Case Report - (2022) Volume 13, Issue 1
Pyogenic - Cerebral (Brain) Abscess
Tshetiz Dahal1*,
Sumit Bhardwaj2 and
Puzan Sharma3
1General Physician, Lugansk State Medical University, Ukraine
2Department of Oral and Maxillofacial Surgery with Plastic and Regenerative Head and Neck Surgery, Ukraine Medical and Stomatological Academy, Ukraine
3GDMO - Department of I/C Emergency and Emergency, Sir Thutob Namgyal Memorial Multi-speciality Hospital, Sikkim, India
*Correspondence:
Tshetiz Dahal, General Physician, Lugansk State Medical University,
Ukraine,
Tel: +918617009714, +380506266617,
Email:
Received: 12-Jan-2022, Manuscript No. ipjnn-22-12307;
Editor assigned: 14-Jan-2022, Pre QC No. P-12307;
Reviewed: 21-Jan-2022, QC No. Q-12307;
Revised: 24-Jan-2022, Manuscript No. R-12307;
Published:
31-Jan-2022
Abstract
Abscesses in the brain have been one of the most challenging wounds, both for surgeons and trainees. It is a packet full of pus of infected material in the part of the brain. It is an important neurological disease and can produce deadly diseases. Since the beginning of the era of Computed Tomography (CT), the diagnosis and treatment of these organizations has become simpler and less invasive. The results have been improved with the development of diagnostic techniques, neurosurgery, and comprehensive antibiotics. Rare bacterial abscesses are usually caused by the use of chemicals in oncology, longevity in patients infected with Human Immunodeficiency Virus (HIV), and immunosuppression associated with organ transplants. Surgical treatment options did not show significant differences in mortality rates, but lower rates of illness were achieved with a stereo-guided curiosity. Eager stereo-directed antidepressant, antibiotic-based treatment based on the effects of culture culture, and repeated desires expressed in the results of periodic CT scans appear to be the most appropriate treatment for brain tumors. Immunosuppression and comorbidities, early neurological conditions, and intraventricular fractures were important factors influencing patient outcomes. Traps and mutations in the diagnosis and treatment of brain tumors have been discussed in this study.
Keywords
Abscess; Abscess in brain; Effect; Stereotaxy; Treatments
Abbreviations
ADC: Diffusion Coefficient; CHD: Congenital Heart Disease; CNS:
Central Nervous System, CSF: Cerebrospinal Fluid; DW: Diffusion Weighted
Introduction
In 1893, Surgeons reported only 1 death in 19 patients with brain
tumors. Unfortunately, until the advent of the CT method, the
results in patients with brain tumors were not as satisfactory as
in the Macewen series [1].
The use of CT and MR imaging, the emergence of microbiological
diagnostic techniques, and the production of comprehensive
antibiotics have improved the results over the past 20-25 years.
Regular use of CT scans has facilitated the detection of tumors in
the brain and makes patient follow-up safe [2]. The mortality rate
drops from 22.7-45% to 0-20% after regular use of CT scans. Prior
to the advent of CT scans, brain tumors were more commonly
diagnosed and removed completely. However, simpler and
more secure diagnostic techniques make stereotactic aspiration
a viable treatment option, especially for large and non-cortical
ulcers. Also, in some cases CT scan makes safe and effective
treatment without surgical intervention [3]. However, there is no consensus on the treatment of tumor in the brain; the need for
surgical intervention and the nature of the surgical procedure is
still in doubt.
The origin of abscesses
Cerebral abscess occurs in patients with the following
predominant conditions:
1) Conjunctival pus (for example, anterior sinus infection
leading to the anterior cruciate ligament, sphenoid sinus
infection leading to enlargement of the cavernous sinus,
and an infection of the middle ear/mastoid air cell leading
to the temporal lobe and spinal cord).
2) Hematogenous or metastatic spread (e.g., lung and
arteriovenous shunts, congenital heart disease and
endocarditis, dental diseases, and gastrointestinal
diseases).
3) Headaches.
4) Neurosurgical procedure.
5) Immunosuppression.
According to previous literature, the most common cause of
boils in the brain was direct transmission from the middle ear,
meninges, mastoid infections and the paranasal sinus. Prior to
the 1980s, CHD (6–50%) and sinus/otitis infections appeared to
be the most common symptoms in brain tumors and in children
[4]. The advent of diagnostic techniques, antimicrobial agents,
and advances in cardiovascular surgery have led to a decrease
in the number of tumors in the brain due to CHD and sinus/otitis
infections and an increase in ulcers in patients receiving immuno
suppressive therapy as a result of reconstructive procedures, in
patients. HIV-positive people who have been living longer, and
those who are receiving chemotherapy for cancer treatment.
