respectively by 2015 [4].
The world figure estimated on maternal mortality rate to be 400/ 100,000 live births. It is higher in Africa (830) followed by Asia (330), Oceania (240), Latin America and Caribbean (199) and at the bottom the developed countries which was 20 [5].
Every day at least 1600 women die worldwide from the complication of pregnancy and child birth, 90% of which occurring in Asia and sub-Saharan Africa. Maternal mortality rate was shown to have the largest discrepancy between developing and developed countries among others. A life risk of mothers’ death in developing countries was forty times higher than that of developed countries [6].
In Ethiopia maternal mortality rate was continuous to be unacceptably high level 673/100,000. As Ethiopian Demographic and Health Survey (EDHS 2011) has shown the maternal mortality was 676/100,000 live births, for the seven years period preceding the survey which was not significantly different from EDHS 2005 report 673/100,000 live birth. The major causes of maternal death in Ethiopia are similar to most developing countries such as infection, hemorrhage, obstructed labor, abortion and hypertension in pregnancy [7]. Serious disease and disabilities which include prolonged uterine rupture, pelvic inflammatory disease, fistula, incontinency and pain during sexual intercourse as a result of inadequate or inappropriate care during pregnancy and delivery affect child bearing women [5].
The proportion of women who delivered with assistance of skilled attendant is one of the indicators in meeting the MDG5. In almost all countries where health professionals attend more than 80% of deliveries, maternal mortality is below 200/100,000 live births. The study conducted in Sekela district Amhara region showed that the percentage of institutional delivery was about 3.5% in EDHS 2005 which in turn was much lower than the national level [8].
Proper medical attention and hygienic conditions during delivery can reduce the risk of complication including infection that may lead to death or serious illness of mothers and baby or both. Hence, an important component in the effort to reduce the health risks of mothers and children is to increase the proportion of babies delivered in a safe and clean environment and under the supervision of health professionals [7,9]. Hence the purpose of this study was to determine the status of skilled delivery service utilization.
Conducting a study on assessment of prevalence of institutional delivery has a great importance to bring behavioral change on the community under the study. According to EDHS 2005, maternal mortality rate in Ethiopia was high. But there was no research done in this area regarding mortality and morbidity of mothers related to unsafe delivery. Therefore, this study was aimed at assessing prevalence of institutional delivery.
Methods
Study area and period
Kometa sub-locality is located in Mizan-Aman town, Bench Maji zone, south west Ethiopia. It has 1260 households and 6003 population. About 85% of population depends on agriculture and the main cash crop of economic source is coffee and fruit. There is one Hospital in Mizan –Aman.
Study design
Community based cross sectional study design was conducted among randomly selected child bearing age women.
Source population
All child bearing age women who gave birth in the last 5 years in the town regardless of their birth outcome were included in the sample.
Study population
The study population was all child bearing age women.
The sample size
Single population proportion formula was used to calculate sample size. The following assumption was made. Proportion of institutional delivery in Ethiopia P=10% [7], d=0.05%, CI=95% (Za/2=1.96) and 5% non-respondent rate.
N = Za/2 p(1− p) / d2
=1.962 (0.1)(1− 0.1) / (0.05)2
=140
Adding 5% non-respondent rate the sample size was =147
Considering design effect of 1.5 the final sample was 220.
Sampling method
Eligible women were selected using simple random sampling techniques during data collection. Kometa kebele (sub-locality) has 8 villages and from those villages 4 were randomly selected and from each randomly selected village 55 participants were selected by using systematic random sampling. When two or more women were available in the same household, lottery method was used to conduct interview. When there was no eligible woman in the selected household during data collection, the nearest household was included in the study.
Data collection procedure
Data was collected using structured questionnaire developed based on the objective of the study after thorough review of different literatures. The questionnaire was prepared in English and later translated to Amharic. Data collection was focus on the following themes: institutional delivery, place of delivery, factor affecting institutional delivery. The questionnaire was assessed for necessary data then the questionnaires modified in relation to the objective of this study. Data was collected by trained health science students.
Data quality assurance
The data collectors were trained on the data collection technique. The questionnaire was pretested and modified. Each completed questionnaire was checked immediately after returning from interview to ascertain that all the questions were answered consistently.
Data analysis procedures
The collected data was analyzed by using scientific calculators, manually and presented by graph, tables and charts. Data was kept with soft copy or hard copy after it is checked for its completeness, entered, cleaned and rechecked.
