Keywords
Physical activity; Older adults; Mediation; Intervention; Health promotion; Public health; Exercise
Introduction
Poor health behaviors (e.g. smoking, poor diet, physical inactivity) are known as the leading causes of actual death in the United States [1]. Given the relationship between poor health behaviors and chronic disease, one potential way for reducing the burden of chronic diseases is by improving health behaviors [2]. A number of effective approaches and strategies for improving health behaviors have been identified [2,3] although given the high rates of chronic diseases [4,5] and poor health behaviors [6,7] among US adults, much work remains. One approach that has successfully increased physical activity levels is behavioral interventions. These types of programs incorporate cognitive-behavioral strategies that focus on changing an individual’s thoughts, behaviors, and circumstances [3].
Understanding the effectiveness of an intervention in exerting its effects on the outcome(s) of interest (i.e., physical activity) is undoubtedly important. However, perhaps just as important, is understanding how interventions exert their effects (i.e., the mechanisms by which behavior change occurs). Mediation analyses allow researchers to better understand the ‘how’ aspect of behavior changes, [8] and should be included as a part of all intervention evaluations. Theory should be used to guide behavior change interventions, as theories help explain behavior and can be used to develop ways to change behavior [9]. Theoretical constructs (e.g. social support, self-regulation, process of change, intention, etc.) are often the targets of intervention activities and are tested as mediators of behavior change. Such information is critical for developing interventions that can have the greatest potential to impact population health.
Although significant progress has been made in understanding how physical activity interventions exert their effects, [10-21] much work remains. Many theoretical constructs have been tested as mediators of change and results are not consistent. Self-efficacy [10,16,20]. Social support, [10] goal setting, [16,19] and behavioral processes [15,21] have been found to mediate change in physical activity behavior in some studies, although other studies have not found support for some of these constructs [12,13,16,19]. It is important to note that the samples included in these studies are quite diverse (i.e., older adults, pregnant women, cancer survivors, healthy populations). The mechanisms by which physical activity behavior change occurs may differ across these samples, potentially explaining some of the inconsistent findings. Therefore, it is important to study mediators across diverse populations in an effort to develop the most appropriate, tailored and effective programs for the population targeted. Very few mediation studies have been conducted with older adult populations [10,11].
The purpose of this paper is to investigate psychosocial mediators of physical activity change in a sample of older adults participating in a behavioral physical activity intervention. Active Living Every Day (ALED) is a 12-week, evidence-based physical activity intervention delivered in a small-group setting. Results from the overall trial showed a significant increase in objectively measured moderate to vigorous intensity physical activity (MVPA) in the ALED compared to a nutrition control group. We hypothesize that social support from family and friends, self-efficacy and selfregulation would be significant mediators of change in MVPA.
Design and Methods
Participants
Inactive older adults were recruited to take part in this study. Eligibility criteria included ≥ 50 years of age, not meeting physical activity guidelines (<150 minutes of moderate and/or <75 minutes of vigorous physical activity per week), and did not endorse any questions on the Physical Activity Readiness Questionnaire (PAR-Q). However, participants were not excluded if they took medication for hypertension, unless it was uncontrolled hypertension (≥ 160/100). Participants who were >69 years of age or endorsed any of the PAR-Q questions could participate if signed physician clearance was obtained.
A number of strategies were used to recruit participants, including announcements and emails to members of a University Learning Institute for older adults, emails via worksite listservs, flyers distributed at community health fairs and events, and newspaper ads. Participants interested in the study completed a phone screener (in person or via telephone) to assess eligibility.
Procedure
Eligible participants were scheduled for a measurement session that took place at Saginaw Valley State University. At the session, participants signed an informed consent document approved by the University’s Institutional Review Board, completed a survey and physical measures, and were given an Actigraph to wear for seven days. Participants were also randomized to one of two intervention groups: the physical activity group (Active Living Every Day ALED) or to the attention control nutrition group (Healthy Eating Every Day HEED). The survey, physical measures, and Actigraph procedures were repeated at the follow-up session (12 weeks, post intervention). The interventions were implemented in two waves, with each group (ALED and HEED) being led by a separate, trained facilitator.
