Keywords
Mental disorders; Compulsive eating; Body weight; Addiction; Eating disorders
Introduction
Overweight/obesity is a public health problem that affects about 2 billion adults and 41 million children [1]. It is the result of reduced physical activity and excessive consumption of high energy foods [2]. The etiology of obesity, however, is far more complex than simply an imbalance between energy intake and energy output; this comes from a set of metabolic and behavioral factors with genetic, endocrine and environmental origins [3-6]. Predisposing environmental factors for obesity can be complex because eating behavior and healthy habits can be influenced by psychosocial, emotional, socioeconomic and cultural conditions [7-9]. Moreover, eating behavior can also be regulated by the hypothalamic centers responsible for controlling homeostasis of food intake, which can often be altered in individuals with obesity [10].
The increase in consumption of hyper palatable foods causes impulsivity over food intake [11]. These foods may contain excess sugar, fat, and calories and activate reward systems in the central nervous system (CNS), leading to hyperphagic behavior [12,13]. The increase in BMI has been associated with the consumption of palatable foods [14]. Boggiano [15] showed an increase in a preference for palatable foods in individuals with obesity and overweight as opposed to eutrophic individuals.
Excessive consumption of palatable foods has also been associated with compulsive behavior, reduced inhibitory control and activation of reward pathways characterize FA [16]. Associated with this, a greater presence of these symptoms has been observed in psychiatric patients [17]. In a study conducted with the female population, the presence of depression and impulsivity was associated with a greater desire for sweet foods, leading to uncontrolled eating [18]. It was also observed that these changes were mediated by changes at the peripheral and central levels, such as changes in leptin expression. In addition, another study noted that impulsivity was related to a sedentary lifestyle and greater preference for high-calorie meals, leading to an increase in overweight and obesity [19]. Thus, changes in inhibitory control and symptoms of depression have been responsible for the development of FA [20].
For the evaluation of FA, the Yale Food Addiction Scale (YFAS) is a sound tool for identifying signs of addiction towards certain types of foods (e.g., high fat and high sugar) [21]. Gearhardt, White, Masheb, Morgan, Crosby and Grilo [22] used YFAS to assess the presence of FA and found that 57% of patients engaged in binge eating and suffered from symptoms of depression. Pedram, Wadden, Amini, Gulliver, Randell, Cahill, Vasdev, Goodridge, Carter, Zhai, Ji and Sun [23], found that BMI, weight, hip and waist circumferences were positively associated with FA. Furthermore, the symptoms found by YFAS have been positively associated with subcutaneous adipose tissue, hunger and chronic stress [24]. In addition, FA has been reported to be responsible for the association between the development of obesity in patients with attention deficit hyperactivity disorder [25].
The notion that FA may be a factor associated with the development of obesity and that psychiatric disorders may mediate this relationship is biologically plausible. Obesity has already been associated with the reward circuit [26], hedonic excesses [27] and compulsive eating disorder [28], demonstrating the establishment of a neurobiological dependence on food. However, the epidemiologic evidence linking obesity to FA and its associations has not been critically reviewed. The main aim of the present study was to demonstrate the relationship between overweight/obesity, depression, impulsity and FA.
Materials and Methods
This systematic review is reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [29].
Search strategy
The search for studies in the scientific literature began in July 2019, using the following databases: PubMed, Science Direct and Scielo. The terms used in the search strategy were: Obesity, overweight, food addiction (FA), food addictions, compulsive eating, depression and impulsity. Changes were made to the search strategy depending on the database used. Studies published between 2009 and 2019 were selected.
Study Selection
Articles were included if they fulfilled the following PICOS criteria (Population: Adults, adolescents and children; Intervention/ exposure: FA; Comparison: Not FA; Outcomes: Overweight/ obesity, depression and impulsivity; Study Design: Cross-sectional and clinical trials studies) [29].
After the removal of duplicates, to determine eligibility for inclusion in the review, titles and abstracts of identified studies were assessed by two independent reviewers using an inclusion criterion: Full text available, articles are written in English, use of YFAS (reference method for FA analysis), assessment of the diagnosis of depression and/or impulsivity, performed in human studies and any age. Exclusion criteria: Reviews, opinions, letters, other languages, animal or experimental studies, no use of YFAS. For quantitative analysis (meta-analyzes), those that showed the percentage or number of study participants were included. For meta-analyzes, studies that did not have control and/or exposure groups and without mean and standard deviation values were excluded.
Data extraction
The selected abstracts were submitted to the second stage of analysis, in which two other independent researchers reviewed the articles completely and, by consensus, excluded articles that did not meet the criteria. Data from articles considered eligible were extracted regarding characteristics of the sample (mean age, distribution between genders, the prevalence of FA), methodology (assessment by the FA scale), and the main results found. The data used in each of the studies meeting the criteria was then processed by a standardized method. Data extracted from the articles were performed by a standardized method among the authors. In the case of quantitative analysis (metaanalyses) studies, those that showed the percentage or number of study participants were included. For review studies, casecontrol, case reports that did not present data corresponding to the subject evaluated were excluded. For meta-analyses, studies that had no control and/or exposure groups and no mean and standard deviation values were excluded.
Quality assessment and risk of bias
The selected studies were evaluated by two reviewers using a standardized tool [30]. The quality criteria evaluated eight items, which include: the method of sample selection, ways of dealing with confounding factors, reliability of outcome measures, and statistical analysis. Each item was classified as present (‘Yes=Y’), absent (‘No=N’) or unclear (U) for each included study [31-78]. The studies were classified as "positive quality", where the studies obtained a "yes" for questions of validity and had a score of ≥ 8. Neutral or negative quality studies were those in which most of the nine responses to the quality criteria were "no" (Table 1).
