Keywords
Prevalence; Occlusion; Epidemiology; Lesions; Para function
Introduction
In dentistry, the gradual loss of teeth and replacement by total dentures motivated the restoration cycle, aiming to maintain the teeth in the mouth [1]. However, the association of factors such as higher intake of acid diets, more brushing and higher level of anxiety resulted in the emergence of another cycle in dentistry, that of non-carious lesions [1,2]. Non-Carious Cervical Lesions (NCCL) is characterized by loss of tooth structure in the cervical portion of the teeth. It may be a physiological process, due to aging or pathological when the degree of destruction creates functional, aesthetic or dental sensitivity problems [2].
NCCL is a highly complex group in clinical dental practice, especially regarding the identification of the etiological agent and the proposed treatment, once the dentinal surface begins to show some degree of sensitivity when exposed to the buccal environment, after wear of the structures (enamel and cement), thus exposing the dentinal tubules [3].
Depending on their magnitude, the lesions may also compromise the aesthetic and flexural strength of the tooth. The identification of the causal agent is above all, essential for initiating any treatment, since this will be inefficient in the long term with the persistence of the triggering factor [3]. Biomechanical theories consider the possibility that stress concentrations in the cervical region, caused by cusp flexion, could contribute, associated with other clinical factors, to the development of these lesions called abfractus [3].
Destruction processes are classified by Neville et al. [4] into four categories. The first, known as the attrition, consists of the loss of tooth structure caused by contact between opposing teeth during occlusion and mastication. It can be accelerated by inferior quality or absence of enamel, premature contacts and intraoral abrasions, erosion and grinding habit the teeth.
The second process of tooth destruction is abrasion, known as pathological loss of tooth structure by the action of an external agent, such as brushing with abrasive paste and strong horizontal brushing, and the habit of interposing pencils, toothpicks, nails, among others.
In erosion the loss of dental structure is caused by chemical process added to the bacterial interaction with the tooth, while in the abfraction the dental structure is destroyed by repeated pressure on the teeth, caused by occlusal stress, so that when occlusal forces are applied eccentrically to the teeth, the tension is concentrated in the cervical fulcrum, which can produce disruption of the chemical bonds of the enamel crystals which, once damaged, can be easily removed by erosion or abrasion.
The occlusal loads lead to flexion and tensions of compression and compression in the cervical region which causes cracks or flaws between the crystals of hydroxyapatite. Enamel fissures can lead to predominant dentin exposure on the buccal surface, and canines and premolars are more common in older age groups, increasing in number and severity, and in patients with good oral hygiene, which shows that, over time, the causal factors or the sum of these become more significant.
The morphological pattern of the lesions suggests eccentric occlusal trauma as an adjunct to the causes of loss of dental substance in the cervical region of the teeth. It is well known that abrasion, erosion or attrition may not be exclusive causes of the lesions, especially those that affect a single tooth without reaching adjacent ones.
The multifactorial etiology is evident. The main triggering factors are the occlusal load and its consequent concentration of stresses, the quality of the periodontium, the acids of the diet, the abrasion by brushing, the characteristics of the teeth of each individual and the peculiarities of the cervical region.
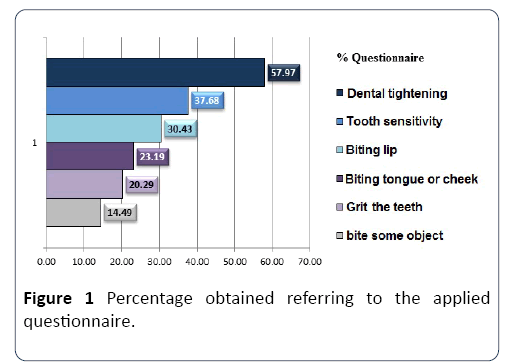
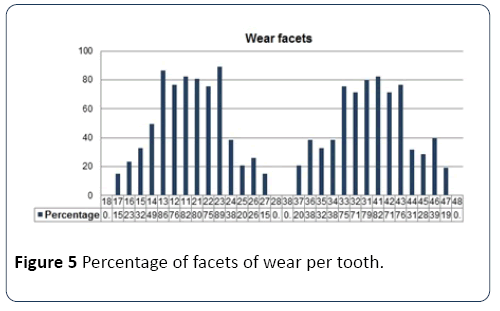
The stomatognathic system constitutes a complex system that acts on vital functions of the organism, such as breathing, swallowing, phonation and chewing. Parafunctional habits such as biting needles, pencils, pipes, tongue, lips and cheeks can cause abnormal tooth positioning and lead to traumatic occlusion, instituting damage to the structures of the stomatognathic system, including teeth (Figure 1). The behaviors cited as parafunction are thus termed as, in contrast to functional behaviors, they appear to have no functional purpose.