Interventions
Active living every day (ALED): Participants randomized to the physical activity intervention received the ALED program, which is a 12-week, physical activity intervention delivered in a small-group setting. This evidence-based program incorporates constructs from the social cognitive theory [22] and transtheoretical model [23] in an effort to help participants engage in 150 minutes of moderate intensity physical activity per week. Structured exercise sessions were not a part of this intervention; instead, a lifestyle approach was emphasized.
Group sessions were held one time a week for 60 minutes, and were led by a trained facilitator. Each week focused on a behavioral strategy that would assist participants in becoming and remaining physically active. Examples of topics included goal setting, self-monitoring, reinforcement management, problem solving, social support, and relapse prevention. Starting in week 2, participants kept a daily log to self-monitor their physical activity, and during week 8, they received a pedometer and were instructed to self-monitor their steps throughout the duration of the intervention. Participants also set weekly goals (minutes of physical activity or steps). They were encouraged to set realistic, attainable goals, and to start small in an effort to enhance self-efficacy. The small-group delivery of the program allowed for social support from both the facilitator and other participants. Participants ‘checked in’ at the beginning of each group-based session, discussed challenges, if they met their physical activity goals, etc. Participants were encouraged by both the facilitator and other participants.
Healthy eating every day: Participants randomized to the attention control group received the HEED program. Although originally developed as a 20-week program, a shortened 14- week program is also available. In order to make the program a consistent length with ALED, the 14-week program was shortened into a 12-week program (per guidelines by the publisher). The HEED program was delivered in the same format as the ALED program by a trained facilitator. The goal of the program was to help participants improve their eating habits, in an effort to attain and maintain public health recommendations for nutrition. Similar to ALED, a number of behavioral strategies were incorporated in the weekly sessions, and a lifestyle approach for improving dietary habits was used.
Measures: All measures were completed at baseline (prior to randomization) and at 12 weeks (post-intervention).
Demographics: Participants self-reported their age, gender, race, marital status, and education level.
Body mass index: Objectively measured height (quarter inch) and weight (tenth of a pound) were obtained by trained staff. Body mass index (BMI) was calculated as kg/m2.
Physical activity: The Actigraph accelerometer (GT3x, Actigraph, LLC and Fort Walton Beach, FL) was used to objectively measure physical activity. Participants were instructed to wear the monitor on their right hip, during all waking hours (except while in water) for seven days. A 60- second epoch was used. In order to be included in analyses, participants had to wear the monitor for a minimum 10 hours per day, on three days [24]. Data recording 60 minutes or more of consecutive zeros were removed from analyses, as it was assumed the participant was not wearing the monitor [25]. The cut points from Freedson et al. [26] were used to convert the raw data counts into minutes of specific intensities of physical activity. Counts ≥ 1952 were considered MVPA. Mean minutes of MVPA per day were calculated and used in this study.
Social support: Social support for physical activity from family and friends in the past three months were measured (separately) using the 10-item Sallis et al. scale [27]. On a scale from 1 (none) to 5 (very often), participants rated how often they received support in various forms from family or friends for being physically active (e.g. gave me helpful reminders to exercise, changed their schedule so we could exercise together).
Self-efficacy: Self-efficacy for physical activity in the past six months was measured using a modified version of the 12-item Sallis et al. scale [28]. On a scale from 1 (not at all confident) to 4 (very confident), participants rated how confident they were that they could be physically active when encountering common barriers (e.g. get up early, even on weekends, to exercise, stick to your exercise program when you have household chores to attend to).
Self-regulation: Self-regulation for physical activity over the past four weeks was measured with the 12-item Umstattd et al. scale [29]. On a scale from 1 (never) to 5 (very often), participants rated how often they used various self-regulatory strategies for engaging in physical activity (e.g. I set short term goals for how often I am active, I rearranged my schedule to ensure I had time for physical activity).
