Case Report - (2022) Volume 13, Issue 1
Recurrent Intracranial Meningioma with
Pulmonary Metastases
Abidi Rim,
Mousli Alia*,
Kchaou Lina and
Nasr Chiraz
Department of Radiation Therapy, Salah Azaiz Institute, Tunisia
*Correspondence:
Mousli Alia, Department of Radiation Therapy, Salah Azaiz Institute,
Tunisia,
Tel: +21695199162,
Email:
Received: 05-Jan-2022, Manuscript No. ipjnn-22-12278;
Editor assigned: 06-Jan-2022, Pre QC No. P-12278;
Reviewed: 21-Jan-2022, QC No. Q-12278;
Revised: 24-Jan-2022, Manuscript No. R-12278;
Published:
31-Jan-2022
Abstract
We report a 40-year-old female diagnosed with histological grade III meningioma of OMS 2016 in the right side of the temporo-parietal region of skull vault. After a partial resection of the primary site, she rapidly developed unusual multiple metastasis in the pulmonary parenchyma. The patient received adjuvant radiotherapy on the residual volume with palliative decompressive intent due to the gross tumor volume. A review of the literature revealed well documented cases of benign meningiomas that metastasized in an interval of up to 10-12 years after primary tumor resection. This case illustrates that meningiomas Grade III WHO with progression disease of the primary tumor have the potential to develop hematogenous rapid metastases, emphasize the role of multimodal management and the role of genetic behavior to predict such evolution.
Keywords
Meningioma; Pulmonary metastases; Radiotherapy; Palliative
Introduction
Meningiomas represent 14-19% of all primary intracranial
neoplasms [1]. They are slow-growing typically benign intracranial
tumors that develop from the arachnoid membrane. After total
resection, meningiomas represent a low rate of recurrence
[2]. Numerous risk factors of recurrence were described in the
literature such as histological grade, subtotal resection, young
age, brain infiltration, and high proliferative rate [2]. Reportedly,
2-10% of meningiomas exhibit aggressive behaviour and the
prevalence of distant metastases is estimated to 0.1-1% of all
meningioma patients [3]. Extracranial meningioma metastases
have been reported to occur mostly in the lungs (61%), followed
by the liver, lymph nodes, and bone [3].
We report a case of multiple pulmonary meningioma metastases
developing after initial resection of right temporo-parietal World
Health Organization Grade III intracranial meningioma.
Case Presentation
Miss Y.N is a 40-year-old woman, with no past medical and family
history. A right cranial vault swelling appeared in May 2020
related to an ipsilateral temporo-parietal exteriorized mass with
necrosis without any neurological symptoms. A Brain Magnetic
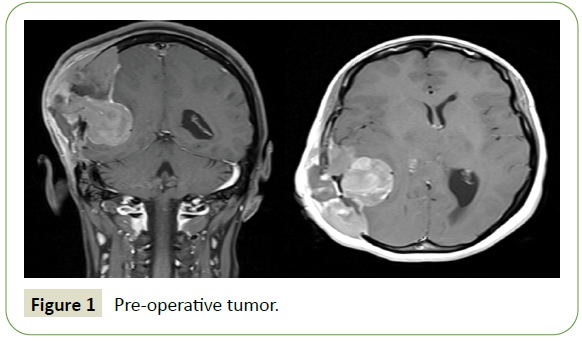
Resonance Imaging (MRI) revealed osteolytic tissue process of the
right temporo-parietal vault measuring 10 cm in the greatest axis with intracranial invasion and ventricular junction’s compression.
It showed a hydrocephalus of the temporal horn with deviation
of the midline reaching the right transverse venous sinus (Figure
1). It was incompletely surgically removed with peripheral bone
and dura infiltration. A cranioplasty with PALACOS® cement was
made.
