Keywords
Rehabilitation, Rheumatoid Arthritis, evidence- based practise
Introduction
Rheumatic diseases are common, most of them are chronic, some of them are serious and they are the most common chronic problems most commonly nursed in primary care. They represent the main cause of disability in ages older than 15 years. There are more than 100 different rheumatic diseases. There is no doubt that they represent one of the most important medical and social problem for the patients,
their families, the society and the economy [1].
According to a recent cross-sectional population based epidemiological study (ESORDIG) that took place in our country (total study population 10.647 people) by the Hellenic Foundation for Rheumatologic Research and several Rheumatologic clinics throughout Greece in 2003, regarding the abundance of rheumatic diseases in Greece, the rheumatic diseases are very common in the general adult population of our country. More than the ¼ of the adults suffer from an active or chronic rheumatic disease in remission [2].
Rheumatoid Arthritis (R.A.) is the main representative of the above mentioned diseases.
The main factors that have to be taken into account for the rehabilitation of people with rheumatic diseases are the restriction of the mobility and the restriction of activity. The rehabilitation uses all the methods and the technological means for the correction of the damages, emphasizing in the preservation and restoration of the function. The rheumatologist constitutes the instructor and the coordinator of a complex group that uses pharmaceutical, surgical, psychological and physical therapies. A program of this kind can lead to a successful functional rehabilitation of the patient even without the control of the process of the rheumatic disease [3].
Classification of the terms impairment, activity and participation by the WHO
In order to offer standards in the classification of disability, the World Health Organization (WHO) issued the “International Classification of Impairments, Disabilities and Handicaps” (ICIDH) in 1980. This report has been an effort in understanding and classifying the status of the people with chronic diseases. The bases of this classification haw been the fact that a situation that affects health (a disease or a disorder) is possible to cause impairment, disability or a handicap and these three situations correlates with each other. In 1988 WHO presented the ICIDH-2 version (“International Classification of Impairments, Activities and Participation”). It was WHO’s intention to use a neutral terminology, to include environmental factors and to offer a social guidance standard. The impairment still stands as it was but disability was replaced by activity and handicap was replaced by participation. With this review, a disease is possible to derive from an impairment which affects activity and participation and these three factors interact. Activity is set to be the functional level of the person and can be limited in regards to its nature, duration and quality. Participation is set to be the involvement in various procedures in life in juncture with impairments, activities, health status and relevant factors. In this new classification the restriction of participation equals disability and the restriction of activity equals handicap. The impairment has to do with the body level, the activity with the level of the whole hypostasis of the person and the participation in the society level.
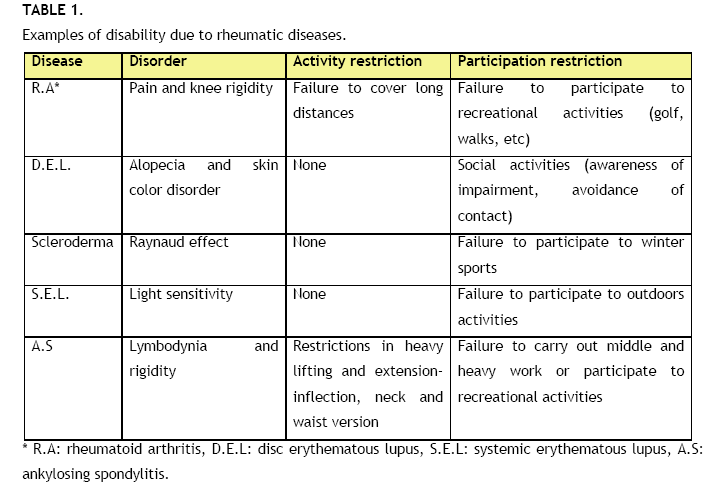
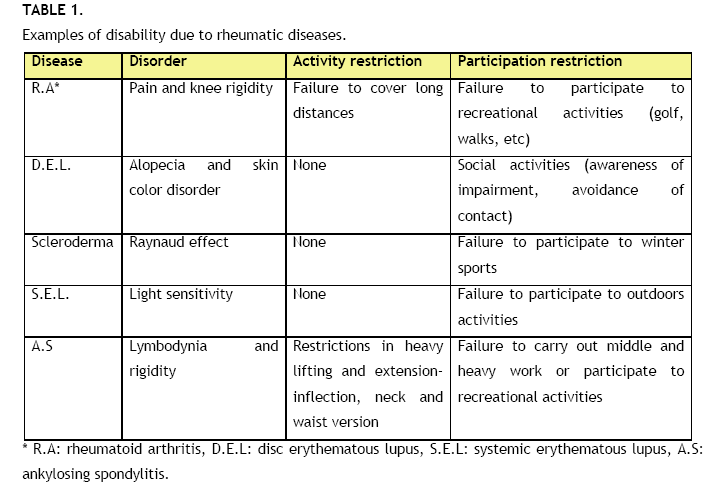
In Table 1 are shown examples of situations of functional offences caused by rheumatic diseases. In the ICIDH-2 standard the pharmaceutical and surgical treatment are impairment management-orientated and the rehabilitation treatments in the restriction of activity. The public education, the legal system and the overall architectural design should improve the restricted as it is participation of people with disabilities [3,4].
