Xiang Wang*, Qixing Xiong and Qi Qin
Department of General Surgery, The Children's Hospital, Zhejiang University School of Medicine, The Children's Hospital, Zhejiang University School of Medicine, Hangzhou, Zhejiang, China
Corresponding Author:
Xiang Wang
Department of General Surgery, The Children's Hospital
Zhejiang University School of Medicine, Hangzhou, Zhejiang, China
Tel: 8613819172702
E-mail: wangxiang81@icloud.com
Received date: March 24, 2017; Accepted date: March 28, 2017; Published date: March 31, 2017
Citation: Wang X. Primary Laparoscopic Deloyers Procedure for Long-Segment Hirschsprung’s Disease. Arch Med. 2017, 9:2. doi: 10.21767/1989-5216.1000206
Copyright: © 2017 Wang X, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Keywords
Children; Deloyers procedure; Hirschsprung's disease; Laparoscopy; Long-segment
Introduction
The rectosigmoid Hirschsprung's disease (HD) has been widely treated with laparoscopic surgery in recent years [1-3]. However, there have been few reports of treatment of long-segment HD when aganglionosis extends to the descending colon, splenic flexure or transverse colon [4-6]. Our hospital treated 13 children with long-segment HD with a single-stage surgery using laparoscopy from June 2008 to October 2016, and a relatively satisfactory effect was achieved.
Subjects and Methods
Clinical data
A total of 13 children (nine male and four female) were included in the present study, with ages ranging from two months to four years (average age, two years and five months) and weighing from 4.3 kg to 13 kg (average weight, 8.2 kg).
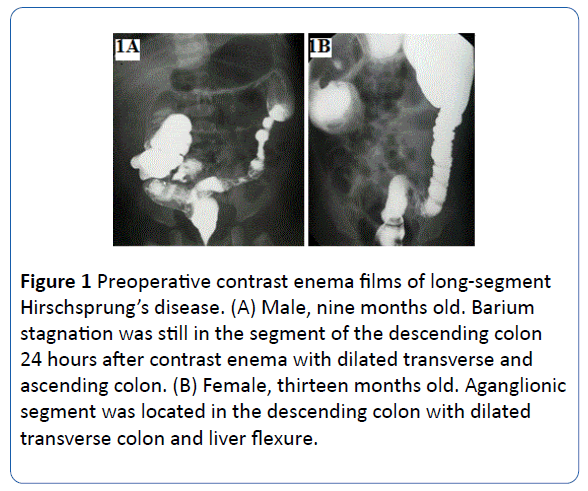
The preoperative diagnoses were based on medical histories, physical examination, abdominal plain films, barium enema Xray films, and anorectal manometric results. This study was approved by the Children’s Hospital Medical Review Board. The preoperative contrast enema results showed that the aganglionic segment was located in the descending colons of nine children (Figures 1A and 1B), the splenic flexures of two children, and the transverse colons of two children.
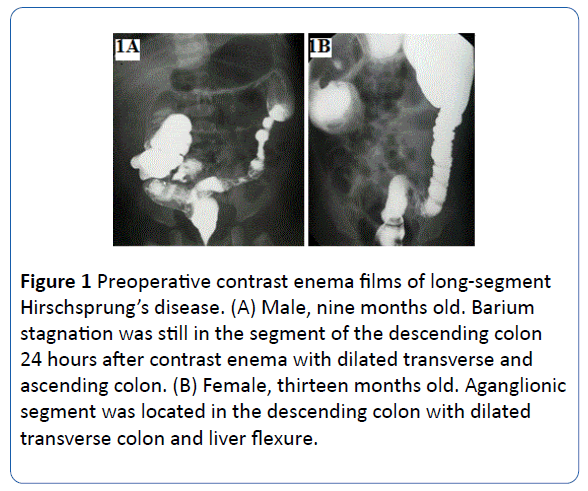
Figure 1: Preoperative contrast enema films of long-segment Hirschsprung’s disease. (A) Male, nine months old. Barium stagnation was still in the segment of the descending colon 24 hours after contrast enema with dilated transverse and ascending colon. (B) Female, thirteen months old. Aganglionic segment was located in the descending colon with dilated transverse colon and liver flexure.
The preoperative preparations included an appropriate rectal wash for 7-10 days and oral antibiotics for two to three days. The intestine segments resected included both the spastic segment and the dilated segment.