Many abscesses appeared in the 1980's in infants and patients
with depressive disorders, and they were diagnosed early, (6
months).
Nowadays, hematogenous or metastatic proliferation has become
a very common factor in brain tumor formation. Organisms that
cause tumors in the brain are usually derived from bacteria.
Pepto-streptococcus and Streptococcus spp (especially S.
viridans and microaerophilic organisms) are more common in
patients with coronary heart disease (cyanotic heart disease)
and shunt bypasses from right to left without the usual filtration
of pulmonary vascular tissue. In CHD, decreased arterial oxygen
uptake and increased blood viscosity may cause focal cerebral
ischemia and serve as a nidus for many diseases, especially in
the combination of gray matter and white matter, usually in the
spread of MCA. CHD has sometimes been an important cause of
childhood ulcers, but there has been a decline in these cases due
to advances in heart surgery and the use of broad-spectrum anti
antiretroviral drugs.
Bactericidal, Pepto streptococcus, and Streptococcus spp are
often identified in brain tumors caused by a combined spread.
This spread is the result of osteo myelitisin the surrounding air
sinus. The risk of developing cerebral palsy in an adult with active
otitis media is ~ 1/10,000 per year, but in a 30-year-old patient
with active infection, the life-threatening risk is ~ 1/200.
Streptococcus, S. aureus, Pseudomonas, and Bacteroides spp
are more common in lung diseases (lung abscess, empyema,
bronchiectasis). They are most common in the distribution of
MCAs and are often repetitive.
Staphylococcus, Streptococcus, Clostridium, and Enterobacter spp
are more common in patients with open-headed trauma. Shoot
wounds, open skull openings and external bodies in the brain
parenchyma, and fractures of the skull with CSF fistula cause
abscesses in the brain, often associated with traumatic brain
injury [5].
Staphylococcus and Streptococcus spp are identified as inpatients
who have previous neurosurgery procedures. Wounds in the
opening hours are less likely to be infected. Additional risk
factors include implantation of an external body such as a shunt
or external ventricular drain, advanced gliomas, and premature
radiation exposure after surgical procedures.
Fungal infections
Toxoplasma, Staphylococcus, Streptococcus, and Pseudomonas spp are identified in non-immune patients who are infected with
HIV, organ transplants, chemotherapy, or steroid use. Branchinfected
fungal infections (e.g., aspergillosis) block large and
medium-sized vessels, resulting in cerebral arterial thrombosis
and infarction. Sterile infarcts can be converted into septic infarcts
by a tumor-related structure. Abscesses can also be caused by
a joint spread. These lesions are most commonly found in the
posterior fossa and lobe of the brain. The mortality rate due to
fungal tumors ranges from 75 to 100%, despite strong treatment
with amphotericin.
It still has a strong representation of anaerobes (30-50%) in
patients with brain tumors. Additionally, atypical bacteria such as Nocardia and Actinomyces spp may appear in affected patients.
Although positive civilization rates have reached 100% in studies
of careful management of clinical models, adverse cultural events
remain as high as 15-30% in most series, especially in patients
where antimicrobial treatment is initiated before surgery.
Polymerase chain reaction analysis of S recombinant DNA and
sequence may identify viruses at the level of species from tumors
in the brain. This method is fast and useful especially in identifying
slow-growing and fast-moving organisms.
Lumbar puncture has been considered dangerous for patients
with a brain tumor. It is usually caused by strong suspicion of
concomitant meningitis and/or ventriculitis, and reveals only 10-
30% of positive CSF cultures in which organisms such as those
implanted in the gut are found. Although a large portion of the
deaths were thought to be caused by lumbar piercing during the
onset of labor, recent studies in which multivariate modifications
were used have failed to reveal such a risk. Therefore, lumbar
piercing may be recommended in patients with brain tumors
where there is no increase in intracranial pressure and with clear
signs of meningitis and/or ventriculitis.
Pathogenesis of brain abscesses
Abscesses in the brain develop as a result of parenchymal
infection by pyogenic bacteria, starting as a local cerebritis
and transforming into a strong wound surrounded by a wellvascularized
fibrotic capsule. Brain tumors in humans have been
based on diagnostic findings during CT scans or MR imaging
sessions.
The first stage or early cerebritis occurs from Day 1 to 3 and is
characterized by the accumulation of neutrophil, tissue necrosis,
edema. Microglial and astrocyte activity is seen in this phase
and continues throughout the development of the tumor. The
intermediate phase, or late cerebritis, occurs in Days 4 to 9 and is
associated with macrophage infiltration and lymphocyte.