Team and placement of rehabilitation
An overall approach of health, which aims in the better patient function, should be focused not only in the recession or absence of amenable rheumatic disease, but to also take into account the individual as total, as a functional individual. A main position in this approach is the attendance of the patient with natural, psychological, community and social sides of health and feeling of well-being [5,6,7].
The possibility of the approach of the patient from a team of experts of many specialties helps in the achievement of better results. In the hospital, this team can be constituted from a rheumatologist as the instructor, ergo therapists and physiotherapists, psychologists and social psychologists, nurses of rehabilitation and orthopedics surgeons. An integral part of this team constitutes the patient himself, who should accept the responsibility of choice and achievement of realistic objectives. In the precocious disease and in patients that are monitored outside of the hospital, there is probably no need for all the specialties of the team of rehabilitation to be included. However the experience of the team is required in the complicated advanced disease when the patient is likely to be confronted with partial elements of the disease, problems of mobility, offence of activities of the daily life, development of depression, loss of profession and social insurance. The instructor of the rehabilitation team selects the suitable advisory interventions as the problems emerge, confirms the communication status between the members of the team and guides the patient in realistic objectives. [5,6,7].
The rehabilitation should begin with the first visit of the patient to the doctor and to extend throughout the course of the disease. During the precocious disease the doctor can address most of the functional problems with caution regarding the pharmaceutical treatment.
The rehabilitation can begin in the doctor’s office and with reference to the suitable healer, e.g. for problems of mobility to the physiotherapist, for the activities of daily life to the ergo therapist and for psychological problems to the psychologist. For more advanced disease, a short-term program of rehabilitation can offer more intense daily activity. The daily monitoring of the patient will allow the adaptation of the pharmaceutical program and the physiotherapy program.
In the USA the so-called "diagnostic related groups" (DRGs) direct the currently applied system of medical care and determine the amount of the compensation. This system was designed to decrease the cost of care in the USA and it looked like to achieve that. In acute diseases the compensations and the cost of health care were decreased. With regard to rehabilitation that concerns the hospitalized patients, this is not determined by the system of DRGs, but it reflects however the tendency of reduction of the hospitalization days. Currently hospitalization is required for patients with the most advanced rheumatic disease and more intense restriction of functional ability [7].
The orders of the insurance institution Medicare dictate the requirements for hospitalization and they require that only the hospitalized patients with restriction of activities of daily life and mobility, which do not respond to outside hospital treatment, are submitted to rehabilitation. The disease should be serious enough to require daily follow-up from a doctor and other health professionals. They should be offered three hours of daily treatment from two of the most major sides of program of rehabilitation, like physiotherapy, ergo therapy or speech therapy. During the hospital stay they could be offered social services and psychological rehabilitation, which are likely to contribute in the required daily treatment without being considered major therapeutic techniques.
A transient unit of in-hospital care or support by specialized nurses can be used for individuals that present important functional problems and require certain therapeutic intervention for one hour a day and not three hours of daily treatment. The abovementioned should be applied also to patients that present smaller disability, but require skilled nurses and functional education (e.g. program of intensification and education of walk after an operation of total hip arthroplastyf). The aim of the programs for in-hospital and out-hospital patients is the maintenance of the rehabilitation program from the patients themselves in the environment of their house [8].
Clinical studies showed favorable correspondence in the care from the complex team of rehabilitation comparatively with the care that is offered periodically outside the hospital. For patients with rheumatoid arthritis (RA) the improvement by the rehabilitation of internal patients was maintained for two years.
The major changes were observed two weeks after their discharge, where a statistically important improvement of the articular indicator Ritchie, the number of edematic articulations, activity of disease with visual proportional scale (VAS), estimate of the pain with the VAS and the total evaluation by the doctor, was noted. In four weeks 18% of the of patients, that was submitted in rehabilitation as internal patients, achieved improvement that was approximately 20% according to the criteria of the American College of Rheumatology (ACR 20) or better level accordingly again to ACR something that did not achieve no patient that was monitored outside the hospital. One year after the treatment the activity of the disease as it was evaluated with VAS remained statistically considerably low in the group of the patients, that were treated as internal patients, and the success of ACR 20 reached 46% in the group of in-hospital and 23% in the group of out-hospital patients [9].
Evaluation of patients
Apart of the usual history and the physical examination there is a need for an evaluation of the functional status of the patient. This information is accessed better with indirect questions, as "how is arthritis influence your life", or "describe me what you do on a usual day". Such questions give patient the opportunity to correlate the disturbance of his functional activity with the important activities for him. The patient and the health care team can use this information in order to determine the therapeutic objectives. All the members of the team should have multifaceted special information. The patients should answer with regard to the activities of their daily life, including those concerning the care and healthy (toilet) of their body, the way that prepare and receive food, the transports and the use auxiliary means, the recreational activities, like their hobbies and activities related with the profession and the care of the house. The ability of implementation of the activities that are related with the daily life may determine the disease status of the patient as independent, as having the need of supervision/help or as incompetent to execute these activities. The ability of the patient to dress himself is divided further into the ability that concerns the clothing of upper and the below parts of the body [10].