Table 1. Critical appraisal results for included studies using the Joanna Briggs Institute.
| Study |
Q1 |
Q2 |
Q3 |
Q4 |
Q5 |
Q6 |
Q7 |
Q8 |
| Ahmed et al [32] |
Y |
Y |
Y |
Y |
U |
U |
Y |
Y |
| Benzerouk et al [64] |
Y |
Y |
Y |
Y |
N |
U |
Y |
Y |
| Blume et al [65] |
Y |
Y |
Y |
Y |
N |
U |
Y |
Y |
| Brunault et al [62] |
Y |
Y |
Y |
Y |
N |
U |
Y |
Y |
| Burrows et al [58] |
Y |
Y |
Y |
Y |
U |
U |
Y |
Y |
| Ceccarini et al [66] |
Y |
Y |
Y |
Y |
Y |
N |
Y |
Y |
| Chao et al [67] |
Y |
Y |
Y |
Y |
N |
U |
Y |
Y |
| Davis et al [68] |
Y |
Y |
Y |
Y |
N |
U |
Y |
Y |
| Eichen et al [69] |
Y |
Y |
Y |
Y |
N |
U |
Y |
Y |
| Filgueiras et al [70] |
Y |
Y |
Y |
Y |
N |
U |
Y |
Y |
| Gearhardt et al [22] |
Y |
Y |
Y |
Y |
U |
U |
Y |
Y |
| Gearhardt et al [71] |
Y |
Y |
Y |
Y |
N |
U |
Y |
Y |
| Guzzardi et al [72] |
Y |
Y |
Y |
Y |
N |
U |
Y |
Y |
| Hsu et al [42] |
Y |
Y |
Y |
Y |
N |
U |
Y |
Y |
| Imperatori et al [73] |
Y |
Y |
Y |
Y |
U |
U |
Y |
Y |
| Imperatori et al [74] |
Y |
Y |
Y |
Y |
N |
U |
Y |
Y |
| Imperatori et al [43] |
Y |
Y |
Y |
Y |
U |
U |
Y |
Y |
| Imperatori et al [75] |
Y |
Y |
Y |
Y |
N |
U |
Y |
Y |
| Ivezaj et al [39] |
Y |
Y |
Y |
Y |
U |
U |
Y |
Y |
| Kozak et al [34] |
Y |
Y |
Y |
Y |
N |
U |
Y |
Y |
| Lee et al [35] |
Y |
Y |
Y |
Y |
Y |
N |
Y |
Y |
| Masheb et al [44] |
Y |
Y |
Y |
Y |
Y |
N |
Y |
Y |
| Meule et al [16] |
Y |
Y |
Y |
Y |
N |
U |
Y |
Y |
| Meule et al [63] |
Y |
Y |
Y |
Y |
N |
U |
Y |
Y |
| Mies et al [40] |
Y |
Y |
Y |
Y |
U |
U |
Y |
Y |
| Ouellette et al [76] |
Y |
Y |
Y |
Y |
N |
U |
Y |
Y |
| Pedram et al [3] |
Y |
Y |
Y |
Y |
N |
U |
Y |
Y |
| Rodrigue et al [46] |
Y |
Y |
Y |
Y |
N |
U |
Y |
Y |
| Schulte et al [41] |
Y |
Y |
Y |
Y |
U |
U |
Y |
Y |
| Steward et al [38] |
Y |
Y |
Y |
Y |
N |
U |
Y |
Y |
| Tompkins et al [77] |
Y |
Y |
Y |
Y |
N |
U |
Y |
Y |
| VanderBroek-Stice et al [37] |
Y |
Y |
Y |
Y |
N |
U |
Y |
Y |
Y: Yes; N: No; U: Unclear; Q1: Have the criteria for inclusion in the sample been clearly defined?; Q2: Were the study subjects and context described in detail?; Q3: Was exposure measured in a valid and reliable manner?; Q4: Were objective, standard criteria used to measure the condition?; Q5: Confounding factors have been identified?; Q6: Were strategies addressed to deal with confounding factors?; Q7: Were the results measured in a valid and reliable way?; Q8: Was appropriate statistical analysis used?
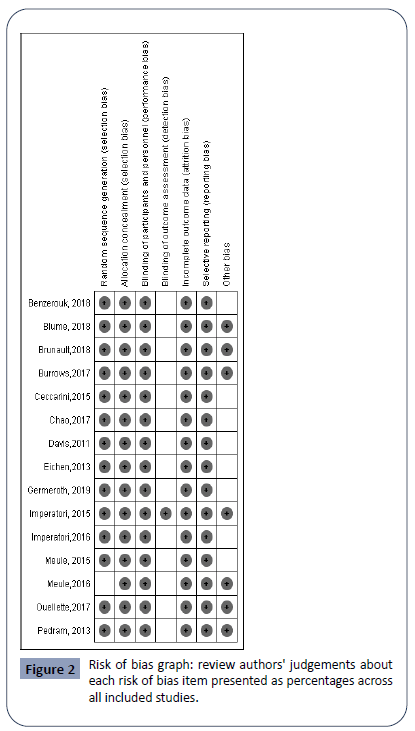
The risk of bias was established through of a critical analysis of the studies selected using seven criteria for a methodological judgment supplied by the software Revman 5.3.0 program [the Cochrane Handbook [31], developed for systematic reviews and available for free download (http//ims.cochrane.org/revman/download)]. Among the criteria that structure the bias assessment are (1) Random sequence generation, (2) Allocation concealment, (3) Blinding of participants and personnel, (4) Blinding of outcome assessment, (5) Incomplete outcome data, (6) Selective reporting and (7) Other bias.
Statistical and meta-analysis
The studies selected for meta-analyses were those that presented values of the MD accompanied by the standard deviation (SD) and the sample number (n) and using the fixed 95% for Confidence Interval (CI). In addition, random effects were used. We assessed heterogeneity with measured inconsistency (the percentage of variation across studies included due to heterogeneity) of across FA effects using I² proposed by [31]. The significant level was set at p<0.05 for all analyses. For all meta-analytical procedures, we use the software Review Manager 5.3.0.