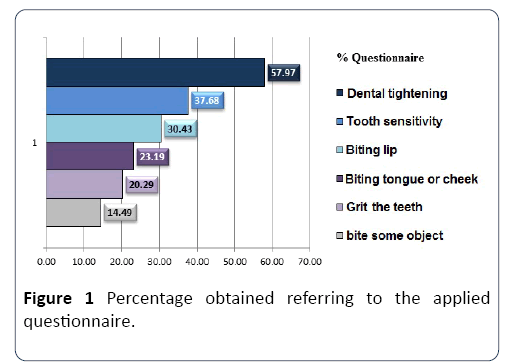
Figure 1: Percentage obtained referring to the applied questionnaire.
Habits are the result of the repetition of an act that has a purpose. Generally they are pleasant, they appear of psychological needs and they bring the personal satisfaction for the individual that realizes it. The parafunction can be defined as all the nonfunctional neuromuscular activities of the stomatognathic system, which produce hyperactivity of the cranio mandibular muscle groups and increase the internal pressure of the TMJ, leading to repetitive micro traumas on the articular surfaces, which may contribute to the appearance of temporomandibular disorders. Some alterations resulting from parafunction may be difficult to solve or even irreversible, such as malocclusions; and prevention, early diagnosis and immediate treatment are essential.
It is considered as a parafunctional habit when there is no apparent functional objective, and mainly because it presents frequency, persistence and intensity, crucial factors to exceed the threshold of resistance of the tissues and cause the appearance and progression of the signs and symptoms in the various components of the masticator apparatus. Pain resulting from one or more parafunctional habits results from the chronicity or frequency and persistence of the practice; the capacity of tissue resistance is often exceeded when the intensity is added to these factors. In addition to these, cognitive factors, anxiety and depression are adjuncts in the cause of temporomandibular joint pain (TMD). Cervical pains, headaches, internal joint disorders, lower degree of buccal opening are frequently reported by patients with parafunctional habits, such as heavy bruxism. Habit is a complex problem that fluctuates in intensity, duration and frequency.
Analyzing the influence of oral habits on the direct or indirect determination of deviations in dental morphology, it was observed that poor oral habits may be related to abnormal bone growth, poor dental position, breathing problems, phonation, oral motility disorders and psychological problems. They also alter craniofacial development, leading to malocclusions as cross bites or open bites. From the consequences of the parafunctional habits presented, it is important to prevent the habits or to treat at an early stage, since some alterations may have difficult resolution or irreversible character.
In a study by Zanini et al. [5] on harmful oral habits in patients with TMD, it was observed that all subjects had at least one parafunctional habit, while 83.0% of the patients associated five or more parafunctional activities. They then report that the type, frequency, intensity and amount of habits are important factors. The withdrawal of the parafunctional habit is considered a difficult task, since these patients, after withdrawal of parafunction, develop compensation habits.
In general, the consequences to the stomatognathic system resulting from a vicious oral habit depend on frequency, intensity, duration and individual predisposition. These factors can be increased by stress, anxiety, sleep difficulties, emotional aspects and some medications.
The two themes addressed in this research constitute real challenges for dentistry. Due to the importance of both, this work aims to evaluate the prevalence of NCCL in University of the Educational Foundation of Barretos (UNIFEB) students of Dentistry and to relate them to the presence of parafunctional habits.
The present study proposed to evaluate the prevalence of NCCL in 31 academics of the XXIV class and 38 academics of XXV class of Dentistry of the University Center of the Educational Foundation of Barretos - UNIFEB, totaling 69 academics, and, in particular, to relate the data collected with the presence of parafunctional habits.
Methods
Sample definition
The sample of the study was carried out randomly among the students of the 7th to 8th terms of the Dental Course of the University Center of the Educational Foundation of Barretos (UNIFEB). A total of 69 academics were evaluated: 38 women and 31 men, aged between 20 and 32 years, with a mean of 22.3 ± 2.7 years; independent of race and dentition with at least 20 functional teeth, that is, that act effectively in the masticatory process. The study started with the approval of the Research Ethics Committee of the University Center of the Educational Foundation of Barretos - CEP/UNIFEB.
The research was carried out in two moments, the first one in the classroom, where the questionnaires were applied to the participating students, and the second moment, in the Dental Clinics of the University Center of the Educational Foundation of Barretos - UNIFEB, which has adequate equipment to the clinical examination.
The research does not present physical, psychic, moral, intellectual, social, cultural or spiritual damages to the evaluated academics. The clinical evaluation does not have invasive intervention, so little bloody procedures. The results obtained may be converted into dental treatment to minimize possible painful and functional symptoms.
