Tziallas D.1, Kastanioti C.2*, Tziallas V.3, Gouva M.4, Skapinakis P.5
1RN MSc, NFESC, Head Nurse of the Department of Internal Medicine, University Hospital of Ioannina
2PhD, Ass. Professor, Faculty of Health management, ATEI Kalamata
3RN- Department of Psychiatry General Hospital of Athens G.Gennimatas
4Psychology, Asis.Professor, ΤΕΙ of Epirus, Ioannina
5Lecturer, Medical School, University of Ioannina
- *Corresponding Author:
- Catherine Kastanioti
Assistant Prof., Faculty of Health care management and Administration,
ATEI Kalamatas, Antikalamos Messinias
24100 Kalamata
E-mail: ckastanioti@teikal.gr
Keywords
Quality of life, smoking cessation, coronary heart disease
Introduction
Quitting smoking after a coronary event reduces the 3-5 years mortality with 35%-50% [1], and this reduction increases further with several years of follow up [2]. Despite this, only 30-40% stops smoking spontaneously [3,4]. Randomized trials have shown that smoking cessation rates after myocardial infarction and percutaneous coronary intervention (PCI) can be significantly increased if applying a smoking cessation program with several months of intervention [5]. Such programs have also been shown to be very cost-effective in terms of years of life saved [6]. Several studies have found that smoking is related to poor quality of life (QoL) [7]. In cardiovascular patients, however, less attention has been given to the effect of smoking cessation on patients' QoL [8].
We therefore sought to explore the extent to which smoking cessation leads to changes in QoL in coronary patients. We were particularly interested in changes in QoL as related to smoking status (such as quitters, smokers, and those who failed their quit attempt). Furthermore, we examined whether patients’ QoL was influenced clinical characteristics (e.g., nicotine dependency).
Materials and Methods
The study protocol conforms to the principles of the Declaration of Helsinki and was approved by the hospital ethical committee. Two hundred (100 smokers and 100 ex-smokers) patients referred for coronary angiography in Cardiology Department of Hospital University of Ioannina between November 2004 and July 2005 gave written informed consent and were enrolled in the study. Patients were considered to be quitters if they had not been smoking for the last 12 months and were considered smokers otherwise. Sociodemographic features, smoking habits and medical history were prospectively recorded. QoL was assessed using SF-36(SF-36 Health Survey) [8] instrument which contains 36 questions and 8 scales (Physical Functioning, Role-Physical, Bodily Pain, General Health, Vitality, Social Functioning, Role-Emotional, Mental Health). For all questions, a high score corresponds to a better QoL. We applied the Greek language version of the SF-36 [10]. Severity of nicotine dependence was measured using the Fagerstro¨m Test for Nicotine Dependence [9], which measures smoking habits using six questions. Sum scores (ranging from 0 to 10) are used to categorize patients as having low (5) or high (>6) nicotine dependency. Out of 200 patients enrolled in the study, 86 smoker (response rate 86%) and 70 non smoker patients (response rate 70%) completed the SF-36 questionnaire. All of the smoker patients completed the Fagerstrom test to assess the nicotine dependence rate. The researcher carrying out the study protocol as well as the assessment of outcomes was blinded to the intervention
Statistical analysis
Continuous variables are expressed as mean ± standard deviation. For categorical variables, analysis included frequencies and percentages. All tests of significance were two-tailed: x2 and Fisher’s exact test for discrete variables and analysis of variance (ANOVA) for continuous variables. We chose a significance level of 0.05. To be able to adjust for differences in baseline characteristics, the QoL scores in non-randomized groups (smokers’ vs non smokers) were compared using multivariate linear regression analysis. We used SPSS for Windows for all analyses.
Results
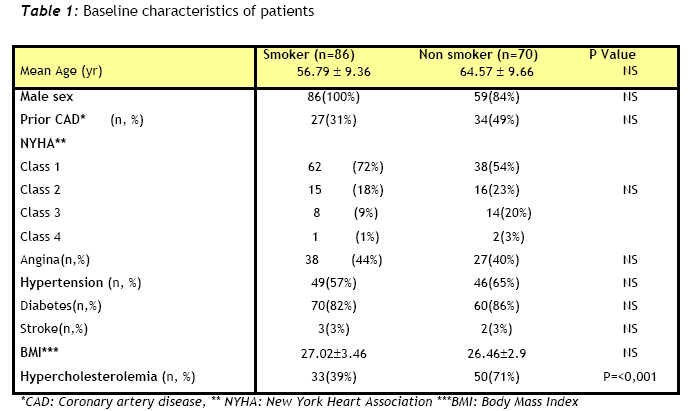
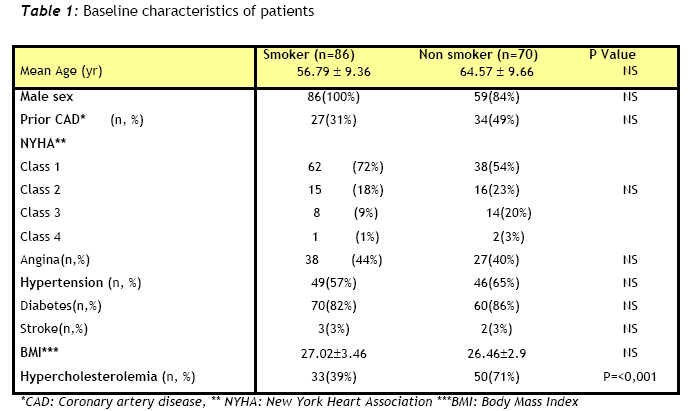
A total of 200 patients were included in the analysis. As shown in Table 1 no significant differences were found between groups in baseline variables such as age or co-morbidities (Table 1). The only baseline characteristic that differed significantly between smokers and non-smokers was the level of hypercholesterolemia.