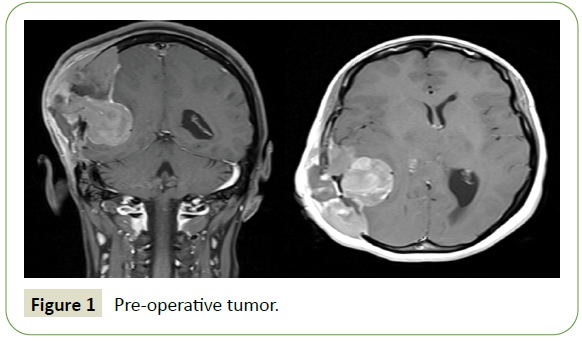
Figure 1: Pre-operative tumor.
The postoperative pathologic examination showed a poorly
undifferentiated tumor proliferation of marked cell density,
composed by anaplastic-looking cells with a nucleus provided
chromatin arranged in a fine clod of vesicular appearance. The
nuclear contours were irregular and the nucleocytoplasmic
ratio was high. Cellular anaplasia was severe with the presence
of atypical nucleus tumor cells. This concluded into aggressive
anaplastic meningioma recurrence with infiltration of adjacent
bone and adjacent glial parenchyma. The immunohistochemically
study revealed cell Epithelial Membrane Antigen (EMA), Vimentin
and PS100 cell expression. The Ki 67 index proliferation was
30% in hot-spot zones. Finally, we don’t find actin and desmin
expression excluding the diagnosis of leiomyosarcoma.
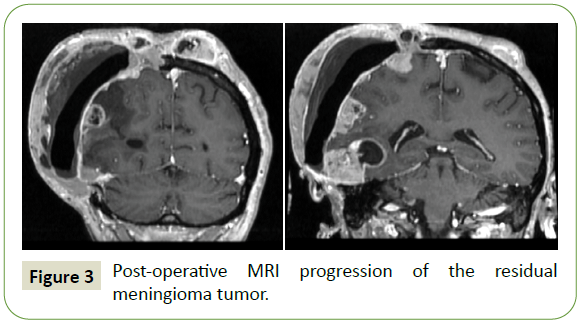
Three months later, after surgery the tumor progressed at the
initial site. She had a voluminous increased temporo-parietal
mass beyond the midline with new appearance of lesions
associated with intracranial hypertension syndrome (Figure
2). A Brain MRI showed significant right hemispherical nodular
tumor recurrence opposite to the cranioplasty, the largest one is a 40 × 30 mm cystic formation in the right temporal lobe. The
cranioplasty implant was deviated outward with extension to the
right hemispherical scalp beyond the midline to the left frontal
scalp and invaded the ipsilateral temporal and occipital bone
with partial extension to the right transverse sinus associated
to oedema (Figure 3). The thoraco-abdominal CT scan showed
multiple bilateral lung nodules.

Figure 2: Voluminous increased temporoparietal mass.
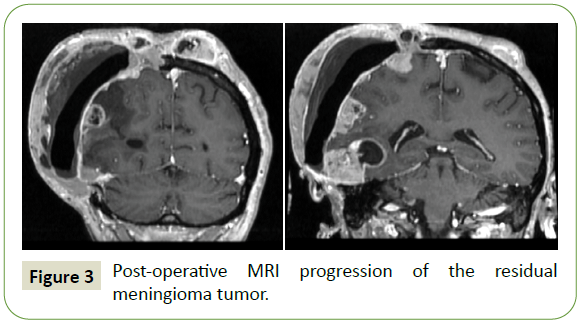
Figure 3: Post-operative MRI progression of the residual meningioma tumor.
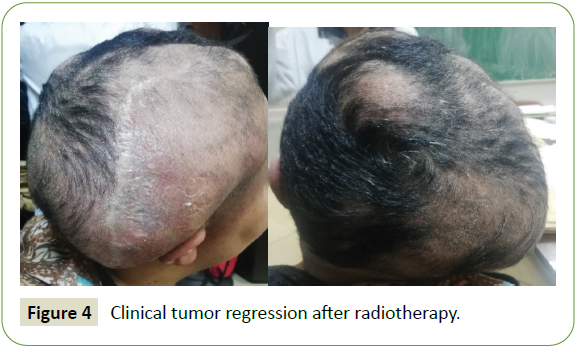
In a multidisciplinary team, we performed a palliative cerebral
radiotherapy given the metastatic status. The patient underwent
a conformational whole brain radiation therapy at the dose of
40Gy in 20 fractions. A partial response was observed in the
latest evaluation with clinical regression in number and size of
lesions (Figure 4). For pulmonary progression, she received an
anti-VEGF therapy by Bevacizumab.