Calibration of examiners
The measurements were carried out by the same examiner. Intra-examiner reliability was assessed by the weighted kappa test, considering the depth and extent of NCCL. For this, more than 10.0% of the sample (seven patients) was examined at different times, with an interval of one hour between the exams, to avoid that the examiner could remember the values computed in the first exam. The reliability of the examiner is considered excellent for both depth (kappa=0.96) and extension (kappa weighted=1.0) [6-8].
Clinical examination
Questionnarie: The patients were clarified regarding the research and only participated so decided, by signing the Term of Free and Informed Consent - TCLE and responding to the questionnaire.
The questionnaire was based on the one presented by Leãoe- Silva [9] and contains items related to demographic information, age group, gender, medical history related to drug use, dentin hypersensitivity (air and temperature changes - cold and hot), parafunctional habits (dental tightening, bruxism, lip biting, cheeks or objects). Completion of the questionnaire was performed by the patient.
Clinical examination
After completing the questionnaire, the patients were submitted to a clinical examination to identify the presence of wear facets, considering only the presence of the facets, without measuring the degree of this wear; and other clinical signs of parafunctional etiology such as alveolar line and scalloped tongue, considering only the presence or absence, not taking into account its extent or density. These three signs, according to Serra-Negra [10], characterize the parafunctional habit called Bruxism. Besides the signs of parafunctional habits, the presence of NCCL was evaluated. The study disregarded the third molars because of instability of results, considering that the majority of the evaluated did not have these teeth.
To classify NCCL for severity, the Dental Detection Index (IDD) was used to standardize dental loss in scientific investigations and clinical practice. The IDD defines the depth of the lesions on a scale of 1 to 4 for each surface of the tooth separately. The same index was adapted to classify lesions as extension; classifying them according to Table 1.
Table 1 IDD scale for cervical teeth.
| IDD |
Depth |
Extension |
| 0 |
No contour changes No contour changes |
No contour changes No contour changes |
| 1 |
Minimum contour loss Minimum contour loss |
Minimum contour loss Minimum contour loss |
| 2 |
Defect <1 mm depth Defect <1 mm extension |
Defect <1 mm depth Defect <1 mm extension |
| 3 |
Defect 1-2 mm deep Defect 1-2 mm long |
Defect 1-2 mm deep Defect 1-2 mm long |
| 4 |
Defect >2 mm deep, or pulp exposure or secondary dentine exposure Defect> 2 mm in length |
Defect>2 mm deep, or pulp exposure or secondary dentine exposure Defect>2 mm in length |
Statistical analysis
Statistical analysis was performed using a specific program (BioEstat 5.0, Sociedade Civil Mamirauá/MCT - CNPq, Belém, Brazil), considering the null hypothesis based on the absence of correlation between the parameters (α=0.05). The unit of analysis was the patient. Correlation was assessed using the phi coefficient, which takes into account dichotomous data (presence/absence).
Results and Discussion
Sixty-nine academics from the UNIFEB Dentistry course were examined, aged between 20 and 32 years, mean age of 22.3 ± 2.7 years, being 38 women and 31 men. The mean age is similar to that of Cauás et al. [11] whose subjects were between 21 and 30 years of age, considering it to be productive in society, and characterized by intense psychological tension. This factor significantly increases the development of mandibular cranial dysfunctions.
All the students, volunteers, answered the questionnaire regarding the research. Through the answers, the following parafunctional habits were observed: 58.0% of the sample tightens the teeth; 20.3% reported grinding teeth; 30.4% have a habit of biting the lip; 23.2% have a habit of biting cheek or tongue and 14.5% bite objects. Most of the patients studied by Cauás et al. [11] also had dental tightening, bruxism, habit of biting objects, onicofagia and habit of placing a hand on the chin, which directed us as to the applied issues. Seraidarian et al. [12] reports the term parafunction for bruxism.
According to Oliveira et al. [13], one of the clinical signs for the diagnosis of eccentric bruxism is the presence of facets of wear on the incisal edges and occlusal surfaces of the teeth. The presence of linea alba in the jugal mucosa and scalloped tongue are considered clinical signs of centric bruxism. The presence of these parafunctional habits was evaluated in a clinical examination performed in all volunteer academics.
Some data obtained through the answers to the questions' 1. Do you have any health problems? 2. Do you use medication? 8. Has or has undergone orthodontic treatment; 10. What kind of brush is used? and 11. What frequency and method of brushing? 'were not used in the statistical analysis of the present study, serving only as inclusion parameters in the research. The answers to the questions considered for the present study are presented in Table 2 and Figure 1.