Operative methods
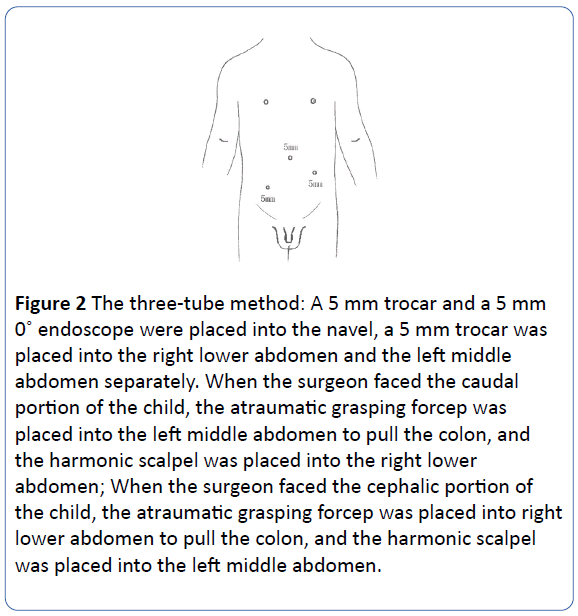
The children fasted for six to eight hours before the operation. Each child received tracheal intubation and intravenous balanced anesthesia and was catheterized with a Foley indwelling catheter. Both lower limbs of each child were bandaged with aseptic towels after disinfection. Each child was first placed in a supine position, and then, a Veress needle was inserted into the abdomen from the right margin of the navel; afterward, CO2 (pressure, 10-12 mmHg) was insufflated into the abdomen via the Veress needle to establish a pneumoperitoneum. The three-tube method (one camera port and two working ports) was used in all 13 children, i.e., a 5 mm trocar and a 5 mm endoscope were placed into the navel, a 5 mm trocar was placed into the right lower abdomen, and another 5 mm trocar was placed into the left middle abdomen (Figure 2). An atraumatic grasping forceps was placed into the left middle abdomen to pull the colon. A harmonic scalpel was placed into the right lower abdomen to free the mesenterium and the greater omentum. Each of the 13 children underwent Swenson’s operation; the ascending colon of each child was rotated according to the Deloyers procedure. First, the abdomen was fully examined using a laparoscope to determine the lesion site and the excision extension. The surgeon then faced the caudal portion of each child. An atraumatic grasping forceps was placed into the trocar in the left middle abdomen to pull the colon, and an harmonic scalpel was placed into the trocar in the right lower abdomen; then, the planned resection level was marked using an harmonic scalpel to gently perform a coagulotomy at the surface of the colon, and some seromuscular tissue was removed for a rapid biopsy. Afterwards, a coagulotomy was performed on the superior rectal artery, sigmoid colonic artery, and left colonic artery closely along the rectal wall and the sigmoid colonic wall using a harmonic scalpel. The descending branch of the arteria colica dextra was preserved. Subsequently, the surgeon faced cephalic portion of the child. A harmonic scalpel was placed into the trocar in the left middle abdomen, and an atraumatic grasping forceps was placed into the trocar in the right lower abdomen to pull the colon; then, a coagulotomy was performed on the middle colonic artery and the ascending branch of the right colonic artery successively, and the descending branch of the right colonic artery was preserved. The splenocolic ligament and the hepatocolic ligament were then cut, the colon frame was freed, and the appendix was resected.
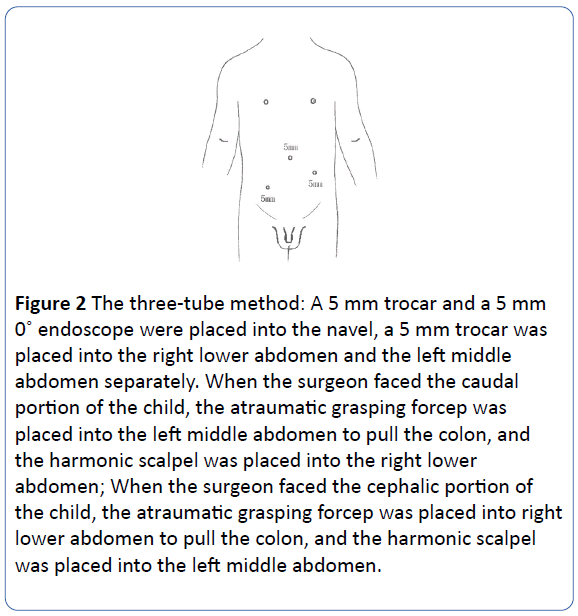
Figure 2: The three-tube method: A 5 mm trocar and a 5 mm endoscope were placed into the navel, a 5 mm trocar was placed into the right lower abdomen and the left middle abdomen separately. When the surgeon faced the caudal portion of the child, the atraumatic grasping forcep was placed into the left middle abdomen to pull the colon, and the harmonic scalpel was placed into the right lower abdomen; When the surgeon faced the cephalic portion of the child, the atraumatic grasping forcep was placed into right lower abdomen to pull the colon, and the harmonic scalpel was placed into the left middle abdomen.