The final or capsule stage occurs from Day 10 onwards and is
associated with the formation of a well-developed vascular wall,
which actually closes the wound and protects the normal brain
parenchyma from further damage. The capsule formation is
usually early from 10 to 13 days and is usually thin on the medial
or ventricular side of the abscess and usually ruptures in this way.
After Day 14, late capsule formation develops, with gliotic,
collagenous and granulation layers. In addition to reducing the
rate of infection, the immune response that is an important
part of tumor formation also destroys surrounding normal brain
tissue. This support is found in experimental models, in which
harmful areas are exaggerated in comparison to the natural
environment for bacterial growth, which is reminiscent of an
overactive immune response. of brain tissue, which often spreads
beyond the initial focus of infection. Therefore, controlling the
intensity and/or duration of the antibacterial immune response
in the brain may allow for effective elimination of bacteria while
minimizing damage to the surrounding brain tissue.
As mentioned earlier, injury sites in both experimental models
and tumors of the human brain are exaggerated in comparison
to the natural environment of viral growth, the eminiscent
of the most effective immune response. Reporting on the
extended region of affected tissue involvement associated with
brain tumors compared with the condition focused on initial
shock, Kielian suggested that the production of inflammatory
mediators following S. aureus infection continue, effectively
increasing damage to the normal surrounding brain parenchyma.
Specifically, the continuous release of pro-inflammatory
mediators by activated glia and internal immune cells may work
through a constructive response loop to enhance the recruitment
and utilization of newly recruited inflammatory cells and glia. This
will effectively promote the antibacterial inflammatory response
through a vicious pathological circle culminating in extensive
collateral damage to normal brain tissue.
Recent research supports the ongoing immune function
associated with experimental tumors, in which high levels of
interleukin-1b, tumor necrosis factor – a, and macrophage
inflammatory protein – 2 were detected between 14 and 21
days after exposure to S. aureus. In line with the long-term
inflammatory mediator, TS aureus infection was found to cause
chronic disruption of the blood-brain barrier, which is associated
with the continued presence of peripheral immune cells and
glial function. Overall, these findings suggest that interventions
with anti-inflammatory compounds following adequate bacterial
neutrality may be an effective strategy to reduce damage to
the surrounding cerebral parenchyma during brain tumor
development, leading to improved cognitive and sensory effects.
R microglia and microcyte-microglia responses in S. aureus is
defined in terms of the burning mediator's expression, and
is generally found to be of the same quality as those detected
after lipopolysaccharide exposure. Although studies containing
basic microglia and astrocytes from Toll-like receptor knockout
mice reveal an important role for this receptor in regulating
S-dependent activity. Aureus, it is clear that additional receptors
are also involved in the inglial response to this virus is surprising
because these pathogens have the potential to have harmful
effects on tissues such as the CNS, which have limited ability to
regenerate.
The effects of glial cell function on brain tumor
context are almost numerous:
1. First, parenchymal microglia and astrocytes may
be involved in the initial recruitment of specialized bactericidal phagocytes in the CNS by their expression of
inflammatory chemokines and cytokines.
2. Second, microglia exhibit bactericidal activity of S. aureus
in vitro, suggesting that they may also be involved in the
initial inhibition of viral replication in the CNS. However,
their bactericidal in vitro activity does not compare with
that of neutrophils or macrophages, suggesting that this
activity may not be a major mechanism of microglia effect
of severe infection.
3. Third, activated microglia have the potential to influence
the type and level of antibacterial adaptive immune
reaction through its phase II complex administration of
the histo-compatibility complex and exposure to the
costimulatory molecule. Finally, if glial activity persists
in the context of progressive inflammation, continuous
release of inflammatory mediators can damage the
normal brain parenchyma.
Clinical Presentation
There are no pathogenic clinical symptoms; most patients with
clinical symptoms depending on the location or major impact
of the lesion: headache, nausea, urination, fever, dizziness,
fainting, and muscle spasms are the most common symptoms.
These symptoms develop rapidly, however about tumor lesions.
The flu is less pronounced, and only 30-55% of patients with
the flu are 38.5ºC. Capture is a symptomatic mark in 16-50% of
patients. Focused neurological loss is seen in 40-60% of patients,
depending on the location of the lesion. Papilledema is not
available to patients, who are 2 years old. Patent sutures with
low ability to limit infection and cranial enlargement are possible.
However, three symptoms of brain tumor (headache, fever, and
neurological deficits) can only be seen in 15-30% of patients.
Paralysis, muscle weakness, and many different symptoms may
be present and degeneration is often very rapid.