Results
Study selection
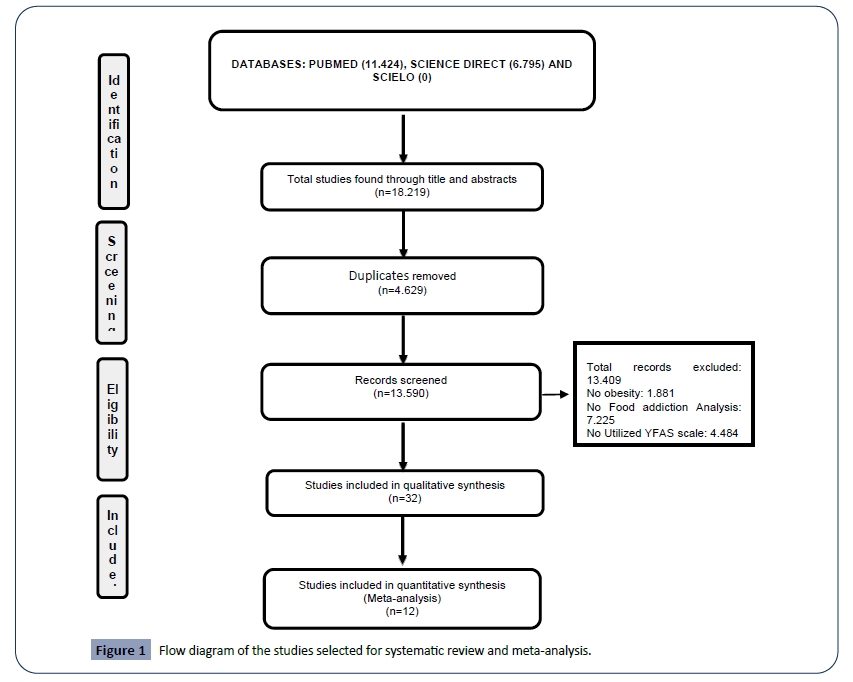
The flowchart in (Figure 1) shows the successive steps taken to select studies for the present research. A total of 13590 titles and abstracts were selected initially, 13409 were excluded because they did not comply with the eligibility criteria or were duplicated. Primary reasons for exclusion included: subjects with not affected with obesity (n=1881 articles), studies with no FA analysis (n=7225 studies) and studies that did not use the YFAS scale (n=4484 studies). Most included studies used a crosssectional analysis (n=30 studies) and two used experimental analysis (Table 2). Following the removal of duplicate references and the assessment of articles using the predefined inclusion criterion, 32 relevant articles were identified and included. For meta analysis, only 12 studies were included since the others (n=20) did not present the necessary quantitative data.
Figure 1: Flow diagram of the studies selected for systematic review and meta-analysis.
Table 2. Description of included studies after the literature search and main results on FA, overweight/obesity and psychiatric disorders.
| Author, year |
Type of study |
Number of participants |
Population studied |
Gender (Female/Male) |
Nutritional Status |
FA examination |
Other eating disorder outcome |
Prevalence of FA |
FA and BMI outcomes |
FA, depression and impulsivity outcomes |
| Ahmed et al [32] |
Cross-sectional |
401 |
Adolescents mean age was 13.98 ± 1.93 year and ranged from 11–18 years |
221/180 |
Thin (8) Eutrophic (133) Overweight (93) Obesity (167) |
Yale Food Addiction Scale for children (YFAS-C) |
34 (27.4%) of the individuals with probable BE and clinical BE 26 (33.8%) presented FA |
81 |
Among individuals thin, eutrophic and overweight, there was no difference regarding BMI and presence of FA. However, individuals with obesity (64.2%) with FA had higher BMI when compared to the group with obesity. p=0.000 |
- |
| Benzerouk et al [64] |
Cross-sectional |
128 |
Childhood: < 12 years; Adolescence: 12 - 18 years;
Adulthood: = 18 years |
91/37 |
Obesity (128) |
YFAS 2.0 |
- |
32 |
There was no difference between BMI of patients who had or did not have FA (t=-0.58; p=0.56) |
Depression disorder (53,1%; ?2=12.18; p<0.001) was higher in patients with FA. |
| Blume et al [65] |
Cross-sectional |
88 |
Adults: 18-60 years of age
BMI<35.0 kg/m2 |
65/23 |
Obesity (88) |
YFAS 2.0 |
23 patients had FA and BE |
23 |
No differences (P=0.58) |
Patients with FA had more depression than only individuals with obesity (7.71 ± 3.80; p=0.001) |
| Brunalt et al [62] |
Cross-sectional |
188 |
Adults: 40.8 ± 12.6 years |
158/30 |
Obesity (188) |
YFAS |
- |
31 |
No differences (p=0.36) |
Patients with FA presented motor impulsivity (22.1 ± 4.2; t=-2.55; p=0.012), cognitive impulsivity (18.1 ± 3.1; t=-4.74; p<0.001) and Non-planning impulsivity (26.6 ± 4.9; t=-2.95; p=0.004) |
| Burrows et al [58] |
Cross-sectional |
150 |
Children: 5-12 years |
74/76 |
Thin (10)
Eutrophic (58)
Overweight (33
Obesity (49) |
mYFAS and YFAS-C |
- |
34 |
Patients with FA presented more obesity (n=23; 67.6%) than no FA.