Statistical analysis
Descriptive statistics included means and frequencies of key demographic and health-related variables. Independent samples t-tests and chi-squares examined 1) differences between participants retained at follow-up and lost to followup; and 2) baseline differences between intervention groups. Residualized change scores were calculated for all mediators and MVPA and used in all analyses. Because MVPA was skewed, a natural log transformation was used in all mediation analyses.
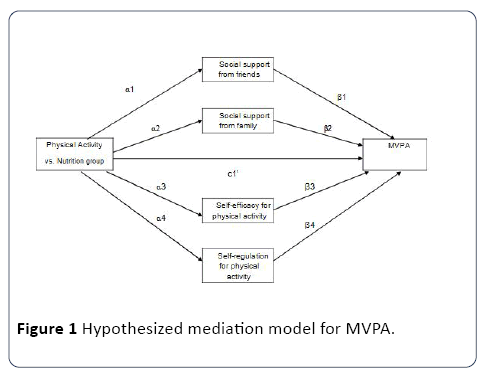
Pearson correlation coefficients were computed to examine correlations between changes in mediators and changes in MVPA. To examine whether changes in self-efficacy for physical activity, support from family and friends (separately) for physical activity, and self-regulation for physical activity mediated changes in MVPA, a parallel multiple mediator model using the SPSS PROCESS macro [30] was conducted (Figure 1). The macro simultaneously computes regression coefficients for the impact of the intervention on changes in the mediators, the associations between changes in the mediators and changes in MVPA, the direct effect, and the total indirect effect. Bias corrected bootstrapping with 10,000 resamples was used to generate 95% confidence intervals for direct and indirect effects. If the confidence interval did not include zero, significant mediation existed. All models controlled for age, gender, and education. Confidence intervals not including zero indicated significant mediation.
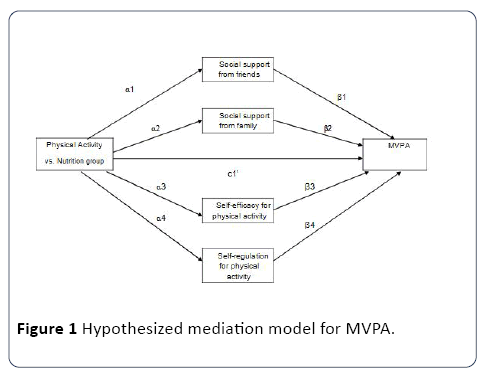
Figure 1: Hypothesized mediation model for MVPA.
Results
A total of 72 participants were randomized; of these, 47 had post data and were included in these analyses (65%). Those included in analyses were more educated than those not included (p=0.03). Demographic characteristics of the sample, by intervention group assignment (Table 1). Participants, on average, were 64.2 ± 8.2 years old and had a BMI of 34.2 ± 7.5 kg/m2. A majority of participants were female (72%), White (85%), had at least some college education (87%) and married (62%). A greater percentage of participants in the healthy eating group were married compared to the physical activity group (p=0.01). Correlations among mediator and outcome variables (Table 2).
Table 1 Demographic characteristics of participants (n=50).