The ergo therapist will specifically report the operation of the hands (extremities) and of the upper members, in which operation the ability of capture, the force and precision of capture with the thumb and the indicator (as tongs), the handling of discs and capture of cylindrical objects are included. The physiotherapist will report activities, regarding the dressing of the torso and the functions and the mobility of the lower members, like the ability to lay down procumbent or in its side, to turn from one side to the other, to raise from the supine position to the sitting position, to move from the sitting position to the standing position, to move and to go up steps. The movement can be divided depending on whether this concerns the area of the house or the community, as well as whether it requires or no auxiliary medium or wheel chairs.
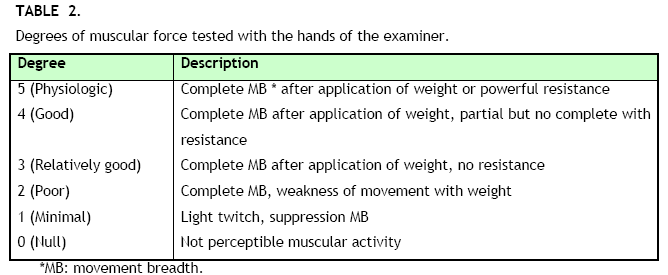
Since rheumatic diseases cause problems related mainly with the mobility, the muscular force and the breadth of the movement of the articulations, the physical examination should be directed in the evaluation of the functional ability of the patient. The test with the help of the examiner’s hands constitutes a usual way of measurement of muscular force (Table 2).
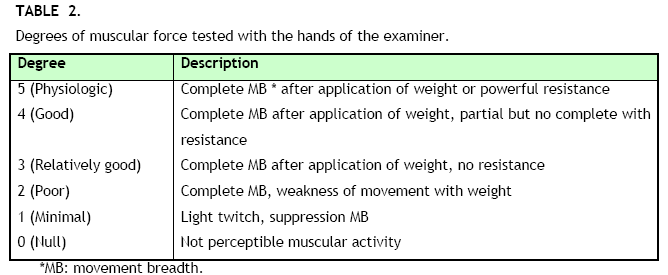
The muscular faculty is measured in a scale of 0 to 5, from not kinetic activity to physiologic muscular force. The evaluation of the physiologic force varies, depending of the sex, patient’s bodily dimensions and their exersice status. Since individuals with physiologic muscular force can lose important amount of their kinetic function before it becomes perceptible from the examiner, the breadth of movement should be measured with the help of angle gauges. Particular attention should be given in the evaluation of axis of the member that is evaluated, the presence of rigidities, instability of articulations and deformities.
There are multiple ways of recording the long-term functional status of the patient. The most common method that is used by the rheumatologists’ community is the functional classification of ACR that groups the patients on the bases of the grading scale [10,11].
Control of pain
Pain constitutes a usual sovereign infliction and causes the lack of activity and losses of functional ability in patients with rheumatoid disease. The collaboration and the success of the rehabilitation cannot be achieved if the patient is in pain. The control of the disease with classic therapeutic forms constitutes sometimes the most effective way to control the pain and to improve the activities. Additional use of intra-articular infusion of glycol-corticoids in insistence offence of articulations can control the inflammation and the pain, to prevent rigidness and improve the breadth of movement and their function.
The use of locally applied medicines (e.g. Capsalcin ointments and salicylic acid) is likely to help particularly in combination with physiotherapy and ergo therapy. The analgesics administrated by mouth, included the low doses of non steroids anti-inflammatory medicines (NSAM) and narcotics, can be beneficial when applied 20-30 minutes before the application of the physiotherapy treatment. They can be used periodically so that they allow periods of physiologic exercise or work [12].
Natural therapeutic means
Hot and cold
Of the natural therapeutic means that are referred in musculoskeletal diseases, hot and cold have the more powerful bibliographic support. They were used for centuries in the confrontation of offence of the musculoskeletal system, in the acute traumatic damages. There aren’t any evidence that their application at equitable way causes damages, there are however evidence (not argued bibliographically) to support their favorable effects, including the reduction of pain and the muscular convulsions, the increase of circulation and the improvement of the movement breadth. Changes in the temperature are observed in the skin, the deeper tissues and in certain cases in the articular cavities. Apart of the favorable effects, which were reported in clinical situations, there are experimental evidence in models of animals on decreased correspondence in the pain in hot and cold stimuli, in inflammatory arthritis. Hot and cold don’t alter the articular inflammation, but improve the secondary answer in the pain and the behavior [12].
