Key words
Refractive errors, myopia, hypermetropia, emmetropia, prevalence.
Introduction
Refractive error may be defined as a state in which the optical system of the non-accommodating eye fails to bring parallel rays of light to focus on the fovea. In myopia the optical system of the eye brings parallel rays of light into focus anterior to the fovea while in hyperopia the optical system of the eye brings parallel rays of light into focus posterior to the fovea, both resulting in blurred vision. [1-5]
It should be noticed that in mild to moderate hyperopia, blurred vision can be overcome by accommodation in youth and early adulthood, with the result that low degrees of hyperopia often are not noticed until the onset of presbyopia in middle adulthood. Myopia results in blurred vision at all ages. Most usually all types of ametropias can be corrected with spectacles, contact lenses, or refractive surgery. [1-5]
Despite the fact that refractive error is one of the most frequent reasons that people go for consulting at an eye care practitioner (ophthalmologist or optometrist) and though refractive error is the most common cause of reduced vision, there have been few population-based studies of refractive error in older populations worldwide and actually non-in Greece. Previous ophthalmic epidemiological studies have demonstrated a variability in refractive error between different ethnic groups. The majority of the early studies have been conducted in European or American populations [1-13] but recently, large-scale population-based studies have provided data about refractive errors in certain Asian regions. [14-22] These studies have generally found high rates of myopia across Asia [21-22] particularly in the younger population.
The aim of the present study was to estimate and determine the prevalence of refractive errors in persons 40 years and older at the north suburbs of Athens-Greece.
Material and Methods
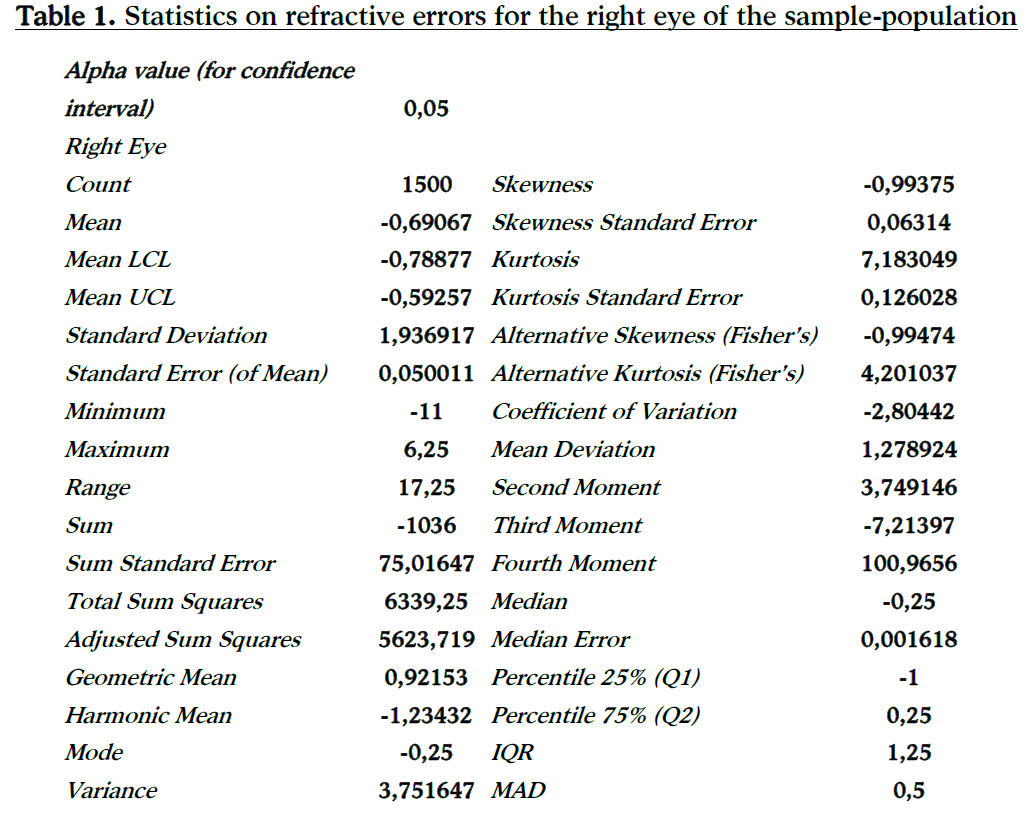
Data for the present study were obtained from a population-based survey conducted in four optometric practices based in the north suburbs of Athens and monitored by TEI of Athens department of Optics & Optometry, during the period 2006-09. The sample of participants was randomly selected from residents of the north suburbs of Athens Greece. A total of 1500 (633 men 42% and 867 women 58%) individuals participate in this survey. As part of our standardized examination, an automated objective refraction test was performed on each participant with an AutoRefractor (NIKON Speedy-1). Visual acuity was then measured with a Snellen test chart at 5 meters under standard lighting conditions, and measured initially using any corrective spectacles the participants were currently using. If the participant was unable to read the 1.0 equivalent line (6/6), subjective refraction was performed using the results of the objective refraction as a starting point. The best-corrected visual acuity was found, and both the derived refractive data and the visual acuity were recorded. When the presenting acuity of the participant was 1.0, the final refraction was recorded as the subject’s refractive data. The spherical equivalent (sphere + ½ cylinder) was used to calculate the refractive error. Because of the age of our study population, cycloplegia was not used. Myopia was defined as the spherical equivalent of < - 0.50 diopters (D). Also myopia was categorized as low myopia (-0.50 D to -3.00 D), moderate myopia (-3.00 D to -6.00 D) and high myopia (> -6.00 D). Hypermetropia was defined as the spherical equivalent of more than +0.50 D, and emmetropia was defined as the spherical equivalent of < ± 0.25 D. Because the spherical equivalents in the right and left eyes were highly correlated (Pearson Correlation Coefficient: 0.9881) data was presented at the beginning for both the right and left eye, but the rest of the statistics (astigmatism prevalence, age and gender distribution) are presented for the right eye only.