Table 2 Frequency and percentage of positive responses to the questionnaire.
| Question |
Frequency of positive responses |
Percentage |
| 1. Tighten your teeth? |
40 |
57.97 |
| 2. Range the teeth? |
14 |
20.29 |
| 3. Bite your lip? |
21 |
30.43 |
| 4. Bite cheek or tongue? |
16 |
23.19 |
| 5. Bite any object? |
10 |
14.49 |
| 6. Do you have dentin sensitivity? |
26 |
37.68 |
Some questions applied in the questionnaire proposed to the researched academics were based on the studies of Cauás et al. [11]. Seraidarian et al. [12] present references that cite oral habits that justify the term parafunction; in the sample surveyed this was constant.
The parafunction is evidenced in the studies 7, 9, 10, 15, 17, 22, 26, 27, 28. However, the multifactorial predominance of the lesions should not be ignored; since several factors may be involved while one or a few of them are determinants in the course of NCCL. As seen in Figure 1, dental tightening showed a higher incidence; habits of chewing lip, tongue or cheek, interposing objects between teeth and grinding teeth were also frequent among the researched academics. Factors that, as noted by the aforementioned authors, are determinant to the loss of tooth structure in the cervical region of the teeth.
Barbosa et al. [14] reports that the teeth of elderly people are more likely to develop NCCL, justified by the longer time in contact with etiological factors. However, results found in our study show a high prevalence of NCCL and parafunctional habits in a population with a mean age of 22.3 ± 2.7 years. The justification for this is in the works of Molina et al. [15] and Zanini et al. [5], which show that the onset of lesions depends on the intensity, frequency and persistence of the causal agents, together with factors cognitive, anxiety and depression; so that tissue resilience can be overcome even in young patients.
As described by Lima et al. [16] parafunctional habits are among the several etiological factors of NCCL. These habits, according to Teixeira et al. [17] generate tensions that differ from compression in the cusps in contact, for traction in the opposite cervical region. The parafunctional habits, as observed in Table 2, affect a significant percentage of the sample, sustaining the predisposition to LCNC in dependence on its multifactorial etiology, described by Rente et al. [18]. Since several factors together contribute to the loss of dental substance, one of them, the parafunction, is undoubtedly a constant in the results of the present study.
Garone-Filho et al. [19] cite the highest level of anxiety as a factor that, together with the higher consumption of acidic fruit and higher frequency of brushing, is responsible for defining the appearance of NCCL. Molina et al. [15] reinforces the importance of psychological factors as determinants to attribute a parafunctional character to a habit. These, like the answers of the studied academics, have no apparent functional objective.
Dental sensitivity is present in 26 academics or 37.6% of the sample, of these, 24 or 34.7% also have NCCL. As observed by Mondelli et al. [20] the abrasioned dentin shows very sensitive, so that when it cannot be removed with fluoride, or when depth or extension threatens the pulp or aesthetics, it indicates restoration of the lesion. Baratieri et al. [21] also indicates the restoration of lesions in cases of associated caries and interference in removable prostheses. For Rente et al. [18] with slow and progressive aggression there is obliteration of the tubules and pain from exposure is absent. NCCL is considered a pathological process when it creates functional, aesthetic or dental sensitivity problems. These, in turn, are constant since the loss of tooth structure will invariably compromise, in varying degrees, the aesthetics and function of the patient, and once exposed dentin, there is the characteristic dentin sensitivity, as evidenced by the present work. Marson et al. [22] under study found that 85.0% of the teeth with NCCL showed some degree of sensitivity. Carvalho et al. [23] reports that the pain symptomatology will recur if the treatment does not happen after elimination of the causal factors.
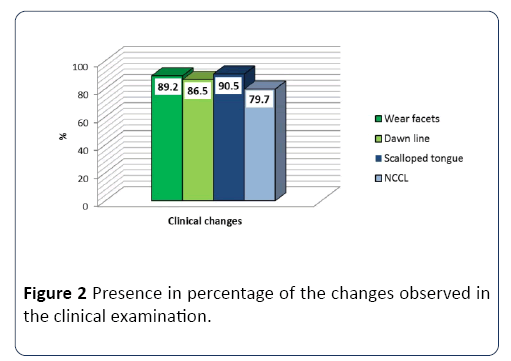
The clinical examination allowed us to observe that 89.2% of the sample presented facets of wear; 86.5% had an occlusion line; 90.5% scalloped tongue and 79.7% showed presence of NCCL, as presented in Figure 2. The association between facets of wear and NCCL is described in the study by Cantagallo et al. [24] where NCCL were diagnosed in 41.4% of the sample and 58.5% of these teeth had facets of wear in 2/5 of the teeth and 17.5% in 3/5 or more.