A systematic examination of the medical bibliography regarding to the application of hot and cold shows that there are minimal tested studies of acceptable quality, particularly regarding the fortuity and the application of placebo treatment. However of the studies that fit these criteria, hot and cold do not affect the activity of disease, as it was evaluated objectively, included the inflammation. All the patients reported that they prefer hot or cold comparatively with the absence of this treatment, without a certain particular preference between those. Due to the fact that this treatment has no damaging effects, it should be recommended for treatment at home, when there is a need for alleviation from the pain.
The treatment with hot is offered with the form of surface application of hot pads, electric hot-water bottles, water baths, paraffin baths or simple hot-water bottles. The use of water or whirl baths can be combined with energetic or passive movement so the breadth of movement is improved. Hot pads contain chemical substances that produce heat, when they are activated with exothermal reactions. They do not have advantages over the electric hot-water bottles or the application of liquids hot pads, they have however the disadvantage regarding the time of use and their increased cost. The application of hot is not advisable in case of loss of physiologic sensitivity and reduction of arterial circulation or venous blood abduction.
The presentation of hot deeper in the tissues can be achieved with the use of therapeutic ultrasounds. There aren’t tested studies that show their usefulness in rheumatic diseases, they however have the disadvantage that they should be applied in a special area by specialized personnel, a fact that increases the cost and complicates the daily life of the patient.
Cold decreases the pain and the muscular convulsion. It also leads in vasospasm which results in the reduction of tissue metabolism, inflammation and edema. Due to these effects it constitutes the classic treatment for direct care after a traumatic damage of the musculoskeletal system. It is locally applied for a time of 30 minutes, causing reduction of the temperature of the skin and subcutaneous tissues. Such reduction of the temperature is observed in deeper tissues and it depends from the duration of the application of cold and the depth of these tissues.
Typically, cold is applied with the form of cold pads, pads with gel, pads that contains chemical substances or ice massages directly onto the painful region. The pads that contain chemical substances produce cold with endothermic reactions have little usefulness because of their big cost and the time that they require. Cold sprayings, as chloride ethyl, are used in the Rheumatology in combination with the application of muscular distention, especially regarding to the painful syndromes of the neck and the back. In the skin they cause reduction of the temperature leading to alleviation from the pain and the muscular convulsion, a fact that allows the application of passive distention [13].
Electrical stimulation
The trancutaneous electrical nerve stimulation (TENS) can be used for the management of pain in patients outside the hospital. A low potential electric stimulus is transported in the skin in a periodical or continuous manner after the activation of the appliance, which can be sustained in the patient’s belt and functions with batteries. The patient can activate and regulate the intensity of the stimuli depending on his needs. TENS is applied for non inflammatory situations, particular chronic rachialgia due to osteoarthritis (OA), pain in the knee, chronic pain in the shoulder or pain in other major articulations of body. It is usually recommended in patients that are hardy in the application cold, hot, distention, exercise and other methods of physiotherapy. It is used commonly but there aren’t however tested studies that would certify its favorable effect [14].
Hydrotherapy
Hydrotherapy combines the treatment with exercise and the buoyancy of hot water. The progressive application outside the hospital or as a part of a therapeutic form with the form of spa therapy can be recommended. There are just a few tested studies for this treatment. There are however some references that the individuals that were submitted in hydrotherapy regularly outside the hospital, had benefited comparatively with the individuals that were treated bathing into water in the sitting position, with floor exercises or with relaxation treatment. This improvement was bodily and sentimental, as it was revealed by the questionnaire AIMS-2 that was applied. A more extensive systematic examination of the published bibliography with regard to the spa therapy showed several weaknesses like the planning of the treatments, with minimal use of measurements for the evaluation of the results, like the use of tools (calibration systems) that evaluates the change in the quality of life. The conclusion of this examination was that the spa therapy cannot be supported as an effective treatment [15].
Rest
The local or systematic immobilization decreases the inflammation and the pain and promotes the physiologic place of articulation. Local immobilization is achieved with the use of splints or “chaperon” and with pressure sore. Short periods of immobilization as parts of a complete program help the patient to participate in exercise programs and activities in his workplace. However extended immobilization, local or systematic, should be avoided due to fact that it results to important loss of muscular mass. After just a few weeks of local immobilization, a reduction of muscular mass of 21% can be observed and there are references that show that the extended pressure sore as a fundamental treatment does not help and should not be recommended as the routine treatment. Certain situations, included the acute lumbago, they are likely to be worsened with pressure sore [16,17].
Treatment with exercises or kinesitherapy
In its application it should is be taken into account the activity of the amenable disease, included the degree of inflammation, the instability of the articulations, the muscular atrophy and short- and long-term functional objectives, have to be anticipated. The exercises that would be applied can be energetic or passive, abetted or aerobic.