Results
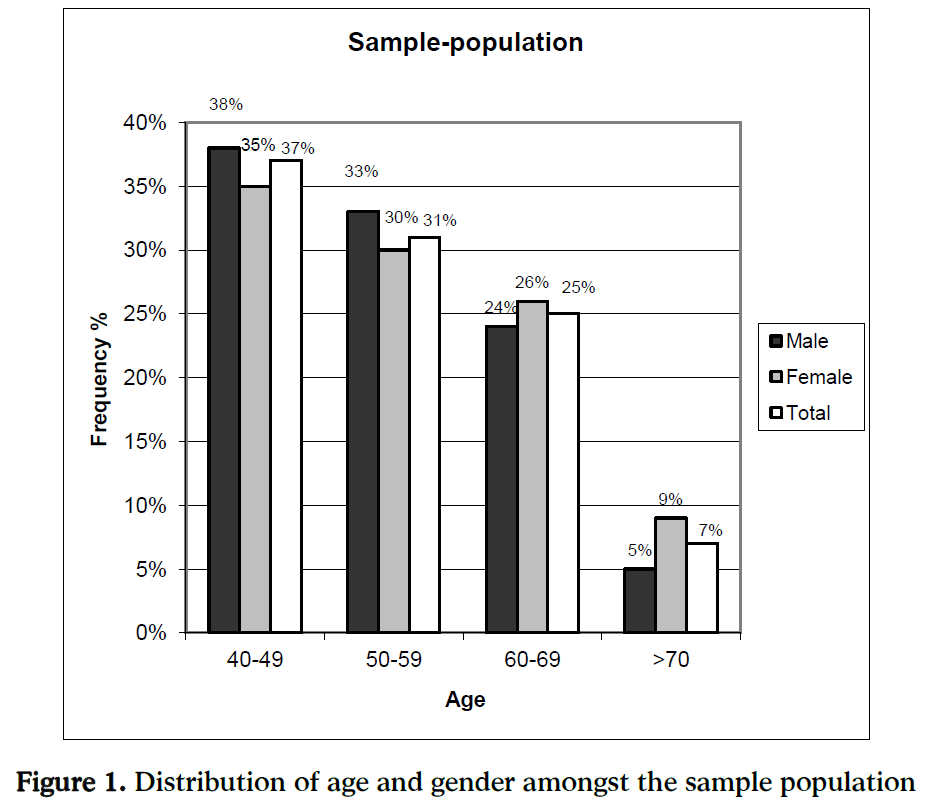
Among the randomly selected 1500 subjects, all are residents at the north suburbs of Athens-Greece during the screening period. The gender ratios (men to women) were 633/867 (42% men and 58% women) for participants. This is seen in Figure 1. The mean age of the 1500 participants was 55.14 years, (standard deviation = 10.42).
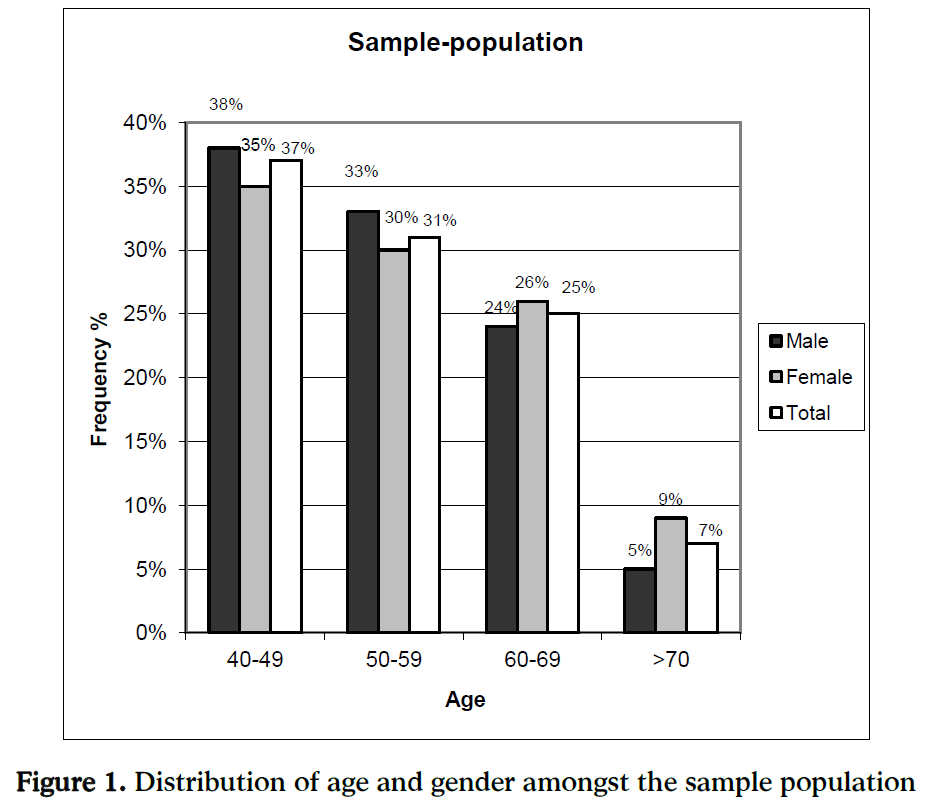
Figure 1: Distribution of age and gender amongst the sample population
The age distribution amongst the sample-population was 40-49 years 37%, 50-59 years 31%, 60-69 years 25%, >70 years 7% (Figure 1). The mean age of the 633 men participants was 54.32 years, (standard deviation = 10.11). The age distribution amongst men of the sample-population was 40-49 years 38%, 50-59 years 33%, 60-69 years 24%, >70 years 5% (Figure 1). The mean age of the 867 women participants was 55.74 years, (standard deviation = 10.61). The age distribution amongst the women of the sample-population was 40-49 years 37%, 50-59 years 31%, 60-69 years 25%, >70 years 7% (Figure 1).
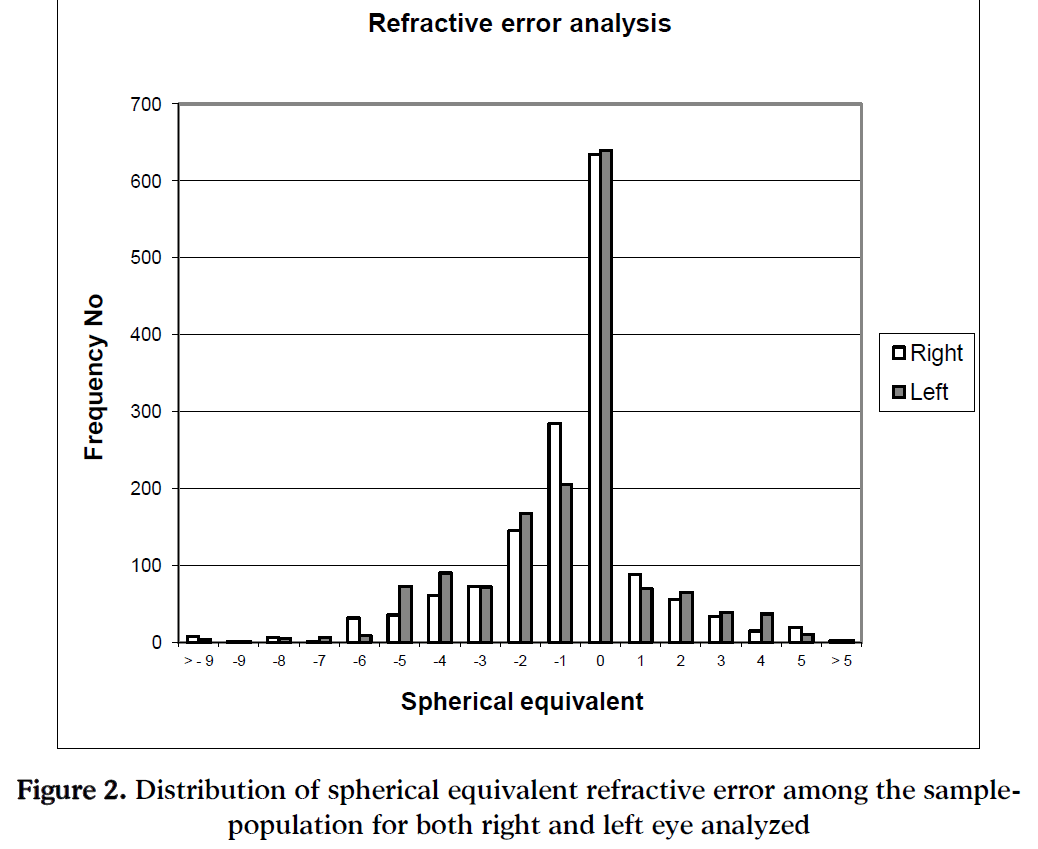
Taking in to account the results for the entire sample-population, the mean refractive error (Spherical Equivalent) in the right and left eyes averaged – 0.6907 D (95% CI, - 0.7888 to – 0.5926 D, standard deviation SD = 1.9369) and - 0.7458 D (95% CI, - 0.8464 to - 0.6453 D, standard deviation SD = 1.9855), respectively.