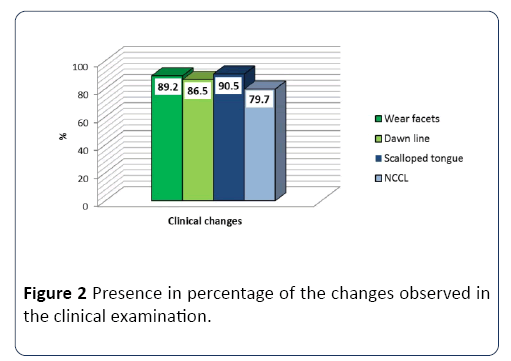
Figure 2: Presence in percentage of the changes observed in the clinical examination.
Seraidarian et al. [12], Koyano et al. [25] and Neville et al. [4] cite the clinical signs of parafunctional habit; are: albedo line of occlusion, edges of the tongue jagged (scalloped tongue) and presence of facets of wear on the incisal edges and occlusal surfaces of the teeth. These signs are observed in the clinical examination of the present study.
The relationship between the presence of clinical signs of parafunctional habits and NCCL. In it we can observe that 53 of the students submitted to the clinical examination presented this positive relation for both. Eight of these academics presented clinical signs but absence of NCCL. Six academics presented NCCL, however, absence of clinical signs of parafunctional habit; while only 2 academics in the sample showed no clinical signs of parafunctional habit, nor did NCCL.
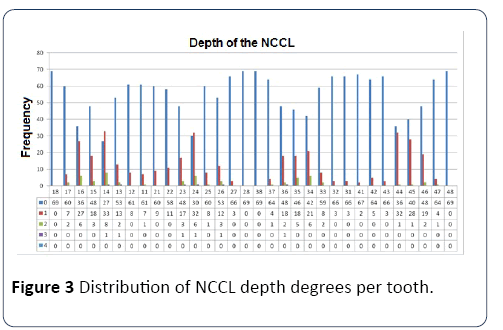
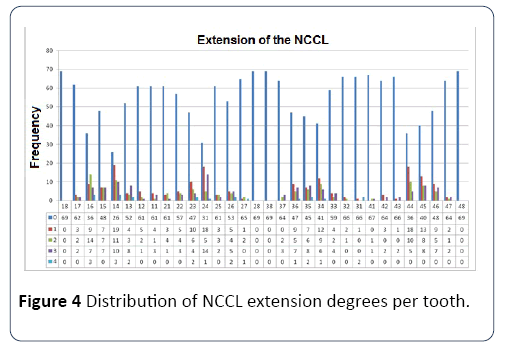
Figure 3 shows the distribution of the degrees of depth of the NCCL per tooth, while Figure 4 shows the distribution of the degree of extension of the NCCL; both classified according to the index previously proposed in the research methodology. The wear facets were evidenced in a higher percentage between the female gender (100.0%) as well as the presence of scalloped tongue (97.37%). Only 21.05% of the women did not present NCCL, but even these had at least one of the clinical signs of parafunctional habits, as shown in Figure 5. Among the males, 93.54% had an occlusion line, only 5.45% of the students did not present NCCL, while 80.64% had the four clinical signs of parafunctional habits that appeared in the research. Oliveira et al. [13] did not find significant differences between the genotypes, while Cantagallo et al. [24] report NCCL proportionally more prevalent in males (50.0%) than in females (36.3%).
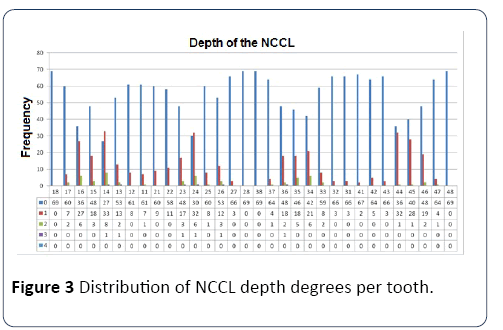
Figure 3: Distribution of NCCL depth degrees per tooth.
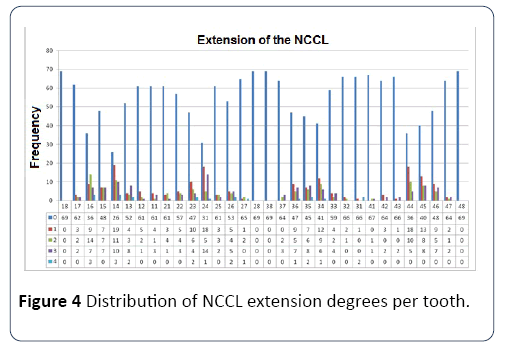
Figure 4: Distribution of NCCL extension degrees per tooth.
