Keywords
Disease perception; Quality of life; Patients; Medical institution
Introduction
According to WHO data, chronic noncommunicable diseases have become a global pandemic scale phenomenon as well as the main cause of death [1].
The illness perception is one of the most important characteristics in terms of the impact on the patients’ chronic condition course [2]. Chronic disease leads to mental and social maladaptation of the patient [3]. In patients with chronic diseases, the level of perception of their disease affects the state’s self-control, medication intake, adherence to the regime and changes the quality of life [4].
The quality of life in chronic diseases includes three broad categories - physical, mental, social functioning and it changes being affected by the disease [5].
The effect of patients' illness perceptions on the quality of life has been studied in various diseases. So, Yaraghchia et al. [6] found out that there was a correlation between the disease perception and the quality of life in patients with coronary heart disease after coronary artery bypass grafting. The regression model showed that identity, care during the disease, the ability to recognize the disease and emotions that make up the perception of the disease can predict changes in the quality of life [6].
The relationship between disease perception and quality of life (only with physical functioning, Questionnaire SF-36) has been established in patients with chronic obstructive pulmonary disease [7].
All forms of spinal pathology in the ICD-10 are designated as dorsopathies (M40-M54). The main cause of dorsopathy is spinal osteochondrosis – a chronic dystrophic process manifested by damage to the vertebral bodies, ligament-articular apparatus, intervertebral discs [8].
According to Za?tsev et al. [9], a deterioration in the quality of life correlated with pain syndrome severity and such signs as dissatisfaction, tension, anxiety, rigidity, focus on personal feelings, a negative approach to life, and low stress resistance in patients with spinal osteochondrosis. The psychological characteristics and quality of life depended on the gender and location of vertebral pain syndrome.
The presence of a chronic disease in a patient increases the risk of hospitalization. The study found that a chronic disease in the circulatory system or in the respiratory system increases the risk of hospitalization by 8,72 and 3,01 times, respectively [10].
The hospitalization is a psychological trauma for a patient, since they lose the right to determine the nature and sequence of their daily activity, become dependent on medical personnel. All of that often leads to depression and fear, reduces the treatment results and the quality of life of a patient with a chronic disease [11].
Then hospitalization should improve the chronic diseases management, as patients are examined by a new health care team and observed in a controlled environment [12].
Therefore, the aim of our research was to study the influence of disease perception on the quality of life of hospitalized patients of a therapeutic profile.
Research Design and Methods
Research design
The study was conducted at Orenburg Regional Clinical Hospital ?2 in January 2019. Patients from the Cardiology, Pulmonology and Neurology Departments, respectively, comprised I, II and III groups, 22 patients each. Voluntary informed consent was obtained from all patients participating in the study. The study is observational, analytical, transverse, the sample is convenient. Patients were interviewed before discharge from the hospital, questionnaires were filled out by the patient in the presence of researchers.
That was an exploratory research aimed to develop the hypothesis that the quality of life of patients being treated in a hospital depends on the perception of the disease.
Criteria for inclusion of patients in the study: men and women with a chronic disease aged 20 to 70, with a disease experience of at least 10 years.
Group I was represented by patients with coronary heart disease, Group II - with chronic obstructive pulmonary disease, Group III - with osteochondrosis.
Exclusion criteria
Persons under the age of 20 and older than 80, severe concomitant diseases, serious general condition of the patient, acute diseases, the presence of another chronic disease in the patient, the patient's refusal to participate in the study.
In total, 147 patients were treated in 3 hospital departments. 8.1% (12) of the patients were excluded from the study due to their grave condition; 15% (22) of patients - had other diseases; 32% (47) patients refused to participate in the study. 44.9% (66) patients took part in the study.
Patients who refused to participate in the study explained their refusal with several reasons: the study would not help in treatment; they wanted to be left alone, they did not want to communicate with anyone;
Research methods
To identify the types of disease perception in patients with chronic somatic pathology, PQBI (Personality Questionnaire of Bekhterev Institute) was used [13].