Diagnosis
The photographic features of the tumor in the brain depend
on the stage at the time of photography and the source of the
infection.
The development of an abscess in the brain can be divided into
4 stages:
1) Early cerebritis (1-4 days)
2) Late cerebritis (4-10 days)
3) Formation of the first capsule (11-14 days) and
4) Capsule formation late (14 days).
Most abscesses show a lot of surrounding edema, which
usually occurs during late cerebritis or the first stage of capsule
formation, which follows a major effect. Blood clots, which can
be seen in the form of endocarditis, cardiac shunts, or paralysis
of the pulmonary vascular malformations, usually numerous,
are identified at the junction of gray and white, and are found
in the MCA area. In the earlier stages, a CT scan was performed
without the addition of brightness can only show low comfort
with great effect. In the later stages, a complete peripheral ring may appear. For CT scans obtained after the administration of
different materials, the development of the same ring remains
in the later stages. In the early stages the capsule will be difficult
to visualize using conventional techniques, and double-sided CT
therapy is often helpful in interpreting tumor closure. Metastatic
tumors, advanced gliomas, cerebral infarction, cerebral palsy or
hematoma, lymphoma, toxoplasmosis, debilitating disease, and
radiation necrosis should be remembered as a separate diagnosis
of brain tumors that appear as enlarging lesions ring.
Techniques in neuro radiology have simplified the diagnosis of
multiple brain tumors. The incidence of multiple abscesses in the
brain, which is reported to be 1.8-17% of patients
The pre-CT period, 23–50% in modern cases. The findings of MR
imaging also depend on the stage of infection. In the first stage,
lesions exposed to MR images may have a low T1-weighted signal
and a high signal in T2-weighted, enhanced and scarred images.
, with a high signal in T2-weighted images, both in the pit and
surrounding parenchyma. The abscess shows hyper-intense
rim in T1-weighted images obtained indistinctly and a strong
rim in T2. As-based images in CT scanning, imaging MRI usually
show a developmental ring around the abscess. The abscesses
usually grow to a white matter, away from the gray-vascularized
gray matter, as well as narrowing of the middle wall. However,
the mark of the developing ring is not specified and should be
examined in the context of clinical history. The size, inconsistency,
and stiffness of the developing ring elevate the tumor (most
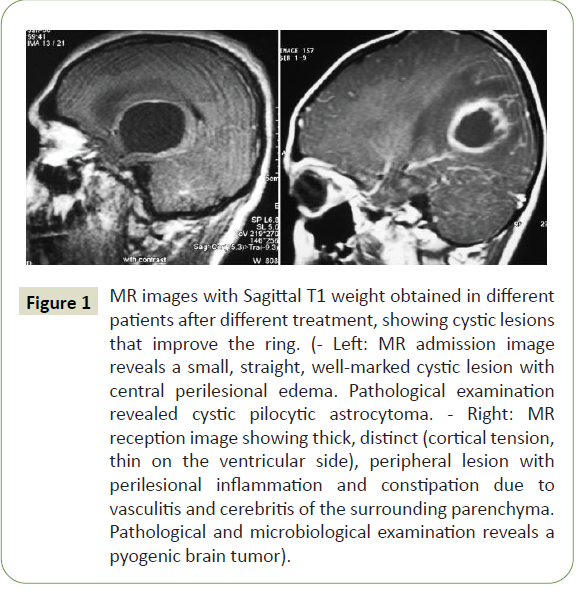
cases), or possible fungal infection (Figure 1).
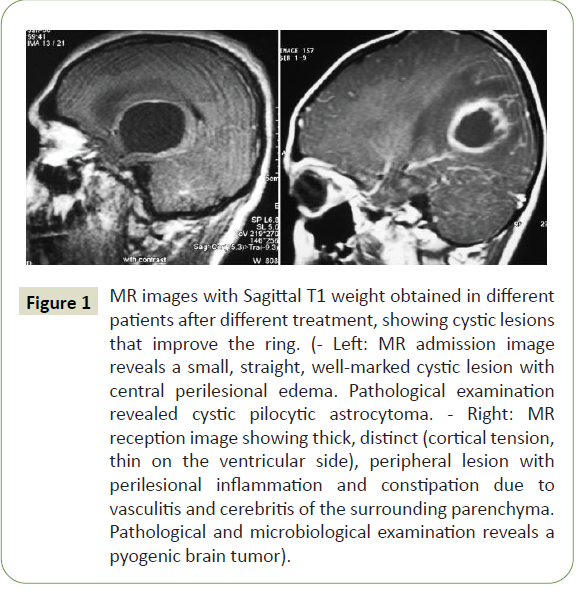
Figure 1: MR images with Sagittal T1 weight obtained in different patients after different treatment, showing cystic lesions that improve the ring. (- Left: MR admission image reveals a small, straight, well-marked cystic lesion with central perilesional edema. Pathological examination revealed cystic pilocytic astrocytoma. - Right: MR reception image showing thick, distinct (cortical tension, thin on the ventricular side), peripheral lesion with perilesional inflammation and constipation due to vasculitis and cerebritis of the surrounding parenchyma. Pathological and microbiological examination reveals a pyogenic brain tumor).