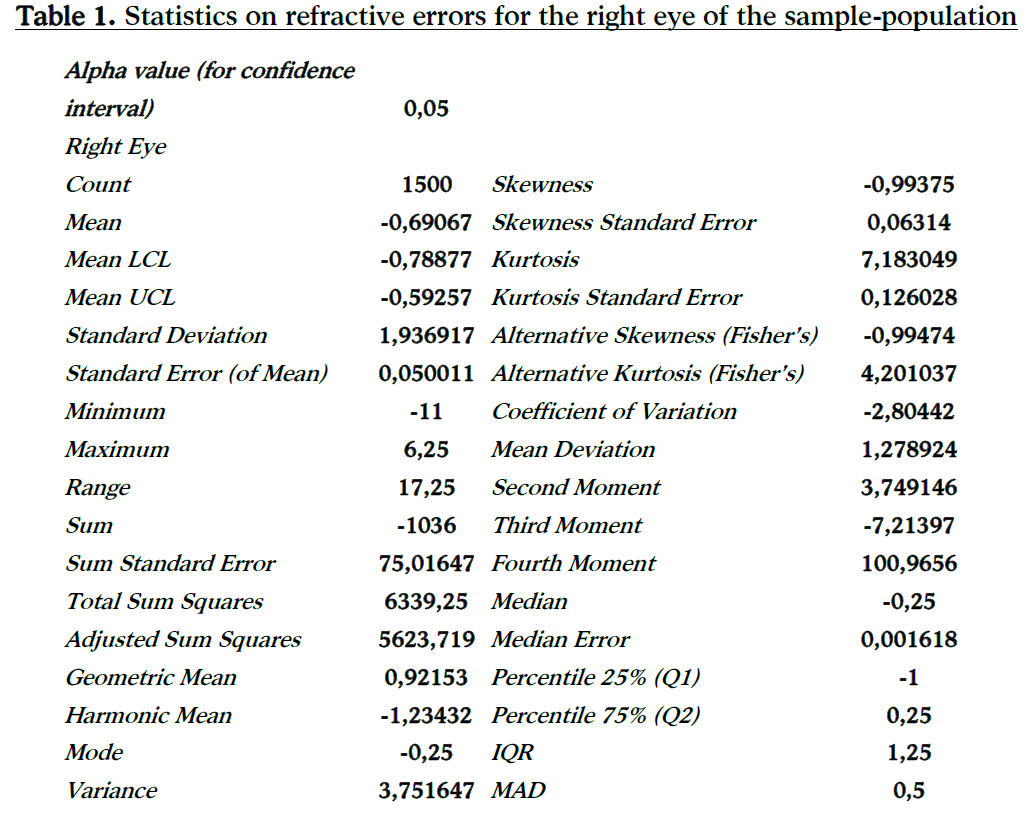
The distribution curve of spherical refractive error was normally distributed (Kolmogorov-Smirnov test showed no evidence against normality) but was slightly skewed to the myopic end (Figure 2). Table 1 shows the statistical analysis for the right eyes of the participants. Because the spherical equivalent was highly correlated between the right and left eyes (Pearson R = 0.9881, P < 0.001, only the results from the right eyes are taking into account and presented to the rest of the statistical analysis.
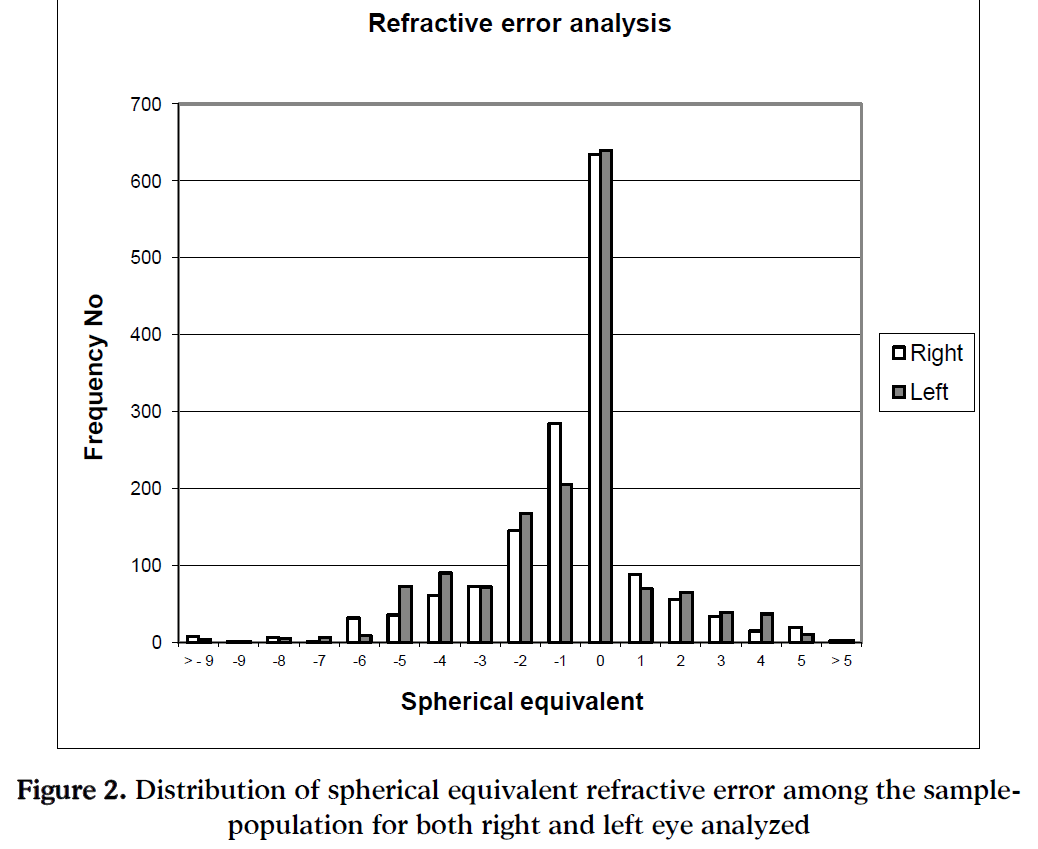
Figure 2: Distribution of spherical equivalent refractive error among the sample-population for both right and left eye analyzed