The passive exercises, included the exercises of distension and those of soft handlings for the increscent of the breadth of the movement, should be applied by a physiotherapist aiming to maintain the elasticity of the articulations and to restrict the rigidities. The passive exercises are applied in situations that correlate with severe pain and weakness, like the acute articular inflammation, inflammatory myopathy and postoperatively periods. The isometric exercise, during which energetic muscular twitch without shortening of the muscular length or movement of articulation are observed, helps in the maintenance of muscular force and it is recommended as an initial treatment in individuals that do not tolerate exercises of mobilisation in complete breadth of movement because of pain, like individuals that were recently submitted in arthroplasty [18,19,20].
Most individuals with a rheumatic disease are profited by programs of exercises of resistance and aerobic exercises. The exercises of resistance should be adapted in the situation of each patient, the region of body that presents muscular weakness and the amenable disturbance, aiming in the increase of muscular force and resistance.
Walking exercises and resistance are recommended for one hour three times a week and correlate with less pain, smaller disability and bigger force of bending in individuals with OA in the knee. Similar effects are presented by the patients with OA of the hip. In its results, mild to mediocre improvement of pain, improvement of functionalism and profit as for the opinion of patients, are included.
The treatment with exercises in individuals with RA improves the aerobic ability and the muscular force without deterioration of pain or activity of disease.
In ankylosing spondylitis the recreational exercise of 30 minutes at least per week improves the pain and the stiffness. Exercises of the back for five days per week improve the situation of the health, as it was measured with the HAQ Disability Index. The outmost profit was observed in individuals with precocious disease [18,19,20].
In patients with systemic erythematous lupus the intensification exercises and the aerobic exercises did not worsen the activity of the disease and were accompanied by reduction of lassitude and improvement of the functional status, muscular force and status of the cardiovascular system [21,22].
Auxiliary means for walking
For the improvement of walking and the alleviation of muscular weakness, pain and instability of the lower members, walking sticks, special canes and walkers are recommended. The most useful walking sticks are manufactured by timber or aluminium. They should not be expensive, they should be light-weighted, to be easily adapted to the patients stature, they have to have a comfortable handhold and a wide rubber supportive base. The length of the walking stick should be selected so that it’s kept with the elbow in a bending position of 30 degrees. With the use of a walking stick or a cane from only the one side of the patient, it can be transported up to 25% of the normal load of the body weight from the feeble or painful articulation of the opposite leg. With bilateral support, up to 100% of the weight can be transported from the painful lower member in the upper members. Certain patients, that have selected to carry a walking stick, they don’t use it or support but as a point of indication towards the others, that they have kinetic problems [23,24].
Patients need guidance for the right use of their walking aid. Only one means of support is transported into the opposite from the painful side, foot and it is used so that it raises the weight during the time that the body leans in the opposite (painful) leg. Walking sticks with multiple support offer increased safety in individuals with offence of proprio sensitivity or with balance problems. For individuals, that should not load the their wrist or present important deformities in their hands, the auxiliary means should be adapted so to facilitate these problems with reception of support in the elbow, with suitably shaped handholds and with Velcro straps. In order to avoid excessive load to the wrists and the hands they should be adapted in the elbow in a bending position of 90 degrees.
The canes are recommended for more serious problems and they offer support, when they are used by both sides of the patient’s body. They are more useful in the postoperative period and in acute disease or trauma, as they allow minimal or none load in the feeble or painful leg. They should be adapted in a manner so that the pressure in the armpit is avoided. The patients should be guided with regard to the way that they hands and upper members can raise the weight in the right way with their wrist and elbow extending. The canes with a platform should be recommended in individuals with severe arthritis of the wrist and upper members that presents the pain during the use of the usual cane [24].
For individuals in need for more assistance in their walking the walkers offer a wider base of support than the walking sticks and canes. They are also useful in the postoperative period with regard to old patients with instability, as well as patients that need wider support for balance. They should be light in order to be lifted off and moved easily. For comfort and safety moving seats with brakes, may be used. Wheel chairs can improve the independence and the social contact, when the mobility of patient is limited in the indoors level. A wheel chair moved by the patient’s hands is recommended in individuals with physiologic operation in the upper members and sufficient force for his movement. The wheel chairs that can be moved with the help of the patient’s members of the family may be recommended in the postoperative period, as well as for feeble old patients, where they do not wish to move by themselves. Electrically driven chairs should be recommended to patients with not satisfactory operation in the upper members [23,24].
Auxiliary means of the upper members
A wide variety of auxiliary means commercially available can improve the activities of daily life of individuals with disturbances of operation of their upper members. The ability to capture and the ability to capture and hold like a tong with the thumb and the indicator can be improved with the use of suitable handholds in various tools, utensils of cooking and uptake of food (knives, forks, spoons etc). Appliances supplied by electric power, as electric knives and tools, can replace the usual instruments in individuals with reduced ability of capture and not satisfactory force of their upper members. One can use special appliances for the capturing of objects from the floor and the selves. Brushes with long handholds, combs and sponges can help in the body hygiene and the cleanness of the perirectal area [23].
The clothing can be facilitated by fabric connectors with films, special buttonholes, clothes and shoes with Velcro closings, trousers with flexible backs and jumpers with V necks. The putting on of socks and shoes is facilitated with suitable structures of long handholds, while most helpful have proven to be bars for the clothes to patients with problems in the mobility of their shoulders.
