Keywords
Reconciliation, Medication discrepancy, Hospital, Medication error, Discharge
Introduction
Medication reconciliation is the comprehensive evaluation of a patient’s medication regimen any time there is a change in therapy in an effort to avoid medication errors such as omissions, duplications, dosing errors, or drug interactions, as well as to observe compliance and adherence patterns. This process includes a comparison of the existing and previous medication regimens and should occur at every transition of care in which new medications are ordered, existing orders are rewritten or adjusted, or if the patient has added non-prescription medications to his or her self-care [1]. Medication discrepancies may occur at any transition of care, when individuals are admitted or discharged from a hospital or nursing home. Poor communication at transition points has been reported as a major source of medication errors and adverse drug events [2].
Medication errors in hospitals are common and potentially harmful. Care interfaces are vulnerable points for the occurrence of drug-related incidents. Medication reconciliation, is a process proven to reduce errors occurring at these transition points [3]. Several studies have reported the prevalence of the medication discrepancy problem in adult patients According to the most conservative estimate in the literature, about half of the adult and geriatric patients in primary care had at least one medication discrepancy [4,5]. The studies investigating the harm associated with medication discrepancies indicated that 30-90% of unintentional discrepancies upon hospital discharge had the potential to cause a significant clinical impact [6]. Literature studies identified various factors contributing to the inadequacy of medication reconciliation, among which two key findings are complexity of the reconciliation process and lack of time in a busy clinical practice setting [7,8].
Each time a patient moves from one setting to another, clinicians should review previous medication orders alongside new orders and plans for care, and reconcile any differences. At discharge, the steps include determining the post discharge medication regimen, developing discharge instructions for the patient for home medications, educating the patient, and transmitting the medication list to the follow up physician [9]. The process starts when the patient is admitted to the hospital, continues whenever the patient is transferred to a different level of care, and occurs again when the patient is discharged from the hospital [10].
An appropriate medication regimen after hospital discharge is an essential component of safe and effective care following hospitalization. Yet, adverse drug events post-discharge are exceedingly common. One study estimated that 12.5% of patients suffered adverse drug events within 30 days of discharge, of which 62% were preventable or ameliorable. These preventable adverse events may be attributable to two primary factors: provider error and patient misunderstanding [11]. Admission and discharge medication lists in institutions, medication lists in physician offices and in community pharmacies may all contain different information. Medication list errors are common with reported rates in hospitalized patients nearing 70% of patient lists in some reports [12,13].
The goal of medication reconciliation is to obtain and maintain accurate and complete medication information for a patient and use this information within and across the continuum of care to ensure safe and effective medication use [1]. Discrepancies identified that are inconsistent with documented care plans and/ or are not explained by the patient’s current clinical status (i.e., unintended discrepancies) should be discussed with the physician for resolution, and resulting changes and/or clarifications should be documented. Patients should be educated on any changes to their medication regimen to ensure understanding in preparation for discharge [14].
Medication discrepancies appear to have a negative effect on morbidity. Coleman et al. observed that among patients 65 years and older, 14.3% of those who had a medication discrepancy were re-hospitalized at 30 days compared to 6.1% of the patients who did not experience a discrepancy [15]. Medication discrepancies can lead to adverse events upon admission to the hospital and at discharge from the hospital to the patient's home community [15,16]. Medication reconciliation is an important strategy to reduce medication error and potential harm [17]. A study conducted by Quélennec et al showed that a combined intervention of pharmacists and physicians in a collaborative medication reconciliation process had a high potential to reduce clinically relevant errors on hospital admission [18]. Medication reconciliation performed by clinical pharmacists increases the safety of patients in the admission process [19].
Avoidable hospital readmissions have persisted despite the introduction of numerous health care services originally designed to improve the hospital discharge process for newly discharged patients. In many ways the new models of advanced discharge planning and transitional care seek to restore the continuity in care that was once provided by primary care or other community-based physicians. In inpatient care unit, there are several situations where medication reconciliation is needed. Patients’ lack of knowledge of their medications, physician and nurse workflows and lack of integration of patient health records across the continuum of care contribute to a lack of a complete medication reconciliation, which in turn creates the potential for error [9].