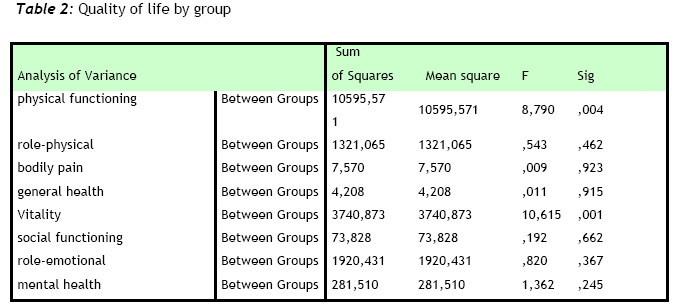
Six out of eight scales such as role-physical, bodily pain, general health, social functioning, role-emotional, and mental health were comparable between the two groups. On the other hand physical functioning and vitality scales were improved in smoker patients. (see Table 2 ).
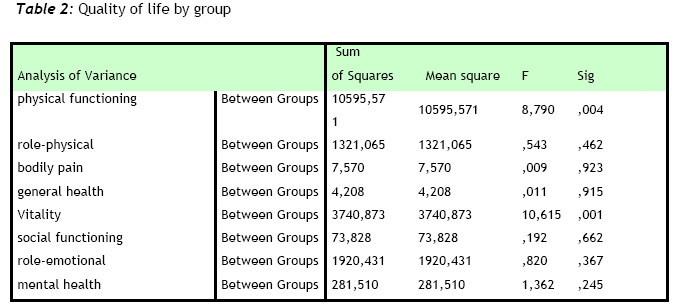
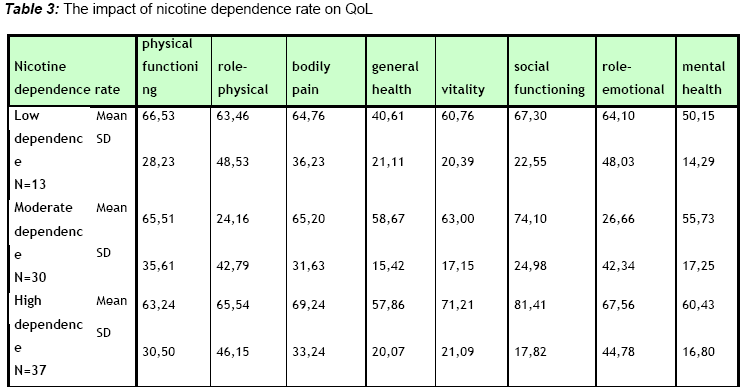
Table 3 shows the impact of nicotine dependence rate on QoL. Although, General health is statistically improved in moderate dependent patients (P=0.011), the role physical (P=0.001) and role emotional (P=0.001) scale are improved in high and low dependent patients.
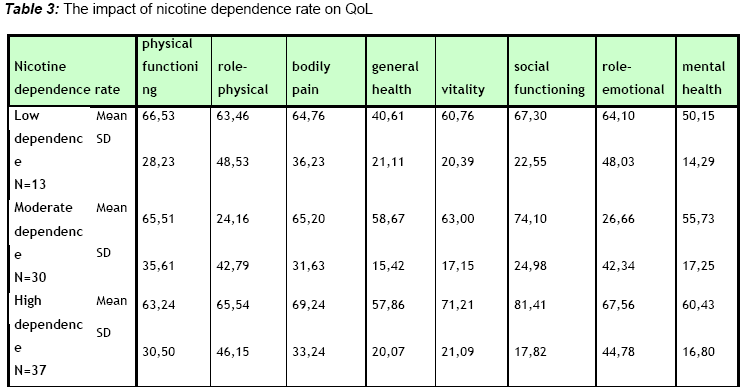
Table 4 shows the impact of CAD on QoL in patients enrolled in the study. Significant differences in QoL scores could be demonstrated between coronary and non coronary patients.