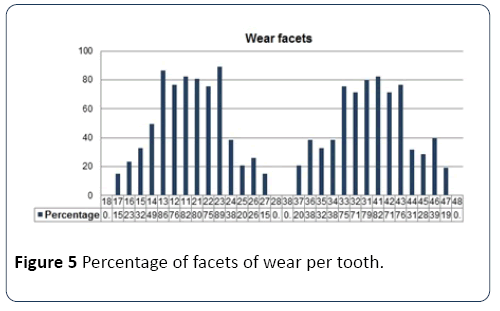
Figure 5: Percentage of facets of wear per tooth.
Further, wear facets are more frequent in anterior teeth, for the upper arch with canines predominance, right 86.3% and left 89.0%, and for the lower arch the central incisors, right 82.2% and left 79.5%. Cantagallo et al. [24] showed that 58.5% of the teeth with NCCL present a wear factor in 2/5 of the teeth and 17.5% in 3/5 or more, either alone or in combination. In the present study, teeth predominantly affected by wear facets are not those that present major involvement by NCCL, the latter being the first upper premolars (14 and 24). Telles et al. [26] classifies NCCL as a local phenomenon, given the occurrence in isolated areas of the dentition. The authors observed that the most affected teeth were the first upper molars with 17.3%, followed by the first and second premolars with 14.5%. In the present study, the prevalence of NCCL in pre-molars was similar to that reported by Teixeira et al. [17], who also cited these teeth as more affected by these lesions.
The difficulty of treatment for lesions involving parafunctional habits was reported in the studies by Zanini et al. [5] since, in removing the bad oral habit, compensation habits can be developed. Rente et al. [18] evidenced the need to record the detailed clinical history associated with a correct clinical examination. According to Garone-Filho et al. [19], the patient should be guided in relation to the etiological factors, so that the treatment becomes viable when corrected for occlusal interferences, parafunctional habits and other factors involved.
The dental tightening, or Bruxism has as clinical signs the presence of linea alba and scalloped tongue. In the present study it can be observed that in the clinical evaluation, 86.5% presented linea alba and 90.5% scalloped tongue. When we relate these data to the questionnaire response, we can see that only 57.97% report this parafunctional habit. It is evident that, much of the sample evaluated has no perception of the habit. This shows the importance of a careful clinical examination to ensure a precise orientation to the patient regarding the necessity of their participation in the maintenance of adequate posture in the oral closure.
Eccentric bruxism, whose clinical sign is the presence of facets of wear on the incisal edges and cusps was found in 89.2% while the questionnaire question referring to this item had a positive incidence of only 20.29%. This discrepancy reinforces the previously mentioned need to inform the patient about the problem, show the need for their awareness to minimize the consequences of such habits, since they are still controversial problems regarding etiology and treatment.
The NCCL and parafunctional habits were evidenced in the present study, so that no treatment was proposed because this is not the focus of the study. It was also considered the complexity of the treatment, time required, that cannot be measured by virtue of the particularities of each individual.
Through the prevalence of the clinical signs of parafunctional habits found in the clinical examination of the present study, it is possible to observe a high incidence, both of clinical signs of parafunctional habits and of NCCL. However, through the statistical test, no correlation was established between them. This occurs because the applied test can only establish this correlation when there are significant amounts of both the presence and the absence of the parameters evaluated, which did not occur in the present study, that is, a minority of the evaluated students did not show signs of the evaluated parameters. This reduced sample where the parameters evaluated were absent, made it difficult to establish the correlation between the presence of parafunctional habits and NCCL, which is the objective of our study [27]. The test can only prove that there was a tendency to this type of correlation, without, however, being able to affirm it as conclusive. In the literature review of the present study, no studies were found to confirm such correlation between clinical signs of parafunctional habits and presence of NCCL. Oliveira et al. [28] report the positive relationship for unilateral chewing and the presence of NCCL, and of the patients with NCCL, 70.45% present premature occlusal contacts.
Data correlation was assessed in two steps and a significance level of 5.0% was considered in both. In the first step, the parameters were correlated to the presence of NCCL. For this, the Phi Correlation Coefficient was calculated, which accepts dichotomous data (presence/absence). In the second stage they were correlated to the different degrees of depth and extension of the NCCL. Therefore, the Contingency Coefficient C, which accepts ordinal data (grades 1, 2, 3, and 4) was calculated.
There was no correlation between the parameters analyzed and the presence of NCCL. However, a positive correlation was observed between some of the analyzed parameters versus the depth of NCCLs and these same parameters versus the extent of NCCLs. That is, the presence of linea alba, scalloped tongue, questions 5-Habit to bite lip, 6-Habit to chew cheek or tongue, 8-Was or is under orthodontic treatment and 9. Presence of dentin sensitivity; were related to the occurrence of deeper NCCL. While the presence of linea alba, questions 5- Habit to bite lip, 6-Habit to chew cheek or tongue, 7-Habit to bite some object, and 8-Was or is under orthodontic treatment; were more often related to NCCL, suggesting that there is a probable positive correlation between the presence of NCCL and parafunctional habits, even though it is not proved by the statistical test. It is possible for the same individual to present the two types of bruxism, centric and eccentric, simultaneously. Therefore, it was also sought the correlation between NCCL and these two types of joint habits. The statistical test also did not show a significant result, as shown in items A and B of Table 3.