Medication reconciliation accuracy has been studied at various transition points. On admission, medication reconciliation is prone to error with an estimated 67% of medication histories being inaccurate, thereby contributing to 27% of inpatient provider errors [20]. Inpatient transfers between units are an additional source of risk for medication provider errors, with one study identifying 62% of inpatient transfers as having at least one unintentional medication error; these errors were most often medication omissions [21]. A further set of errors can be made at the time of hospital discharge [22]. Medication reconciliation inaccuracies accumulating at all these points of transition create substantial risk for medication errors on hospital discharge [23].
Generally, patients are admitted to the hospital for a specific procedure, such as surgery, or on an urgent basis. When specialty health care providers are focused on one component of care related to the specific encounter and do not take a holistic view to other aspects of the patients’ health care needs and practices, it is easy to overlook medications that may cause an adverse event when combined with new medications or different dosages. Additionally, inability of a patient to be able to articulate his or her medication regimen accurately to healthcare providers can lead to adverse medication events that can then lead to re-hospitalizations, extended hospital stay and possibly death. Published reports of medication discrepancy in Ethiopia are scarce, so this study was initiated to provide baseline data on reconciliation of medication discrepancies at hospital discharge for inpatients in medical ward of St. Paul’s hospital millennium medical college.
Methods
Description of study area
St. Paul’s Hospital Millennium Medical College is referral and teaching hospital found in Addis Ababa, Ethiopia. The hospital currently provide medical specialty services to an estimated 200,000 people annually who are referred from all over the country and also teach the students in different undergraduate and postgraduate programs. An average of 650 patients visits the hospital as an outpatient and emergency in daily basis with a capacity of 360 beds.
Study design
Prospective cross sectional study was conducted at St. Paul’s hospital millennium medical college. During 2 months of study (March 14 –May 14, 2013), all consecutive patients discharged from the general internal medicine ward were prospectively identified. Each medical chart was screened.
Source and Study population
The source population constituted of all patients admitted to St. Paul’s Hospital Millennium Medical College. The study population consisted of patients who were admitted to medical ward of St. Paul’s Hospital Millennium medical college.
Inclusion and exclusion criteria
These patients who were included in this study were age not less than 18 and taking at least one regular prescription medication during or before hospitalization. Patients were excluded from the study if they were discharged with verbal prescription, transferred to another health facility or died during hospitalization.
Sampling and sample size determination
The sample size was calculated assuming the expected prevalence to be 50%, margin of error to be 10% with 90% confidence interval. Hence the sample size was calculated as 68. With the assumption of 10% contingency, the minimum number of patients involved in the study was determined to be 75. Although the minimum sample was calculated, we performed the survey for 2 months and a total of 111 patients fulfilling the inclusion criteria were included in the study.
Data collection and analysis
Two pharmacy staffs were recruited as data collectors for the study. Both the data collectors were given a one day training prior to data collection about how to extract information using data abstraction format and how to approach physicians. Data was collected from March 14 to May 14, 2013. Supervision and spot checking was made by the principal investigator during the data collection process. Data were abstracted using modified medication reconciliation tool. The tool was pre-tested on 10% of the estimated sample size and some modifications were made. The data were entered and analyzed using SPSS for windows version 16.0. For this study, descriptive statistics on sample characteristics was computed including percentages, frequencies and mean.
Ethical clearance
Ethical approval was obtained from the ethics review committees of the school of pharmacy, Addis Ababa University and St Paul’s Hospital Millennium Medical College. In addition verbal consents were obtained from the patients.
Results
Patient characteristics
During the study period 237 patients were screened for eligibility. Of this, 126 patients were excluded; 57 patients do not have regular medication at discharge, 47 died at discharge, 20 transferred to other health facility and 2 were self-discharged. Finally, 111 patients were included in the final analysis. From the total of 111 eligible patients 60 (54.1%) were female and 51 (45.9%) were male. The minimum age observed was 18 and the maximum age of 81 was seen with an average age of 40.6. The most frequent diagnosis at admission was infectious disease (30.6%), followed by congestive heart failure (26.1%).
Prevalence of medication discrepancy
From our 111 observations 46(41.4%) had at least one unintended discrepancy at the time of discharge. 13(11.7%) had more than one unintended discrepancy. The average number of discrepancy per patient was 0.53.