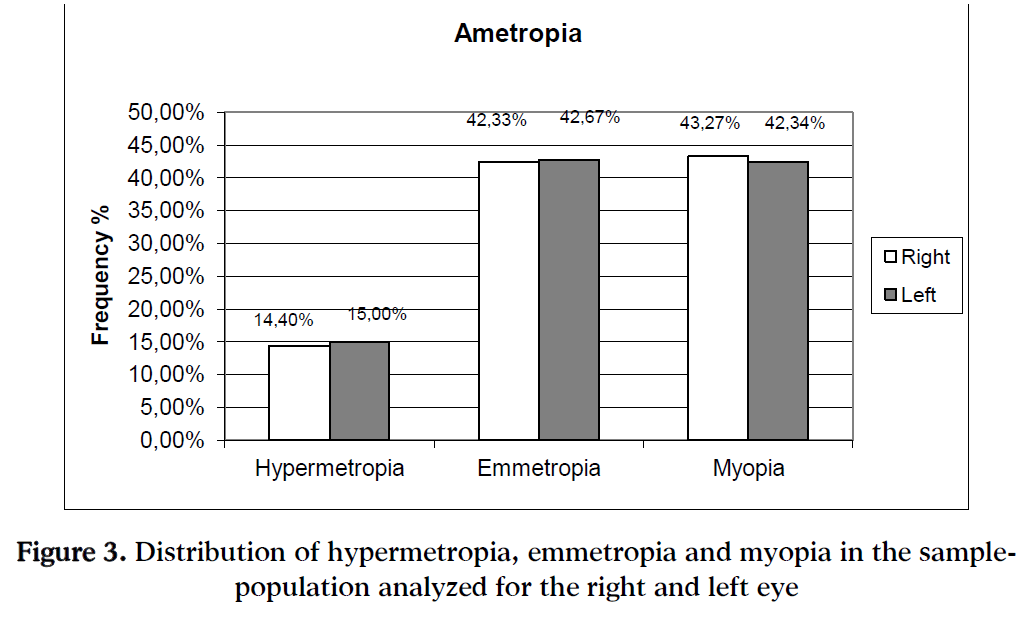
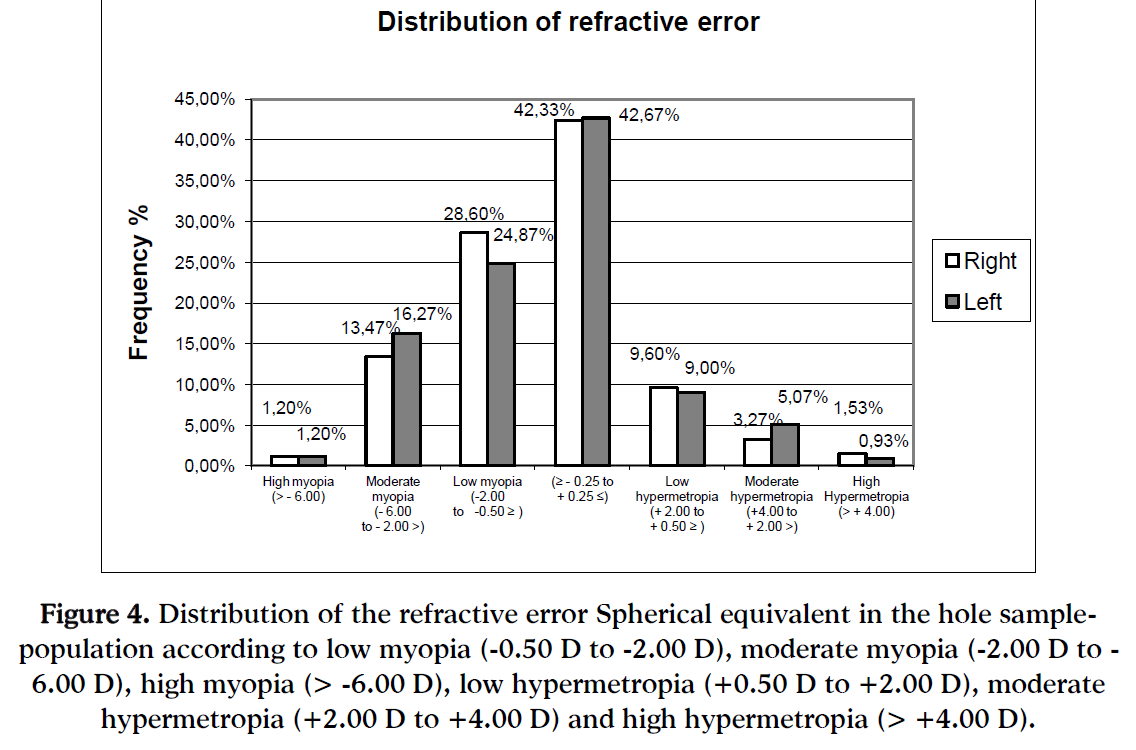
In the entire study population prevalence rates were determined for myopia 43.27%, (95% CI, 41.44 to 45.30%), hypermetropia 14.40%, (95% CI, 12.57 to 16.43%), and emmetropia 42.33% (95% CI, 40.50 to 44.36%), (Figure 3). Myopia was categorized as low myopia (-0.50 D to -3.00 D) with 28.60% prevalence, as moderate myopia (-3.00 D to -6.00 D) with 13.47% prevalence and high myopia (> -6.00 D) with 1.20% prevalence. Hypermetropia categorized as low hypermetropia (+0.50 D to +2.00 D) with 9.60% prevalence, as moderate hypermetropia (+2.00 D to +4.00 D) with 3.27% prevalence and high hypermetropia (> +4.00 D) with 1.53% (Figure 4).
