Introduction
Heterotopic ossifications (HO) are benign conditions triggered by normal bone formation abnormally localised. There are three possible causes:
-progressive myositis ossificans: rare genetic disease described since 1692 by Patin [1]
-traumatic myositis ossificans: the most frequent cause, through direct or surgical trauma
-neurogenic heterotopic ossification (HO): described by Dejerine and Ceilier in 1918 as para-osteoarthropathy in patients with medullary lesions [2].
The latter makes the object of this article and occurs in severe medullary and brain traumatisms, less frequently in vascular accidents, encephalitis, tetanus and severe burns. It is a condition that exacerbates the morbidity of HO neurologic traumatism, leading to important range of motion limitations, even more so when it localises near joints. The most frequently affected is the hip joint, then shoulder, elbow and rarely the knee.
Case presentation
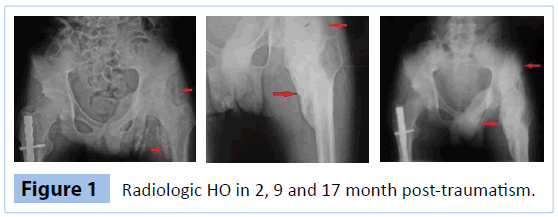
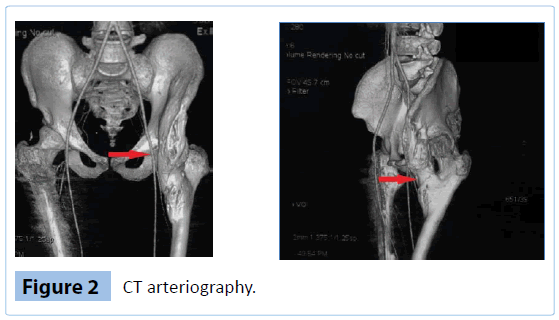
The patient, aged 22, involved in a road traffic accident, was admitted in hospital with medium cranio-cerebral traumatism and spinal traumatism, sternum and bilateral clavicle fracture, right femur fracture, bilateral lung contusions. The patient was kept in induced coma, requiring assisted ventilation for 2 months; meanwhile his health underwent complications due to septic shock and development of multiple organ failures (lung, cardio-circulatory, renal, hepatic). After 2 months, X-ray tests (radiography) revealed left hip HO signs (Figure 1). The patient was transferred in a medical recovery section with tetraparesis with predominant spastic paraplegia and sensitivemotor polyradiculoneuritis of unknown aetiology (normal brain and spinal computed tomography–CT scan0. Throughout the next 17 months, the patient underwent kinetotherapy, physiotherapy and neurologic treatments focused mainly on the recovery of the neurologic deficits. No drugs were administrated to the patient for the HO prophylaxis neither in the hospital nor afterwards. Hence, the passive motion in the left hip joint was gradually impaired and after 9 months from the accident a massive 25 cm HO was identified. The patient was admitted in our clinic after 17 months post-traumatism with complete left hip ankilosis, diagnosed with spastic paraplegia, his upper limbs being partially recovered. The local exam reveals a tough well-confined tumour formation at the level of the femoral trigon. For the surgical excision of the formation, a simple X-ray (Figure 1), CT scan and CT arteriography with 3D reconstruction were performed to establish the relations with the vascular-nervous formations. Following these medical investigations, it is determined that the ossification, which had already reached maturity, affects the area corresponding to the iliopsoas muscle and tendon, localised anteromedial, from the left iliac crest and fossa up to the lesser trochanter; neither the iliac or femoral vascular axis nor their emergent branches were affected (no embedment, contact or position change) (Figure 2). MRI (magnetic resonance imagery) exam was impossible due to the metallic implants.
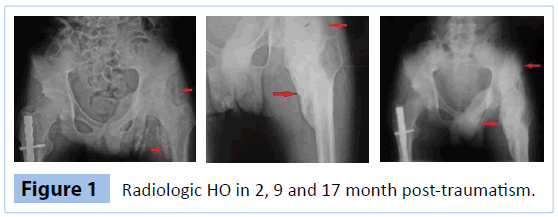
Figure 1: Radiologic HO in 2, 9 and 17 month post-traumatism.
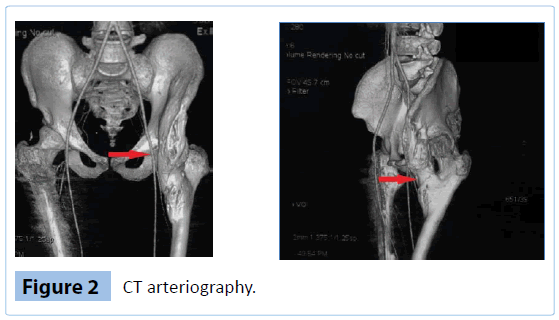
Figure 2: CT arteriography.