The PQBI Questionnaire is designed to diagnose 12 types of disease perception. The TOBOL Questionnaire includes 12 sets of tables: well-being, mood, sleep and waking up from sleep, appetite and attitude to food, attitude to illness, attitude to treatment, attitude to doctors and medical staff, attitude to relatives and friends, attitude to work (study), attitude to others, attitude to loneliness, attitude to the future. Each set contains from 1 to 17 numbered statements, from which the patient is to choose two most suitable for them. The researcher indicated with a circle the numbers of the choices made in the registration sheet. The time for filling was not limited. The type of disease perception that scored the maximum number of points was diagnosed. If the same number of points scored many types of perception of the disease from different blocks, an undifferentiated (unidentified) type of attitude to the disease was diagnosed.
Conditionally adaptive types; intrapsychically and interpsychically maladaptive, undifferentiated (unidentified) types of disease perception were allocated. Table 1 presents the blocks, types of perception of the disease and their brief description.
Table 1 Blocks, types of attitude to the disease and their characteristics - PQBI (Personality Questionnaire of Bekhterev Institute).
| Blocks of «types of attitude towards the disease» |
Types of Attitude to the Disease |
Characteristics of types of attitude towards the disease |
| Conditionally Adaptive Types |
Harmonious |
An objective assessment of the condition. There is a desire to actively contribute to the treatment success and ease the burdens of caring for their close people. |
| Ergopathic |
Selective attitude to examination and treatment, conditioned upon the desire to continue to work despite the severity of the illness. |
| Anosognosic |
Actively rejecting thinking about the disease, its possible consequences, up to the denial of the obvious things. |
| Intrapsychically maladaptive types |
Disturbing |
Continuous anxiety and suspiciousness regarding the adverse course of the disease, possible complications, inefficiency and even the danger of treatment. |
| Hypochondriac |
Focus on subjective feelings, the desire to constantly talk about them to others; exaggeration of the valid and the statement of non-existent diseases and suffering. |
| Neurasthenic |
Irritation outbreaks, especially with pain, with discomfort, with treatment failures. Intolerance of pain, impatience, inability to wait for relief. |
| Melancholic |
Dejection with the disease, disbelief in recovery, in possible improvement and effect of treatment. |
| Apathetic |
Complete indifference to their fate, to the outcome of the disease, to the results of treatment; passive submission to procedures and treatment |
| Interpsychically maladaptive types |
Sensitive |
Excessive preoccupation with the possibility of an adverse impression that may produce on others information about his illness. Fear of becoming a burden for close people, due to illness and an unfavorable attitude on their part in this regard. |
| Egocentric |
«Advantage by illness», putting on display their sufferings and experiences to relatives and those around in order to fully capture their attention; demanding exceptional self-care. |
| Paranoid |
Confidence that the disease is the result of someone’s intent, extreme suspicion of drugs and procedures. |
| Dysphoric |
Gloomy mood prevails, constant gloomy look; envy and hatred of the healthy, a tendency to blame others for their illness, a requirement for special attention to oneself, suspicion to procedures and treatment. |
| Undifferentiated (undefined) type |
The type of attitude to the disease has not been diagnosed. |
Patients characterized by the simultaneous presence of multidirectional psychological reactions to the disease and communication with them requires a special psychological approach. |
To assess the quality of life, the SF-36 International Questionnaire for quality of life was used [14].
The SF-36 Questionnaire consists of 36 detailed questions grouped into 8 main scales: physical functioning (PF); rolephysical condition (RP); bodily pain (BP); general health (GH); vitality (VT); social functioning (SF); role-emotional (RE); mental health (MH). All scales are grouped into two main indicators - the physical and mental components of health. Scale indicators range from 0 to 100 points, while the higher the value, the higher the well-being is.
The interpretation of test results in points: 0 - 20.0 - low indicator of quality of life; 21.0 - 40.0 - reduced indicator of quality of life; 41.0 - 60.0 - the average indicator of quality of life; 61.0 - 80.0 - increased indicator of quality of life; 81.0 - 100.0 - a high indicator of quality of life [15].
Statistical processing
SPSS-Statistical Package for the Social Sciences (SPSS Inc., Chicago IL, USA), Ms. Excel. The normality of the distribution of variables was checked using the Kolmogorov-Smirnov Test. The following statistical criteria were used: univariate analysis of variance (patients’ age, 3 groups); to compare qualitative indicators - Pearson's Chi-Square Test (type of attitude to the disease; demographic and social data); to compare variables with a distribution that differs from the normal one, the Mann-Whitney U test (quality of life); factor analysis. 5% were taken as a critical level of alpha error during statistical calculations.