| |
Exercise Group |
Nutrition Group |
| |
N |
Mean (SD) or % |
N |
Mean (SD) or % |
| Age, years |
23 |
64.1 (6.8) |
24 |
64.3 (9.6) |
| Gender |
| Male |
7 |
30.4 |
6 |
25 |
| Female |
16 |
69.6 |
18 |
75 |
| Race |
| White |
20 |
87 |
20 |
87 |
| Non-white |
3 |
13 |
3 |
13 |
| Marital statusa |
| Married/partnered |
10 |
43.5 |
19 |
79.2 |
| Not married |
13 |
56.5 |
5 |
20.8 |
| Education |
| High school graduate or less |
5 |
21.7 |
1 |
4.2 |
| Some college |
7 |
30.4 |
10 |
41.7 |
| College graduate |
11 |
47.8 |
13 |
54.2 |
| BMI, kg/m2 |
22 |
34.5 (7.8) |
24 |
33.9 (7.4) |
| Weight status |
| Normal weight (BMI<25) |
2 |
9.1 |
1 |
4.2 |
| Overweight (25³BMI<30) |
7 |
31.8 |
6 |
25 |
| Obese (BMI≥30) |
13 |
59.1 |
17 |
70.8 |
asignificant difference between groups, p<0.05
Table 2 Correlation matrix of mediator and outcome variables.
| |
|
1 |
2 |
3 |
4 |
| 1 |
Change in MVPAa |
- |
- |
- |
- |
| 2 |
Change in social support-friends |
0.03 |
- |
- |
- |
| 3 |
Change in social support- family |
-0.15 |
0.26 |
- |
- |
| 4 |
Change in self-efficacy for physical activity |
0.18 |
0.36b |
0.09 |
- |
| 5 |
Change in self-regulation for physical activity |
0.24 |
0.25 |
0.36b |
0.67b |
alog transformed
bp<0.05
Results from the mediation analyses (Table 3). There was no significant relationship between group assignment and changes in any of the hypothesized mediators (α path). There was a trend towards significance for the association between changes in social support from family (p=0.07) and changes in self-regulation for physical activity (p=0.07) and changes in MVPA (β path). There was no evidence of significant mediation for any of the mediators examined: social support from family (indirect effect=-0.04; 95% CI, -0.37, 0.07), social support from friends (indirect effect=-0.004; 95% CI, -0.13, 0.06), selfefficacy for physical activity (indirect effect=0.05; 95% CI, -0.06, 0.40) and self-regulation for physical activity (indirect effect=-0.11; 95% CI, -0.45, 0.06).
Table 3 Results from the mediation models: Change in MVPA.
| |
Social Support-Friends |
Social Support-Family |
Self-efficacy |
Self-regulation |
| Path coefficients |
| |
Estimate (SE) |
Estimate (SE) |
Estimate (SE) |
Estimate (SE) |
α path (group→
mediator) |
-0.08 (0.25) |
0.11 (0.21) |
0.22 (-0.18) |
-0.29 (0.26) |
| β path (mediator→MVPA) |
0.04 (0.15) |
-0.36 (0.19) |
-0.24 (0.29) |
0.38 (0.20) |
| Indirect and direct effects |
| |
Estimate (SE) 95% CI |
Estimate (SE) 95% CI |
Estimate (SE) 95% CI |
Estimate (SE) 95% CI |
αβ (group→mediator→
MVPA) |
-0.004 (0.04) |
-0.04 (0.10) |
0.05 (0.10) |
-0.11 (0.12) |
| |
-0.13, 0.06 |
-0.37, 0.07 |
-0.06, 0.40 |
-0.45, 0.06 |
| Total indirect |
-0.10 (0.12)
-0.39, 0.12 |
| Direct effect |
-0.598 (0.23)
-1.04, -0.12 |
| |
Note: All models adjusted for age, gender, and education; Unstandardized coefficients and standard errors are presented; Log transformation of MVPA was used in analyses; Bold indicates significant pathway, indirect, or direct effect
Discussion
Finding effective ways to promote physical activity in older adults is important, given the aging population [31]. Older adults have an increased risk of chronic health conditions which can negatively affect quality of life, independence and cost of health care; [32] physical activity may help alleviate some of the burdens associated with aging. Although a number of interventions have been developed and implemented in an effort to increase physical activity in older adults, very few studies have examined how these interventions exert their effects.