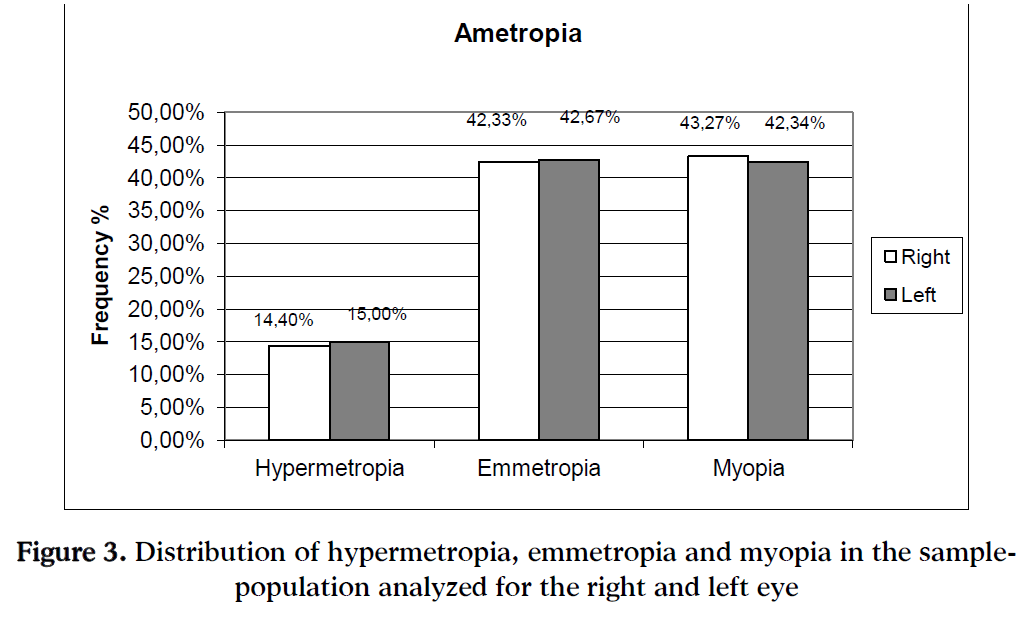
Figure 3: Distribution of hypermetropia, emmetropia and myopia in the sample-population analyzed for the right and left eye
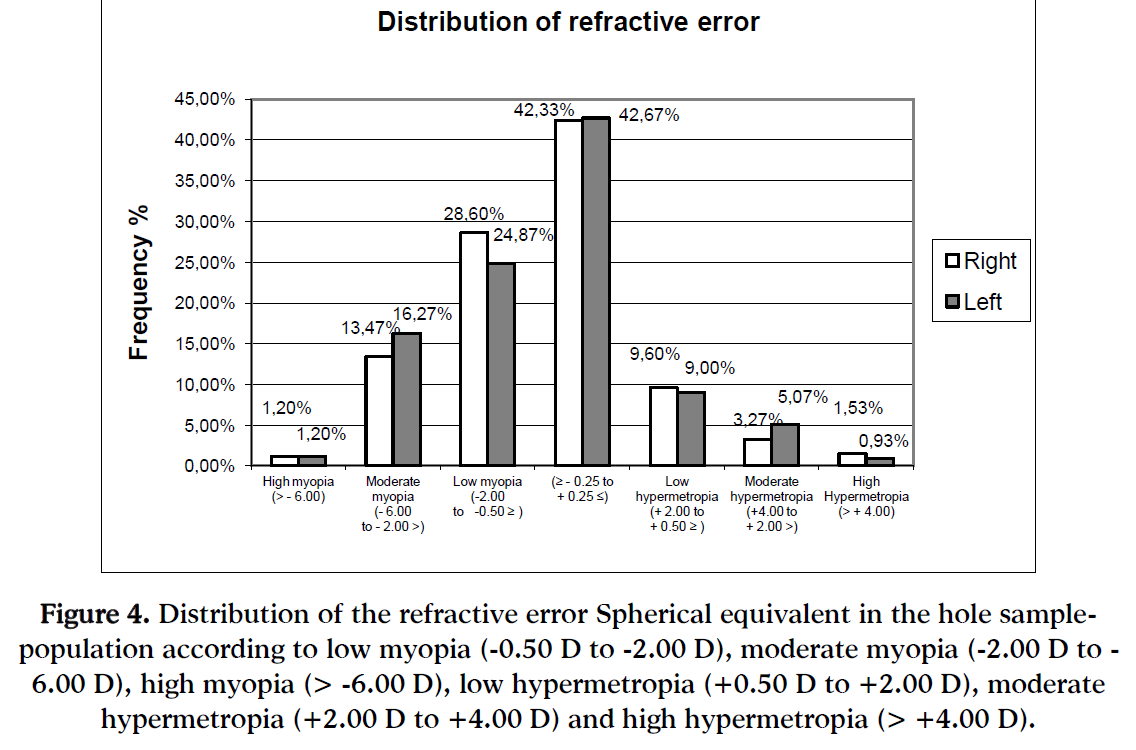
Figure 4: Distribution of the refractive error Spherical equivalent in the hole sample-population according to low myopia (-0.50 D to -2.00 D), moderate myopia (-2.00 D to -6.00 D), high myopia (> -6.00 D), low hypermetropia (+0.50 D to +2.00 D), moderate hypermetropia (+2.00 D to +4.00 D) and high hypermetropia (> +4.00 D).
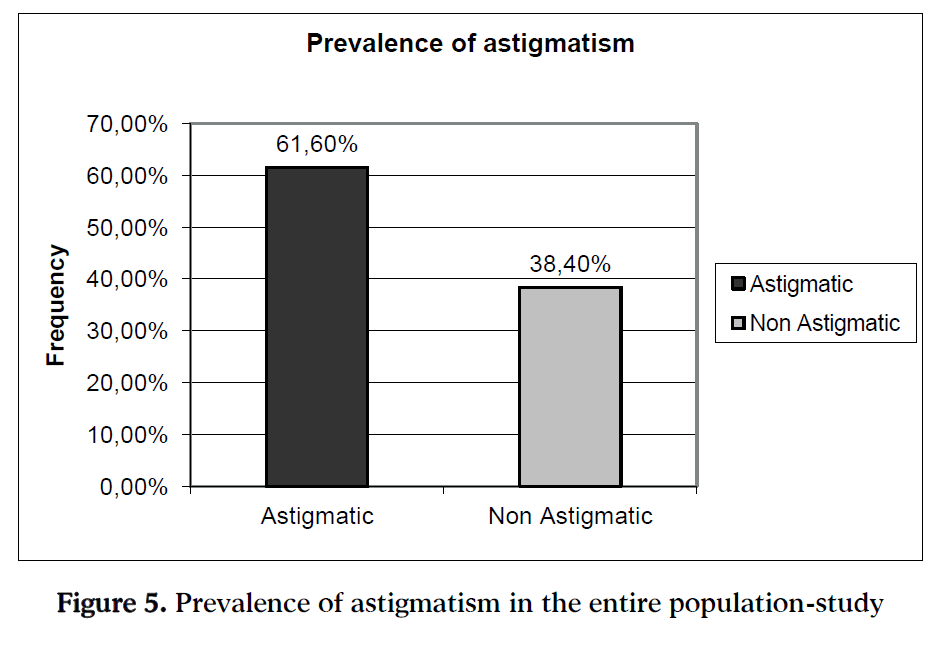