The Results of the Study
Demographic and social data
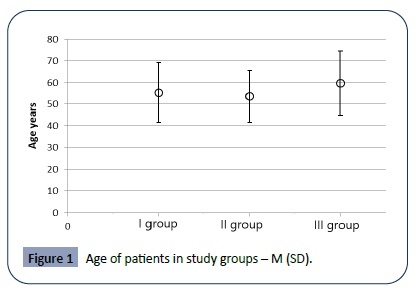
Comparison of the groups by age composition showed that there were no statistically significant differences between the study groups (F=1,12, P=0,33- a The differences between the groups were checked using the one-way ANOVA test).
Most patients were between 40 and 70 years old (Figure 1). In each group, a half were men, the other one – women. The groups were represented by workers, employees, pensioners, disabled and temporarily non-working people. Most pensioners were in groups II and III. There were no differences between the groups according to their social status.
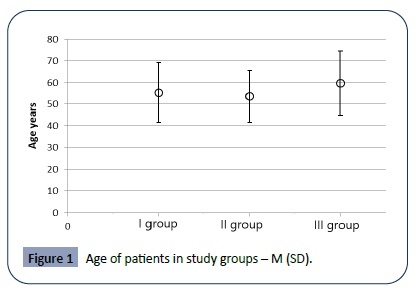
Figure 1: Age of patients in study groups – M (SD).
Thus, patients with coronary heart disease all had secondary specialized and higher education; patients with obstructive pulmonary disease - mainly secondary and specialized secondary education; half of patients with osteochondrosis had secondary and the other half had a secondary special and higher education (Table 2).
Table 2 Distribution of patients by level of education and social status in study groups.
| |
Group I
N (%) |
Group II
N (%) |
Group III
N (%) |
Value ? |
| Education |
<0,001b
Chi-Square: 21.097, 4df |
| Secondary-level education |
|
9 (40,90) |
12 (54,60) |
|
| Professional (secondary specialized) education |
19 (86,40) |
9 (40,90) |
5 (22,70) |
|
| Higher |
3 (13,60) |
4 (18,20) |
5 (22,70) |
|
| Social position |
0.07b |
| Workers |
5 (22,70) |
4 (18,20) |
4 (18,10) |
|
| Employees |
8 (36,50) |
5 (22,70) |
4 (18,10) |
|
| Pensioners |
5 (22,70) |
12 (54,60) |
8 (36,50) |
|
| Working pensioners |
1 (4,50) |
|
2 (9,10) |
|
| Disabled people |
3 (13,60) |
1 (4,50) |
2 (9,10) |
|
| Temporarily jobless |
|
|
2 (9,10) |
|
a Differences between groups were verified using one-way ANOVA Test
b Differences between groups’ proportions were tested by the Chi-Square
c Differences between groups’ proportions were tested by the Mann-Whitney U test |
Types of perception of the disease and their distribution in blocks
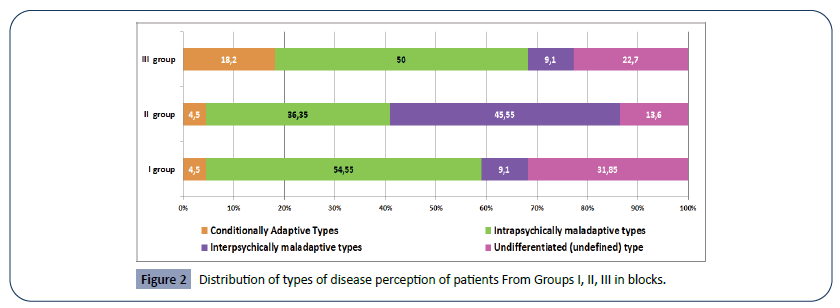
The types of disease perception of patients from different groups and their distribution by blocks are presented in Table 3 and Figure 2. Chi-Square test showed that there is a relationship between patients with different diseases and types of disease perception (Chi-Square: 44.136, 16df, p=0,01), in blocks of various «types of disease perception» (Chi-Square: 14.582, 6df, p=0.05; V Kramera = 0,33). The first and third groups were dominated by patients with intrapsychically maladaptive types and undifferentiated (unidentified) types; intrapsychic and interpsychically maladaptive types of perception of the disease. Prevailed in the second group.
