Keywords
Antenatal depression; Trait anxiety; Marital satisfaction; Counselling; Pregnancy
Introduction
According to World Health Organization [1] depression has been found to be the primary cause of morbidity in middleand high- income countries. Postnatal depression shares similar prevalence ratings to those of depression in the general population, ranging from 12-20%, with risk factors of postnatal depression. However, individual studies suggest that the rate of antenatal depression (AD) ranges from 4.8% up to 40% [2-9]. The rate of antenatal depression identified by previous studies are of concern and underscore the importance of investigating factors which contribute to the presentation of depression during pregnancy. Therefore, several professional organizations now recommend routine screening for antenatal depression either in every antenatal visit [10] or in each trimester of pregnancy [11]. It is noteworthy, that the prevalence of antenatal depression in a recent Irish study [12] was 86.5%. The authors claimed that the extremely high rate of depression might was attributed to economic hardship, loss of salary and unemployment. Obviously, the rapid collapse of the Irish economy in 2008 might led the pregnant women to experience economic insecurity and subsequent loss of subjective well-being and therefore it seems that the investigation of the antenatal depression rate in Greece would be of great interest.
According to the previous literature, risk factors for antenatal depression include history of depression, lack of a partner, marital difficulties, maladaptive coping strategies, family violence, increased life stress, maladaptive coping strategies, substance abuse, history of previous abortions, unplanned pregnancy, ambivalence toward the pregnancy and anxiety about the fetus [2,13-15]. The current literature also suggests that low income and unemployment are major risk factors of antenatal depression too [4,9,10].
Although the aforementioned risk factors for antenatal depression have been extensively investigated, it is noteworthy that investigation of the association between personality traits (e.g. neuroticism), and antenatal depression is a relatively neglected area of research. Personality traits are stable patterns of thought, emotion and behaviour that characterise an individual across time and situations [16] With respect to personality characteristics, there is substantial evidence that higher levels of neuroticism seem to be predictive of higher levels of stress and of a negative emotional response to stressors outside of pregnancy [17]. More specifically, neuroticism is a personality trait that may predict individual’s susceptibility to psychological stress as it is characterized by the tendency of the individual to experience negative emotions (anxiety) [18]. Trait anxiety is a central component of neuroticism [19].
The role of social and marital support has been extensively studied concerning antenatal depression. However, the evidence regarding marital support, social support and antenatal depression is contradictive. Many previous studies have shown that low perception of social support is an important predictor of antenatal depression [2,20,21]. However, many studies have failed to find a stress buffering effect of social support on depression during pregnancy [22-26].
Therefore, the aim of this study was to investigate the predictive value of trait anxiety, social support and marital support on antenatal depression.
Methods
Sample and data collection procedures
The study was conducted in a public hospital of Athens, Greece. The questionnaires were administered to a sample of pregnant women with a gestational age of between 11 and 26 weeks, who were booked for antenatal screening in the antenatal clinic of the hospital. During the recruitment period (from January 2011 to March 2011), all eligible women who attended antenatal clinic (N=180) were invited to participate in the study. Inclusion criteria were:
1) Age equal or higher than 18 years old, and
2) High fluency in Greek language.
Finally, 165 women agreed to participate and completed the questionnaires (response rate 91%). Non- participation was mainly due to time constraints (lack of time to complete the questionnaire). According to Green [27], this sample size is considered adequate for testing the overall fit of a regression model with up to 10 independent variables.
Study instruments
The Center for Epidemiologic Studies- Depression scale (CES-D) was used to assess depression symptoms of the study population [28]. CES-D is a self-reporting 20-item scale that covers affective, behavioral, and somatic symptoms experienced during the past week. Responses to item statements are graded from 0 (rarely or none of the time) to 3 (most or all of the time). Four items are reverse-scored items. Scores for each item in the CES-D scale are summed to obtain an overall score. The overall score ranges from 0 to 60, where the higher the score the more frequent the depressive symptoms. A cut-off score of 16 or higher has been used in this study as the point which is indicative of significant or mild depressive symptomatology [29,30]. The CES-D has been adapted to Greek and has been found to have satisfactory psychometric properties [31]. A Cronbach’s alpha of 0.86 was obtained in this study.
Trait anxiety was measured with the Trait Anxiety Subscale of the State- Trait Anxiety Inventory (STAI) [32]. Trait anxiety is a central component of neuroticism and reflects how dispositionally anxious is a person across time and situations [19]. The trait scale consists of 20 items and ask people to describe how they generally feel (e.g., confident), rated on a four-point frequency scale ranging from (1) almost never to (4) almost always. Total score for trait anxiety ranges from 20 to 80. The STAI has been adapted to Greek and has been found to have satisfactory psychometric properties [33]. Cronbach’s alpha of 0.87 was obtained in the present study.