Types of medication discrepancies
Types of the 46 unintentional discrepancies are summarized in Table 1. The most common unintentional discrepancy was discrepant dosing of the medication 21 (45.6%) followed by omission of the regularly used medications 14 (30.4%). Characteristics of some of discrepancies are described in Table 2.
| Type ofDiscrepancy |
Frequency |
Percentage |
Cumulative percentage |
| Discrepant dose |
21 |
45.6 |
45.6 |
| Omissions |
14 |
30.4 |
76 |
| Commissions |
7 |
15.3 |
91.3 |
| Discrepant frequency |
4 |
8.7 |
100 |
| Total |
46 |
100 |
|
Table 1: Types of unintended medication discrepancy at hospital discharge in St. Paul’s Hospital Millennium Medical College medical ward, Addis Ababa, Ethiopia.
| Type of discrepancy |
Frequency |
Example |
| Discrepant dose |
21(45.6%) |
Patient admitted for NYHA class IV CHF was takingFurosemide 20mg iv bid during hospitalization; on discharge, Furosemide 20mg po bid was written |
| Omissions |
14(30.4%) |
Patient admitted for NYHA class IV CHF was takingFurosemide 40mg iv bid during hospitalization; on discharge, Furosemide was unintentionally omitted. |
| Commissions |
7(15.3%) |
Patient admitted for GBS was taking Amitriptyline 25mg ponocte and then it was changed to Carbamazepine 200mg po daily due to side effects but at discharge, both medications were written. |
| Discrepant frequency |
4(8.7%) |
RVI patient admitted for pulmonary tuberculosis was taking Co-trimoxazole 960mg po daily, but at discharge the frequency was changed to every other day unintentionally. |
Table 2: Characteristics of unintended medication discrepancy at hospital discharge in St. Paul’s Hospital Millennium Medical College medical ward, Addis Ababa, Ethiopia , March - May, 2013.
Drugs involved in discrepancy
The unintended discrepancies were also classified into the following groups of medications: cardiovascular medications (e.g. Furosemide, Digoxin, and Enalapril) 29 (63%), drugs used in endocrine disorders (eg. Insulin, Glibenclamide) 7 (15.2%), antiinfective (e.g. Co-trimoxazole,) 4 (8.7%), others 6 (13.1%) (Table 3).
| Type of medication |
Frequency |
Percentage |
cumulative percentage |
| Cardiovascular drugs |
29 |
63 |
63 |
| Drugs used in endocrine disorders |
7 |
15.2 |
78.2 |
| Anti-infectives |
4 |
8.7 |
86.9 |
| Others |
6 |
13.1 |
100 |
| Total |
46 |
100 |
|
Table 3: Drugs involved in unintended medication discrepancy at hospital discharge in St. Paul’s Hospital Millennium Medical College medical ward.
Length of hospital stay and number of drugs at discharge
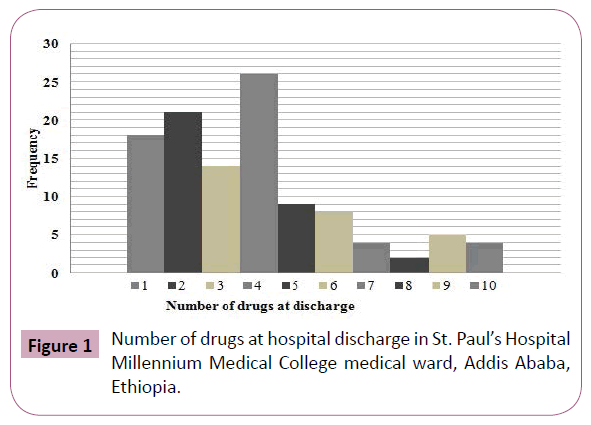
The number of days of hospitalization was calculated for each patient. The minimum days of hospitalization were 3 and the maximum was 104 days (Table 4). The average number of medication at discharge was 3.9. The minimum number of drugs at discharge was 1 and the maximum number was 10 (Figure 1).
| Type of medication |
Frequency |
Percentage |
cumulative percentage |
| Cardiovascular drugs |
29 |
63 |
63 |
| Drugs used in endocrine disorders |
7 |
15.2 |
78.2 |
| Anti-infectives |
4 |
8.7 |
86.9 |
| Others |
6 |
13.1 |
100 |
| Total |
46 |
100 |
|
Table 3: Drugs involved in unintended medication discrepancy at hospital discharge in St. Paul’s Hospital Millennium Medical College medical ward.
