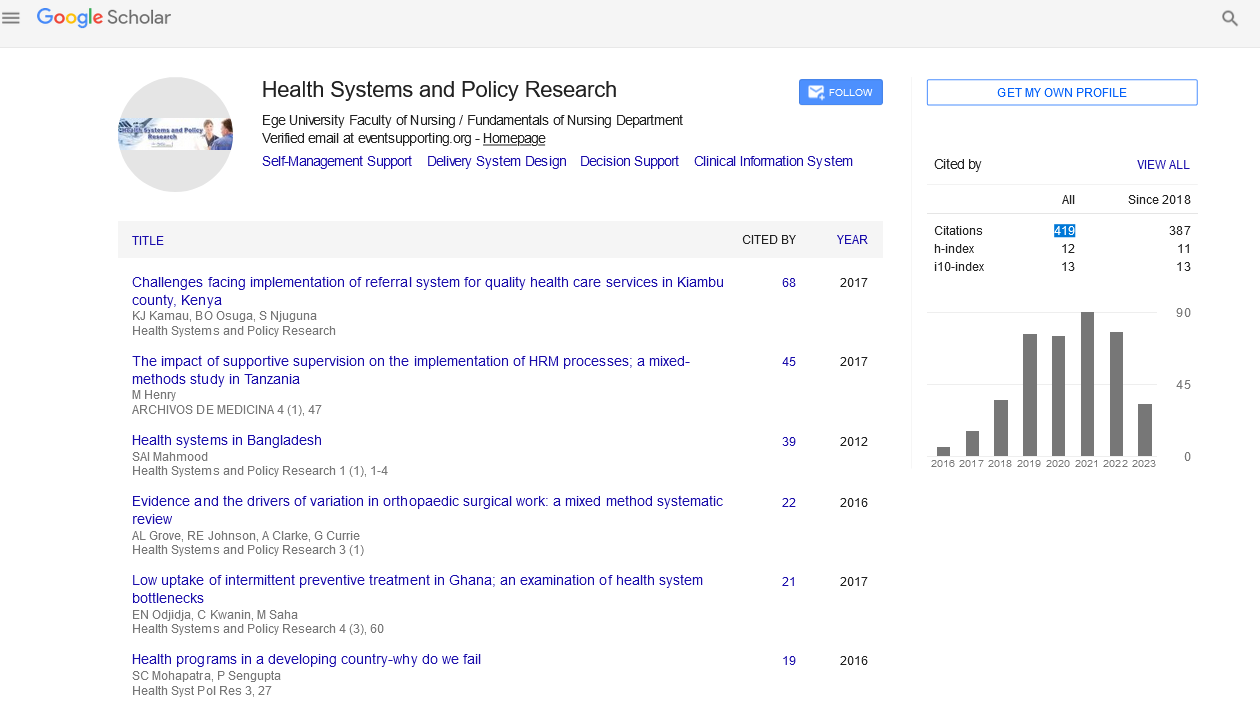
Editorial - (2022) Volume 9, Issue 11
Public Health Ethics and Risk Communication in a Pandemic by Health Policy
Mark Krutzinna*
Department of Medicine, University of Geneva, University of Geneva, Switzerland
*Correspondence:
Mark Krutzinna, Department of Medicine, University of Geneva, University of Geneva,
Switzerland,
Email:
Received: 03-Nov-2022, Manuscript No. Iphspr- 22-13247;
Editor assigned: 07-Nov-2022, Pre QC No. Iphspr-22-13247;
Reviewed: 18-Nov-2022, QC No. Iphspr-22-13247;
Revised: 24-Nov-2022, Manuscript No. Iphspr- 22-13247 (R);
Published:
30-Nov-2022, DOI: 10.36648/2254- 9137.22.9.157
Abstract
Risk reduction during emergencies and epidemics depends on effectively communicating public health advice, and ethical communication advice places a strong emphasis on being completely open. However, communicating during the epidemic has occasionally been difficult, in part because being transparent can be difficult from a practical and conceptual standpoint. When scientific understanding of COVID-19 was changing and there was hesitation to accept that concerns about resource limitation were impacting public health recommendations, a unique dilemma arose.
Keywords: Risk communication; COVID-19; Pandemic; Transparency; Precautionary principle; Infection prevention and control
INTRODUCTION
The ethical difficulties of creating and disseminating public health advice under the dual circumstances of uncertainty and resource scarcity are shown in this article using the example of delivering public health counsel on masking in the United States [1]. The precautionary principle and harm reduction must be balanced under these circumstances, two essential ethical concepts in public health. Risk communication, but maximising openness necessitates taking into account extra ethical principles when creating and putting into practise risk communication techniques [2]. During an infectious disease outbreak, public acceptance of risk mitigation strategies is influenced by a number of variables, including perceptions of risk severity and vulnerability, the veracity, credibility, and dependability of messengers, feelings of self-efficacy, and community attitudes and norms [3]. Public health professionals' communications may have an impact on all of them, making it one of the most crucial strategies for reducing risk during an outbreak [4]. Over the duration of the coronavirus disease pandemic in the United States, communication attempts have been characterised by confusing messaging, public bewilderment, party politics, and accusations of ineptitude or even malice on the side of public officials [5]. It resulted in a less than ideal public adoption of straightforward remedies like face coverings, physical segregation, and immunisation [6]. Public health officials have frequently been criticised for failing to uphold the fundamental ethical principle of openness in their communications [7]. To be fair, though, maintaining transparency during the epidemic has been quite difficult. Particularly, some of the most confused messages have developed in part as a result of public health professionals' reluctance to admit that their recommendations were impacted by both shaky evidence and a lack of resources. In this essay, we look at how risk mitigation methods for public health, which are closely related to swift-moving public health emergencies, are designed and communicated. We provide the design and dissemination of masking advice as an example [8].