No differences found in thinness, eutrophic and overweight. |
- |
| Ceccarini et al [66] |
Cross-sectional |
88 |
Adults: 18-74 years |
63/25 |
Obesity (88) |
YFAS |
Most individuals with FA present BE (20 ± 9.3; p<0.001) |
30 |
No difference was found |
No differences were found in individuals with FA or no FA about Attentional impulsivity (16.8 ± 4.2; p=0.182) and
motor impulsivity (21.8 ± 5.4; p=0.21). However, Non-planning impulsivity (27.9 ± 6.4; p=0.026) was greater patients with FA. |
| Chao et al [67] |
Cross-sectional |
178 |
Adults: = 21 and = 65 years |
157/21 |
Obesity (178) |
YFAS |
2.2% had both FA and clinical or subclinical BED. |
12 |
No differences found (p=0.20) |
19.1% of patients with FA presented depression (p<0.001) |
| Davis et al [68] |
Cross-sectional |
72 |
Adults: 25-46 years |
49/23 |
Obesity (71) |
YFAS |
Most individuals with FA presented BE (4.2 ± 1.2; p<0.0001) |
18 |
No difference were found (p=0.46) |
Individuals with FA present more depression (27.8%; p=0.018) and impulsivity (3.2 ± 12; p<0.0001) |
| Eichen et al [69] |
Cross-sectional |
178 |
Adults: 51.2 ± 11.7 years |
133/45 |
Overweight (14)
Obesity (164) |
YFAS |
- |
27 (15.2%) |
No difference were found (p=0.92) |
Depression was greater in patients with FA (17.1 ± 6.6; p<0.001) |
| Filgueiras et al [70] |
Cross-sectional |
139 |
Children: 9-11 years |
75/64 |
Overweight (78)
Obesity (60) |
YFAS-C |
- |
33 |
No difference was found between the BMI of overweight and individuals with obesity and with or without FA (p=0.348) |
- |
| Gearhardt et al [78] |
Cross-sectional |
81 |
Adults: 28-64 years |
64/17 |
Obesity (81) |
YFAS |
FA was related to the occurrence of BED (r=0.26; p<0.01) |
46 |
- |
- |
| Gearhardt et al [71] |
Cross-sectional |
96 |
Adults: 19-65 years |
72/24 |
Obesity (96) |
YFAS |
FA was correlated with BED eating (1.81 ± 1.25; r=0.55; p<0.01) |
39 |
- |
- |
| Guzzardi et al [72] |
Clinical trial |
36 |
Adults>18 years |
36/0 |
Obesity (36) |
YFAS |
FA was correlated with BE (r=0.58; p=0.001) |
22 |
There is no difference between the BMI of patients with low YFAS and high YFAS (p=0.858). |
- |
| Hsu et al [42] |
Cross-sectional |
40 |
Adults |
40/0 |
- |
YFAS |
- |
20 |
FA group present higher BMI (33.09 ± 3.01; p<0.001) when compared to the control group |
- |
| Imperatori et al [73] |
Cross-sectional |
112 |
Adults=18 - 73 years |
80/32 |
Overweight and obesity (112) |
YFAS |
FA was correlates with BE (r=0.78; p=0.05) |
38 |
- |
- |
| Imperatori et al [74] |
Cross-sectional |
28 |
Adults |
22/06 |
Overweight and obesity (28) |
Italian version of Yale FA Scale (I-YFAS) |
- |
14 |
There were no differences between the BMI of patients who had 3 or more symptoms (29.35 ± 3.49) and 2 or fewer (27.56 ± 1.84) FA symptoms.
(t=1.70; p=0.10) |
- |
| Imperatori et al [43] |
Cross-sectional |
301 |
Adults > 18 years |
301/0 |
Overweight (137)
Obesity (164) |
YFAS |
FA severity was positively associated with BE (r=0.71; p<0.001) |
24 |
FA severity was positively associated with BMI (r=0.26; p<0.001) |
FA severity was positively associated with depressive symptoms (r=0.41; p>0.001). |
| Imperatori et al [75] |
Cross-sectional |
70 |
Adults=18-71 years |
70/0 |
Overweight and obesity (70) |
YFAS |
75% (N=12) of the participants with AF had BE.
FA symptoms were strongly associated with binge eating severity (r=0.63; p < 0.01) |
16 (22.9%) |
BMI was not associated with FA
(r=0.14; p>0.05) |
FA symptoms were positively associated with depressive symptom severity (r=0.43; p<0.01). |
| Ivezaj et al [39] |
Cross-sectional |
502 |
Adults=38 ± 13.1 years |
415/87 |
Overweight and obesity (502) |
YFAS |
12.0% (n=60) met criteria for BED and 26.7% (n=134) met FA criteria |
84 |
19.3% (n=97) of the overweight and participants with obesity had FA |
- |
| Kozak et al [34] |
Cross-sectional |
190 |
Adults=18 - 65 years |
103/87 |
Eutrophic (50)
Overweight (50)
Obesity (90) |
YFAS |
FA total symptom score (YFAS) were inversely related to distress tolerance (p<0.001) |
152 |
No differences in BMI |
- |
| Masheb et al [44] |
Cross-sectional |
128 |
Adults=61.8 ± 8.6 years |
13/113 |
Overweight and obesity (126) |
Modified Yale FA Scale (mYFAS) |
75% of BED participants met FA criteria
(t=40.2, p<.001) |
12 |
FA was significantly and highly correlated with BMI (r=0.43; p<0.001) |
FA was significantly correlated with depression (r=.43, p<.001) |
| Lee et al [35] |
Cross-sectional |
476 |
Adults=18-64 years |
383/93 |
Thin (14)
Eutrophic (228)
Overweight (104)
Obesity (133) |
YFAS |
- |
59 |