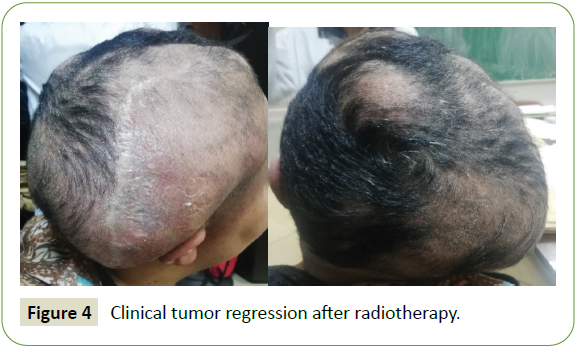
Figure 4: Clinical tumor regression after radiotherapy.
Discussion
Meningiomas annual incidence is about 4-5 cases in 100,000
people. They are commonly associated to genetic alterations in
the neurofibromatosis type 2 gene. Diagnosis is based on MRI
and confirmed by histopathological finding [4]. The World Health
Organisation (WHO) classified meningioma in 3 subtypes [5]. An
atypical and anaplastic meningioma is present in 20% of cases [4].
Metastasis outside the brain is an extremely rare entity less than
0.1% of all cases [6]. Metastatic meningioma may occur even a
decade after initial tumor resection. The mean interval between
diagnosis of the primary tumor and discovery of the first
metastases ~6 years [7]. Metastases generally occurs through
haematogenous or lymphogenous way. Pulmonary metastases are the most frequent [8]. They rarely induce symptoms and
are commonly present as a single lesion, or, less frequently, as
multiple round noncalcified parenchymal nodules of different
sizes. Multiple deposits are identified in 50% of cases [7]. High
cellularity, cellular heterogeneity, high mitotic rate, nuclear
pleomorphism, tumor necrosis and invasion of adjacent blood
vessels are histological factors of metastases [9]. On the other
hand, the authors showed that a higher cell proliferation is not a
necessary factor of extra-cranial metastasis, and that metastases
can occur in any type of individual meningioma. For recurrent
intracranial meningioma, comprehensive examinations should
be conducted for an early detection of distant metastasis even
when the primary tumor is benign [10].
There is a relationship between metastasis and tumor location.
Especially, parasagittal and falcine located meningioma
metastasized more frequently than other location [11]. Another
hypothesis of tumor spread is the blood-brain barriers damage
at the moment of primary craniotomy. Intracranial tumor
recurrence as well as papillary morphology and histological
malignancy may predict of multiple metastases [12].
Furthermore, loss of heterozygosity at 9p, 1p and 22q has been
reported to be a potential predictor of multiple pulmonary
metastases [12]. The molecular properties of meningiomas
have identified genetic biomarkers that effect tumor behaviour.
Analyses of genetic and epigenetic changes may reveal better
understanding of meningioma progression mechanisms [13].
In our case MRI found that the tumor invades the transverse
venous sinus and we found also an infiltration of bone and
adjacent glial parenchyma. The pathologic examination showed hypercellularity and infiltration of cranial bone and adjacent
normal parenchyma. Ki67 was also high. Some author mentioned
that Ki67 was related to the potential risk of recurrences but also
metastases [11].
Nowadays, there are no established guidelines for optimal
treatment in the case of extensive pulmonary metastatic
meningioma. In the present case the brain tumor recurrence was
early detected with synchronous diffuse pulmonary metastases.
This emphasizes the need for an early detection of distant
metastases. We performed a whole brain irradiation with partial
response and start bevacizumab for pulmonary Metastasis.