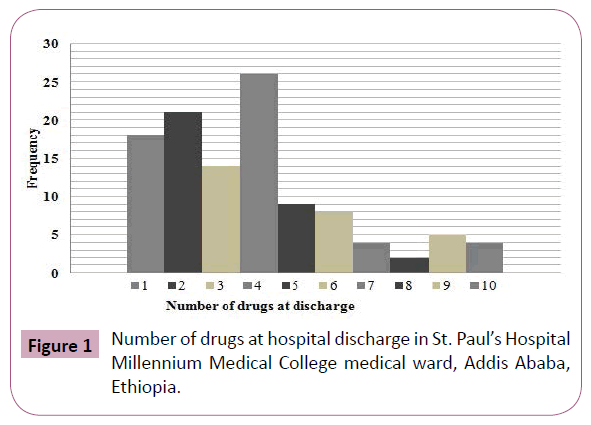
Figure 1: Number of drugs at hospital discharge in St. Paul’s Hospital Millennium Medical College medical ward, Addis Ababa, Ethiopia.
Discussion
The objective of the study was to evaluate medication discrepancy at hospital discharge. Discharge medication reconciliation requires multiple comparisons between different pieces of information, including medications on the best possible medication history (BPMH), medications prescribed in the hospital (adjusted, new, discontinued), unchanged home medications, and medications to be started at discharge, which makes this process complex. The process of discharge reconciliation on a general medicine service is especially critical given the complex needs of the patients involved.
Upon discharging the patient to home, a discharging institution lists the discharge medication regimen on the discharge summary. In our study when we compare the medications that the patient was taking before or during hospitalization with the discharge summary, we found that 41.4% of patients had at least one medication discrepancy. This was consistent with the findings of previous studies [24-26]. This is partially explained by transcription errors known to occur in discharge summaries. Although they are meant to be reviewed, corrected and signed prior to discharge, this often does not occur. However, apart from transcription errors, discharge summaries often contain missing or incorrect medication information. Physicians should take care to ensure that the medication information contained in the discharge summary is correct at the time of discharge. The inpatient clinical workflow may also explain some of discrepancies.
Discharge summary may be completed in anticipation of a discharge. Further, cancelled or delayed discharges due to deterioration in a patient’s condition necessitate that a previously dictated discharge summary be updated prior to the actual discharge. In such cases, great care should be exercised to update the discharge medication list. The result of this study demonstrated that the number of discrepancies per patient was 0.53. This number is smaller than other findings. This may be due to smaller number of medications at discharge. In other report the mean number of discharge medication discrepancies was 3.3 per patient [27]. Another study reported by Jennifer et al [28] showed that 3.5 discrepancies per patient.
The finding in the present study demonstrate that discrepant dosing of medication was the most frequent type discrepancy at discharge in contrast to previous studies which had shown that omission of the regularly taken medication was the most common discharge discrepancies[25,26,29]. This might be due to; first there is lack of information about what medications the patient was taking before admission. In developed countries the health care professional can easily access the type of medication, dosing and frequency through the community pharmacy database.
Whereas in our setting where one cannot know where the patient get the medication, it will be too difficult to prepare BPMH. Second, there is lack of involvement of pharmacy staffs in patient care service. All healthcare professionals in hospital are more or less involved in the drug therapy process. Physicians’ role is evident as they have the overall responsibility for prescribing drugs. Nurses administer most drugs, and may also monitor patients’ clinical condition in relation to drug therapy. But, the critical role played by pharmacists in the areas of medication safety and management has been left for the last many years in developing countries like Ethiopia. The role of pharmacists as members of the healthcare team should be expanded beyond conventional medication dispensing.
