Jamuneswary Selvarajoo* and Sakinah Ghauth
Faculty of Medicine, Department of Otorhinolaryngology-Head and Neck Surgery, University Malaya, Malaysia
*Corresponding Author:
Jamuneswary Selvarajoo
Faculty of Medicine
Department of Otorhinolaryngology-Head and Neck Surgery
University Malaya, Malaysia
Tel: +6037947 6686
E-mail: jamunes_my@yahoo.com
Received Date: January 14, 2019; Accepted Date: January 31, 2019; Published Date: February 02, 2019
Citation: Selvarajoo J, Ghauth S (2019) Primary Ethmoidal Sinus Extra-nodal Lymphoma: A Rare Case. Ann Clin Lab Res Vol.7 No.1: 283. doi: 10.21767/2386-5180.100283
Keywords
Lymphoma; Tumour of nasal cavity
Introduction
Malignant lymphoma of the ethmoid sinus is rare. We are repeating a case of a 55-years-old gentleman. A case of an extensive primary extranodal DLBCL of the left ethmoidal sinus is presented here. We trust that our report will build familiarity with this infection for doctors to get prior conclusion, all the more opportune medications, and, above all, enhanced patient's results.
Case Report
We are repeating a case of a 55-years-old gentleman who presented to our centre with huge tumour involving the left eye and left cheek with prior history of Functional Endoscopic Sinus Surgery (FESS) for sinusitis that was done in a different centre prior to his presentation to ours. Initial complaints were left sided nose block, foul smelling discharge and occasional sinusitis. Initial Computer Tomography (CT) of para nasal sinuses showed thickened mucosa over the left ethmoidal sinus with no other mass seen for which he underwent the FESS as his symptoms did not improve with oral antibiotics.
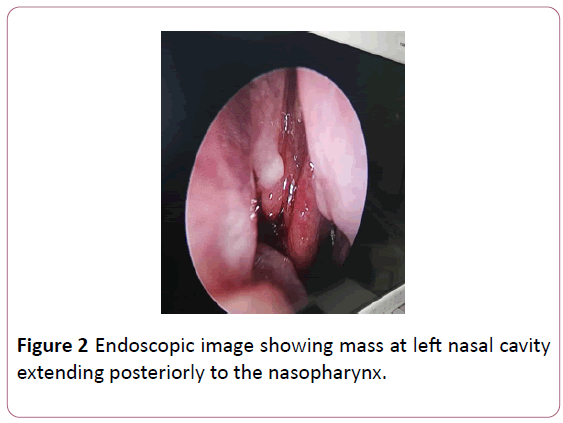
There were no tissue biopsy from first surgery. However, 2 days post-surgery, he developed left eye proptosis and swelling over the check. The swelling rapidly increased in size that when he presented to our centre a week later, the swelling has extended to the mandibular edges and left eye causing left eye proptosis and deterioration of vision. Nasal endoscopy revealed left sided nasal cavity mass medial to middle turbinate extending to the Fossa of Rossenmuller (FOR). Mass also appears to be extending to right nasal cavity. Oral cavity examination shows fullness at left soft and hard palate extending toward the tonsillar fossa. Patient also noted to have enlarged liver with multiple subcutaneous lesions over the abdomens.
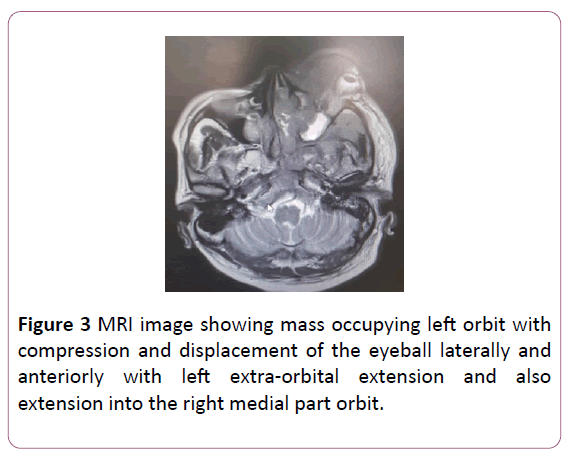
He had massive pleural effusion who which urgent pleura drainage was done. MRI showed an irregular enhancing lesion measuring 113 × 71 × 45 mm over left mandible up the front temporal region extending into the left para pharyngeal space causing narrowing of the oropharynx and there is also an irregular enhancing lesion measuring 71 × 70 × 59 mm seen in nasal space (more on the left) extending into the frontal lobe, through cribriform plate, sphenoid bone, sphenoid sinus and clivus with left extra orbital extension displacing the left medial rectus. While waiting for the biopsy results, there was increase in tumour size despiting starting patient on IV Steroids. HPE revealed diffuse large B Cell Lymphoma, non GCB type with the malignant cells are strongly diffusely positive for CD220, co-express MUM1 and BCL 6. The patient was subsequently evaluated by haematology for systemic chemotherapy with R-CHOP (Rituximab, Cyclophosphamide, Doxorubicin, Vincristine, Prednisone). He is still undergoing chemotherapy, but his tumour has shrunken in size with resolution of the pleural effusion (Figures 1-3).

Figure 1: Showing huge tumour involving the left eye, unable to visualize normal eyeball with left eye.