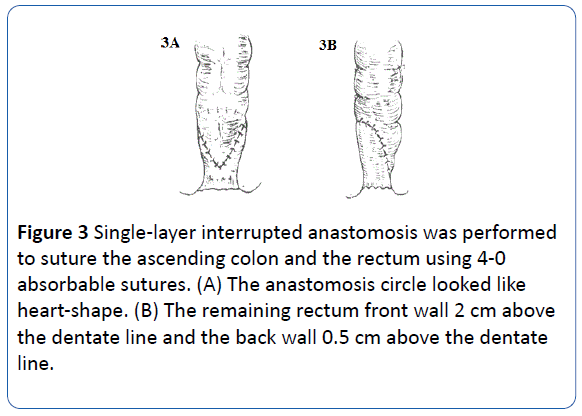
Before removing the colon, the small intestine was pushed to the left side of the abdomen. Then, the chief surgeon and the first assistant turned to the perineum of the child. The child was placed in the lithotomy position. After anal dilation, oval forceps were inserted into the anus to grasp the rectal wall. Next, the freed colon was pulled from the intrarectal intussusception until the colon reached the resection mark under laparoscopy, and the pulled ascending colon was rotated 270° counterclockwise. The intestine lesion was then resected at the mark, and a part of the front wall (2 cm above the dentate line) and a part of the back wall (0.5 cm above the dentate line) of the distal rectum were preserved (Figures 3A and 3B). After ensuring that the pulled intestine had no tension, torsion, or bleeding by laparoscopy, a single-layer interrupted anastomosis was performed to suture the ascending colon and the rectum using 4-0 absorbable sutures. An anal tube was inserted into the anus and passed through the anastomosis and fixed to perianal skin. The umbilical fascia was closed using 3-0 vicryl suture and the skin was approximated using biological glue.
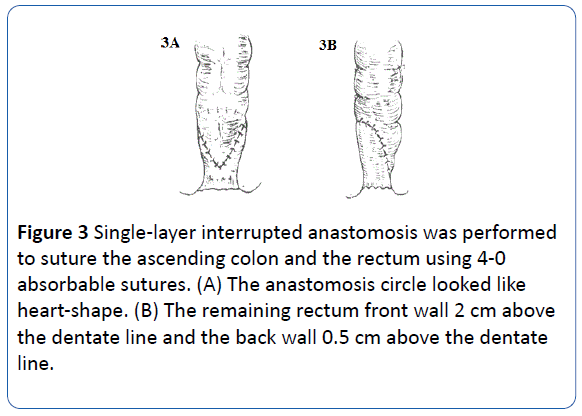
Figure 3: Single-layer interrupted anastomosis was performed to suture the ascending colon and the rectum using 4-0 absorbable sutures. (A) The anastomosis circle looked like heart-shape. (B) The remaining rectum front wall 2 cm above the dentate line and the back wall 0.5 cm above the dentate line.
Postoperative treatment
The gastric tube was removed two days after the operation. Each child was allowed to drink water and have a liquid diet. The anal tube was removed five days after the operation. Each child was administered broad-spectrum antibiotics intravenously for 72 hours and then orally for one week. Neither sedatives nor analgesics were needed. Two weeks after the operation, each child was re-examined and started receiving anal dilation treatment, which lasted for three months.