FA individual was obese (mean (M) BMI=33.8 ± 10.8), while undiagnosed participants were on average overweight (M BMI=26.5 ± 7.3). |
- |
| Meule et al [16] |
Cross-sectional |
50 |
Adolescents=14 - 21 years |
31/19 |
Overweight and obesity |
YFAS |
Patients with FA have more eating concern when compared to no FA (p<0.001) |
19 |
No differences found between FA or No FA (p=0.73) |
Individual with FA presented more Attentional impulsivity (p<.001) and Motor impulsivity (p=0.01) than no FA |
| Meule et al [63] |
Cross-sectional |
455 |
Study 1:Adults=25.57 ± 6.97 years
Study 2: Adults=39.52 ± 10.71 years |
Study 1: 405/50
Study 2: 108/25 |
Study 1: Thin (31)
Eutrophic (354)
Overweight (53)
Obesity (17)
Study 2: Obesity (133) |
YFAS 2.0 |
Study 1: Patients with FA present food cravings traits (p<0.001)
Study 2: Patients with FA present EDE (p<0.001) |
Study 1: 44
Study 2: 63 |
Study 1: Individuals with FA present higher BMI than individuals who do not have FA (P=0.003)
Study 2: No differences found between FA or no FA (p=0.29) |
Study 1: Individuals with FA present more symptoms of Attentional impulsivity (p<0.001 and Motor impulsivity (p=0.01
Study 2: No differences in impulsivity |
| Mies et al [40] |
Cross-sectional |
2653 |
Adolescents=14 - 21 years |
1626/1027 |
Thin (210)
Eutrophic (2052)
Overweight (339)
Obesity (52) |
YFAS - C |
- |
69 |
Most adolescents diagnosed with FA were overweight (5.9%) |
- |
| Ouellette et al [76] |
Cross-sectional |
146 |
Adults=39.8 ± 7.1 years |
112/34 |
Obesity (146) |
YFAS |
- |
24 |
No difference was found in BMI (p=0.968) |
Impulsiveness acts as mediator of FA (95% CI 0.0063 - 0.0254) |
| Pedram et al [23] |
Cross-sectional |
652 |
Adults=44.3 ± 12.9 years |
415/237 |
Thin and eutrophic (249)
Overweight and obesity (403) |
YFAS |
- |
35 |
88.6% of the participants with FA were overweight and obese |
- |
| Rodrigue et al [46] |
Cross-sectional |
86 |
Adults=18-55 years |
66/20 |
Severe obesity (86) |
YFAS |
High FA group reported more BE (p<0.01) |
69 |
Individuals with low FA presented higher BMI (p<0.01) |
No difference between groups was observed regarding impulsivity (p=0.07) scores.
More depressive (p<0.01) and anxiety (p<0.01) symptoms than the low FA group. |
| Schulte et al [41] |
Cross-sectional |
181 |
Adolescents=12-16 years |
122/59 |
Overweight and obesity (81) |
YFAS-C |
FA symptoms were significantly associated with more Objective Binge Eating (r=.48, p<0.001), Objective overeating episodes (r=.22, p=0.004), and Subjective binge episodes (r=.28, p<0.001) |
18 |
FA was positively associated with percent overweight (r=.19; p=0.011) |
- |
| Steward et al [38] |
Cross-sectional |
69 |
Adults=18-55 years |
69/0 |
Eutrophic (36)
Obesity (33) |
YFAS 2.0 |
No difference was found in eating disorders (p=0.52) |
9 |
Obesity was higher in the FA group (P=0.008) |
- |
| Tompkins et al [77] |
Clinical trial |
26 |
Adolescents=12-18 years |
14/12 |
Obesity (26) |
YFAS -C |
- |
8 |
No difference was found |
- |
| VanderBroek-Stice et al [37] |
Cross-sectional |
181 |
Adults=18-55 years |
129/52 |
Non-obesity (123) Obesity (58) |
YFAS |
- |
12 |
FA was positively associated with BMI (r=.20; p=0.01) |
FA may be a candidate to etiological pathway towards obesity for individuals presenting impulsivity |
BE: Binge-eating; BED: Binge-eating disorders; BMI: Body Mass Index; CT: Childhood Trauma; DT: Distress Tolerance; EDE: Eating Disorder Examination; EEG: Electroencephalography; EMS: Early Maladaptive Schemas; FC: Food Craving; FA: Food Addiction; HRQOL: Health-Related Quality of Life; HC: Healthy Controls; US: United State; YFAS: Yale Food Addiction Scale; YFAS-C: Yale Food Addiction Scale.
Description of included studies
Most studies were carried out with adults (>18 years, n=24 studies), two studies were carried out with children/adolescents, five only with adolescents and one study included all three, children, adolescents, and adults. Differences among these groups represent adaptations of each YFAS and/or geographical variations. Further, references to YFAS include all FA’s on these rating scales, such as mYFAS 2.0 and YFAS 2.0. Five studies were conducted with exclusively female population groups, with all other studies including both sexes.
Besides the FA, 20 studies presented eating disorders (Table 2). Regarding weight status, 31 studies presented individuals with obesity. In addition, among the other studies, 17 evaluated overweight, 8 evaluated eutrophic and 6 thin (Table 2).
Risk of bias assessment
No studies were excluded based on quality ratings and the risk of bias was classified as low risk of bias. The results are expressed in Figure 2.