The safety and comfort in the house can be evaluated during the visits of physiotherapists and ergo therapists. People with problems of mobility can be facilitated with steps of half from usual height, with side supports (ramps) and handgrips in the beginning of the scales. The doors should be as wide as for the patient to have an easy pass through them either on foot or in a wheel chair. The placement of the furniture and the size of a room should allow the easy transfer of the patients with auxiliary means and with wheel chairs. Electric wires (cables, etc.) should be removed. For patients with problems in their knees and hips, the height of the seats can be increased with additions under the feet of the chairs or with the placement of cushions of four inches thickness (4x2,5cm = 10cm), of high density foamy material. The raised seats in the basin of the toilet facilitate the seating and the raising of it. Elements from rubber in the bathtub and in the basin of the bathroom, improve the ability of the patient to seat and to be lifted off by supporting themselves in them and also they anticipate the falls. Over the side handholds and supports, as well as seats in the basin of the bathroom should be used from individuals with balance problems. The washing of the body is facilitated by a suitable handhold in the shower [23].
Lifting up structures
The splints and the chaperons can improve the stability and decrease the pain and the inflammation. However due to the fact that they limit the mobility, it recommended that their application should be short termed in order to maintain the muscular force. Splints for the upper members are more frequently used and they are more acceptable by the patients and doctors. Even though they limit the pain and the inflammation, there aren’t studies to support that they can anticipate the development of deformities.
Wrist splints are likely to decrease the operation of the member (as this it is measured by the improvement of the capturing ability), the ability of the fingers and the member, at least in the short term. People with severe deformities it is likely that they are going to need the advisory intervention of an expert for the lifting up structures or of an ergo therapist with regard to the use of usually manufactured lifting up structures.
Splints that immobilize the wrist in a neutral position, with an extent of 20-30o of the upper members up to wrist, are used in the syndrome of the carpal pipe. For flexible deformities of the swan neck type of the fingers, a splint with the form of a ring facilitates the force of capture as tongs and the precision of the movements, placing the close medium phalanx articulation in light bending and a more functional position. The splints in the form of a ring are not effective in deformities that cannot be lifted with the hands of the examiner, and there aren’t studies to support their extended use in the prevention of the development of such deformities. These splints can be manufactured of silver in order to be elegant and to become more acceptable by the patients.
The splint of immobilization of the carpometacarpal (KMK) articulation of the thumb decreases the pain in patients with degenerative arthritis in this articulation in the periods of elevated pain in the base of the thumb. They impede however activities that increase the load of the KMK articulation, like in the case of capture as tongs between the thumb and the indicator. In the strategies of reduction of such loads, the use of increased size of pencils and pen with rubber or foamy material handholds and light handholds of objects of writing is included. For the immobilization, casts of glass fibers can be used or even of thermo plastic material. If this immobilization leads to reduction of pain, then a costlier constant lifting up structure (chaperon) or a chirurgical binding of the articulation can possibly decrease the pain and improve the function [23,24].
Lifting up structures of the lower members
Flexible bandages, flexible or neoprene splints and bandaging are the simpler chaperons for the restriction of the movement breadth and the reduction of pain in the lower members. A lot of patients with OA in the knees ease themselves and they improve their foot function using splints that decrease their breadth of movement. For individuals with arthritis of the kneecap articulation and irregular movement of the kneecap, the knee bandaging improves this movement and decreases the pain in the knee in 25% of the patients comparatively with the standards.
For individuals with marked muscular weakness and deformities, the advisory intervention of an expert in the lifting up structures or of an orthopedic surgeon with training in vital mechanics, can offer a lot. Larger and more extensive immobilizations with proportional sized chaperons are expensive and can not be easily adapted by the patients [23].