Ethical consideration
Ethical clearance and approval was sought from Mizan-Tepi University, college of health science. Formal letter requested to the kebeles. Consent was obtained from the study participants. Data was collected after informing about the objective of the study and the benefit and the fact that they have the right to decide not to participate in the study. Confidentiality was kept during data collection and thereafter.
Results
Sociodemographic characteristics study participants in kometa sun-locality, 2013
A total number of 220 samples, making 95% response rate were participated in the study. Two third 66(31.58%) of the study respondents i.e. women who gave birth in the last five years were between the age of 20-24 years. The majority of the respondents were married 172(82.29%). More than half were housewives 109(55.02%): almost one quarter of the respondents 52(24.88%) had no education. About 8.61% respondents’ husband had no education. More than half were orthodox Christians 115(55.02%). Nearly two-third of the respondents were in low economical level (66.50%) (Table 1).
Table 1: Sociodemographic characteristics of women in kometa kebele 2013, (N=209).
| Variable |
N (%) |
Variable |
N (%) |
| Age group |
|
Religion |
|
| 15-19 |
33(15.78) |
Orthodox |
115(55.02) |
| 20-24 |
66(31.58) |
Protestant |
44(21.05) |
| 25-29 |
38(18.18) |
Muslim |
32(15.31) |
| 30-34 |
26(12.44) |
Catholic |
18(8.61) |
| 35-39 |
29(13.87) |
Ethnicity |
|
| 40-44 |
14(6.69) |
Bench |
86(41.14) |
| 45-49 |
3(1.43) |
Kafa |
52(24.88) |
| Marital status |
|
Amara |
42(20.9) |
| Married |
172(82.29) |
Sheka |
16(7.66) |
| Single |
6(2.9) |
Oromo |
13(6.22) |
| Divorced |
16(7.66) |
Income |
|
| Widowed |
15(7.17) |
<500 |
139(66.50) |
| Occupation |
|
500-1000 |
55(20.31) |
| Farmer |
46(22.00) |
>1000 |
15(7.17) |
| House wife |
109(55.02) |
Distance to reach HF |
|
| Daily labor |
10(4.78) |
<2km |
127(60.16) |
| Employee |
28(13.39) |
>2km |
82(39.23) |
| Merchants |
16(7.66) |
Time to reach HF |
|
| Mothers education |
|
<30min |
107(51.19) |
| Illiterate |
52(24.88) |
>30 min |
102(46.80) |
| 1-4 |
84(40.19) |
|
|
| 4-9 |
50(23.92) |
|
|
| 10-12 |
23(11.00) |
|
|
Institutional delivery
Regarding the place of delivery, among 209 respondents nearly two-third of respondents 139(66.50%) delivered at health facility and nearly one-third of the respondent 70(33.50%) delivered at home: of those who delivered at home only 5(7.14%) were assisted by skilled personnel and about 58(82.86%) did not know the effect of home delivery (Table 2).
Table 2: Frequency distribution of recent place of delivery, assistance during delivery for recent birth and reason for home delivery in kometa kebele, 2013.
| Variable |
Frequency (%) |
Place of recent delivery
Home
Hospital |
70 (33.49)
139(66.5) |
Assistance during delivery at home
TBA
Education skilled person
Relative
Neighbor |
34(48.57)
5(7.14)
15(21.42)
40(57.14) |
Reason at home delivery recently
Easily labor
Transport problem
Health facility far
Don’t know effect |
55(78.57)
32(45.7)
15(21.42)
58(82.86) |
Obstetric history
Among 209 respondents about 160(76.56%) women gave birth more than three times and of this 84(40.02%) had more than three children. Majority of the respondents’ age at first marriage was between age of 15-19 years 110(52.63%) and age at first delivery was between 20-24 years 109(52.15%) (Table 3).
Table 3: Percentage distributions showing obstetric history of women in kometa kebele, 2013.
| Variable |
Frequency |
| Total number of pregnancy |
|
| 1-2 |
30(14.35) |
| 3-4 |
160(76.56) |
| 4-5 |
39(18.66) |
| Number of children |
|
| 1-2 |
92(44.01) |
| 3-4 |
84(40.02) |
| +5 |
28(13.40) |
| Age at first marriage |
|
| 15-19 |
110(52.63) |
| 20-24 |
65(31.1) |
| +25 |
34(16.27) |
| Age at first delivery |
|
| 15-19 |
71(33.97) |
| 20-24 |
109(52.15) |
| +25 |
3(1.44) |
Ante natal care follow-up
Out of 209 respondents about 172(82.3%) had got health education and of this about 120(69.77%) had got education by HEW (Health Extension Workers) and 52(30.23%) by CHWs (Community Health Workers). Majority of the respondents attended ANC 179(85.65%), out of this, 146(69.86%) had visited once. Among those who attended ANC about 108(60.34%) had follow up because of they got good service. Among respondents 20(14.35%) didn’t attend ANC, out of this 19(95.00%) didn’t know importance and 8(40.00%) said that health facility was far (Table 4).