In DW images, limited streaming (bright signal) may be visible;
this helps to separate tumors from necrotic neoplasms, which are
usually not prevented, although not all tumors follow this rule.
Fungal abscesses and tuberculosis may increase the distribution
and low signal in DW thinking.
Numerous studies show the benefits of DW imaging in
distinguishing between necrotic or cystic ulcers and brain tumor
ADC. Initially, DW hypotheses were thought to be helpful in
differentiating toxoplasmosis and lymphoma. In a study ADC limit
of 0.8 was proposed, where ADC values, 0.8 may favor lymphoma
over toxoplasmosis; However, that study showed a significant
increase in ADC values in toxoplasmosis and lymphoma. As the
author concluded that in most patients, ADC values are not clear
in making a distinction between toxoplasmosis and lymphoma.
However, DW imaging has a high sensitivity to the detection of
rapid ischemic changes in the cortical and deep white matter that
can occur in cases of infectious vasculitis. The tumor hole in the
brain shows regions of increased levels of partial anisotropy, which
have a relative variability compared to other cystic intracranial
lesions. This information may prevent misinterpretation of
diffusion tensor image information as abnormal mass of white
matter fiber associated with large lesions. Intracerebral tumors
are characterized by certain resonances in MR spectroscopy that
are not detected in a sterile human tissue. MR spectroscopy
modality has been shown to be particularly useful in distinguishing
between brain tumors and other cystic ulcers, information that
can be used to speed up the implementation of appropriate
antimicrobial treatment. Metabolic substances, such as succinate
(2.4ppm), acetate (1.9 ppm), alanine (1.5 ppm), amino acids (0.9 ppm), and lactate (1.3 ppm), may all be present. in bacterial
tumors that can be treated or immediately after initiation for
treatment.
Treatment
There are 3 treatment options for brain tumors:
1. Medical
2. Respiration (freehand, stereotactically or neuro
endoscopically guided).
3. Total cut
In choosing the appropriate treatment option, the following
factors should be considered: Karnofsky performance measure;
primary infection; predisposing condition; and number, size,
location, and stage of the tumor. Modern treatments for brain
tumors often include a combined surgical and therapeutic
approach.
Medical management
Antibiotics play a key role in regulating abscesses in the brain. The
agent's characteristics (such as brain infiltration) and previous
use of intrathecal or interstitial treatment should be known
prior to treatment. Choosing the right antibiotic, microorganism
or underlying disease should be identified. If the patient is not
in sepsis or in a critical situation, antibiotic treatment should
be postponed until cultural factors are identified. We have
reported eight times the number of invasive cultures in patients
receiving antibiotics before surgery. The author reported that
intra-cerebral material cultures remain infertile (34%) of their
surgical patients. Of the 76 patients whose culture was infected,
(89%) identified one virus and (11%) viruses were detected. If a
predisposing condition is spread with hematogenous or patients
have symptoms of systemic infection, blood tests may be helpful in identifying the microorganism. After performing blood tests
on 49 of the 122 patients who had a clinical presentation of
systemic infection (fever and leukocytosis). Only 13 of those
patients had blood clots that raised viruses (positive rate, 26.5%);
Seven of them had the same pathogen in both cultures of the
blood and brain tumors. Blood test is a very small, inexpensive,
and quick way to detect a pathogenic microorganism. Despite
the low levels of positive findings, blood tests should be taken
from every patient who is suspected of having a brain tumor and
who has symptoms of systemic infection. Only medical treatment
can be considered if patients are poor partners of surgical
intervention in the following terms: if the lesions are numerous;
1.5 cm wide; found in clever places; or if there are concomitant
diseases such as meningitis or ependymitis. The most important
objection to empirical treatment without microbiological
identification; another microorganism may cause an abscess. At
least one aspiration procedure can be very helpful in identifying
a microorganism, if the patient does not have coagulopathy.