This study examined psychosocial mediators of a 12-week, behavioral physical activity intervention that resulted in significant increases in MVPA. Interestingly, none of the variables tested were found to be significant mediators of change in MVPA. It appears that other variables, not measured in this study, may have caused the changes in physical activity. For example, behavioral processes of change (transtheoretical model), which have been shown to mediate change in physical activity in other studies, [15,21,33] were not assessed in this study. Although social support, self-efficacy and self-regulation were not found to be significant mediators in this study, the importance of these variables in changing older adults’ physical activity should not be discounted. The sample size of this pilot study was small, potentially limiting power to detect significant relationships. A fully powered trial may provide more insight into what causes changes in physical activity in group-based interventions with older adults.
Mediation analyses are valuable, as they allow researchers to explore how effective the intervention was in (1) changing the theoretical constructs targeted (i.e., mediators), and (2) if changes in those theoretical constructs were associated with changes in the outcomes. The results from this study indicate that the intervention may not have been effective in changing any of the hypothesized mediators. Although evidence-based programs such as ALED can be adapted to the targeted population, one must assure implementation fidelity; therefore the content and overall philosophy of the groupbased sessions should not be changed. It is possible that the content included in the group-based sessions was not delivered effectively or intensely enough for changes in the mediators to occur. Alternatively, it is possible that the intervention did change the mediators, but the measures used were unable to accurately capture change or were not sensitive enough to change [34]. This may be particularly relevant to social support. An important piece of this intervention was support from the group facilitator and other participants in the intervention. Although social support from family and friends was assessed, participants may not have considered the facilitator or other group members as ‘friends’. Therefore, changes in perceived support from these individuals may have been missed.
Much work remains in how to effectively design intervention components/activities that can successfully change the underpinning theoretical variables hypothesized to change physical activity, as many studies examining mediators of physical activity change have failed to change the targeted mediators [35]. A recent review by Prestwich and colleagues [36] found that although over half of intervention studies focused on physical activity or healthy eating (56%) reported that the intervention was based on theory, theory was rarely used to extensively develop the intervention, and few studies targeted all of the theoretical constructs, or linked the behavior change techniques used to the underlying theoretical constructs [36]. These findings may in part explain why many interventions have not been successful in changing mediating variables.
Changes in the mediators were not significantly associated with changes in MVPA, which not surprising is given the fact that the intervention was not successful in producing changes in the mediators (i.e., if mediators do not change, one would not expect changes to be related to outcomes). However, there was a trend towards significance for social support from family and self-regulation, perhaps pointing to the importance of these variables in changing physical activity behaviors in older adults, and the appropriateness of the theoretical underpinnings of the ALED program. Self-regulation, particularly self-monitoring, has been shown to be effective in increasing physical activity, [37] and should continue to be explored in future mediation analyses.
Although the ALED program is an evidence-based program shown to be effective in changing physical activity (and is supported by the outcomes in this study, mediators of change in the ALED program have not been readily studied [10]. Although one can speculate, the mechanisms by which the program actually ‘works’ are unknown. A study by Becofsky et al. [10] found that social support and self-efficacy mediated changes in physical activity in a large sample of adults ≥ 50 years of age. However, it is important to note that this study did not have a control group; instead, they examined if social support and self-efficacy mediated the relationship between attendance at ALED group sessions and changes in physical activity. The lack of mediation studies conducted in older adult samples, [10,11] and the inconsistent findings in understanding how interventions exert their effects, [33,35,38] confirm the need for future research. Not only should studies report the effects of the intervention on targeted outcomes, but they should also report results from mediation analyses. However, this can be challenging in community-based interventions, as there is a fine balance between appropriately measuring all variables/outcomes at multiple time points, while also considering participant burden.
Furthermore, studies with null findings [12,13,18,39] should also be published, as they contribute significantly to our overall understanding of how we can develop and implement more effective physical activity interventions.
Conclusion
Although insightful, some limitations should be considered when interpreting the findings of this study. These include the small sample size of this pilot-study (underpowered to detect meditational effects), the high attrition rate, and demographic characteristics of our sample (mostly white, well-educated, females), which may limited the generalizability of our findings. Limitations withstanding, this study contributes to the small number of studies examining mediators of physical activity change in older adult populations, and is among the small number of mediation studies using objective measures of physical activity.