Table 4: Percentage distribution showing history of antenatal care follow-up among women in kometa kebele 2013.
| Characteristics |
Number (%) |
Number (%) |
| Yes |
No |
| Those who get HE |
172(82.3) |
37(17.7) |
Who give HE:
HEW
CHW |
127(69.77)
52(30.23) |
52(30.23)
127(69.77) |
| Attend ANC |
179(85.65) |
20(14.35) |
Number of visit
1st visit
2nd visit
3rd visit
4th visit |
146(69.86)
118(56.46)
72(34.45)
51(24.40) |
53(30.14)
61(43.54)
107(65.55)
128(75.60) |
Reason for follow up
Sick
Health facility near
Good service
Husband encourage
To know health status |
30(16.76)
70(39.1)
108(60.34)
40(19.14)
20(9.57) |
149(83.24)
109(60.90)
71(39.66)
139(80.86)
159(90.43) |
Reason not follow up
No health problem
Work load
Health facility far
Don’t know importance |
18(90)
16(80)
8(40)
19(95) |
12(10)
14(20)
22(60)
1(5) |
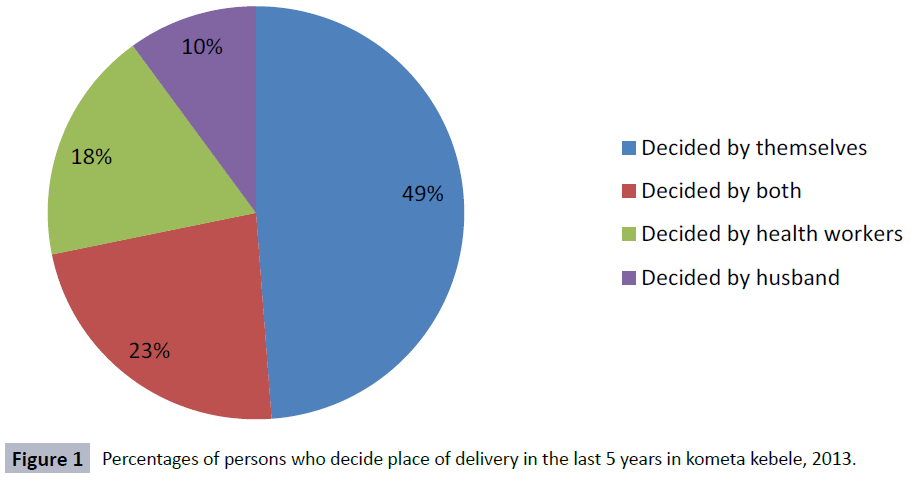
Decision on place of delivery
Out of all 209 respondents only 102(48.80%) were decided place of delivery by themselves, 48(22.97%) by both women and their husbands, 38(18.18%) and 21(10.05%) by health worker and her husband respectively (Figure 1).
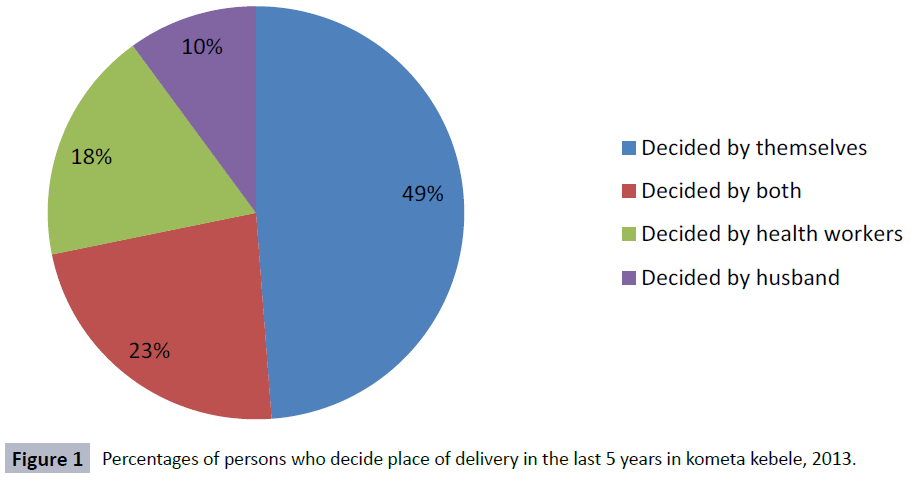
Figure 1: Percentages of persons who decide place of delivery in the last 5 years in kometa kebele, 2013.