Treatment alone is most effective if treatment is started during
cerebritis, if the wound is 1.5 cm wide, if the duration of symptoms
is 2 weeks, and if the patient shows improvement in the first
week. Systemic antibiotics have been given for 6 weeks, although
some institutions now offer 2 weeks of intravenous antibiotics
followed by up to 4 weeks of oral antimicrobial treatment. If the
microorganism is undetectable, 6-8 weeks of intensive treatment
may be required.
Despite appropriate treatment, a 5-10% recurrence rate has been
reported in brain tumors, which can be caused by discontinuation
of treatment early. I reported a series in which the duration of
antibiotic treatment was not based on a specific time but rather
on the levels of C-reactive protein levels. In addition, high levels
of C-reactive protein can be used in differentiating the tumor
of the brain from other lesions that improve the ring. Three of
the 26 patients had been elevated C-reactive protein levels
and were found to have recurrent abscesses. It did not happen
again in patients their levels returned to normal. Antibiotics and
hyperbaric oxygen therapy were given for a total of 4 weeks in
13 patients, even in patients who did not have a bacteriological
diagnosis. Overall, the first operation failed in 2 patients (15.3%).
Two re-emerging tumors were resuscitated for 6 and 9 days,
respectively, after the initial procedure. However, long-term
radiological tests failed to show recurrence of tumors in any of
these conditions after a 9.5-month follow-up period. The main
difference between their research and other reported cases in
the reduced duration of antibiotic treatment.
Discussion
Nowadays, with easy radiological monitoring of brain tumors and
extensive antibiotics, doctors often choose treatment, especially
if the pathogen can be detected based on blood culture, CSF, or
specific desire. It was reported in 56 patients who were randomly
selected for treatment, anticipation, or surgery for their brain
tumor and found no statistically significant difference. In fact,
boils in the brain cause significant physical stress in patients, and
surgical stress should not be added if necessary. Corticosteroids
can be used, but they have side effects, and their use in the
treatment of vasogenic edema due to an abscess on the brain is still debated [6]. The adverse effect of dexamethasone on capsule
formation has been demonstrated in experimental studies and
made similar comments about the effect of corticosteroids.
However, it is reported that corticosteroids do not inhibit capsule
formation, and that they only act as reversible forces. Mampalam
and Rosenblum reported high mortality rates in patients treated
with corticosteroids, but these patients were in a critical state
at first and had decreased levels of awareness. These authors
recommend the use of corticosteroid in patients with significant
perilesional edema that was radiologically diagnosed and
reported in a previous study of 26 patients who showed no
adverse effect on the effect when corticosteroids were used in
patients with intracranial tumors [7]. It should be borne in mind
that steroids may reduce the brightness of the tumor capsule in
the early stages of infection and that this may be a false indication
of radiological development, or it may delay diagnosis [8].
Surgical management
Throughout the history of neurosurgery, treatment of brain
tumors has been challenging. Non-surgical treatment of
suspected small brain tumors with antibiotics has been
recommended. Reasonable control of intracranial mass lesions
requires the establishment of a thorough diagnostic prior to
the initiation of therapeutic measures [9]. Indeed, patients
presenting with progressive progressive neurological deficits
resulting in a significant neuro-radiologically verified brain tumor
by neuro radiologically verified decompression, both by surgeons
and internists. Different types of surgical procedures have been
used in the treatment of brain tumors.
The choice of procedure has been the subject of much debate.
Craniotomy, previously promoted in the past when no antibiotics
or CT scanning was available, is no longer used. Breathing,
repeated as needed or by draining water, has replaced the
exhaustion efforts completely.
However, an open surgery procedure is still preferred to treat brain
tumor with a combination of treatment and surgical removal, in
the following cases: if there is evidence of increased intracranial
pressure due to a major brain tumor effect; there is difficulty in
diagnosis; if the abscess is the result of traumatic injury presented
by foreign objects; if the wound is located in the posterior fossa;
and if there is any consideration of fungal infection. Even stress
with Craniotomy or Craniectomy will be helpful for patients with
a serious emotional condition.
Because diagnoses based solely on clinical radiological and
neuro-radiological findings may be erroneous, non-surgical
treatment decisions should not be made without a thorough
pathogen diagnosis. Control of the brain stereo strategy in
the brain, which allows for both diagnostic and therapeutic
confirmation of the desired wound content and identification of
the traumatic organism, has expanded since the introduction of
CT-guided stereotaxy [10]. A recent review of the literature shows
a series of tumors in the brain treated primarily with stereotactic
techniques and a review of their 11-patient series, concluding
that stereotactic cravings should be considered as an alternative
treatment for all but the most external and major and related
tumors. failure of stereotactic treatment of tumors in a series of 29 cases, due to insufficient appetite, lack of catheter drainage,
prolonged immunosuppression, or lack of antibiotic treatment.