Pharmacists are especially well suited for performing medication related issues [30] and their deep knowledge in pharmacokinetics, pharmacodynamics and drug formulation is valuable when conducting medication reviews, adjusting doses and IV to PO conversions. This is supported by the finding that demonstrated that the mean number of discharge medication discrepancies decreased from 3.3 per patient to 1.8 per patient after pharmacists’ participation in medication reconciliation process [27].
Our finding demonstrated that cardiovascular drugs were the most frequent medications involved in discrepancy. This finding is comparable with other previous reports [7]. During our study we observed that hospitalization as a result of cardiovascular diseases is increasing as CHF was the second most frequent diagnosis at admission which comprises 26.1%. The most frequent diagnosis at admission was infectious diseases, mostly RVI admitted for pulmonary or disseminated tuberculosis. But in this group of patients the rate of discrepancy was rare since there is a lot of continuing medical education and updates on RVI management, whereas cardiovascular diseases are not given attention. In fact high complexity of the cardiovascular disease regimen and change in life style of people in the country might shift attention. Our finding showed that occurrence of discrepancy had no statistically significant association with the number of drugs at discharge, length of hospitalization and age of the patient. This may be due to small sample size.
Limitation of the Study
There were some limitations in our study. Although patients were assessed prospectively, final reconciliation was completed retrospectively within a few days of discharge for a number of patients due to time constraints. This timeframe allowed the data collectors to speak with the physician caring for the patient on whether a discrepancy was intentional or unintentional. A BPMH was not completed for all patients because since the hospital is referral, patients came from different parts of Ethiopia so it was very difficult to bring medications that they were taking at home. Small sample size also limited our confidence to extrapolate our results at larger scale.
Conclusions
Medication discrepancies occur in 41.4% of patients at hospital discharge. Discrepant dosing of medication was the most frequent type of medication discrepancy identified which consisted 45.6% and cardiovascular drugs were the classes of drugs with highest frequency. Understanding the type and frequency of discrepancies and group of patients at risk of medication discrepancy can empower clinicians to better understanding of ways to prevent them.
Acknowledgments
The authors would like to thank all the participants of the study and staffs in St. Paul’s Hospital Millennium Medical College for their cooperation in the data collection. The study was partly supported by Addis Ababa University
Contributors
MF was responsible for conception and design of study, acquisition and analysis of data, AB drafted and reviewed the article. WS supervised the study, approved the results and revised the final manuscript.
7984
References
- (2012) American Society of Health-System Pharmacists. Improving transitions of care. J Am Pharm Asso 52: 1-20.
- Farley TM, Shelsky C, Powell S, Farris KB, Carter BL(2014) Effect of clinical pharmacist intervention on medication discrepancies following hospital discharge. Int J Clin Pharm 36: 430-437.
- Magalhães GF, Santos GN, Rosa MB, NoblatLde A (2014) Medication reconciliation in patients hospitalized in a cardiology unit.PLoS One 9: e115491.
- Wong JD, Bajcar JM, Wong GG, Alibhai SM, Huh JH, et al. (2008) Medication reconciliation at hospital discharge: evaluating discrepancies.Ann Pharmacother 42: 1373-1379.
- Cornu P, Steurbaut S, Leysen T, De Baere E, Ligneel C, et al. (2012) Discrepancies in medication information for the primary care physician and the geriatric patient at discharge.Ann Pharmacother 46: 983-990.
- Nickerson A, Mackinnon NJ, Roberts N, Saulnier L (2005) Drug-therapy problems, inconsistencies and omissions identified during a medication reconciliation and seamless care service. Healthc Q 8: 65-72.
- Van Sluisveld N, Zegers M, Natsch S, Wollersheim H(2012) Medication reconciliation at hospital admission and discharge: insufficient knowledge, unclear task reallocation and lack of collaboration as major barriers to medication safety. BMC Health Serv Res 12:170.
- Greenwald JL, Halasyamani L, Greene J, LaCivita C, Stucky E, et al. (2010) Making inpatient medication reconciliation patient centered, clinically relevant and implementable: a consensus statement on key principles and necessary first steps. J Hosp Med 5: 477-485.
- Barnsteiner J (2008) Medication reconciliation: patient safety and quality: an evidence-based handbook for nurses. Available at: www.nursing.upenn.edu/faculty/pubs,pp.1-14.