As health professionals and educators continue to develop and implement interventions aimed at improving health behaviors such as physical activity across various populations, efforts to better understand how/why these programs are successful must also continue. Each published mediation study contributes to the growing knowledge base of understanding the ‘how’ and ultimately moves us one step closer to developing the most effective, targeted, cost-effective, and appropriate interventions for various populations trying to improve their health by increasing physical activity.
20135
References
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL (2004) Actual causes of death in the United States, 2000. JAMA 291: 1238-1245.
- Mozaffarian D, Afshin A, Benowitz NL, Bittner V, Daniels SR, et al. (2012) Population approaches to improve diet, physical activity, and smoking habits: A scientific statement from the American Heart Association. Circulation 126: 1514-1563.
- Artinian NT, Fletcher GF, Mozaffarian D, Kris-Etherton P, Van Horn L, et al. (2010) Interventions to promote physical activity and dietary lifestyle changes for cardiovascular risk factor reduction in adults: a scientific statement from the American Heart Association. Circulation 122: 406-441.
- Flegal KM, Carroll MD, Ogden CL, Curtin LR (2010) Prevalence and trends in obesity among US adults, 1999-2008. JAMA 303: 235-241.
- Ward BW, Schiller JS (2013) Prevalence of multiple chronic conditions among US adults: estimates from the National Health Interview Survey, 2010. Prev Chronic Dis 10: E65.
- Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, et al. (2008) Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc 40: 181-188.
- Krebs-Smith SM, Guenther PM, Subar AF, Kirkpatrick SI, Dodd KW (2010) Americans do not meet federal dietary recommendations. J Nutr 140: 1832-1838.
- Hayes A (2013) Introduction to mediation, moderation, and conditional process analysis: Aregression-based approach. The Guilford Press, New York.
- Glanz K, Bishop DB (2010) The role of behavioral science theory in development and implementation of public health interventions. Annu Rev Public Health 31: 399-418.
- Becofsky K, Baruth M, Wilcox S (2014) Psychosocial mediators of two community-based physical activity programs. Ann Behav Med 48: 125-129.
- Stralen MM, de Vries H, Mudde AN, Bolman C, Lechner L (2009) The working mechanisms of an environmentally tailored physical activity intervention for older adults: A randomized controlled trial. Int J BehavNutrPhys Act 6: 83.
- Baruth M, Wilcox S (2014) Psychosocial mediators of physical activity and fruit and vegetable consumption in the faith, activity, and nutrition programme. Public Health16: 1-9.
- Baruth M, Wilcox S, Blair S, Hooker S, Hussey J, et al. (2010) Psychosocial mediators of a faith-based physical activity intervention: implications and lessons learned from null findings. Health Educ Res 25: 645-655.
- Plotnikoff RC, Pickering MA, Rhodes RE, Courneya KS, Spence JC (2010) A test of cognitive mediation in a 12-month physical activity workplace intervention: Does it explain behaviour change in women? Int J BehavNutrPhys Act 7: 32.
- Lewis BA, Williams DM, Martinson BC, Dunsiger S, Marcus BH (2013) Healthy for life: A randomized trial examining physical activity outcomes and psychosocial mediators. Ann Behav Med 45: 203-212.
- Fjeldsoe BS, Miller YD, Marshall AL (2013) Social cognitive mediators of the effect of the MobileMums intervention on physical activity. Health Psychol 32: 729-738.
- Valle CG, Tate DF, Mayer DK, Allicock M, Cai J (2015) Exploring mediators of physical activity in young adult cancer survivors: Evidence from a randomized trial of a facebook-based physical activity intervention.J Adolesc Young Adult Oncol 4: 26-33.