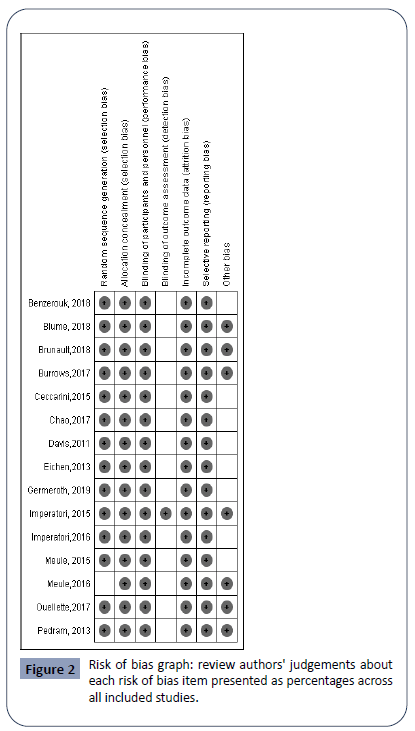
Figure 2: Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Body mass index (BMI) related to patients with or without FA
The relationship between BMI and FA was assessed in 29 studies. No differences were found between the BMI of patients with or without FA in 12 studies. Nine studies observed that individuals with FA presented higher levels of overweight and obesity. In relation to the different levels of FA and BMI, one study did not observe a difference, and another found that individuals with low FA had a higher BMI. Among the studies that evaluated the association between FA and BMI, four studies found a positive association and one found no association. Regarding the individuals who were thin and had normal weight, no differences were found in relation to the BMI, either in individuals with or without FA [23,32-38]. However, it was seen that individuals with FA had a higher incidence of overweight rather than being thin or eutrophic [23,39-41]. Moreover, when observed the overweight group with FA was analyzed, the studies showed increased BMI (>25 kg/m²) [22,23,32,33,35,37-39,42-46].
Twelve studies showed low heterogeneity (I2 8%, p=0.37) (Figure 3). When the mean difference between groups (FA or no FA) was analyzed, it was found that patients with FA presented higher BMI (MD=1.23; 95% CI 0.50 to 1.97%), leading to the conclusion that FA can influence the increase in BMI (>25 kg/m²).

Figure 3: Forest plot of comparison: Food addiction vs No Food addiction, outcome: Food addiction increases body mass index.
Depression and patients with or without FA
Ten studies were found that evaluated the relationship between depression and FA. Seven of these showed that individuals with FA exhibited symptoms of depression. Among the different levels of FA, one study reported that individuals with less FA had higher levels of depression. In addition, among the relationship studies, two studies found a positive correlation between depression and the presence of FA.
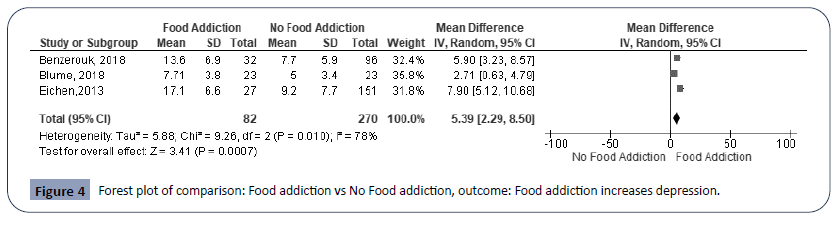
From the meta analysis, the three studies that evaluated the presence of depression in individuals with FA, showed high heterogeneity (I2 78%, p=0.01) (Figure 4). Regarding the difference between averages, it was seen that individuals with FA presented a higher mean score of depression (MD=5.39; 95% CI 2.29 to 8.50). In summary, the data demonstrated that patients with FA presented a higher score for depression.
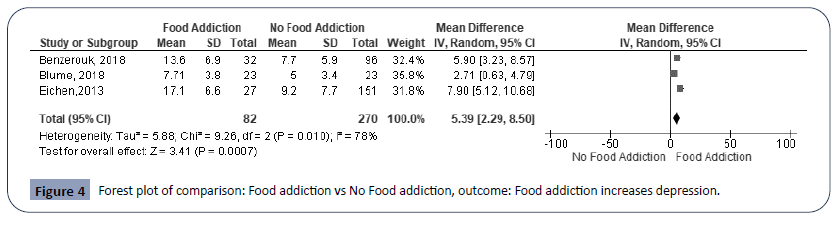
Figure 4: Forest plot of comparison: Food addiction vs No Food addiction, outcome: Food addiction increases depression.
Impulsivity and patients with or without FA
Nine studies evaluated the relationship between impulsivity and FA. Five studies found that individuals with FA had a higher level of lack of self-control and three studies did not find differences between groups. One study found a positive correlation between impulsivity and FA. On the different types of impulsivity, it was observed that 3 studies found higher levels of motor impulsivity, 2 studies found higher levels of non-planning and attentional impulsivity and 1 study found more cases of motor impulsivity in patients with FA.
Meta-analysis of five studies indicated marked heterogeneity among them (I2 73%, p=0.005); the mean difference was 2.78 (95% CI 1.23 to 4.33) (Figure 5). This indicates that individuals with FA are more predisposed to impulsivity.

Figure 5: Forest plot of comparison: Food addiction vs No Food addiction, outcome: Food addiction increases impulsivity.
Discussion
The development of overwiegth/obesity is often associated with FA. With this in mind, we performed a systematic review and meta-analysis examining the association between FA with overweight and obesity. From the methodological quality assessment questions, we observed that all selected studies, classified as medium or high quality, were qualified to identify FA and outcomes of interest (overweight and obesity). The result of the meta-analysis indicated that, among individuals with overweitght/obesity, FA was present in individuals with the highest BMI levels. In addition, the meta-analysis identified high scores for depression and impulsivity in individuals with FA.
Among the studies selected for the meta-analysis of BMI and FA, two studies identified that the highest BMI values were found in individuals with FA and 10 studies found no difference between the BMI of individuals either with and without FA. Although 10 studies found no differences, 7 other studies indicated a tendency to higher BMI in FA. This indicates that the use of the test for overall effect (3.46, <0.001) was efficient in indicating that FA was present in people with higher BMI levels. Moreover, from the heterogeneity test and the calculated value of I2, low heterogeneity was evidenced between the studies.
Chronic access to palatable and calorically dense foods can be one of the “trigger mechanisms” for FA. These foods can reshape the brain-motivating circuits (reward and attention). This is true for the striatum, for example, which make individuals dependent on the desirable properties of these foods [47]. The pattern of intake of these foods resembles patterns of drug use that cause addiction, where addicted individuals fail to control consumptive behavior even though they are aware of the associated harm. According to Lennerz and Lennerz [48], high glycemic carbohydrates and sugars (additives in highly palatable foods) cause a rapid change in blood glucose and insulin levels that are similar to the pharmacokinetic properties of drug abuse and may trigger addictive behaviors. The three clinical features evidenced in FA are feelings of deprivation when food is withheld, a propensity to relapse during periods of abstinence and consumption that persists despite awareness of negative health, social, financial and other consequences [49].