Table 3 Result of the correlation between NCCL presence and the parameters tested.
| Parameter |
Coefficient |
p-value* |
| Wear facet |
0.1141 |
Ns |
| Dawn line |
0.0437 |
Ns |
| Scalloped tongue |
0.1743 |
Ns |
| Tighten your teeth |
0.1003 |
Ns |
| Range the teeth |
0.1053 |
Ns |
| Bite your lip |
0.2645 |
Ns |
| Bites cheek or tongue |
0.0664 |
Ns |
| Bite some object |
0.0644 |
Ns |
| Has or has undergone orthodontic treatment |
0.0262 |
Ns |
| Has dentin sensitivity |
0.1236 |
Ns |
| A. Alba line and scalloped tongue associated |
0.0747 |
Ns |
| B. Wear facet, alba line and associated scalloped tongue |
0.0228 |
Ns |
*Coefficient of Phi correlation, Ns: Not significant
In the Tables 4 and 5 below, we also included the association of clinical findings (A and B), presenting a significant result for the correlation sought. For this parameter, again, the association of clinical data showed positive correlation, as evidenced in items A and B of the table below:
Table 4 Result of the correlation between the NCCL Depth and the parameters tested.
| Parameter |
Coefficient |
p-value* |
| Wear facet |
0.0454 |
Ns |
| Dawn line |
0.1009 |
0.0001 |
| Scalloped tongue |
0.1095 |
<0.0001 |
| Tighten your teeth |
0.0511 |
Ns |
| Range the teeth |
0.0520 |
Ns |
| Bite your lip |
0.1108 |
<0.0001 |
| Bites cheek or tongue |
0.0655 |
0.049 |
| Bite some object |
0.0636 |
Ns |
| Has or has undergone orthodontic treatment |
0.0673 |
0.040 |
| Has dentin sensitivity |
0.0728 |
0.019 |
| A. Line alb and scalloped tongue associated |
0.1009 |
0.0001 |
| B. Wear facet, alba line and associated scalloped tongue |
0.0707 |
0.026 |
*Contingency coefficient C, Ns: Not significant
Table 5 Result of the correlation between the NCCL extension and the parameters tested.
| Parameter |
Coefficient |
p-value* |
| Wear facet |
0.0516 |
Ns |
| Dawn line |
0.1022 |
0.0001 |
| Scalloped tongue |
0.0586 |
Ns |
| Tighten your teeth |
0.0289 |
Ns |
| Range the teeth |
0.0356 |
Ns |
| Bite your lip |
0.0998 |
0.0002 |
| Bites cheek or tongue |
0.1014 |
0.0001 |
| Bite some object |
0.0732 |
0.018 |
| Has or has undergone orthodontic treatment |
0.0658 |
0,048 |
| Has dentin sensitivity |
0.0629 |
Ns |
| A. Line alb and scalloped tongue associated |
0.1022 |
0.0001 |
| B. Wear facet, alba line and associated scalloped tongue |
0.0793 |
0.007 |
*Contingency coefficient C, Ns: Not significant
Conclusion
Based on the results obtained and considering the specific conditions of this study, it was possible to conclude that the prevalence of NCCL and parafunctional habits was high in the evaluated population; there was no positive and significant correlation between the presence of NCCL and parafunctional habits for the population evaluated. There was, however, a tendency for this probable correlation, although not detected by the statistical test; there was a positive and significant correlation between the presence of functional habits and NCCL and the depth and extent of NCCL; the results found justify the accomplishment of new works to elucidate existing doubts.
Conflict of Interests
There is no conflict of interest between authors.
22579
References
- Moraschini V, da Costa LS, Santos GO (2018) Effectiveness for dentin hypersensitivity treatment of non-carious cervical lesions: A meta-analysis. Clin Oral Investig 22:617-631.
- Coe J(2017) Which adhesive strategy for non-carious cervical lesions? Evid Based Dent 18: 119-120.
- Duangthip D, Man A, Poon PH, Lo ECM, Chu CH (2017) Occlusal stress is involved in the formation of non-carious cervical lesions. A systematic review of abfraction. Am J Dent 30:212-220.
- Neville BW(2004) Patologia oral e maxillofacial.Guanabara Koogan, Rio de Janeiro. pp. 54-58.