Discussion
According to the AHA/ACC guidelines for the treatment of coronary artery disease “patient and physician together should explore the potential benefits of improved quality of life with the attendant risks of the procedure versus alternative therapy, taking into account baseline functional capacities and patient’s preferences”. Moreover, Health related quality of life is increasingly preferred as an endpoint in the assessment of efficacy and effectiveness of surgical interventions.
In this prospective study, we aimed to show the Quality of life (QoL) profile in smoker and ex-smoker patients referred for coronary angiography. The QoL subscales such as vitality and physical functioning were improved in smoker patients. Quist-Paulsen P and his colleagues8 have shown that the difference in QoL between quitters and smokers increased as the amount of smoking increased, but no trend in the difference in QoL was observed with time since quitting.
With regard to nicotine dependency this study found that general health improved in moderate smokers than heavy. On the other hand the physical and emotional vitality scales were improved in low dependant smokers. Wilson and colleagues [11] reported significantly lower general and mental health QoL scores among heavy and moderate smokers than among light and never smokers, indicating that the number of cigarettes smoked each day was related to QoL. In addition, Schmitz [12] found that nicotine-dependent smokers reported significantly poorer overall QoL and greater disability than nondependent smokers. However, they found only small differences when they compared QoL and disabilities between current nondependent smokers and never-smokers.
In cardiovascular patients, however, less attention has been given to the effect of smoking cessation on patients’ wellbeing. According to the results of the study patients after a coronary event have impaired QoL compared to those without such an event. According to Haddock et al [13] never-smokers and quitters experienced significantly higher physical and mental QoL than smokers at 12 months after the procedure.
For our data to be interpreted properly, the limitations of our study must be addressed. One limitation of the study is the small number of patients enrolled compared to other studies and a larger sample size may have shown significant differences in QoL outcomes. Furthermore, the patients enrolled in the study were not randomized to either group. Nevertheless factors that may affect QoL outcomes such as functional classification according to the New York Heart Association, age and cardiovascular risk factors did not differ significantly between the two groups.
Several investigators have shown that patients with coronary heart disease who smoke have inferior QoL compared to non-smokers [7,8], but only a few studies have analysed whether nicotine dependence rate has impact on QoL. Further studies are needed to conclude whether nicotine dependence rate is a negative predictor of QoL and if QoL has impact on smoking cessation in patients with coronary heart disease. Moreover, research into psychosocial adjustment and quality of life reflect nursing’s long-standing interest in these important outcomes [14].
3668
References
- Critchley JA,Capewell S Mortality risk reduction associated with smoking cessation in patients with coronary heart disease JAMA 2003; 290:86-97
- Daly LE, Mulcahy R, Graham IM, Hickey N. Long term effect on mortality of stopping smoking after unstable angina and myocardial infarction. BMJ 1983;287:324-326
- Taylor CB, Houston-Miller N, Killen JD, DeBusk RF. Smoking cessation after acute myocardial infarction: effects of a nurse-managed intervention. Ann Intern Med 1990; 113:118-123.
- Erickson SR, Thomas LA, Blitz SG, Pontius LR. Smoking cessation: a pilot study of the effects on health-related quality of life and perceived work performance one week into the attempt. Ann Pharmacother. 2004; 38(11):1805-10.
- Tziallas D, Kastanioti CK, Alevizatou A., Katsaraki A, Skapinakis P. The value of nicotine dependence rate measurement in coronary artery disease patients. Nosileftiki 2006;45(2):248-253
- Probstfield J. How cost-effective are new preventive strategies for cardiovascular disease? Am J Cardiol 2003;91:22G-27G
- Taira DA Impact of smoking on health-related quality of life after percutaneous coronary revascularization. Circulation 2000;102:1369-1374
- Quist-Paulsen P, Bakke PS, Gallefoss F. Does smoking cessation improve Quality of Life in patients with coronary heart disease? Scan Card J 2006; 40: 11_/16
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO The Fagerstrom Test for Nictoine Dependence: A revision of the Fagerstrom Tolerance Questionnaire. . British Journal of Addictions 1991;86:1119-27
- Κontodimopoulos Ν., Fragouli D, Pappa Ε., Νιakas D. Statistical tests of the validity and reliability of the Greek SF-36. Qual Life Res 2005;14:1433-1438
- Wilson DH, Chittleborough CR, Kirke K, Grant JF, Ruffin RE.The health-related quality of life of male and female heavy smokers. Soz Praventivmed. 2004; 49(6):406-12.
- Schmitz JM. Conference summary Fifth Annual Meeting. Society for Research on Nicotine and Tobacco. San Diego, CA, USA. 5-7 March 1999.Nicotine Tob Res. 1999 Sep; 1(3):269-71.
- Haddock CK, Lando H, Klesges RC, Peterson AL, Scarinci IC.Modified tobacco use and lifestyle change in risk-reducing beliefs about smoking.Am J Prev Med. 2004; 27(1):35-41.
- Deaton C., Namasivayam S. Nursing Outcomes in Coronary Heart Disease. J Cardiovascular Nursing 2004;19(5): 308-315