Marital quality was measured with the Quality of Marriage Index [34]. The QMI is a self-report measure which contains 6 items regarding marital quality and satisfaction. Sample items include ‘‘My relationship with my partner is very stable’’ and ‘‘My relationship with my partner makes me happy.’’ The first five items are scored on a seven-point Likert-type scale ranging from very strongly disagree (1) to very strongly agree (7). The sixth item is scored on a ten-point Likert-type scale ranging from extremely unhappy (1) to extremely happy (10). Higher scores indicate overall satisfaction with one’s marriage. The QMI has been adapted to Greek language and has been found to have satisfactory psychometric properties [35]. Cronbach’s alpha coefficient of 0.91 was obtained in the present study.
Satisfaction with perceived social support was measured with the Social Support Questionnaire-6 [36]. SSQ-6 is a self-administered questionnaire used to measure the availability of social support/ number of supporters (SSQ-Network) and the satisfaction with social support (SSQ-Satisfaction). The SSQ-6 contains six items and each item involves two parts: a) respondents are asked to list all the individuals whom they can count for support or help (SSQ-N) and, b) how satisfied they are with the support available (SSQ-S). The subscale of SSQ-S was used in this study for measuring satisfaction with perceived social support. The SSQ-S items are scored on a six point Likert scale ranging from very dissatisfied (1) to very satisfied (6). Total score for SSQ-S ranges from 6 to 36 and higher scores indicate higher satisfaction with perceived support. The SSQ-6 has been adapted to Greek and has been found to have satisfactory psychometric properties [37]. Cronbach’s alpha coefficient of 0.83 was obtained in the present study.
Basic demographic and medical information included: age, gestational age, parity, previous miscarriages, previous deliveries, complications during previous pregnancy and labour, previous infertility problems and previous in-vitro fertilization (IVF) treatment, marital status, educational level, economic level, and employment status. The educational level was categorized as low (up through elementary school), medium (high school certificate) or high (university degree). The annual income level was categorized as low (9,600-17,999 €), medium (18,000-35,999 €) or high (>36,000 €) [38].
Statistical analysis
The statistical analyses were conducted using SPSS version 20.0. Univariate frequency distributions, means and standard deviations were calculated for the variables (demographic characteristics of participants). Hierarchical multiple linear regression was performed to test the relationships between a set of independent variables (e.g. marital satisfaction) and a dependent variable (e.g. depression). First, the relationships between individual psychosocial, demographic and medical independent variables (continuous and categorical) and dependent variable were explored by using independent t-test, chi-square, Pearson correlations and one-way ANOVA. Then multiple regression analysis was performed with the independent variables that were significant in bivariate analyses at a 0.05 significance level. Two steps were conducted: the demographic and medical variables were entered in the first step, while the psychosocial variables were entered in the second step. The independent variables regarding “previous miscarriage”, and “employment” were used as dichotomized categorical variables (“yes” coded 1 vs. “no” coded 0). The independent variables regarding “income level” and “educational level” were used as categorical independent variables (low coded 1, medium coded 2 and high coded 3). The R-square was an indicator of how much variance was explained by the model compared to how much variance was not explained after the model had been fitted. Large R-square values indicated that the model explained high proportion of variance in the outcome variable. All statistical tests were two-sided and performed at a significance level of 0.05.
Ethics
The Research and Ethics Committee of the Elena Benizelou hospital approved this study protocol. All participants in this study were informed about the scope and the purpose of the study. Eligible women were also assured that the collected data would be used only for the purpose of the study, and that their decision to withdraw would not compromise the standard of the received care. A signed informed consent was obtained from all study participants.
Results
Characteristics of participants and preliminary analysis
The mean age of participants was 31.2 years (SD 4.2; range 22–44 years). Sixty-two percent had education beyond high school, 37% had high school and 1% had less than a high school education. Forty-three percent of women had low annual income level, 51% had medium annual income level and 6% had high annual income level. Eighty percent of women participated in the workforce and 96% were married. For 46% of the sample this was their first pregnancy, 36% had already a child, 22% of the women had experienced previous miscarriages and 12% of the participants had experienced a complication during previous pregnancy or previous labour. The mean score for CES-D was 13.4 (SD= 9.2). More specifically, 32.7% of participants had depression score ≥ 16 indicating depressive symptoms.