Results
All children underwent surgical laparoscopy. The lengths of the resected intestines ranged from 36 cm to 47 cm (average length, 42 cm). The surgical times ranged from 140 minutes to 220 minutes (average surgical time, 168 minutes). The largest intraoperative blood loss volume was 28 ml, and the remaining intraoperative blood loss volumes were all less than 10 ml. No transfusion was performed during any of the operations. Neither sedatives nor analgesics were used after the operation. One sixmonth- old child with moderate preoperative malnutrition experienced pyrexia, abdominal distention, and poor response five days after the surgery; a reoperation revealed that the child had an anastomotic leakage. Therefore, the child underwent an ileum colostomy. After the ileum colostomy, the child recovered well, and the stoma was closed two months later. For follow-up evaluation, each child returned to the hospital to receive monthly medical consultations beginning two weeks after the operation. The follow-up visits were conducted on all 13 children for a period ranging from 3 to 48 months. The children defecated one to eight times per day and experienced no abdominal distension, emesis, or pyrexia. Five children had soft stools within three months after the operation and gradually started having formed stools six months after the operation. Six children experienced skin erosion around the anus or had a perianal infection but showed improvement after receiving treatment. No fecal incontinence occurred in any of the children.
Discussion
Georgeson et al. [1] reported a laparoscopic-assisted radical operation for HD for the first time. Currently, laparoscopic operations are widely used for treating the sigmoid HD [7-10]. The aganglionic segment of long-segment HD can reach the proximal end of the descending colon or the transverse colon; the intestine segments that should be resected include the significantly dilated part of the colon in addition to the narrow zone and the transitional zone of the colon. Therefore, the resection range usually includes the hepatic flexure of the colon or the ascending colon. Due to the wide range and complexity of laparoscopic surgery, there have been few reports on the treatment of long-segment HD with laparoscopic surgery in recent years. In our opinion, another reason for the relative difficulty of treating long-segment HD with laparoscopic surgery is the difficulty in rotating the ascending colon during an endoscopy. In a standard Deloyers procedure, the residual ascending colon is first turned 270 counterclockwise and then pulled into the pelvic cavity to the anastomosis with the rectum. No difficulty in performing the Deloyers procedure has been encountered during past laparotomy processes. However, it is difficult to perform the Deloyers procedure under laparoscopy. Nevertheless, with the accumulation of experience, perfection of the operative techniques, and the application of harmonic scalpels, it should not be too difficult to conduct the radical operation for long-segment HD using laparoscopy. We used the following specific measures during the operation:
Setting of trocars
In the traditional laparoscopic operation for HD, trocars need to be placed at four locations on the abdominal wall, i.e., the four-hole method [11]. In the present study, the laparoscope was inserted through the left side of the navel. When dissecting the rectum, sigmoid colon, and descending colon, the harmonic scalpel was placed in the trocar in the right lower abdomen. When freeing the splenic flexure, greater omentum, transverse colon, hepatic flexure, and ascending colon, the harmonic scalpel was placed in the trocar in the left upper abdomen. Thus, only three holes were needed to complete the operation.
Correct use of harmonic scalpels
Using an harmonic scalpel in laparoscopic surgical procedures for children has the following advantages: (1) a harmonic scalpel can be used to separate and cut off the mesenteric blood vessels at the same time; (2) a harmonic scalpel replaces ligatures and titanium clips as the tool for closing and cutting blood vessels, which avoids foreign body residues in the tissue, reduces the frequency of changing instruments during surgery, and shortens the operation time; and (3) a harmonic scalpel can be used to effectively perform a coagulotomy of blood vessels with a diameter of less than 5 mm, which allows the operation to be performed on newborns and small infants. The aforementioned advantages of harmonic scalpels can be used to address the difficulty in dissecting the mesocolon when treating longsegment HD. In the present study, a 5 mm harmonic scalpel was used to dissect the mesocolon in all 13 surgeries. When using the scalpel, we correctly used either the coagulating function or the cutting function according to different types of tissue. Tissues such as the greater omentum, colonic ligament, and the surrounding of the rectum are loose and have relatively small blood vessels; therefore, it is possible to grasp and lift these tissues appropriately to increase tension, increase the grip on the handle of the harmonic scalpel, or select a relatively large energy output to accelerate the cutting speed. The blood vessels at the root of the mesentery are relatively thick; therefore, it is appropriate to use the “breakwater” method (i.e., blood vessels are first sealed and then cut off) to treat these blood vessels and ensure safety.
Treating of the intestines
• It is necessary to protect the marginal vessels of the colon when treating the mesocolon to ensure the circulation of the branches of the colon. When dissecting the middle colonic artery, it is necessary to pay attention to avoid damaging the right colonic artery. When freeing the middle segment of the ascending colon, it is possible to cut off the ascending branch of the right colonic artery, but it is also necessary to ensure that the descending branch is not damaged.