Out of all the respondents who were asked about the next place of delivery 23(11.00%) and 186(88.00%) wanted to give birth at home and health facility respectively.
Discussion
Our study tried to identify prevalence of institutional delivery among women with in reproductive age group living in kometa kebele. This study revealed that among 209 respondents who were asked about ANC follow up in the last five years; about 85.65% had ANC follow up prior to the study, while the rest had no ANC follow up. This was high compared to the study conducted in Jhang district in Pakistan and Sahrti Samre district Tigray where 34.6% and 54% of women had ANC follow-up respectively [5]. The fact that majority of those who attend ANC were might be due to information they got from health personnel or it could be due to availability and accessibility of health facility near to their area of living and husband encouragement or it might be due to our small sample size relative to the study which is conducted in Pakistan and Tigray respectively. Our study result was also higher than the study conducted in Mizan health center (near to the current study area) which was 47.9% [10]. This could be because those coming to mizan health center may be from rural area where as our study participants were from urban area. Among the respondents who follow ANC 75.11% were literate On contrary this is higher than the study conducted in the 2005 EDHS which was 21% [5,9]. This could be due to that our study area was relatively urban.
Regarding place of recent delivery, majority of the respondents 139(66.50%) delivered at health facility recently and of this about 69.86% had received ANC from the trained health professional at least once for their last birth. This was high when compared to the study of 2011 EDHS result which was 34% and the study conducted in Tanzania which was 56% [7,11]. Our study result of institutional delivery was also higher than the study conducted in Awi zone which was 15.7% [24]. In our study prevalence of home delivery was 33.5%. This was lower compared with the study conducted in Oromia region which was 81.8% [12,13]. Our study result of home delivery was also lower than the study conducted in Arbaminch zuria district which was 79.8% [14]. Concerning skilled birth attendants about 5(7.14%) delivered at home by skilled birth attendants. However, this was low compared to the study conducted in Burji special province which was 15% [7].
Concerning the issue of women decision making power, this study showed that 102(48.80%) able to choose place of delivery. But another research conducted in Harar in Eastern Ethiopia showed that 61.5% were able to choose place of delivery which was higher [15].
Conclusion
The prevalence of institutional delivery was high. This could be achieved due to high ANC utilization. Therefore efforts should be made to sustain ANC utilization in the study area.
8302
References
- Spiegel PB, Hering H, Paik E, Schilperoord M (2010) Conflict-affected displaced persons need to benefit more from HIV and malaria national strategic plans and Global Fund grants. Confl Health 4: 2.
- Ashley (2006) Uganda bureau of statics: UDHS 2006 Caiverton marbland .ORCmacro.
- EPH 22nd Annual public health conference October 31st - November 3rd 2011, No 3
- Addis Ababa (2005) Ethiopian Central Statistical Authority, Ethiopia demographic and health survey 2005. Central Statistical Authority, Ethiopia.
- Addis Ababa (2011) Central Statistical Authority. Ethiopia demographic and health survey 2011. Central Statistical Authority, Ethiopia.
- Hailu N (2010) Asssessment of ANC followup among reproductive age group.Ethiop J Health Dev 24: 228.
- Henok A,Getachew HWH, Workiye H (2015) Knowledge, Attitude and Practice of Antenatal Care Service among Married Women of Reproductive Age Group in Mizan Health Center, South West Ethiopia. J Med Physiol Biophys 16: 53-59.
- Wolelie A, Aychiluhm M, AwokeW (2014) Institutional delivery service utilization and associated factors in Banja District, Awie Zone, Amhara Regional Sate, Ethiopia. Open J Epidemiol 4: 30-35.
- Mageda K, Mmbaga EJ (2015) Prevalence and predictors of institutional delivery among pregnant mothers in Biharamulo district, Tanzania: a cross-sectional study. Pan Afr Med J 21: 51.
- Fikre A, Demissie M (2012) Prevalence of institutional delivery and associated factors in Dodota Woreda (district), Oromia regional state. Ethiopia Reprod Health 9: 33.
- Bisrat A (2004) Magnitude and factors affecting safe delivery service utilization Harer Bulletin of Health .