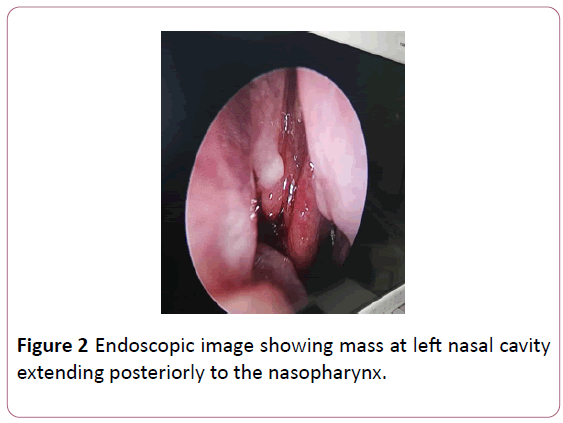
Figure 2: Endoscopic image showing mass at left nasal cavity extending posteriorly to the nasopharynx.
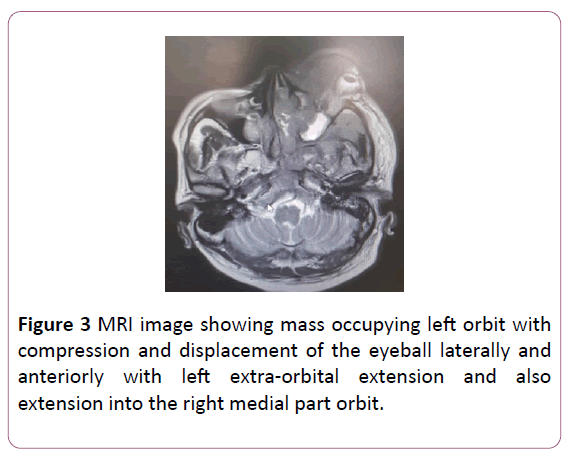
Figure 3: MRI image showing mass occupying left orbit with compression and displacement of the eyeball laterally and anteriorly with left extra-orbital extension and also extension into the right medial part orbit.
Discussion
Diffuse large B-cell lymphoma is mostly diagnosed in the sixth decade of life. DLBCL claims male pre-dominance, and incidence varies both with ethnicity and increased age [1]. The aetiological factors have not yet been fully untangled, but immunodeficiency, infections such as HIV and EBV, exposure to noxious chemical agents, autoimmune disease and as well as hereditary factors has been linked with this disease [2]. The most common clinical aspects of DLBCL of the ethmoidal sinus are facial asymmetry, eyelid oedema and tumefaction involving oral tissues that may or may not exhibit ulceration with nasal obstruction; nasal bleeding, pain and paraesthesia are also frequently reported [3]. In accordance, our patient initial presentation was nasal block, epistaxis and in addition to non-specific signs and symptoms such as rhinorrhoea, tearing in the left eye. Our patient received an erroneous prescription of antibiotics prior to our care, indicating that this malignant neoplasm was first misdiagnosed as an infectious disease, probably as ethmoidal sinusitis. FESS was also performed to ease patient symptoms. Yen et al. analysed 32 patients diagnosed with sinonasal lymphoma and reported that when they were initially referred to hospital, the first impression of 20 patients (62.5%) was malignant neoplasm and that of the other 12 patients (37.5%) was rhinosinusitis [4].
Paranasal sinuses especially the ethmoid sinus as primary site for DLBCL is rare. Clinically, the most common location of extra nodal DLBCL in the head and neck is the maxillary sinus [5]. Extra nodal DLBCL usually comprises a mass of soft tissue that causes significant bone destruction and involves oral tissues [5]. Nevertheless, non-specific signs and symptoms such as rhinorrhoea, bloody discharge, facial tumefaction or nasal obstruction may be present, which may also be associated with benign inflammatory conditions and upper respiratory infections, delaying the diagnosis [2,3].
The diagnosis of paranasal sinus lymphoma may remain elusive for months leading to delays in treatment. The experience in our case is that even intraoperative an infection was presumed, hence there were no tissue biopsy. It was only certain that it is a malignant tumour upon patient’s deterioration.
Therefore, an attempt at biopsy of mucosa of sinuses for histologic examination should be considered during the sinus surgery. Though we may assume a primary paranasal location would not alter patient’s prognosis, but however the variable presentation and late diagnosis are the leading detriments affecting patient survival.
We hope that our report will help to increase awareness of this disease for physicians to obtain earlier diagnosis, more timely treatments, and, most importantly, improved patient’s outcomes.
Conclusion
Paranasal sinus DLBCL is rare but can occur in the ethmoidal sinus. Most of the symptoms are tumour non-specific. Patient can present with non-specific nasal symptoms and may be easily overlooked at surgery unless histologic specimens are submitted and reviewed in detail. A high clinical suspicion is necessary for early diagnosis and treatment. Prior to surgery, endoscopic biopsy should be considered in suspected cases.
Conflict of Interest
The authors declare no conflict of interests.
24140
References
- Yasumoto M, Taura S, Shibuya H, Honda M (2000) Primary malignant lymphoma of the maxillary sinus: CT and MRI. Neuroradiology 42(4): 285-289.
- Cleary KR, Batsakis JG (1994) Sinonasal lymphomas. Ann Otol Rhinol Laryngol 103(11): 911-914.
- Sands NB, Tewfik MA, Hwang SY, Desrosiers M (2008) Extranodal T-cell lymphoma of the sinonasal tract presenting as severe rhinitis: Case series. J Otolaryngol Head Neck Surg 37(4): 528-533.
- Yen TT, Wang RC, Jiang RS, Chen SC, Wu SH, et al. (2012) The diagnosis of sinonasal lymphoma: A challenge for rhinologists. Eur Arch Otorhinolaryngol 269(5): 1463-1469.
- O’Connor RM, Vasey M, Smith JC (2010) Diffuse large B-cell lymphoma of the maxillary sinus. Ear Nose Throat J 89(6): 8-10.