Discussion
The US from February to July 2020 to highlight the moral dilemmas authorities face when attempting to communicate honestly public health guidelines in the context of both changing research and resource constraints policy backing 6 By promoting "threat dismissal," media that promotes these arguments and downplays risks to population health outcomes might further postpone preventative behaviour. The United States was not the only country with this dynamic [9]. Even longer was required for the World Health Organization to modify its masking advice [10]. By the beginning of summer 2020, several research had generated strong proof of viral transmission by smaller and bigger respiratory particles. 239 scientists from 32 nations demanded that WHO update its guidelines in a July 2020 open letter to reflect the aerosol transmission of SARS-CoV-2 and modify protective measure recommendations accordingly. The experts advised widespread use of N95 respirators and stricter ventilation regulations for interior locations, notably in hospital settings. Messaging that was disjointed, incoherent, opaque, or even false had several negative effects. The people developed a growing mistrust of reliable specialists. Uncertainty in research, which is normal in the presence of a novel disease, started to be perceived as representing poor science. Arguments for and against different mitigation techniques have occasionally ignored statistics entirely in favour of ideals, pitting individual freedom and rights against concern for the whole. Due to behaviours that allowed the virus to spread quickly and result in many more deaths, emotional reactions to the risk of sickness and to these value inequalities were to blame.
Conclusion
Centers for Disease Control and Prevention Only health professionals and people with COVID-19 symptoms should use masks, according to the Centers for Disease Control and Prevention. Population health officials chose to continue spreading the message that masks are not required for the general public and may even be ineffective by the time evidence on masking for the general public was complete but had begun to point toward advantages. This strategy was driven by concerns that the public would panic buy medical-grade masks, which might exacerbate the existing serious shortages of respirators masks in healthcare settings if done with sufficient training and fit testing. In brief, despite mounting evidence that using surgical masks or respirators often was the best way to prevent catching the virus and transmitting it, limited mask supply rendered advising the public to wear them impractical and perhaps dangerous.
Acknowledgement
None
Conflict of Interest
None
REFERENCES
- Abbott A (2021) COVID’s mental-health toll: How scientists are tracking a surge in depression. Nature 590: 194-195.
Indexed at, Crossref, Google Scholar
- Baniamin HM, Rahman M, Hasan MT (2020) The COVID-19 pandemic: Why are some countries coping more successfully than others? Asia Pac J Public Adm 42: 153-169.
Crossref, Google Scholar
- Buchman DZ, Ho A, Goldberg DS (2017) Investigating trust, expertise, and epistemic injustice in chronic pain. JBI 14: 31-42.
Indexed at, Crossref, Google Scholar
- Camporesi S, Vaccarella M, Davis M (2017) Investigating public trust in expert knowledge: Narrative, ethics, and engagement. JBI 214: 23-30.
Indexed at, Crossref, Google Scholar
- Chernozhukov V, Kasahara H, Schrimpf P (2021) Causal impact of masks, policies, behavior on early COVID-19 pandemic in the U.S. J Econom 220: 23-62.
Indexed at, Crossref, Google Scholar
- Chu DK, Akl EA, Duda S (2020) Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: A systematic review and meta-analysis. The Lancet 395: 1973-1987.
Indexed at, Crossref, Google Scholar
- Czypionka T, Greenhalgh D, Bassler, MB Bryant (2020) Masks and face coverings for the lay public: A narrative update. Ann Intern Med.
Indexed at
- Day M (2020) Covid-19: Identifying and isolating asymptomatic people helped eliminate virus in Italian village. BMJ 368: m1165.
Indexed at, Crossref, Google Scholar
- Esposito S, Principi CC, Leung GB, Migliori (2020) Universal use of face masks for success against COVID-19: Evidence and implications for prevention policies. Eur Respir J.
Indexed at
- Freimuth VS, Musa D, Hilyard K, Quinn SC, Kim K, et al. (2014) Trust during the early stages of the 2009 H1N1 pandemic. J Health Commun 19: 321-339.
Indexed at, Crossref, Google Scholar
Citation: Krutzinna M (2021) Public Health
Ethics and Risk Communication in a
Pandemic by Health Policy. Health Sys Policy
Res, Vol.9 No. 11: 157.