• The ascending colon is rotated 270 counterclockwise; i.e., the ascending colon is translocated first backward and then downward to allow it to freely descend into the pelvic cavity. The translocated intestine segment is examined to determine whether the mesocolon is pulled or compressed. In addition, the blood supply conditions in the intestine are also observed. The ascending colon that has been rotated downward should exhibit a ruddy color. In the present study, the Deloyers procedure was used to rotate the ascending colon. Treating the freed colon in the closed abdominal cavity is a difficult point and the key step of this operation. We used the following procedure: (1) the surgical table was positioned to lean to the left at an angle of 20° to allow the small intestine to move to the left abdomen; (2) grasping forceps were used to first lift the freed colon frame and then place the colon frame to the right abdomen; (3) the caecum, together with the ascending colon, was rotated forward and upward at the same time; and (4) the colon was pulled out of the anus and rotated, the ascending colon was appropriately rotated in such a way that it was neither excessively turned nor insufficiently turned, and the freed colon was pulled outside of the anus. The key points of the operation are summarized by the following. (1) It is necessary to dilate the anus properly before the operation. (2) When rotating and pulling the intestine, it is necessary to rotate and pull the intestine at the same time and not rotate the intestine after it has been removed; in addition, the rotation angle should be 270 counterclockwise. (3) The entire pulling and rotating process should be monitored under laparoscopy to ensure that the rotation angle of the intestine inside the abdominal cavity is consistent with that of the intestine outside the anus.
Among the 13 children in the present study, with the exception of one six-month-old child with moderate malnutrition who experienced anastomotic leakage after the operation, no children experienced any severe complication. Our laparoscopic radical operation for long-segment HD shows that this procedure can resolve a technical limitation of the operation that involves removing the colon via the anus, reduce the trauma caused by open operations, and produce the advantages of a minimally invasive technique.
Conclusion
The surgical procedure performed on the children in the present study showed a good short-term effect. Further followup evaluations will be conducted to determine the long-term effects of the procedure.
18802
References
- Georgeson KE, Fuenfer MM, Hardin WD (1995) Primary laparoscopic pull-through for Hirschsprung's disease in infants and children. J Pediatr Surg 30: 1017-1022.
- Hoffmann K, Schier F, Waldschmidt J (1996) Laparoscopic Swenson's procedure in children. Eur J Pediatr Surg 6: 15-17.
- Wang NL, Lee HC, Yeh ML, Chang PY, Sheu JC (2004) Experience with primary laparoscopy-assisted endorectal pull-through for Hirschsprung's disease. Pediatr Surg Int 20: 118-122.
- Cobellis G, Noviello C, Cruccetti A, Romano M, Mastroianni L, et al. (2011) Staged laparoscopic-assisted endorectal pull-through for long segment Hirschprung's disease and total colonic aganglionosis. Minerva Pediatr 63: 163-167.
- Rothenberg SS, Chang JH (1997) Laparoscopic pull-through procedures using the Harmonic Scalpel in infant and children with Hirschsprung's disease. J Pediatr Surg 32: 894-896.
- Bonnard A, de Lagausie P, Leclair MD, Marwan K, Languepin J, et al. (2001) Definitive treatment of extended Hirschsprung's disease or total colonic form. Surg Endosc 15: 1301-1304.
- Giuliani S, Betalli P, Narciso A, Grandi F, Midrio P, et al. (2011)Outcome comparison among laparoscopic Duhamel, laparotomic Duhamel, and transanal endorectal pull-through: a single-center, 18-year experience. J Laparoendosc Adv Surg Tech A 21: 859-863.
- van de Ven TJ, Sloots CE, Wijnen MH, Rassouli R, van Rooij I, et al.(2013) Transanal endorectal pull-through for classic segment Hirschsprung's disease: with or without laparoscopic mobilization of the rectosigmoid? J Pediatr Surg 48: 1914-1918.
- Craigie RJ, Conway SJ, Cooper L, Turnock RR, Lamont GL, et al.(2007) Primary pull-through for Hirschsprung's disease: comparison of open and laparoscopic-assisted procedures. J Laparoendosc Adv Surg Tech A 17: 809-812.
- Muensterer OJ, Chong A, Hansen EN, Georgeson KE (2010) Single-incision laparoscopic endorectal pull-through (SILEP) for hirschsprung disease. J Gastrointest Surg 14: 1950-1954.
- Tang ST, Yang Y, Wang GB, Tong QS, Mao YZ, et al. (2010) Laparoscopic extensive colectomy with transanal Soave pull-through for intestinal neuronal dysplasia in 17 children. Wordl J Pediatr 6: 50-54.