It was therefore reported that 4 patients with brain tumors
underwent surgery using a free-neuro endoscopic method with
freehand stereotaxy. They breathe in pus and clean the hole
with antibiotics. The author reported their self-awareness with a
flexible scooter (free-directed or natural-directed), while choosing
the strongest in the children’s series [11]. It has now reported the
usefulness of flexible endoscopes for certain important surgical
procedures, such as wishing and examining the tumor in all local
directions or dealing with a strong and elastic membrane that
requires scissors or other implants. It is now maintained that
drainage catheters do not need to be inserted into the tumor
after endoscopy (to be used to give him antibiotics and the desire
continues within the next few days), while others are reported
to place catheters in all cases but avoid drain implants in only
one patient, and not a moment. Surgery was needed because no
tumors were left with the effect of replacement; on the contrary,
they underwent subsequent surgery on their 4 patients. There
are reports that no significant differences can be found in the
length of hospital stay, the number of postoperative CT scans,
and the duration of antibiotic treatment between traditional and
endoscopic stereotactically guided aspiration. Internal sampling
of abscess material operations and smear arrangements for
microscopic analysis and biological detection of tumors is fraught
with pitfalls.
First, tumor-related necrosis should be separated from tumor
necrosis. Small or large areas of coagulation necrosis are often
seen in glioblastomas [12]. Sometimes the necrotic site of a
tumor is replaced by a large infiltration of a polymorphonuclear
leukocyte that transforms the necrotic area into a liquefactive,
resulting in a misdiagnosis of brain tumor. On the other hand,
perilesional gliosis of the abscess may be marked to mimic lowgrade
astrocytoma. Although in the non-neoplastic proliferation
of active astrocytes cellular cells are usually low and individual
cells are very common, they are rarely associated with cellular
domains especially of the growing astrocytes with pleomorphic
and hyper chromatic nuclei. Brain tumors were thus classified as
cerebritis (StageI) when polymorphonuclear leukocyte deficiency
and perivascular erythrocyte were recovered and encapsulation
(StageII) in frank pus, a polymorphonuclear leukocyte.
Constipation, necrosis, granulation tissue, and active active
gliosis were detected; this provided a better understanding
and simplification of pathological features as well as effective
pathological-radiological communication [13].
On the other hand, advanced neuro radiological methods can
be used in different diagnoses of these lesions. In deep, multisite
lesions, and near the ventricle wall, a reduction of 1 mm
between the ventricle and brain tumors will increase the rate
of fracture by 10%. Although a combination of intra-cal and
intravenous antimicrobial therapy has been recommended for
intraventricular rupture, treatment strategies in this specialized
group of patients remain controversial. Alternative therapies
have been recommended, including the following:
Emergency craniotomy with immediate removal of the abscess; Emergency evacuation with washing of the ventricles and
placement of ventriculostomy accompanied by administration of
intraventricular antibiotics;
A 5-step treatment regimen, including open-ventilated
craniotomy, ventricular detoxification, intravenous administration
of antibiotics for 6 weeks, intraventricular administration of
gentamicin twice daily for 6 weeks, and intraventricular drainage
for 6 weeks.
Conclusion
The mortality rate ranged from 40 to 60% in the pre-CT period
and decreased to 10% from the beginning of the CT period to
2000. After 2000, the mortality rate was reported to be between
17 and 32%. Mainly due to the major changes in epidemiology
occurring today.
Compared to previous reports, the incidence of brain tumors
caused by sinus/otitis infection has decreased, while those
associated with a deficiency of immune system have increased
significantly. It is a challenge to treat patients who are receiving
cancer chemotherapy or immuno-suppressive therapy for organ
transplants, or who are infected with HIV. The author reported
a 2.8-fold increased risk of adverse outcomes in patients with
immuno-suppressive immunity. Other comorbidities such as
diabetes mellitus or cirrhosis are also factors that have a negative
effect on the outcome. Worst predictions were reported in
patients presenting with low Glasgow Coma Scale scores. Than
reported that (62%) of the 21 patients with the first figures for
the Glasgow Coma Scale, 9 either died or fell into a vegetarian
state. Intraventricular rupture is a traumatic and often fatal
complication of a brain tumor and is associated with a high
mortality rate.
Deaths were reported in (84.5%) of 129 patients in a literature
review between 1950 and 1993. In another recent study from
Japan, the overall mortality rate was 38.7% (12 of 31 patients).