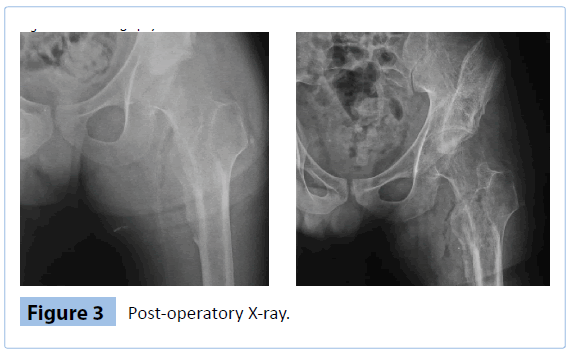
The patient was operated on dorsal decubitus position, anterior approach, reflecting the sartorius and right femoral muscles. The thorough dissection emphasised femoral vascular package, a vascular surgeon standing close-by. The resection piece was extracted in segments. Blood losses were important: 1000 ml intra-operatory and 500 ml post-operatory. After surgery, the patient was subject to an antibiotic, prophylactic treatment, anticoagulant and Indomethacin, 75 mg/day for 6 weeks, kinetotherapy (Figure 3). Immediately after surgery, the flection was >90, and within 11 months the passive mobility was restored. At present, the patient maintains seated position for brief intervals and his hygiene is correctly ensured.
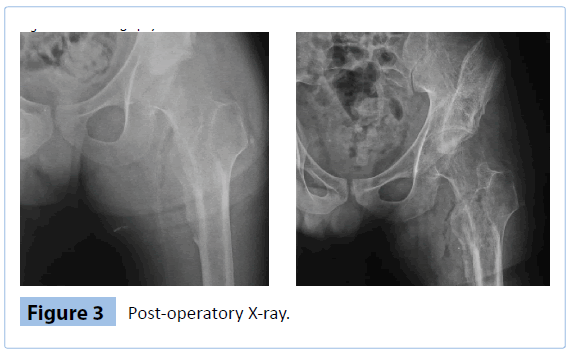
Figure 3: Post-operatory X-ray.
Discussion
HOs are complications that need to be considered in patients with neurologic traumatisms. They may appear in any joint but mainly at hip level. The related etiopathogeny is currently unknown, the existing data referring to the factors triggered by neurologic traumas: increased calcium and prolactin levels, BMP (bone morphogenetic protein), precipitation of calcium and phosphates, tissue hypoxia, genetic factor, etc. There are studies that determined several important HO risk factors in such patients: spasticity [3], thoracic trauma, presence of tracheostomy and urinary tract infections [4]. A long immobilisation period is also associated to HO [5] as well as the need for mechanical ventilation through the generated systemic ankilosis [6]. Many of these factors also affected our patient. It has been suggested that the diffuse axonal lesions lead more quickly and more frequently to HO than focal brain lesions. Such lesions appear mostly in younger patients in coma for large periods of time and developing spasticity [7]. Our patient falls into this group, the brain and spinal exams failing to point out a more precise neurological diagnosis.
The hip localization of these ossifications varies, the most frequent being anterolateral, inferior-medial and posterior. The anteromedial position is less recurrent, sometimes encountered in medullar traumatisms or through direct traumatism [4,8,9]. This rare position of a big HO was last time cited in 2012 [9].
From a biological standpoint, some important markers were recommended, especially the follow-up of the alkaline phosphatasis-PA whose levels are enhanced by osteoblastic activity [3,8,9]. However, it couldn’t be used here. A valuable indicator is the increase of urinary PGE2 (prostaglandin E2) level but, due to related high expenses, this test was left aside. The most efficient and cost-effective method of HO detection remains the simple radiography although it takes between 6-8 months to set the final diagnosis. Less frequently, the 3-phase scintigraphy is used, detecting HO within 2-3 weeks [10,11]. The MRI study can detect the formation in an early stage [17], but it is not applicable in our case due to the presence of metallic implants.