Footwear
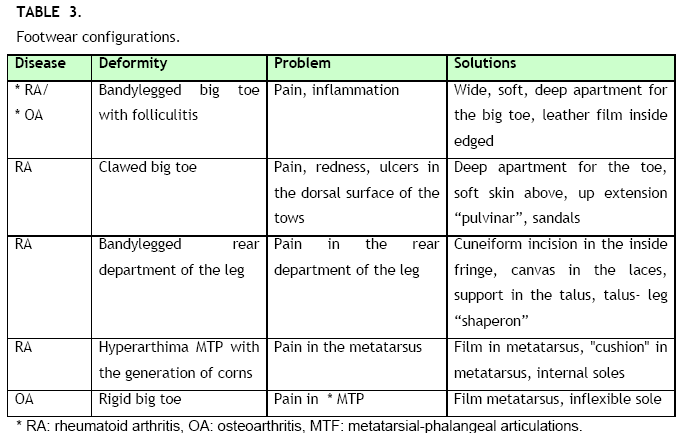
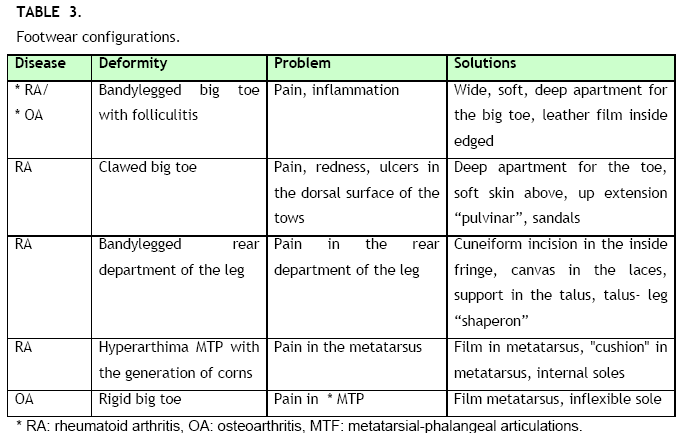
The pain and the deformities of the lower feet are a usual situation in the RA and the OA. Many such problems can be treated sufficiently with careful configuration of footwear. Their upper department should be soft and have comfortable space for the toes that they present deformities, measures that can prevent splint, friction and the bruising of the skin of the lower feet.
A lot of patients with RA present pain in the soles, especially in the regions of the metatarsus. The appearance of clubbed fingers in the big toe, falling of the heads of the metatarsus with anterior ectopia of the fatty body, deformities that can cause pain in the metatarsus along with generation of callus and fissions of the skin, are usual. These problems can be avoided using intentions, "cushions" in the heads of the metatarsus in the internal sole of the footwear or exterior addition of film close to the heads of the metatarsus. Insertions ("insoles") from high density polypropylene, that are commercial available are likely to constitute satisfactory treatment of the pain in the metatarsus and the painful bone ledges. In insistent symptoms, the patients should be referred to an expert in the lifting up structures for the choice of more suitable insertions available in the market for footwear or in the manufacture of special footwear with thermo plastic material. The use of sandals and insertions from thermo plastic material can offer painless transfer for the patient [24].
Professional rehabilitation and disability
Musculoskeletal diseases constitute sovereign causes of disability and absence from the work (days off work) in the USA. The RA is combined with high frequency of disability, as the one third of the individuals, that works and has developed RA, is unable henceforth to work after five years. Three years after the diagnosis of systemic erythematous lupus, 40% of the patients cannot work any longer. One of the objectives of rehabilitation is the maintenance of the professional employment by the patients. The achievement of this objective requires modification of the working conditions, reeducation and professional rehabilitation. Amongst the individuals with arthritis and disturbances of the musculoskeletal system, up to 71% of those that have professional rehabilitation, return to work.

The insurance compensations for the disability constitute the main obstacle for satisfactory professional rehabilitation. Amongst the individuals with RA, the high intensity of pain, the age and the lower level of education constitute obstacles for the redefinition of the professional employment. For individuals suffering from systemic erythematous lupus, the low level of education, the compensation from the insurance institution Medical in the USA, the absence of medical insurance cover, the employment in professions that require intense bodily effort, the level of poverty and the more prominent activity of the disease, constitute prognostic factors of precocious disability at work. The race, the sex, the total offence of the organs and the duration of the disease cannot forecast the appearance of work disabilities [24].
Social Security Administration manages the uniformly shaped program of disability throughout USA. There are two programs out of which the patients can select: the Social Security Disability Insurance (SSDI) and the Usual lifting structures of the upper members.
Social Security Insurance (SSI). For the SSDI the patients should fulfill the requirements of the determination of disability and have been already compensated by the system of Social Security with a required time usually up to 40 quarters. For the choice of SSI the patients should present disability and decreased incomes, but do there isn’t any requirement about their job. In the system frame the disability is determined by law and basically means weakness of implementation of any type of work, regardless of the previous profession or the professional experience. As disability is set to be the "weakness of occupation in any successful activity because of one (or more) medical determinable bodily or mental offence, that is expected to lead to death or has lasted or expected to last for a continuous period of at least 12 months.
As soon as a decision is made on the demand of disability confrontation it should be dispatched in the offices of the institution a long-term and argued information, that would show the effect of the disease in the disturbance of functional ability and the ability to work. For the system cover the patients fill in forms in the local offices of the institution. The application is supervised so as to verify that the patient fulfills the terms that are determined for the definition of disability. If this is not the case, then additional information by the patient and his doctor is required. It is likely that an examination by an experienced clinical doctor or psychologist that is remunerated by the institution will be demanded. If the terms are again not satisfied then the patient can refer to juridical hearing, where he should answer about the way that his rheumatic disease influences his life and his ability to work. He can adduce additional medical information, call witnesses and a lawyer who will interpret the legal sides of disability. When it is decided that the patient fulfills the terms, then the compensation is determined by law. Apart from the monthly compensations, the individuals that have SSI are covered immediately by Medicaid. The individuals that have SSDI are covered by Medicare after two years [25].