- (2011) Institute for Healthcare Improvement. Prevent adverse drug events by implementing medication reconciliation. Available at: www.ihi.org, 2-14.
- Ziaeian B, Araujo KL, Van Ness PH, Horwitz LI (2012) Medication reconciliation accuracy and patient understanding of intended medication changes on hospital discharge.J Gen Intern Med 27: 1513-1520.
- Gleason KM, McDaniel MR, Feinglass J, Baker DW, Lindquist L, et al. (2010) Results of the Medications at Transitions and Clinical Handoffs (MATCH) study: an analysis of medication reconciliation errors and risk factors at hospital admission.J Gen Intern Med 25: 441-447.
- Green CF, Burgul K, Armstrong DJ (2010) A study of the use of medicine lists in medicines reconciliation: please remember this, a list is just a list.Int J Pharm Pract 18: 116-121.
- Gleason KM, Groszek JM, Sullivan C, Rooney D, Barnard C, et al. (2004) Reconciliation of discrepancies in medication histories and admission orders of newly hospitalized patients.Am J Health Syst Pharm 61: 1689-1695.
- Coleman EA, Smith JD, Raha D, Min SJ (2005) Posthospital medication discrepancies: prevalence and contributing factors.Arch Intern Med 165: 1842-1847.
- Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW (2003) The incidence and severity of adverse events affecting patients after discharge from the hospital.Ann Intern Med 138: 161-167.
- Lehnbom EC, Stewart MJ, Manias E, Westbrook JI (2014) Impact of medication reconciliation and review on clinical outcomes.Ann Pharmacother 48: 1298-1312.
- Quélennec B, Beretz L, Paya D, Blicklé JF, Gourieux B, et al. (2013) Potential clinical impact of medication discrepancies at hospital admission.Eur J Intern Med 24: 530-535.
- Leguelinel-Blache G, Arnaud F, Bouvet S, Dubois F, Castelli C, et al. (2014) Impact of admission medication reconciliation performed by clinical pharmacists on medication safety.Eur J Intern Med 25: 808-814.
- Tam VC, Knowles SR, Cornish PL, Fine N, Marchesano R, et al. (2005) Frequency, type and clinical importance of medication history errors at admission to hospital: a systematic review.CMAJ 173: 510-515.
- Lee JY, Leblanc K, Fernandes OA, Huh JH, Wong GG, et al. (2010) Medication reconciliation during internal hospital transfer and impact of computerized prescriber order entry.Ann Pharmacother 44: 1887-1895.
- Bell CM (2007) Unintentional discontinuation of long-term medications for chronic diseases after hospitalization.Healthc Q 10: 26-28.
- Grimes TC, Duggan CA, Delaney TP (2011) Medication details documented on hospital discharge: cross-sectional observational study of factors associated with medication non-reconciliation. Br J ClinPharmacol 71: 449-457.
- Moore C, Wisnivesky J, Williams S, McGinn T (2003) Medical errors related to discontinuity of care from an inpatient to an outpatient setting.J Gen Intern Med 18: 646-651.
- Vira T, Colquhoun M, Etchells E (2006) Reconcilable differences: correcting medication errors at hospital admission and discharge.QualSaf Health Care 15: 122-126.
- Wong JD, Bajcar JM, Wong GG, Alibhai SM, Huh JH, et al. (2008) Medication reconciliation at hospital discharge: evaluating discrepancies.Ann Pharmacother 42: 1373-1379.
- Varkey P, Cunningham J, O'Meara J, Bonacci R, Desai N, et al. (2007) Multidisciplinary approach to inpatient medication reconciliation in an academic setting.Am J Health Syst Pharm 64: 850-854.
- Pippins JR, Gandhi TK, Hamann C, Ndumele CD, Labonville SA, et al. (2008) Classifying and predicting errors of inpatient medication reconciliation.J Gen Intern Med 23: 1414-1422.
- Arora V, Kao J, Lovinger D, Seiden SC, Meltzer D (2007) Medication discrepancies in resident sign-outs and their potential to harm.J Gen Intern Med 22: 1751-1755.
- Reeder TA, Mutnick A (2012) Clinical pharmacy services within a multiprofessional healthcare team. Linnaeus University Dissertations 84: 28-44.