Table 3 Types of attitude to the disease of patients from the studied groups and their distribution in blocks.
| Blocks of «types of attitude towards the disease» |
Types of attitude to the disease |
Group I
N (%) |
Group II
N (%) |
Group III
N (%) |
Value ? |
| Conditionally Adaptive Types |
Harmonious |
|
|
3 (13,7) |
0,01b |
| Ergopathic |
1 (4,50) |
1 (4,50) |
1 (4,50) |
| Anosognosic |
|
|
|
| Intrapsychically maladaptive types |
Disturbing |
2 (9,10) |
1 (4,50) |
5 (22,70) |
| Hypochondria |
5 (22,75) |
|
|
| Neurasthenic |
1 (4,50) |
5 (22,75) |
|
| Melancholic |
|
|
|
| Apathetic |
4 (18,20) |
2 (9,10) |
6 (27,30) |
| Interpsychically maladaptive types |
Sensitive |
|
|
|
| Egocentric |
|
|
|
| Paranoid |
2 (9,10) |
3 (13,70) |
2 (9,10) |
| Dysphoric |
|
7 (31,85 ) |
|
| Undifferentiated (undefined) type |
Diagnosed with more than three types of attitude to the disease from different blocks |
7 (31,85) |
3 (13,60) |
5 (22,70) |
a Differences between groups were verified using one-way ANOVA Test
b Differences between groups’ proportions were tested by the Chi-Square
c Differences between groups’ proportions were tested by the Mann-Witney U test |
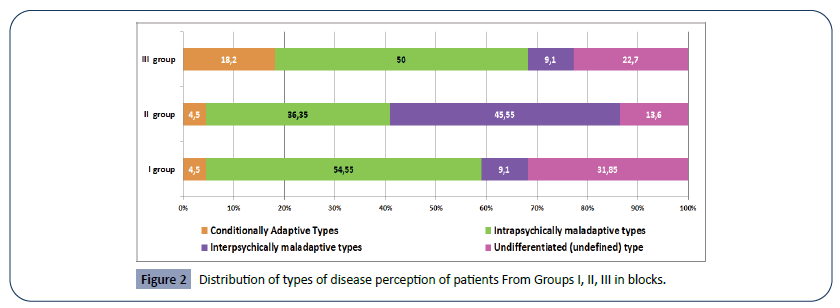
Figure 2: Distribution of types of disease perception of patients From Groups I, II, III in blocks.
The largest number of patients with conditionally adaptive type of disease perception was found in group III.
Intrapsychically maladaptive types of perception of the disease in Group I were mainly represented by patients with hypochondriac and apathetic types, in Group II - by patients with neurasthenic type; in Group III - patients with anxious and apathetic types. Patients with intrapsychic maladaptive types were characterized by obsessive fears, irritable weakness, a pessimistic assessment of their condition and prospects that caused suffering to the patient themself.
The interpsychically maladaptive types of disease perception of patients in Group II were mainly represented by paranoid and dysphoric types. The following features characterized patients with interpsychically maladaptive types of disease perception: they were embarrassed of their disease in front of others, “used” it to achieve certain goals, built a paranoid nature of the concept regarding the causes of their disease and its chronic course, manifested heterogeneous aggressive tendencies, accusing others of their illness.
The largest number of patients with an undifferentiated (unidentified) type of disease perception was identified in Groups I and III. Patients with an undifferentiated (unidentified) type of perception of the disease did not accept responsibility for the disease; had unstable, dependent on the opinions of others ideas about their disease; often used unconventional methods of treatment.
Thus, maladaptive types of disease perception in which there was a violation of adaptation to their disease were diagnosed in most patients.
Quality of life of the patients
No statistically significant difference was found between most indicators of the quality of life of patients of various groups, with the exception of three indicators – bodily pain (BP), general health (GH), which relate to the physical component of health and social functioning (SF) related to the mental health (Table 4).
Table 4 Quality of life of patients of the studied groups, SF-36 Questionnaire.