HO treatment comprises two aspects: prophylactic aiming at the reduction or the complete cessation of the osteoformation process and curative through the surgical removal of the already formed bone and the joint mobility restoration. Drug prophylaxis is possible with bisphosphonates and NSAID (nonsteroidal anti-inflammatory drugs). The most frequently used bisphosphonates were etidronate and pamidronate which have more anti-bone formation properties than antiresorptive effects [12]. However, the in-vitro studies with this type of drugs have proven to be relatively efficient especially in infraradiological stages [13,14]. The indomethacin proved its efficiency in the HO prevention, reducing the ectopic bone formation process through a partially known mechanism, especially anti PGE2 [15,16]. The early mobilisation, albeit not very aggressive, is recommended from the very beginning in patients at risk, even if sometimes mobilisation is obtained at the expense of a pseudarthrosis in the ossification mass [17]. HO can be treated only surgically and usually once the ossification reached maturity (12 months after medullar lesions and 18 months after craniocerebral lesions) [18]. This maturity is the hardest to determine, in general based on X-ray and biological markers dynamics (AP and PGE2). There is a major femoral neck fracture risk intra and post-operatory (post immobilization osteoporosis) which can be avoided through careful handling. Furthermore, arthrofibrosis, ankilosis, which is hard to recover from, can be present postoperatory.
Conclusion
The patient developed a rare form of iliopsoas hip ossification. The induced coma, the spasticity, the assisted mechanical ventilation along with the organic complications during coma, increased the HO risk. The neurological diagnosis of sensitive-motor polyradiculonevritis or axonal lesion within dominant spasticity paraplegia is compatible with frequent HO. In such patients it is mandatory to biologically and radiologically check the HO occurrence and drugs prophylaxis must be initiated as soon as possible to prevent ankilosis. Once this complication arises, the only remaining efficient treatment is the surgical excision of the formation. In the future it would be interesting to study the effect of other drug related therapies not only for the prevention, but for the treatment of this kind of complications in the early stages of evolution.
Consent
Written consent was obtained from the patient for publication of the case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of the journal.
6735
References
- Geschickter CF, Maseritz IF (1938) Myositis ossificans. J Bone Joint Surg Am 20: 661-674.
- Dejerine A, Ceiller A (1918) Para-osteo-arthropathies des paraplegiques par lesion medullaire: etude cliniqueetradiographique. Ann Med 5: 497.
- Garland DE (1988) Clinical observations on fractures and heterotopic ossification in the spinal cord and traumatic brain injured populations. ClinOrthopRelatRes : 86-101.
- Citak M, SueroEM, Backhaus M, Aach M, Godry H, et al. (2012) Risk factors for heterotopic ossification in patients with spinal cord injury: a case-control study of 264 patients. Spine (Phila Pa 1976) 37: 1953-1957.
- Mielants H, Vanhove E, de Neels J, Veys E (1975) Clinical survey of and pathogenic approach to para-articular ossifications in long-term coma. ActaOrthopScand 46: 190-198.
- Newman RJ, Stone MH, Mukherjee SK (1987) Accelerated fracture union in association with severe head injury. Injury 18: 241-246.
- Garland DE (1991) A clinical perspective on common forms of acquired heterotopic ossification. ClinOrthopRelatRes : 13-29.
- Sirvanci M, Ganiyusufoglu AK, Karaman K, Tezer M, Hamzaoglu A (2004) Myositis ossificans of psoas muscle: magnetic resonance imaging findings. ActaRadiol 45: 523-525.
- Citta-PietrolungoTJ, Alexander MA, Steg NL (1992) Early detection of heterotopic ossification in young patients with traumatic brain injury. Arch Phys Med Rehabil 73: 258-262.
- Shehab D, Elgazzar AH, Collier BD (2002) Heterotopic ossification. J Nucl Med 43: 346-353.
- Vavken P, Castellani L, SculcoTP (2009) Prophylaxis of heterotopic ossification of the hip: systematic review and meta-analysis. ClinOrthopRelat Res 467: 3283-3289.
- Pélissier J, Grasset G, Moulin M, Soulignac J, Arrighi de CasanovaJ .Traitement précoceparl’ Ethane Hydroxy Diphosphonate Des Paraostéoarthropathies Neurogènes des traumatiséscrâniens.
- Raisz LG, Pilbeam CC, Fall PM (1993) Prostaglandins: mechanisms of action and regulation of production in bone. OsteoporosInt 3 Suppl 1: 136-140.
- Chouhan DK, Dhillon M, Bachhal V, Prabhakar S (2012) Atraumatic heterotopic ossification of iliopsoas muscle: a case report. OrthopSurg 4: 197-201.
- Garland DE, Blum CE, Waters RL (1980) Periarticular heterotopic ossification in head-injured adults. Incidence and location. J Bone Joint Surg Am 62: 1143-1146.
- Subbarao JV (1990) Pseudoarthrosis in heterotopic ossification in spinal cord-injured patients. Am J Phys Med Rehabil 69: 88-90.
- Enjalbert M, Marcelli C, Pélissier J, Kanj A (1995) Traîtement des paraostéoarthropathiesneurogènes par le Pamidronate. Ann RéadapMédPhys 38:409-414