Correlations between demographical/ medical variables and depression
The relationship between women’s depression and their demographic characteristics was explored. Women with low annual income level and low educational level had higher incidence of depressive symptoms than women with medium or high income or educational level (F=3.219, p=0.043; F=4.718, p=0.010, respectively). Women with a previous history of miscarriage had higher levels of depressive symptoms than women with no history of miscarriage (t=2.340, p=0.024). Age, marital status, parity, employment, gestational age and previous history of obstetric complications were not significantly related to depressive symptoms.
Correlations between trait anxiety, social support, marital satisfaction and antenatal depression
Intercorrelations between psychosocial variables and depression were explored. Most of the correlations were statistically significant and in the expected direction. Findings suggested that depression was statistically significantly correlated with low social support, low marital satisfaction and high trait anxiety (r=- 0.200, p=0.018, r=-0.280, p=0.001, r=0.739, p<0.001, respectively).
Multiple Linear Regression Analysis
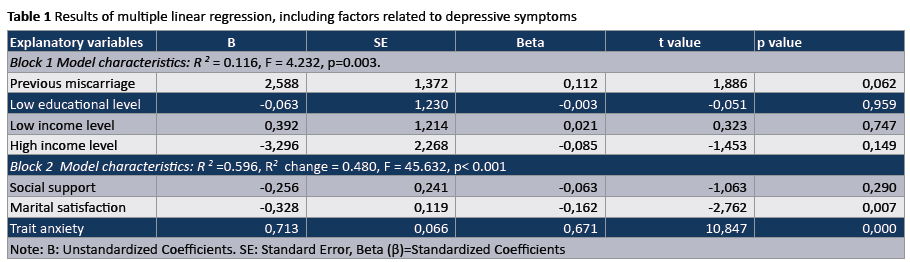
Hierarchical linear multiple regression analysis was conducted to identify variables that were significantly related to depressive symptomatology. According to the standardized regression coefficients no demographic or medical independent variable was significantly related to depressive symptomatology. According to their standardized regression coefficients, quality of marriage and trait anxiety were the psychosocial variables that were significantly related to depressive symptomatology (β=- 0.328, p=0.007; β=0.713, p<0.001, respectively). The negative regression coefficient for the variable of “marital satisfaction” suggested that women who had lower marital satisfaction had higher levels of depressive symptomatology. Accordingly, the positive regression coefficient for the variable of “trait anxiety” suggested that women who had higher trait anxiety had higher levels of depressive symptomatology (Table 1).
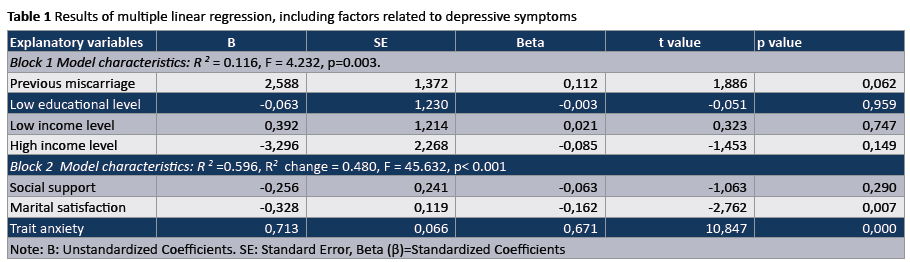
The model R2 when only the medical and demographic variables were entered in the model was equal to 0.116, suggesting that approximately 11% of the variance in depressive symptomatology was explained by these variables (income level, educational level, history of miscarriage). When the psychosocial variables were added to the model, there was a significant improvement (R2 change =0.480, F=45.632, p<0.001). More specifically, an additional 48% of the variance in depressive symptomatology was explained by the psychosocial variables. The total proportion of variance in depressive symptomatology explained by all the independent variables was 59%.
Discussion
The authors of this study aimed to investigate the psychosocial risk factors for depressive symptomatology, applying multivariate statistical techniques to control for the effects of demographic and medical background variables. Results of this study suggest that antenatal depression is prevalent in almost one third of pregnant women in Greece. Previous history of miscarriage, low income and low educational level showed significant associations with antenatal depressive symptomatology at the univariate level. In addition, low marital satisfaction and high trait anxiety showed significant associations with antenatal depressive symptomatology at the multivariate level.
It is noteworthy that the stress buffering effects of social support on antenatal depression was not confirmed by our study findings. This is consistent with previous studies that have failed to find a significant association between low social support and high antenatal depression [22-26]. Consistent with previously reported findings, a strong association was identified between poor marital relationships and depression during pregnancy [25,39,40]. According to the study findings, it may be concluded, that pregnant women living in the Greek society may desire to share pregnancy worries only with their partners and not with their social network.