SF-36 Points
(Median; P25 – P75) |
Group I
N=22 |
Group II
N=22 |
Group III
N=22 |
P1 |
P2 |
P3 |
| PCS |
35,43
(31,41-38,03) |
36,25
(29,22-45,10) |
37,86
(32,28-42,56) |
0,4c |
0,5c |
0,5c |
| Physical Functioning (PF) |
65,0
(40, 0 – 85,9) |
45,0
(30,0 – 90,0) |
80,0
(46,25 – 90,0) |
0,9c |
0,9c |
0,2c |
| Role-Physical Functioning (RP) |
0
(0 – 50,0) |
0
(0 - 68,75) |
0
(0 – 43,75) |
0,5c |
0,4c |
0,9c |
| Bodily pain (BP) |
61,0
(41,0 - 100,0) |
52,0
(22,0 - 81,50) |
31,0
(14,5 - 41,0) |
<0,05c |
<0,01c |
<0,02c |
| General Health (GH) |
30
(25,0 - 53,75) |
55
(40,0 - 78,0) |
50
40,0 - 70,0 |
<0,001c |
<0,008c |
0,3c |
| MCS |
48,71
(42,54 – 54,0) |
45,16
(38,03 - 54,17) |
49,4
(33,49 - 56,36) |
0,2c |
0,5c |
0,8c |
| Vitality (VT) |
40,0
(35,0 - 58,75) |
45,0
(30,0 – 65,0) |
35,0
(35,0 – 65,0) |
0,5c |
0,5c |
0,9c |
| Social Functioning (SF) |
100,0
(81,25 – 100) |
75,0
(31,25 - 96,87) |
62,5
(50,0 - 87,5) |
0,001c |
0,01c |
0,9c |
| Role-Emotional (RE) |
100,0
(0 – 100,0) |
33,33
(0 – 100,0) |
100,0
(33,33 -100,0) |
0,4c |
0,6c |
0,1c |
| Mental Health (MH) |
76,0
(60,0 – 79,0) |
68,0
(52,0 – 80,0) |
52,0
(45,0 – 84,0) |
0,4c |
0,1c |
0,4c |
P1 – between groups I ? II, P2 - between groups I ? III, P3 – between groups II ? III.
a Differences between groups were verified using one-way ANOVA Test
b Differences between groups’ proportions were tested by the Chi-Square
c Differences between groups’ proportions were tested by the Mann-Witney U test |
The physical health component in patients of all groups was rated as reduced; mental component of health - as an average. Role- Physical Functioning (RP) is a person’s physical ability to carry out their professional or homework. This indicator was 0 in patients of all groups.
Bodily Pain (BP) - measures the intensity of the pain syndrome and its effect on the ability to engage in normal activities during the last month: the higher the indicator was, the more pain the patients experienced. Low values of the scale indicate that pain did not significantly limit the physical activity of the subjects. In patients of Group I, the bodily pain showed the highest level and in Group III the lowest one.
The General Health status (GH) scale is the subjective assessment by the respondent of their general state of health in present (the higher the indicator, the better the respondent perceives his overall health). The highest GH score was observed in patients of Group II, in contrast to Groups I and III. Social Functioning (SF) is the emotional and physical ability to communicate with other people. The highest level of this indicator was in patients from Group I, and the lowest - in patients from Group III.
Thus, the quality of life in the three groups revealed differences in only three components - pain intensity (BP), general health (GH), and social functioning (SF).
Factor analysis
Factor analysis revealed four factors that affect the components of quality of life: age, gender, type of perception of the disease, diagnosis.
A factor model was built in which the variables were uniquely classified according to 4 factors. The numbers in this table (factor loads) should be understood as correlation coefficients between variables and factors. The Mental Component Summary (MCS) of patients in all groups was 91% determined by the age of the respondents; the Physical Component Summary (PCS) and physical functioning (PF) - by gender, by 92% and 81%, respectively, general health - by the type of perception of the disease by 84%, social functioning (SF) - by the disease by 82% (Tables 5 and 6).
Table 5 The final factorial solution: analysis of the main components with a Variamax rotation in Groups I, II, III.