A series of 62 patients there (48%) had adverse effects (severe
disability, vegetative status, and death) due to intraventricular
rupture of brain abscess. The patient's neurological pre-treatment
condition is an independent factor with a significant effect
associated with the outcome. It is rare for survivors to experience
neurological sequelae that include hemiparesis, epilepsy, and
psychiatric disorders. Abduction is a long-term risk for 30-50% of
patients suffering from brain tumors. The delay time can be up to
5 years, but it is short for older patients. Started immediately and
lasts for at least 1 year due to the high risk of subsequent fainting
in patients with brain tumors [14].
Treatment may be discontinued if no significant epileptogenic
activity can be demonstrated in electroencephalograms [15].
Abscess management is one of the most important factors in
both arousal and nerve effect. It was therefore reported that,
after surgical removal of the abscesses, severe neurological
deficits (5.2% compared to 0%) and fainting (47.7% compared to
31.2%) were observed compared with stereotactic cravings. The
location of the abscess did not contribute to the formation of
fainting. However, the hypodense areas around the tumor cavity were wider in patients treated with surgery. These areas were
thought to be a damaged brain parenchyma that was causing
neurological deficit and epilepsy. Recurrence rates are estimated
at 10-50%. The observation period should be held for at least 1
year. The solution to the surrounding edema and the loss of the developing rim should be recorded at this time, which can take
up to 6 months. In the first 6 weeks. wounds that do not show
a decrease should be sought as well. Surgical treatment may be
recommended for patients with dementia and/or ulcers that
cannot be resolved radiologically.
REFERENCES
- Agarwal AK, Garg R, Simon M (2007) Ring enhancing lesion on CT scan: Metastases or a brain abscess? Emerg Med J 24: 706.
Google Scholar, Crossref
- Alderson PO, Gado MH, Siegel BA (1977) Computerized cranial tomography and radionuclide imaging in the detection of intracranial mass lesions. Semin Nucl Med 7: 161–173.
Google Scholar, Crossref
- Ashdown BC, Tien RD, Felsberg GJ (1994) Aspergillosis of the brain and paranasal sinuses in immuno compromised patients: CT and MR imaging findings. AJR Am J Neuroradiol 162: 155–159.
Google Scholar, Crossref
- Baldwin AC, Kielian T (2004) Persistent immune activation associated with a mouse model of Staphylococcus aureus-induced experimental brain abscess. J Neuroimmunol 151: 24–32.
Google Scholar, Crossref
- Barlas O, Sencer A, Erkan K, Eraksoy H, Sencer S, et al. (1999) Stereotactic surgery in the management of brain abscess. Surg Neurol 52: 404–411.
Google Scholar, Crossref
- Barsoum AH, Lewis HC, Cannillo KL (1981) Nonoperative treatment of multiple brain abscesses. Surg Neurol 16: 283–287.
Google Scholar, Crossref
- Beller AJ, Sahar A, Praiss I (1973) Brain abscess. Review of 89 cases over a period of 30 years. J Neurol Neurosurg Psychiatry 36: 757–768.
- Black P, Graybill JR, Charache P (1973) Penetration of brain abscess by systemically administered antibiotics. J Neurosurg 38: 705–709.
Google Scholar, Crossref
- Black PM, Levine BW, Picard EH, Nirmel K (1983) Asymmetrical hydrocephalus following ventriculitis from rupture of a thalamic abscess. Surg Neurol 19: 524–527.
Google Scholar, Crossref
- Boom WH, Tuazon CU (1985) Successful treatment of multiple brain abscesses with antibiotics alone. Rev Infect Dis 7: 189–199.
Google Scholar, Crossref
- Brewer NS, MacCarty CS, Wellman WE (1975) Brain abscess: a review of recent experience. Ann Intern Med 82: 571–576.
Google Scholar, Crossref
- Britt RH, Enzmann DR, Placone RC Jr, Obana WG, Yeager AS (1984) Experimental anaerobic brain abscess. Computerized tomographic and neuropathological correlations. J Neurosurg 60: 1148– 1159.
Google Scholar, Crossref
- Burtscher IM, Holtås S (1999) In vivo proton MR spectroscopy of untreated and treated brain abscesses. AJNR Am J Neuroradiol 20: 1049–1053.
Google Scholar, Crossref
- Calfee DP, Wispelwey B (2000) Brain abscess. Semin Neurol 20: 353–360.
Google Scholar
- Canale DJ (1996) William Macewen and the treatment of brain abscesses: Revisited after one hundred years. J Neurosurg 84: 133–142.
Google Scholar
Citation: Dahal T, Bhardwaj S, Sharma P (2022) Pyogenic - Cerebral (Brain) Abscess. J Neurol Neurosci Vol.13 No.1:408