Conclusion
Patients suffering from Rheumatoid Arthritis should have a complete phychosocial support, all of us should be their family, we have to fight all the time for their rights, their social rehabilitation as well as for their professional rehabilitation.
3669
References
- Andrianakos A., Trontzas P. «Prevelance of Rheumatic diseases in Creece. A cross-sectional population based epidemiological study. The ESORGIC study. Iatriki 2003,84(3-4):188-206
- Guidelines for the Management of Rheumatoid Arthritis. American College of Rheumatology.2002; Vol.45, No.2 :328-346.
- Backman L. Catherine . “Psychosocial aspects in the management of arthritis pain”. Arthritis Research and Therapy 2006 8:221.
- Bradley L., Alberts. K . «Psychological and Behavioral Approaches to Pain Management for Patients with Rheumatic Diseases». Rheumatic Disease Clinic of North America,1999. Vol.25(1).
- Chorus A.M.J.. « Quality of Life and work in Patient with rheumatoid arthritis and ankylosing spondylitis of working age ». Ann.Rheum.Diseases, 2003;62 :1178-1184.
- Saralynn H. Allaire « Reduction of job Loss in Persons with Rheumatic Diseases Receiving Vocational Rehabilitation. A Randomized Controlled Trial». American College of Rheumatology. Arthritis & Rheumatism.2003; Vol.48, No.11: 3212-3218.
- Register C. : Living with chronic illness, Bantam Books, New York. 1987.
- Katz P.P., Morris A., Yelin H.E. “Prevalence and predictors of disability in valued life activities among individuals with rheumatoid arthritis”. AuuRheum Dis 2006; 65: 763-769.
- American College of Rheumatology Subcommittee on Rheumatoid Arthritis Guideline. “Guidelines for the Management of Rheumatoid Arthritis 2002 update”. Arthritis & Rheumatism. 2002; Vol.46, No.2:328-346
- Savelkoul M., Post MW, de wittclP., Vau den Borne Hb. “Social support, coping and subjective well-being in patients with Pneumatic Diseases” Patient Educ.Counsil. 2000;39(2-3) : 205-218.
- Daltroy LH.. “Doctor – Patient Communication in rheumatologic disorders”. Baillieres Clin. Rheumatology. 1993; 7(2): 221-239.
- Hammond Alison «Rehabilitation in rheumatoid arthritis: A Ctirical Review». Musculoceletical Care. 2004; Vol.2(3):135-146.
- Piccini Armando, Maser D. Jack . « Clinical significance of lifetime mood and panic – agoraphobic spectrum symptoms on quality of life of patients with Rheumatoid arthritis ». Comprehensive Psychology.2006; 4:201-208.
- Abdel-Naser, Abdel- zim «Depression and depressive symptoms in rheumatoid arthritis patients: an analysis of their occurrence and determinates» Rheumatology. 1998; Vol 37 (4) :391-397.
- Andrianakos A. ,&Voudouris K. "RHEUMATOLOGY" Greek Institution of Rheumatologic Researches. Medical Publications: P.H. Paschalidis. Athens, 2005.
- Barlow JH., Turner AP., Wright CC.A randomised controlled study of the arthritis self – management programme in the U.K. Health Education Research. 2000;15(6): 665-680.
- Astin JA., Beckner W., Soeken K., Hochberg MC., Berman B. Psychological interventions for Rheumatoid Arthritis: A meta-analysis of randomised contolled trials. Arthritis and Rheumatism 2002; 47(3):291-302
- BSRM: British Society of Rehabilitation on Medicine. Vocational Rehabilitation: The Way Forward. London: British Society of Rehabilitation on Medicine. 2000;1-107
- Covic T, Adamson B, Hough M .The impact of passive coping on rheumatoid arthritis pain. Rheumatology. 2000; 39:1027-1030.
- De Buck PDM, Schoones JW, Allaire SH, Vliet Vlieland TPM . Vocational Rehabilitation in patients with chronic rheumatic diseases. A systematic Literature Review. Seminars in Arthritis and Rheumatism . 2002;32:196-203
- Fries JF, Carey C McShane DJ . Patient education in arthritis: A randomised controlled trial of a mail-delivered program. Journal of Rheumatology.1997;24(7):1378-1383.
- Hammond A, Young A, Kidao R. A randomised controlled trial of occupational therapy for people with early rheumatic arthritis. Annuals of the Rheumatic Diseases. 2004;63:23-30
- Van den Ende CHM, Vliet Vlieland TPM, Munneke M, Hazes JMW Dynamic exersice therapy for treating rheumatoid arthritis:(Cochrane Review). In the Cochrane Library. Chichester, U.K.: Wiley. 2003.
- Vlie Vlieland TPM. Rehabilitation of people with rheumaroid arthritis.Best Practise and Research. Clinical Rheumatology.2003; 17(5):847-861.
- Woodburn J., Barker S., Helliwell PB . A Randomised controlled trial of foot orthoses in rheumatoid arthritis. Journal of Rheumatology. 2002; 29(7):1377-1383