Quality of life indicators,
SF-36 Questionnaire |
Indicators |
| 1 |
2 |
3 |
4 |
| Physical Heath (PH) |
-0,14 |
0,92* |
0,11 |
0,18 |
| Physical Functioning (PF) |
0,23 |
0,81* |
-0,23 |
-0,12 |
| Role-Physical Functioning (RP) |
0,20 |
0,55 |
0,10 |
0,70 |
| Bodily Pain (BP) |
0,42 |
0,51 |
0,26 |
0,17 |
| General Health (GH) |
0,20 |
0,23 |
0,84* |
0,18 |
| Mental Health (MH) |
0,91* |
-0,18 |
0,34 |
0,27 |
| Vitality (VT) |
0,65 |
0,49 |
0,26 |
0,34 |
| Social Functioning (SF) |
0,39 |
0,33 |
0,50 |
0,82* |
| Role-Emotional (RE) |
0,77 |
0,15 |
-0,19 |
-0,10 |
| Mental Health (MH) |
0,78 |
0,35 |
0,14 |
0,21 |
| Explained variance |
4,26 |
2,08 |
1,77 |
1,21 |
| Explained variance rate,% |
30,46 |
14,87 |
12,66 |
8,68 |
Table 6 Cronbach alpha for four factors.
| Factors |
1 |
2 |
3 |
4 |
| Age |
Gender |
type of perception of the disease |
Diagnosis |
| Cronbach alpha |
0,78 |
0,48 |
0,84 |
0,77 |
Discussion
We tried to find out how the perception of the disease affects the quality of life of hospitalized patients, but beforehand we established the types of perception of the disease and determined the quality of life.
In all study groups, patients had maladaptive types of disease perception, i.e. adaptation to the disease was impaired.
In Group I (patients with coronary heart disease), the majority were patients with hypochondriac and apathetic types of perception of the disease; Group II (chronic obstructive pulmonary disease) - patients with neurasthenic, paranoid and dysphoric types and Group III (osteochondrosis) - patients with anxious and apathetic types of disease perception. Only in Group III, in 18.2% of patients did we establish conditionally adaptive types of disease perception (harmonious and ergopathic). Our study failed to diagnose the type of perception of the disease in 15 patients from all groups.
The prevalence of the hypochondriacal and apathetic types of perception of the disease in patients with coronary heart disease is consistent with the data of Lee et al. 2016, which found that the data on the hypochondria scale were significantly increased in these patients and their character began to manifest such traits as sensibility, suspiciousness, pessimism, which leads to the formation of neurovegetative disorders [16].
Our data contrast with those of other researchers [17,18] who observed conditionally adaptive types of disease perception (from 40 to 70%; harmonious, ergopathic, and anosognosic) in most hospitalized patients with coronary heart disease. However, these studies included mainly men and the average duration of the disease was only 3 years. Chronic obstructive pulmonary disease negatively affects brain function and contributes to the development of cognitive impairment [19].
Patients with COPD differ in significant changes in their personality and are characterized by: nervousness, anxiety and irritability [20], emotional lability, demonstrativeness, high sensitivity to environmental influences, fixation on negative emotional experiences, which contributes to their social isolation and further maladaptation [21].
Namely these features were inherent to patients in Group II (chronic obstructive pulmonary disease) with neurasthenic, paranoid and dysphoric types of perception of the disease. The main personality traits found in patients with osteochondrosis were anxiety, hypochondria, passivity and demonstrativeness. Clinical signs of nonspecific psychoemotional stress were detected in 70% of cases [22].
These data are confirmed in our study: patients with anxious and apathetic types of perception of the disease are characterized by anxiety and suspiciousness, passive submission to procedures and treatment.
There was no statistically significant difference between most indicators of the quality of life of patients of various groups (coronary heart disease, obstructive pulmonary disease), with the exception of three indicators - pain intensity (BP), general health (GH), which relate to the physical component of health and social functioning (SF) related to the mental component of health. The physical component of health in patients of all groups was rated as lowered; mental component of health was rated average. The life quality indicators for patients with coronary heart disease (Group I) are at the level of international reference values for Russia (PCS - 34,1 ± 6,9; MCS – 43,3 ± 9,6) [23].
Life quality indicators for hospitalized patients with chronic obstructive pulmonary disease [24], osteochondosis [8] did not significantly differ from data obtained by other researchers. We found that the perception of the disease affects general health (the physical component of the quality of life, SF-36 Questionnaire). This component of the quality of life evaluates the patients’ current state of health, treatment prospects and resistance to the disease: the higher the indicator, the better the health status of the respondent or patient is. The general state of health was assessed in Groups II (chronic obstructive pulmonary disease) and III (osteochondrosis), as an average indicator and in Group I (chronic coronary heart disease), a reduced indicator of quality of life.