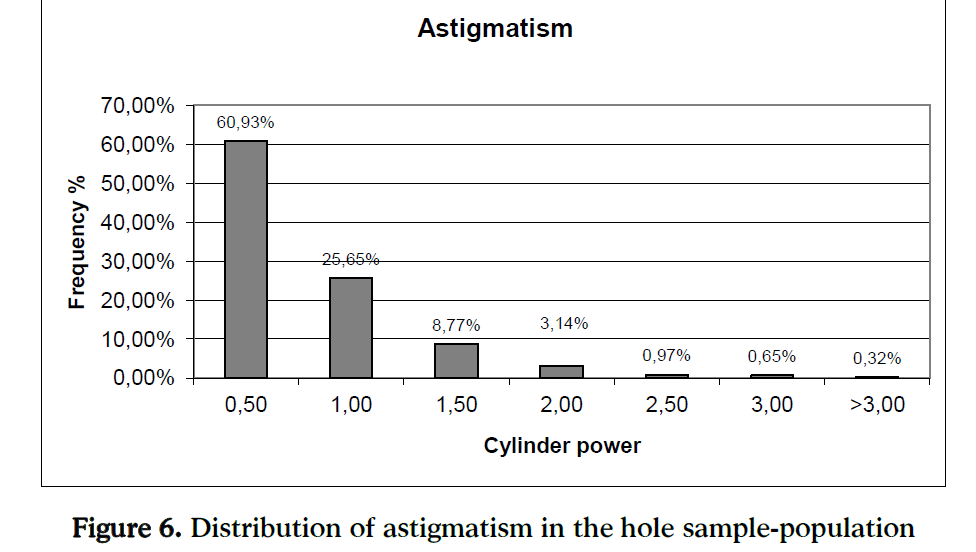
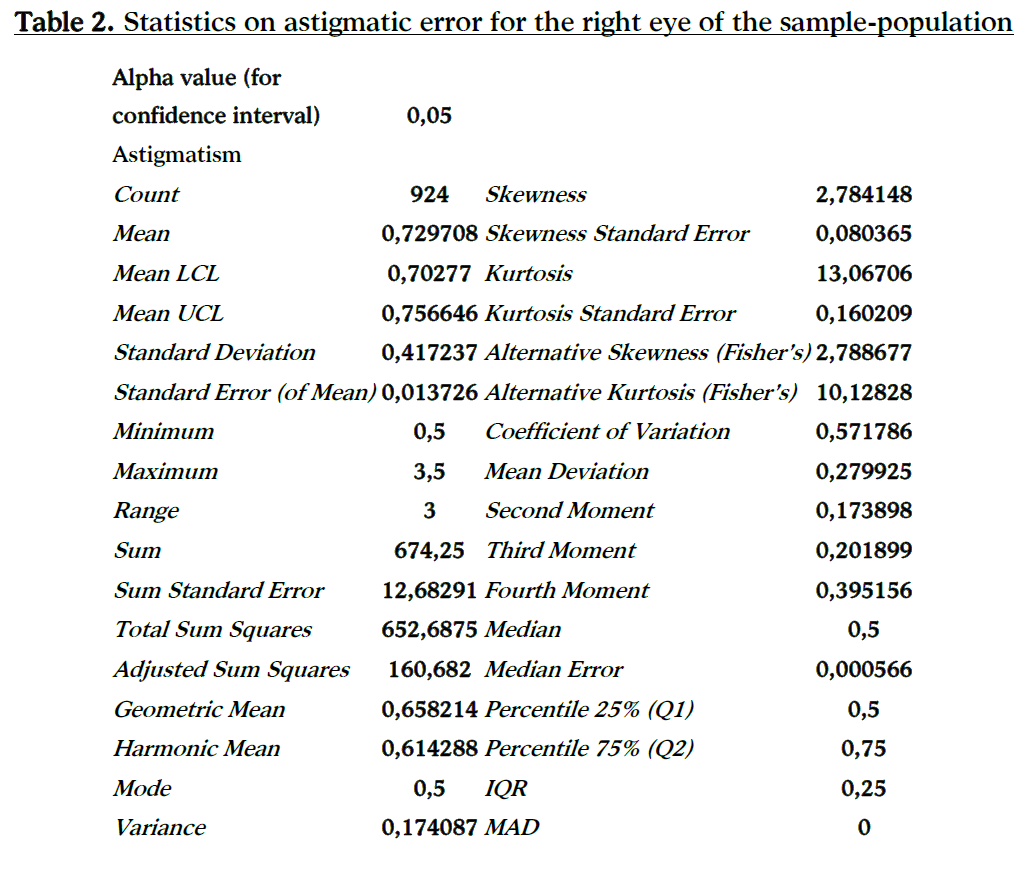
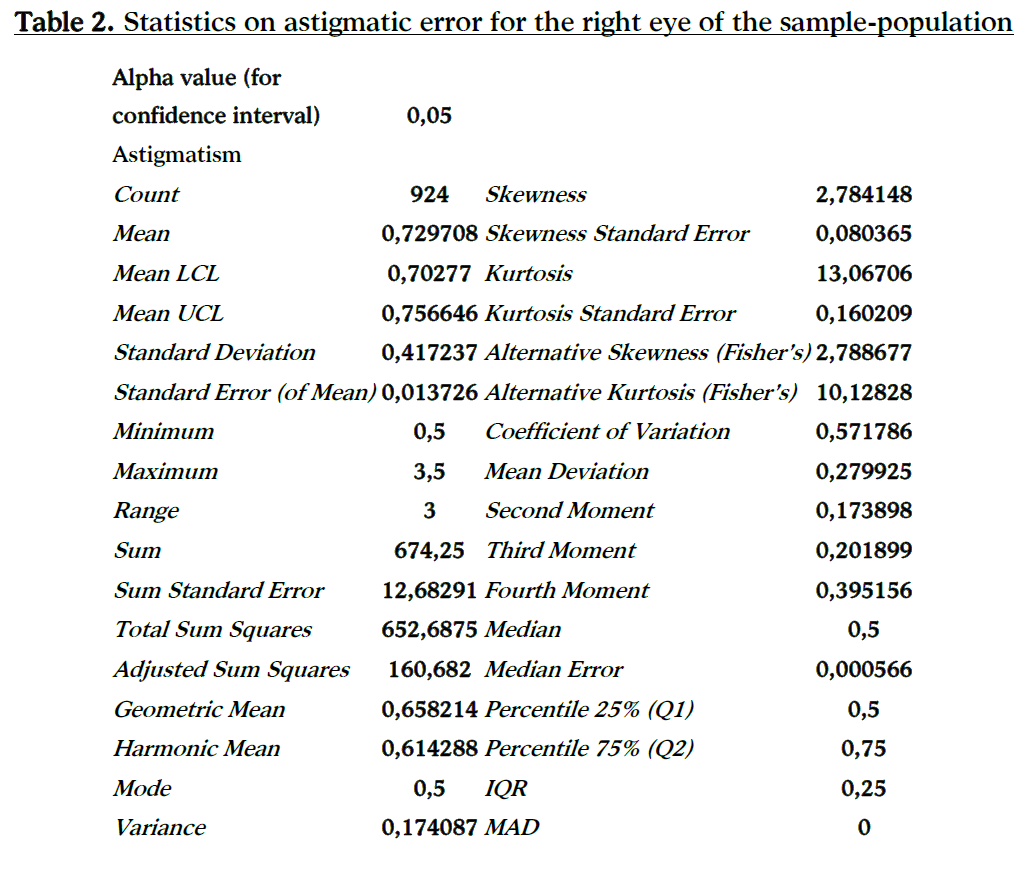
In the entire study population prevalence rates of astigmatism were determined in 61.60% (95% CI, 62.04 to 61.99%) of the population (Figure 5) the mean astigmatic error in the right eye averaged 0.7297 D (95% CI, 0.7027 to 0.7566 D, standard deviation SD = 0.4172). Table 2 shows the statistical analysis for the right eyes of the participants for astigmatic error. The distribution curve of astigmatic refractive error is presented in Figure 6.