Conclusion
Atypical meningiomas, sinus invasion and tumor recurrence may
be the more predictive factors of pulmonary metastases. For
early detection, enhanced pulmonary computed tomography
is recommended for recurrent intracranial meningioma. There
are no established guidelines for the optimal management of
extensive pulmonary metastatic meningioma and it should be
considered as part of the differential diagnosis.
Acknowledgements
I am very thankful to all contributors, who were very helpful and
without their support this case study would have never come
into its present form.
Ethics Approval and Consent to Participate
Consent for publication written informed consent for publication
of clinical details and clinical images was done.
Consent for Publication
A written consent for publication is given by the patient.
Authors' Contributions
Both authors contributed equally to the final version of the
publication, have read, and approved the manuscript.
REFERENCES
- Rampurwala M, Pazooki M, Schauer P (2011) Delayed hepatic metastasis from a benign fibroblastic meningioma thirty-one years after surgical resection of the intracranial tumor. J Clin Oncol 29: e214-e215.
Google Scholar, Crossref, Indexed at
- Abboud M, Haddad G, Kattar M (2009) Extraneural metastases from cranial meningioma: A case report. Radiat Oncol 4: 20.
Google Scholar, Crossref, Indexed at
- Kaminski JM, Movsas B, King E (2001) Metastatic meningioma to the lung with multiple pleural metastases. Am J Clin Oncol 24: 579-582.
Google Scholar, Crossref, Indexed at
- Riemenschneider MJ, Perry A, Reifenberger G (2006) Histological classification and molecular genetics of meningiomas. Lancet Neurol 5: 1045-1054.
Google Scholar, Crossref, Indexed at
- Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, et al. (2016) The 2016 World Health Organization classification of tumors of the central nervous system: A summary. Acta Neuropathologica 131: 803-820.
Google Scholar, Crossref, Indexed at
- Nakano M, Tanaka T, Nakamura A, Watanabe M, Kato N, et al. (2012) Multiple pulmonary metastases following total removal of a bilateral parasagittal meningioma with complete occlusion of the superior sagittal sinus: Report of a case. Case Rep Neurol Med 2012: 121470.
Google Scholar, Crossref, Indexed at
- Kovoor JM, Jayakumar PN, Srikanth SG, Indiria B, Devi MG (2002) Solitary pulmonary metastasis from intracranial meningiothelial meningioma. Australas Radiol 46: 65-68.
Google Scholar
- Incarbone M, Ceresoli GL, Di Tommaso L, Cappuzzo F, InzirilloFnfante M, et al. (2008) Primary pulmonary meningioma: Report of a case and review of the literature. Lung Cancer 62: 401-407.
Google Scholar, Crossref, Indexed at
- Surov A, Gottschling S, Bolz J, Kornhuber M, Alfieri, et al. (2013) Distant metastases in meningioma: an underestimated problem. J Neurooncol 112: 323-327.
Google Scholar, Crossref
- Wang DA, Bing YI, Yan SU (2015) Recurrent intracranial meningioma with multiple pulmonary metastases: A case report. Oncology Letters 10: 2765-2768.
Google Scholar, Crossref, Indexed at
- Drummond KJ, Bittar RG, Fearnside MR (2000) Metastatic atypical meningioma: Case report and review of the literature. J Clin Neurosci 7: 69-72.
Google Scholar, Crossref, Indexed at
- Gladin CR, Salsano E, Menghi F (2007) Loss of heterozygosity studies in extracranial metastatic meningiomas. J Neurooncol 85: 81-85.
Google Scholar, Crossref, Indexed at
- He N, Zhong L, Lei K (2020) Multiple pulmonary and pleural metastases in recurrent intracranial Meningioma with genetic changes: Case report and review of the literature. World Neurosurg 136: 337-340.
Google Scholar, Crossref, Indexed at
Citation: Rim A, Alia M, Lina K and Chiraz N (2022) Recurrent Intracranial Meningioma with Pulmonary Metastases. J Neurol Neurosci Vol.13 No.1:407.