Many studies have established the effect of disease perception on quality of life: in patients with coronary heart disease [6], chronic obstructive pulmonary disease [7].
We also found that age, gender, and disease affect the quality of life of patients. The psychological (mental) component of the health of patients in all groups was determined by the age of the respondents in 91% ; the physical component of health and the physical functioning - 92% and 81%, respectively; social functioning was 82% determined by the disease.
Our data confirm the studies of other authors who found that patients with chronic diseases have a significant decrease in the quality of life with age [5,25] and this decrease was also detected in the mental health component [26]. The studies found gender differences in the quality of life of patients with coronary heart disease [27], obstructive pulmonary disease [28].
How can a patient change their perception of a disease and, accordingly, the quality of their life? According to Petrie, Weinman [29] direct psycho-educational interventions can change negative beliefs about the disease and lead to improvements in a number of different health outcomes.
In this case, we can talk about the patient’s communication with a clinical psychologist, as well as with nurses and doctors, which is especially important in hospitalization. Such studies have only recently become widespread and need further probation.
The results of our study are of clinical significance: it was found out that the hospitalized patients' perception of their illness affects their quality of life; a hidden problem was revealed - communication failure between patients and medical personnel, as evidenced by a significant number of patients who refused to participate in the study, patients with an unknown type of disease perception who preferred to receive information about their disease not from medical personnel, but from roommates, magazines, Internet. The data obtained allow us to plan studies of the level of communication competence of medical personnel and the level of patients' satisfaction with medical care.
The limitations of our study are associated with a small convenient sample, due to the significant number of patients who refused to participate in the study.
Conclusions
The disease perception affects the general health status of hospitalized patients (SF-36), which determines the patient’s current state of health, treatment prospects and disease resistance. All factors affecting the quality of life of patients can be divided into two groups: non-modifiable (age, gender, disease) and modifiable factors (type of perception of the disease). By changing the patient's perception of the disease it is possible to change the quality of life of hospitalized patients.
Funding
The authors declare no grants or financial support.
Conflict of Interest
The authors declare that they have no conflicts of interest.
Ethical Approval
The study was reviewed and approved by the ethics committee of the Orenburg State Medical University (OrSMU). All procedures performed were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Patients were informed verbally and in writing about the study and gave written informed consent.
26680
References
- Jakovljevic MB, Milovanovic O (2015) Growing burden of non-communicable diseases in the emerging health markets: the case of BRICS. Front Public Health 3: 65.
- Adrián-Arrieta L, Casas-Fernández de Tejerina JM (2018) Self-perception of disease in patients with chronic diseases. Semergen 44: 335-341.
- Dekker J, de Groot V (2018) Psychological adjustment to chronic disease and rehabilitation – an exploration. Disability and Rehabilitation 40: 116-120.
- Tiemensma J, Gaab E, Voorhaar M, Asijee G, Kaptein AA (2016) Illness perceptions and coping determine quality of life in COPD patients. Int J Chron Obstruct Pulmon 11: 2001-2007.
- Megari K (2013) Quality of Life in Chronic Disease Patients. Health Psychol Res 1: e27.
- Yaraghchi A, Rezaei O, Mandegar MH, Bagheriand R (2012) The relationship between illness perception and quality of life in Iranian patients with coronary artery bypass graft. Procedia: Social and Behavioral Sciences 46: 3329-3334.
- Scharloo M, Kaptein A, Schlösser M, Pouwels H, Bel E, et al. (2007) Illness Perceptions and Quality of Life in Patients with Chronic Obstructive Pulmonary Disease. The Journal of asthma: official journal of the Association for the Care of Asthma 44: 575-581.
- Komleva NE, Spirin VF (2013) Spirin Quality of life in patients with back pain. Acta Biomedica Scientifica 3: 19-22.
- Zaĭtsev VP, Tiurina OG, Aĭvazian TA, Gorbunov FE, Maslovskaia SG (2002) Pain perception and psychological status of patients suffering from spinal osteochondrosis with pain syndrome. Vopr Kurortol Fizioter Lech Fiz Kult 6: 30-33.