FA can be diagnosed in individuals with different nutritional states, but the risks associated with a high prevalence of FA and failure to control food intake are higher in overweight and individuals with obesity. A question raised in the context of FA in individuals with obesity: why among individuals with obesity, only some are addicted to food and others are not. The genetic origin of obesity has been associated with mutations that disrupt signaling through the melanocortin 4 receptor (MC4R). These mutations are present in up to 6% of severely individuals with obesity and are associated with hyperphagia [50,51]. Some studies have attempted to demonstrate activation of the reward system through ingestion and dietary preferences in individuals with MC4R mutations. In evaluating children and adolescents with obesity and with or without the MC4R mutation, [52] identified that girls with obesity who were carriers of the C allele had lower scores of satiety responsiveness and higher scores of uncontrolled eating. Boys with obesity carrying the C allele presented a lower value of food reward than non-carrier boys. A study by van der Klaauw, von dem Hagen, Keogh, Henning, O'Rahilly, Lawrence, Calder and Farooqi [53] aimed to investigate how melanocortin signaling modulates food reward in individuals with MC4R mutations. They identified a higher striatal (basal core) response to food stimuli in individuals with MC4R mutations, compared to their controls with obesity.
The industrial revolution boosted the productivity of the food and beverage industry by changing the food systems and patterns of most developed and developing countries [54]. The food environment changed dramatically, from a diet rich in proteins and grains, and low in sodium, fat, and sugars, to an adapted diet, with a production of artificial foods high in fat and sugars [55]. From a nutritional point of view, most of these artificial foods have lost the characteristics of food and turned into industrial ingredient formulations that contain little or no whole food [54]. These artificial foods are palatable, fast and practical, and have become the target of a population marked by pressure and lack of time [56]. Thus, today, it is more common to ingest more practical snacks, with high energy density and poor nutritional quality [57]. Concomitantly with the change in the dietary pattern experienced after the industrial revolution, there was an increase in the prevalence of overweight and obesity in the population [55].
Based on the findings of the systematic review and meta-analysis, factors such as depression and impulsivity were associated with FA. However, the presence of heterogeneity significant differences among the studies reviewed suggests a cautious analysis. Studies that aimed to evaluate the association of FA with depression and/ or impulsivity were found to be inconsistent, heterogeneous and even contained contradictory results. A meta-analysis developed by [58] in 2018 identified an association between depression and FA, but serious differences were observed among the 18 studies analyzed. Regarding the association between FA and impulsivity, the literature presents divergent results on the subject [12,59-63]. Although the results suggest that individuals with depression and impulsivity are more likely to trigger FA as an emotional regulation strategy (activation of the reward system), our work did not perform an exhaustive search along this theme.
Given the sizable literature on the studies between FA and psychiatric disorders, considerable heterogeneity may have occurred due to our search strategy. However, a recent metaanalysis of FA and depression also found heterogeneity among the studies [58]. In the present review, we have systematically tried to identify reasons for heterogeneity by grouping studies according to similarities in studies with FA, but could not identify definitive conclusions. Our study found that there is a mutualistic relationship between overweight/obesity and FA and psychiatric disorders (depression and impulsivity). In addition, presented data that can serve as a basis for interventions and planning in multi-professional studies in the area of FA and overweight.
Acknowledgments
Fundação de Amparo a Ciência de Pernambuco (FACEPE), the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) and the Conselho Nacional de Desenvolvimento científico e tecnológico (CNPq). All authors participated in the work to fulfill the authorship criteria. In particular, the contributions were as follows: Desing study: MSSF, GCJS and IGN; Practical performance: MSSF, GCJS, RMS, JRSB and IGN; Data analysis: MSSF and GCJS; Preparation manuscript: MSSF, GCJS, RMS, JRSB and IGN, Critical review of systematic review: MSSF, RMS and JRSB
Disclosure statement
The English text of this paper has been revised by Sidney Pratt, Canadian, MAT (The Johns Hopkins University), RSAdip - TESL (Cambridge University).
No potencial conflict of interest was reported by the authors
Funding
None
29794
References
- Hawkes C, Fanzo J (2017) Nourishing the SDGs: Global nutrition report 2017. City Research Online.
- Lartey ST, Si L, Otahal P, de Graaff B, Boatengc GO, et al. (2020) Annual transition probabilities of overweight and obesity in older adults: Evidence from World Health Organization Study on global AGEing and adult health. Social science & medicine 247: 112821.
- Butler MG, Wang K, Marshall JD, Naggert JK, Rethmeyer JA, et al. (2015) Coding and noncoding expression patterns associated with rare obesity-related disorders: Prader-Willi and Alstrom syndromes. Adv Genomics Genet 2015: 53-75.
- Rotondi M, Leporati P, La Manna A, Pirali B, Mondello T, et al. (2009) Raised serum TSH levels in patients with morbid obesity: is it enough to diagnose subclinical hypothyroidism? European journal of endocrinology/European Federation of Endocrine Societies 160: 403-408.
- Haghighian, Roudsari A, Vedadhir A, Amiri P, Kalantari N, et al. (2017) Psycho-Socio-Cultural Determinants of Food Choice: A Qualitative Study on Adults in Social and Cultural Context of Iran. Iran J Psychiatry 12: 241-250.
- Ganasegeran K, Al-Dubai SA, Qureshi AM, Al-abed AA, Am R, et al. (2012) Social and psychological factors affecting eating habits among university students in a Malaysian medical school: a cross-sectional study. Nutrition journal 11: 48.