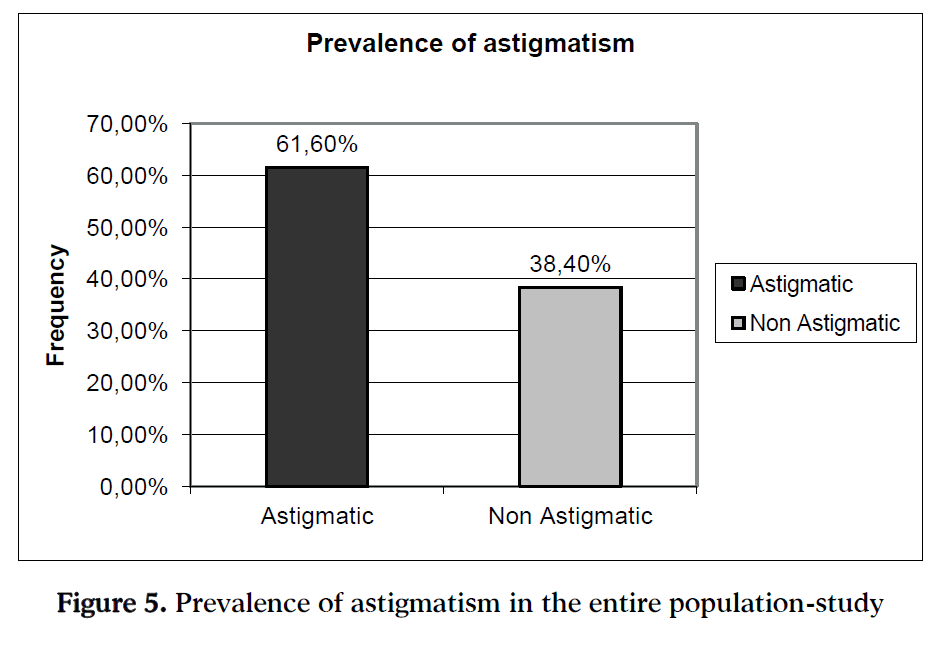
Figure 5: Prevalence of astigmatism in the entire population-study
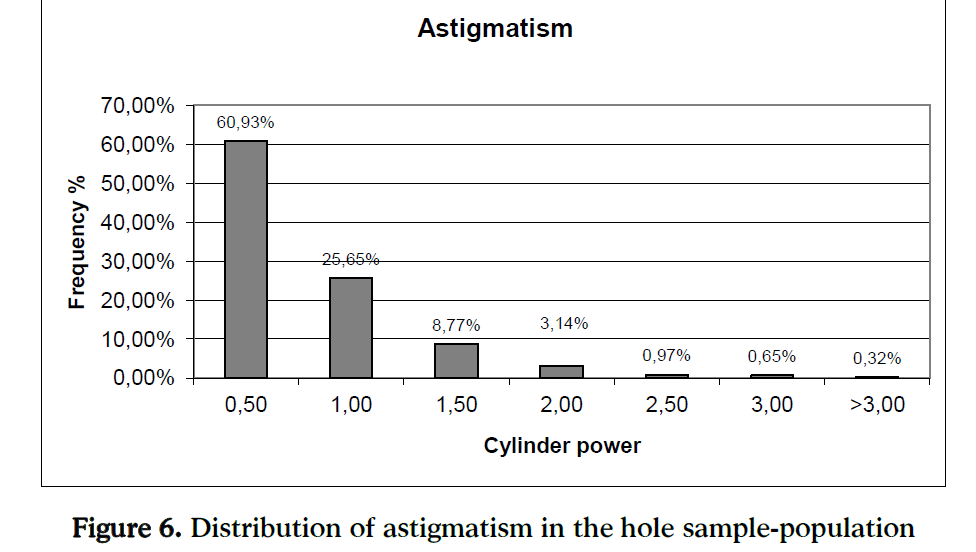
Figure 6: Distribution of astigmatism in the hole sample-population
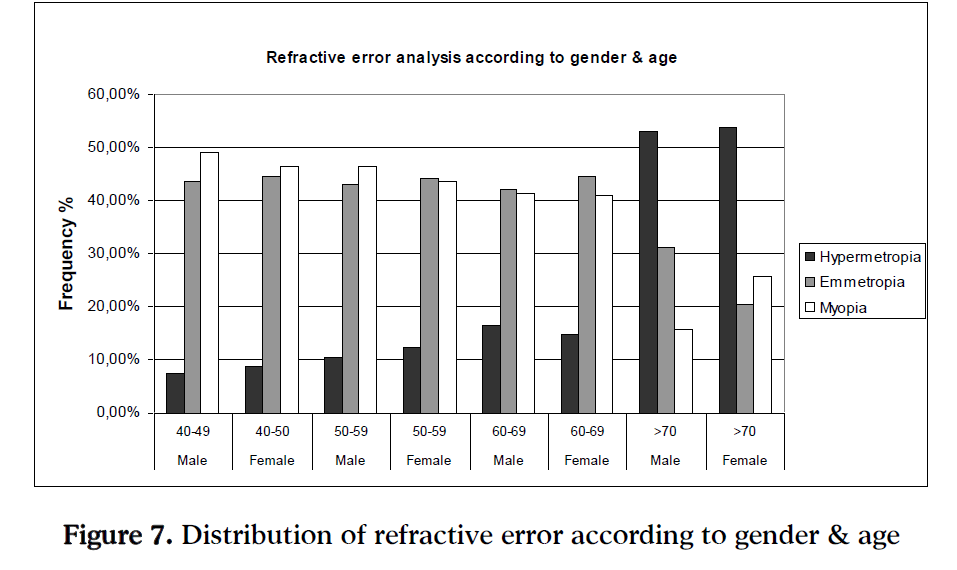
Regarding to gender (men/women) and age, the prevalence rates are presented in Figure 7.
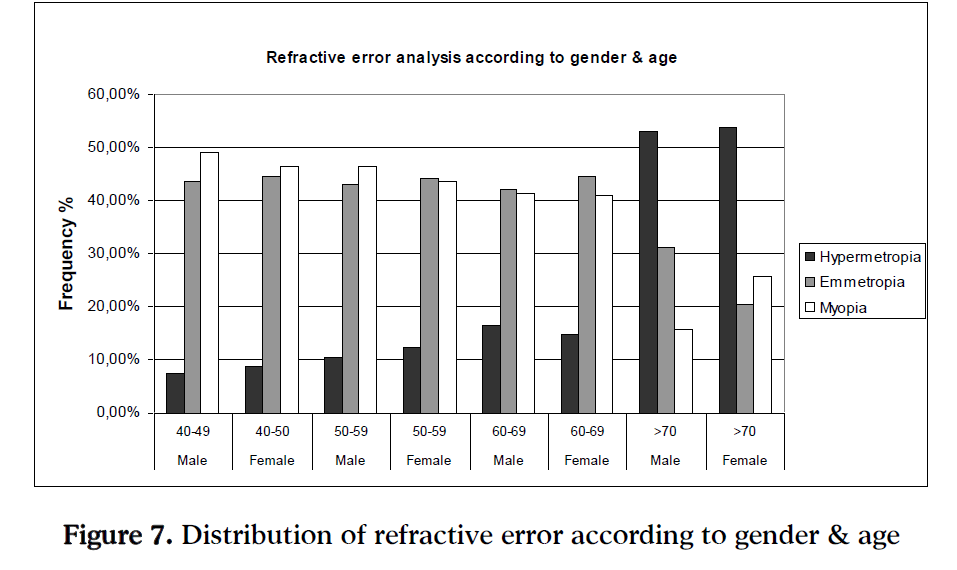
Figure 7: Distribution of refractive error according to gender & age
It is understood that refractive errors prevalence differs as age increases where participants become more hyperopic especially after 70 years old. From the graph it is understood that the results between the two genders are more about the same regardless age.