- Dantas I, Santana R, Sarmento J, Aguiar P (2016) The impact of multiple chronic diseases on hospitalizations for ambulatory care sensitive conditions. BMC Health Services Research 16: 348.
- Chhari N, Mehta SC (2016) Stress among patients during hospitalization: a study from central India. National Journal of Community Medicine 7: 274-277.
- Blecker S, Meisel T, Dickson VV, Shelley D, Horwitz LI (2017) "We're Almost Guests in Their Clinical Care": Inpatient Provider Attitudes Toward Chronic Disease Management. J Hosp Med 12: 162-167.
- Yaltonsky VM, Moskovchenko DV, Sirota NA, Yaltonskaya AV (2017) Psychometric Properties of Revised Illness Perception Questionnaire: Testing on Patients with Breast Cancer and Ischemic Heart Disease. Clinical Psychology and Special Education 6: 158–174.
- de Vet HC, Adèr HJ, Terwee CB, Pouwer F (2005) Are factor analytical techniques used appropriately in the validation of health status questionnaires? A systematic review on the quality of factor analysis of the SF-36. Qual Life Res 14: 1203-1218.
- Ware JE Jr, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30: 473-483.
- Lee JG, Choi JH, Kim SY, Kim KS, Joo SJ (2016) Psychiatric Characteristics of the Cardiac Outpatients with Chest Pain. Korean Circ J 46: 169-178.
- Solodukhin AV, Bezzubova VA, Kuhareva IN, Inozemtseva AA, Seryy AV, et al. (2017) The Relationship between Psychological Characteristics of the Attitude to the Disease, Coping Behavior of Patients with Ischemic Heart Disease, and their Cognitive Status. RUDN Journal of Psychology and Pedagogics 14: 178-189.
- Shtrakhova AV, Semiryazhko AV (2015) Features and intratseptsii internal picture of illness in patients with painful and painless coronary heart disease. Bulletin of the South Ural State University. Ser Psychology 8: 43-58.
- Schou L, Østergaard B, Rasmussen LS, Rydahl-Hansen S, Phanareth K (2012) Cognitive dysfunction in patients with chronic obstructive pulmonary disease--a systematic review. Respir Med 106: 1071-1081.
- Blinderman CD, Homel P, Billings JA, Tennstedt S, Portenoy RK (2009) Symptom distress and quality of life in patients with advanced chronic obstructive pulmonary disease. J. Pain Symptom Manage 38: 115-123.
- Khramtsova VV (2014) Influence of personality traits on the quality of life of patients with chronic obstructive pulmonary disease (copd) of dust etiology. Journal of the Grodno State Medical University 1: 70-72.
- Grigor'eva VN, Gustov AV (1997) The psychological characteristics of patients with neurological manifestations of lumbar osteochondrosis. Zh Nevrol Psikhiatr Im S S Korsakova 97: 12-15.
- Huber A, Oldridge N, Höfer S (2016) International SF-36 reference values in patients with ischemic heart disease. Qual Life Res 25: 2787-2798.
- Wacker ME, Hunger M, Karrasch S, Heinrich J, Peters A, et al. (2014) Health-related quality of life and chronic obstructive pulmonary disease in early stages – longitudinal results from the population-based KORA cohort in a working age population. BMC Pulm Med 14: 134
- Parker L, Moran GM, Roberts LM, Calvert M, McCahon D (2014) The burden of common chronic disease on health-related quality of life in an elderly community-dwelling population in the UK. Fam Pract 31: 557-563.
- Hsiao-Mei Chen, Ching-Min Chen (2017) Factors Associated with Quality of Life Among Older Adults with Chronic Disease in Taiwan. International Journal of Gerontology 11: 12-15.
- Westin L, Carlsson R, Erhardt L, Cantor-Graae E, McNeil T (1999) Differences in quality of life in men and women with ischemic heart disease. A prospective controlled study. Scand Cardiovasc J 33: 160-165.
- Katsura H, Yamada K, Wakabayashi R, Kida K (2007) Gender-associated differences in dyspnoea and health-related quality of life in patients with chronic obstructive pulmonary disease. Respirology 12: 427-432.
- Petrie KJ, Weinman J (2012) Patients’ Perceptions of Their Illness: The Dynamo of Volition in Health Care. Current Directions in Psychological Science 21: 60-65.