Study results also suggested that antenatal depression and trait anxiety, which is a central component of neuroticism, were significantly associated with each other. The association between trait anxiety and depression is well documented in psychological research outside of pregnancy [17]. However, as it has been referred in the introduction section, investigation of the association between trait anxiety and antenatal depression is a relatively neglected area of research. Only a few studies have explored the association between antenatal trait anxiety and depression. A study by Da Costa et al., [22] concluded that more depressed women during pregnancy had higher levels of trait anxiety. The study by Moos et al., [41] which explored the nature of the relationship between anxiety and depression during pregnancy concluded that antenatal anxiety was a significant predictor of antenatal depression. A recent study by Roos et al., [42] which investigated the predictors of distress and anxiety in pregnancy found that trait anxiety was a significant predictor of antenatal distress and anxiety. Univariate findings regarding the significant associations between low income, low educational level and high depressive symptomatology have been interpreted and discussed elsewhere [15].
Most of the tested psychosocial variables significantly contributed to antenatal depression. Nevertheless, the findings indicated that medical, demographic and psychosocial variables explained no more than 57% of the variance in the antenatal depression. Therefore, the potential importance of other variables remains to be explored.
Conclusion and Implications for Practice
The importance of antenatal depression has been largely underestimated with the focus of research and intervention programs maintained on postnatal depression. Depression, and other stressful feelings such as anxiety during prenatal period can be proved harmful to the mother, fetus and the expectant newborn’s health. Therefore, it is essential to investigate the incidence and risk factors for antenatal depression during pregnancy in order to implement interventions for reducing depressive symptomatology levels. The current study suggests that low marital satisfaction and high trait anxiety, which is a central component of neuroticism, are major risk factors for antenatal depression. Therefore, health care professionals must enhance the implementation of interventions and counseling services for decreasing the levels of trait anxiety and improving the marital relationships during pregnancy. Interventions could include relaxation techniques, stress management, couple counseling, group therapies. Midwives in particular should be trained in the detection of antenatal depression by using validated instruments and structured interviews and in the subsequent referral of high-risk women.
3803
References
- Leigh B, Milgrom J (2008) Risk factors for antenatal depression, postnatal depression and parenting stress. BMC Psychiatry 8: 24.
- Qiao YX, Wang J, Li J, Ablat A (2009) The prevalence and related risk factors of anxiety and depression symptoms among Chinese pregnant women in Shanghai. Aust N Z J Obstet Gynaecol 49: 185-190.
- Melville JL, Gavin A, Guo Y, Fan MY, Katon WJ (2010) Depressive disorders during pregnancy: prevalence and risk factors in a large urban sample. Obstet Gynecol 116: 1064-1070.
- Mohammad KI, Gamble J, Creedy DK (2011) Prevalence and factors associated with the development of antenatal and postnatal depression among Jordanian women. Midwifery 27: e238-245.
- Bödecs T, Horváth B, Kovács L, Diffellné Németh M, Sándor J (2009) Prevalence of depression and anxiety in early pregnancy on a population based Hungarian sample. Orv Hetil 150: 1888-1893.
- Faisal-Cury A, Savoia MG, Menezes PR (2012) Coping style and depressive symptomatology during pregnancy in a private setting sample. Span J Psychol 15: 295-305.
- Kaaya S, Mbwambo J, Kilonzo G, Van Den Borne H, Leshabari M, et al., (2010) Socio-economic and partner relationship factors associated with antenatal depressive morbidity among pregnant women in Dares Salaam, Tanzania. Tanzan J Health Res 12: 23-35.
- Lee AM, Lam SK, Sze Mun Lau SM, Chong CS, Chui HW, et al. (2007) Prevalence, course, and risk factors for antenatal anxiety and depression.Obstet Gynecol 110: 1102-1112.
- National Collaborating Center for Mental Health. (2007) Antenatal and postnatal mental health: the NICE guideline on clinical management and service guidance. The British Psychological Society and The Royal College of Psychiatrists; London, Great Britain.
- American College of Obstetricians and Gynecologists Committee on Health Care for Undeserved Women1 (2006) ACOG Committee Opinion No. 343: psychosocial risk factors: perinatal screening and intervention.Obstet Gynecol 108: 469-477.
- Carolan-Olah M, Barry M (2014) Antenatal stress: an Irish case study. Midwifery 30: 310-316.
- Lancaster CA, Gold KJ, Flynn HA, Yoo H, Marcus SM, et al. (2010) Risk factors for depressive symptoms during pregnancy: a systematic review. Am J Obstet Gynecol 202: 5-14.
- Breedlove G, Fryzelka D (2011) Depression screening during pregnancy. J Midwifery Womens Health 56: 18-25.