Discussion
This study provides the first population-based data on the prevalence and distribution of refractive errors in persons 40 years and older at the north suburbs of Athens-Greece. Also provides an opportunity to compare the prevalence of refractive errors with other ethnic populations in similarly aged elderly groups.
The mean refractive error (Spherical Equivalent) for both eyes checked averaged 0.7182 D myopic which was same as the mean astigmatic error 0.7297 D. Refractive errors affect approximately 57% of the population (40 years or older) at the north suburbs of Athens. The frequency for myopia was 43.27%, hypermetropia 14.40%, and emmetropia 42.33%, which findings are not similar to those found in other USA and Asian surveys. Only in an epidemiological study presented in 2004 the results for the Western Europe [3] population were similar to ours that is 43.70% for myopia, 11.60% for hypermetropia and 44.70% for emmetropia.
In the present study the age groups between 50 to 69 years old, for both genders, had results within the confidence limits of the entire population, while for the age group of 40 to 49 years old the participants were more myopic again for both genders (males were 2% more than women). For the elderly group of people over 70 years old the results presented a remarkable shift to the hyperopic side reducing the percentages of myopia approximately half of the result for the entire population.
The use of non-cycloplegic auto-refraction is a point in our study that someone might be against it and criticize it. Because in our study population the participants were over 40 years old, we did not expect excessive residual accommodation to become a problem and alter our results. Although that the use of auto-refraction, in previous studies have shown an overestimate refractive error, a previous validation study showed that the auto-refractor measured an average refractive error of 0.28 D more “plus” compared with subjective refraction. [23]
It should be noted that this study probably does not show the prevalence of refractive errors in the entire country. The sample of participants is not representative for the population of Greece due to the fact that they belong to the upper class of the country and this study did not link refractive error with other factors such as environmental, occupational (nearwork-related), education level, living standards (income) and general health.
Conclusions
The results indicate that refractive errors affect approximately more than half of the population (40 years or older) at the north suburbs of Athens. Myopia prevailed in 43.27%, with the majority being low (≤ - 2.00), while hypermetropia prevailed in 14.40%, also with the majority being low (≤ + 2.00) of the entire sample population. Refractive errors prevalence differs with age, where hypermetropia prevails especially after 70 years old. Also the results showed that there is no significant difference between the two genders. These data on the prevalence of refractive errors can be useful for the planning of refractive eye-care services.
5303
References
- Sperduto RD., Seigel D., Roberts J., Rowland M. Prevalence of myopia in the United States. Archives of Ophthalmology. 1983;101(3):405–407.
- Wensor M., McCarthy C.A., Taylor J.R. Prevalence and risk factors of myopia in Victoria, Australia. Archives of Ophthalmology 1999;117(5):658–663.
- Eye Diseases Prevalence Research Group. “The prevalence of refractive errors amongst adults in the United States, Western Europe, and Australia” Archives of Ophthalmology 2004;122(4):495–505.
- Katz J., Tielsch J.M., Sommer A. Prevalence and risk factors for refractive errors in an adult inner city population. Investigative Ophthalmology & Vision Science 1997;38(2):334–340.
- Hyams SW., Pokotilo E., Shkurko G. Prevalence of refractive errors in adults over 40: a survey of 8102 eyes. Br. J. Ophthalmol. 1977;61:428 –432.
- Wu S.Y., Nemesure B., Leske M.C. Refractive errors in a black adult population: the Barbados Eye Study. Investigative Ophthalmology & Vision Science 1999;40:2179–2184.
- Wang Q., Klein B.E., Klein R., Moss S.E. Refractive status in the Beaver Dam Eye Study. Investigative Ophthalmology & Vision Science 1994;.35: 4344–4347.
- Evans B.J., Rowlands G. Correctable visual impairment in older people: a major unmet need” Ophthalmic & Physiological Optics 2004;24(3):161-180.
- Vitale S., Ellwein L., Cotch M.F., Ferris III F.L., Sperduto R. Prevalence of Refractive Error in the United States, 1999-2004. Archives of Ophthalmology 2008;126(8): 1111-1119.
- Attebo K., Q Ivers R., Mitchell P. Refractive errors in an older population: the Blue Mountains Eye Study”. Ophthalmology. 1999;106(3):1066-1072.
- Angle J., Wissmann D.A. The epidemiology of myopia. Am. J. Epidemiol. 1980; 111:220–228.
- Angle J., Wissmann D.A. Age, reading and myopia. Am. J. Optom. Physiol. Opt. 1978; 55:302– 308.
- Slataper FJ. Age norms of refraction and vision. Archives of Ophthalmology 1950;43(3):466–481.
- Saw S.M., Gazzard G., Koh D., Farook M., Widjaja D., Lee J. et al. Prevalence rates of refractive errors in Sumatra, Indonesia. Investigative Ophthalmology & Vision Science 2002;45: 3174–3180.
- Xu L., Li J., Cui T., Hu A., Fan G., Zhang R. et al. Refractive error in urban and rural adult Chinese in Beijing. Ophthalmology 2005; 112:1676–1683.
- Hashemi H., Fotouhi A., Mohammad K. The age-and gender specific prevalences of refractive errors in Tehran: the Tehran Eye Study. Ophthalmic Epidemioly 2004;11(3):213–225.
- Dandona R., Dandona L., Marmamula-Srinivas M., Giridhar P., McCarty C.A., N- Rao G. Population-based assessment of refractive error in India: the Andhra Pradesh Eye Disease Study. Clin. Experiment Ophthalmol. 2002; 30:(2): 84 –93.
- Bourne R.R., Dineen B.P., Ali S.M., Noorul Hug D.M., Johnson G.J. Prevalence of refractive error in Bangladeshi adults. Results of the National Blindness and Low Vision Survey of Bangladesh.Ophthalmology 2004; 111(6):1150–1160.
- Cheng C.Y., Hsu W.M., Liu J.H., Tsai S.Y., Chou P. Refractive errors in an elderly Chinese population in Taiwan: the Shiphai Eye Study. Investigative Ophthalmology & Vision Science 2003;44:4630–4638.
- Wong T.Y., Foster P.J., Hee J., Pin Ng T., Tielsch J.M., Chew S.J., et.al. Prevalence and risk factors for refractive errors in adult Chinese in Singapore. Investigative Ophthalmology & Vision Science 2000 ;41:2486 –2494.
- Lin LL., Chen CJ., Hung PT., Ko LS. Nation-wide survey of myopia among school children in Taiwan, 1986. Acta Ophthalmol. Suppl. 1988;185:29 –33.
- Lin L.L., Shih Y.F., Tsai C.B., Chen C.J., Lee L.A., Hung, P.T., Hou, P.K. Epidemiologic study of ocular refraction among schoolchildren in Taiwan in 1995. Optom. Vis. Sci. 1999;76(5):275– 281.
- Wesemann W., Dick B. Accuracy and accommodation capability of a handheld autorefractor. J. Cataract Refract. Surg. 2000;.26:(1):62–70.