- Thomson JL, Tussing-Humphreys LM, Zoellner JM, Goodman MH (2016) Psychosocial constructs were not mediators of intervention effects for dietary and physical activity outcomes in a church-based lifestyle intervention: Delta Body and Soul III. Public Health Nutr19: 2060-9.
- Stacey FG, James EL, Chapman K, Lubans DR (2016) Social cognitive theory mediators of physical activity in a lifestyle program for cancer survivors and carers: Findings from the ENRICH randomized controlled trial. Int J BehavNutrPhys Act 13: 49.
- Plotnikoff R, Lubans D, Penfold C, Courneya K (2014) Testing mediator variables in a physical activity intervention for women with type 2 diabetes. Psychol Sport Exerc 15: 1-8.
- Baruth M, Wilcox S, Dunn AL, King AC, Marcus BH, et al. (2010) Psychosocial mediators of physical activity and fitness changes in the activity counseling trial. Ann Behav Med 39: 274-289.
- Bandura A (1986) Social foundations of thought and action: A social cognitive theory.Prentice Hall, New Jersey.
- Prochaska JO, DiClemente CC, Norcross JC (1992) In search of how people change. Applications to addictive behaviors. Am Psychol 47: 1102-1114.
- Trost SG, McIver KL, Pate RR (2005) Conducting accelerometer-based activity assessments in field-based research. Medicine Sci Sports Exercise 37: S531-543.
- Masse LC, Fuemmeler BF, Anderson CB, Matthews CE, Trost SG, et al. (2005) Accelerometer data reduction: a comparison of four reduction algorithms on select outcome variables. MedSci Sports Exercise 37: S544-554.
- 26.Freedson PS, Melanson E, Sirard J (1998) Calibration of the computer science and applications, Inc. accelerometer. Med Sci Sports Exercise 30: 777-781.
- Sallis JF, Grossman RM, Pinski RB, Patterson TL, Nader PR (1987) The development of scales to measure social support for diet and exercise behaviors. Prev Med 16: 825-836.
- Sallis JF, Pinski RB, Grossman RM, Patterson TL, Nader PR (1988) The development of self-efficacy scales for health-related diet and exercise behaviors. Health Educ Res 3: 283-292.
- Umstattd MR, Motl R, Wilcox S, Saunders R, Watford M (2009) Measuring physical activity self-regulation strategies in older adults. J Phys Act Health 1: S105-112.
- Hayes AF (2013) Introduction to mediation, moderation and conditional process analysis. The Guilford Press, New York.
- Ortman J, Velkoff V, Hogan H (2014)An aging nation: The older population in the UnitedStates. US Census Bureau,Washington, DC.
- Centers for disease control and prevention (2013) Thestate of aging & health in America 2013. Centers for Disease Control and Prevention, US Dept of Health and Human Services, Atlanta, GA.
- Lewis BA, Marcus BH, Pate RR, Dunn AL (2002) Psychosocial mediators of physical activity behavior among adults and children. Am J Prev Med 23: 26-35.
- MacKinnon DP(1994) Analysis of mediating variables in prevention and intervention research. NIDA Research Monograph Series 139: 127-153.
- Rhodes RE, Pfaeffli LA (2010) Mediators of physical activity behaviour change among adult non-clinical populations: a review update. Int J BehavNutrPhys Act 7: 37.
- Prestwich A, Sniehotta FF, Whittington C, Dombrowski SU, Rogers L, et al. (2014) Does theory influence the effectiveness of health behavior interventions? Meta-analysis. Health Psychol 33: 465-474.
- Michie S, Abraham C, Whittington C, McAteer J, Gupta S (2009) Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychol 28: 690-701.
- Lubans DR, Foster C, Biddle SJ (2008) A review of mediators of behavior in interventions to promote physical activity among children and adolescents. Prev Med 47: 463-470.
- Lubans D, Mundey C, Lubans N, Lonsdale C (2013) Testing physical activity mediators in an intervention for sedentary older adults. Int J Sport Psychol44: 252-262.