- Gourounti K, Anagnostopoulos F, Lykeridou K (2013) Coping strategies as psychological risk factor for antenatal anxiety, worries, and depression among Greek women. Arch Womens Ment Health 16: 353-361.
- Ogden J (2007) Health Psychology (4thedn) Open University Press, New York.
- Holahan CJ, Moos RH (1985) Life stress and health: personality, coping, and family support in stress resistance. J Pers Soc Psychol 49: 739-747.
- Morrison V and Bennett P (2006) An introduction to health psychology. Pearson Education Limited , UK.
- Spielberger C, Gorsuch R and Lushene R (1970) STAI manual for the State-Trait Anxiety Inventory. Consulting Psychologists Press, Paulo Alto.
- Rich-Edwards JW, Kleinman K, Abrams A, Harlow BL, McLaughlin TJ, et al. (2006) Sociodemographic predictors of antenatal and postpartum depressive symptoms among women in a medical group practice.J Epidemiol Community Health 60: 221-227.
- Faisal-Cury A, Menezes P, Araya R, Zugaib M (2009)Archives of Women's Mental Health (12thedn) Springer Vienna.
- Da Costa D, Larouche J, Dritsa M, Brender W (2000) Psychosocial correlates of prepartum and postpartum depressed mood. J Affect Disord 59: 31-40.
- Ritter C, Hobfoll SE, Lavin J, Cameron RP, Hulsizer MR (2000) Stress, psychosocial resources, and depressive symptomatology during pregnancy in low-income, inner-city women. Health Psychol 19: 576-585.
- Pakenham KI, Smith A, Rattan SL (2007) Application of a stress and coping model to antenatal depressive symptomatology.Psychol Health Med 12: 266-277.
- Escribè-Agüir V, Gonzalez-Galarzo MC, Barona-Vilar C, Artazcoz L (2008) Factors related to depression during pregnancy: are there gender differences? J Epidemiol Community Health 62: 410-414.
- Latendresse G, Ruiz RJ (2010) Maternal coping style and perceived adequacy of income predict CRH levels at 14-20 weeks of gestation. Biol Res Nurs 12: 125-136.
- Green S (1991) How many subjects does it take to do a regression analysis? Multivariate Behav Res 26: 499-510.
- Radloff, L (1977) The CES-D Scale: a self report depression scale for research in the general population. Applied Psychol Measur 1: 385-401.
- Räikkönen K, Pesonen AK, Kajantie E, Heinonen K, Forsén T, et al. (2007) Length of gestation and depressive symptoms at age 60 years. Br J Psychiatry 190: 469-474.
- Beeghly M, Weinberg MK, Olson KL, Kernan H, Riley J, et al. (2002) Stability and change in level of maternal depressive symptomatology during the first postpartum year. J Affect Disord 71: 169-180.
- Madianos MG, Stefanis CN (1992) Changes in the prevalence of symptoms of depression and depression across Greece.Soc Psychiatry Psychiatr Epidemiol 27: 211-219.
- Spielberger C (1972) Anxiety: Current trends in research. Academic Press, London.
- Liakos A, Gianitsi S (1984) The validity and reliability of the revised Greek anxiety scale by Spielberger. Encefalos 21: 71–76.
- Norton R (1983) Measuring marital quality: A critical look at the dependent variable. J Marriage Fam 45: 141–151.
- Tsaggarakis M, Stalikas A (2012)The psychometric instruments in Greece: Quality of Marriage Index. Pedio, Athens.
- Sarason, I., Sarason B, Shearin E, Pierce G (1987) A brief measure of social support: practical and theoretical implications. J Soc Pers Relat 4: 497-510.
- Kafetsios K (2002) The psychometric instruments in Greece: Social Support Questionnaire-Short Form. Ellinika Grammata, Athens.
- Records K, Rice M (2007) Psychosocial correlates of depression symptoms during the third trimester of pregnancy. J Obstet Gynecol Neonatal Nurs 36: 231-242.
- Nasreen HE, Kabir ZN, Forsell Y, Edhborg M (2011) Prevalence and associated factors of depressive and anxiety symptoms during pregnancy: a population based study in rural Bangladesh. BMC Womens Health 11: 22.
- Moss KM, Skouteris H, Wertheim EH, Paxton SJ, Milgrom J (2009) Depressive and anxiety symptoms through late pregnancy and the first year post birth: an examination of prospective relationships. Arch Womens Ment Health 12: 345-349.
- Roos A, Faure S, Lochner C, Vythilingum B, Stein DJ (2013) Predictors of distress and anxiety during pregnancy. Afr J Psychiatry (Johannesbg) 16: 118-122.