- Zanini CFC (1999)Theparafunctional habits in temporomandibular joint dysfunction [thesis].Center for Specialization in Clinical Speech-Language Pathology, Porto alegre.
- Estrela C(2001) Scientificmethodology - Teaching and research in dentistry.EditoraArtesMédicasLtda, São Paulo.pp: 303-310.
- Faria GJM, Villela LC(2000) Etiology and treatment of dentin hypersensitivity in teeth with non-carious cervical lesions. Rev Biocienc6: 21-27.
- Hoeppner MG, Massarollo S,Bremm LL (2007) Clinical considerations of non-carious cervical lesions. UEPG CiBiol Health 13: 81-86.
- Leão-e-Silva FM (2006) Non-carious cervical lesions: Presence, severity and correlation with etiological factors [thesis]. Federal University of Uberlândia, Uberlândia.
- Serra-Negra JMC(2006) Bruxism in children: internal and external reactions of subjects [thesis].Federal University of Minas Gerais, Belo Horizonte.
- Cauás M,Alves IF, Tenório K, Filho JBHC, Guerra CMF, et al. (2004) Incidência de hábitosparafuncionais e posturaisempacientesportadores de disfunção da articulaçãocrâniomandibular. Rev Cir TraumBuco-Maxilofac 4: 121-129.
- Seraidarian PI (2011) Reabilitação oral, previsibilidade e longevidade. EditoraNapoleão, São Paulo.pp: 227-247.
- Oliveira GAS, Beatrice LCS, Leão SFS(2007) Reabilitação oral empacientes com bruxismo: o papel da OdontologiaRestauradora. International J Dentistry Recife 6: 117-123.
- Barbosa LPB, Prado RR, Mendes RF (2010) Lesõescervicaisnãocariosas: Etiologia e opções de tratamentorestaurador. RevistaDentística.
- Molina OF, Gaio DC, Cury MDN, Cury SE, Gimenez SRM,et al. Uma análisecrítica dos sistemas de classificaçãosobre o bruxismo: implicações com o diagnóstico, severidade e tratamento dos sinais e sintomas de DTM associados com o hábito. JBA Curitiba 2: 61-39.
- Lima LM, FilhoHH, Lopes MGK(2005) Contribuiçãoaoestudo de prevalência, do diagnósticodiferencial e de fatoresetiológicos das lesõescervicaisnão-cariosas. Rev Sul-Bras Odontol 2: 17-21.
- Teixeira AC (2006) Análise das tensõesnosprimeirospré-molares superior e inferior, emcontato, através do método de elementosfinitos [tese]. Rio de Janeiro: Universidade do Estado do Rio de Janeiro.
- Rente AT, Pereira D, Paula A, Tomaz J, Carrillho EV(2007) Reabilitaçãoestética anterior: A propósito de um casoclínico. Rev Port Estomatol Cir Maxilofac 48: 55-62.
- Garone-filho W, Abreu-e-Silva V (2008) Lesõesnãocariosas. São Paulo: Santos.
- Mondelli J, Ishikiriama A, Galan Jr J, Navarro MFL(2005) Dentíticaoperatória. São Paulo: Sarvier. pp. 239-246.
- Baratieri LN(2001) Dentística: Procedimentospreventivos e restauradores. São Paulo: Santos.
- Marson FC, Campanholo JR, Cápua MD, BeraldoTF(2010) Avaliaçãoclínica das lesõescervicaisnãocariosas. Rev UNINGÁ 24: 137-156.
- Carvalho PASM(2010) Lesõescervicaisnãocariosas – etiologia, planos de tratamento e relação com profissões de estresse. Porto: Faculdade de Medicina Dentária - Universidade do Porto.
- Cantagallo FC(2009) et al. Avaliação da associação entre lesõescervicaisnãocariosas e forçasoclusais. Araçatuba.Faculdade de Odontologia e MedicinaVeterinária.
- Koyano K,Tsukiyama Y, Ichiki R, Kuwata T (2008) Assessment of bruxism in the clinic. Joral Rehabi l35: 495-508.
- Telles D(2000) Incidência de lesõescervicaisnãocariosasemestudantes de odontologia e suarelação com aspectosoclusais [tese]. Bauru: Faculdade de Odontologia da Universidade de São Paulo pp.1-92.
- Silva-e-Souza Jr MH, Carvalho RM, Mondelli RFL(2000) Odontologiaestética: Fundamentos e aplicaçõesclínicas. São Paulo: Santos Livraria Editora pp. 111-118.
- Oliveira ACSDamascena NP, Souza CS,et al. (2010) Análiseclínica de pacientesportadores de lesõescervicaisnãocariosas e suarelação com hábitos. Rev Sul-Bras Odontol 7: 182-192.