- Weden MM, Brownell P, Rendall MS (2012) Prenatal, perinatal, early life, and sociodemographic factors underlying racial differences in the likelihood of high body mass index in early childhood. Am J Public Health 102: 2057-2067.
- Gonzalez-Muniesa P, Martinez-Gonzalez MA, Hu FB, et al. (2017) Obesity. Nature reviews Disease primers. 3: 17034.
- Kumar S, Kelly AS (2017) Review of Childhood Obesity: From Epidemiology, Etiology, and Comorbidities to Clinical Assessment and Treatment. Mayo Clin Proc 92: 251-265.
- Ziauddeen H, Alonso-Alonso M, Hill JO, Kelley M, Khan NA (201) Obesity and the neurocognitive basis of food reward and the control of intake. Adv Nutr 6: 474-86.
- Leigh SJ, Lee F, Morris MJ (2018) Hyperpalatability and the Generation of Obesity: Roles of Environment, Stress Exposure and Individual Difference. Curr Obes Rep 7: 6-18.
- Pivarunas B, Conner BT (2015) Impulsivity and emotion dysregulation as predictors of food addiction. Eat Behav 19: 9-14.
- Cerit H, Christensen K, Moondra P, Klibanski A, Goldstein JM, et al. (2019) Divergent associations between ghrelin and neural responsivity to palatable food in hyperphagic and hypophagic depression. J Affect Disord 242: 29-38.
- Appelhans BM, Woolf K, Pagoto SL, Schneider KL, Whited MC, et al. (2011) Inhibiting food reward: delay discounting, food reward sensitivity, and palatable food intake in overweight and obese women. Obesity (Silver Spring, Md) 19: 2175-2182.
- Boggiano MM (2016) Palatable Eating Motives Scale in a college population: Distribution of scores and scores associated with greater BMI and binge-eating. Eat Behav 21: 95-98.
- Meule A (2015) Back by Popular Demand: A Narrative Review on the History of Food Addiction Research. Yale J Biol Med 88: 295-302.
- Kekic M, McClelland J, Bartholdy S, Chamali R, Campbell IC, et al. (2019) Bad Things Come to Those Who Do Not Wait: Temporal Discounting Is Associated With Compulsive Overeating, Eating Disorder Psychopathology and Food Addiction. Front Psychiatry 10: 978.
- Yen JY, Lin HC, Lin PC, Liu TL, Long CY, et al. (2020) Leptin and ghrelin concentrations and eating behaviors during the early and late luteal phase in women with premenstrual dysphoric disorder. Psychoneuroendocrinology 118: 104713.
- Efraim M, Kirwan CB, Muncy NM, Tucker LA, Kwon S, et al. (2020) Acute after-school screen time in children decreases impulse control and activation toward high-calorie food stimuli in brain regions related to reward and attention.
- Nicolau J, Romerosa JM, Rodríguez I, Sanchís P, Bonet A, et al. (2020) Associations of food addiction with metabolic control, medical complications and depression among patients with type 2 diabetes. Acta Diabetologica 57: 1093-1100.
- Gearhardt AN, Corbin WR, Brownell KD (2009) Preliminary validation of the Yale Food Addiction Scale. Appetite 52: 430-436.
- Gearhardt AN, White MA, Masheb RM, Morgan PT, Crosby RD, et al. (2012) An examination of the food addiction construct in obese patients with binge eating disorder. Int J Eat Disord 45: 657-663.
- Pedram P, Wadden D, Amini P, Gulliver W, Randell E, et al. (2013) Food addiction: its prevalence and significant association with obesity in the general population. PLoS One 8: e74832.
- Beyer F, Garcia-Garcia I, Heinrich M, Schroeter ML, Sacher J, et al. (2019) Neuroanatomical correlates of food addiction symptoms and body mass index in the general population. Human brain mapping 40: 2747-2758.
- Brunault P, Frammery J, Montaudon P, de Luca A, Hankard R, et al. (2019) Adulthood and childhood ADHD in patients consulting for obesity is associated with food addiction and binge eating, but not sleep apnea syndrome. Appetite 136: 25-32.
- Leigh SJ, Morris MJ (2018) The role of reward circuitry and food addiction in the obesity epidemic: An update. Biol Psychol 131: 31-42.
- Lee PC, Dixon JB (2017) Food for Thought: Reward Mechanisms and Hedonic Overeating in Obesity. Curr Obes Rep 6: 353-361.
- Brownley KA, Berkman ND, Peat CM, Lohr KN, Cullen KE, et al. (2016) Binge-Eating Disorder in Adults: A Systematic Review and Meta-analysis. Ann Intern Med 165: 409-420.
- Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6: e1000097.
- Institute JB (2016) Joanna Briggs Institute reviewers' manual: 2016 edition. Australia: Joanna Briggs Institute.
- Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327: 557-560.
- Ahmed AY, Sayed AM, Alshahat AA, Elaziz EAA (2017) Can food addiction replace binge eating assessment in obesity clinics? Egyptian Journal of Medical Human Genetics 18: 181-185.
- Pursey KM, Stanwell P, Gearhardt AN, Collins CE, Burrows TL (2014) The prevalence of food addiction as assessed by the Yale Food Addiction Scale: a systematic review. Nutrients 6: 4552-90. 34. Kozak AT, Davis J, Brown R, Grabowski M (2017) Are overeating and food addiction related to distress tolerance? An examination of residents with obesity from a US metropolitan area. Obesity research & clinical practice 11: 287-298.
- Lee N, Hall W, Lucke J, Forlini C, Carter A (2014) Food addiction and its impact on weight-based stigma and the treatment of obese individuals in the US and Australia. Nutrients 6: 5312-5326.
- Meule A, Müller A, Gearhardt AN, Blechert J (2017) German version of the Yale Food Addiction Scale 2.0: prevalence and correlates of ‘food addiction’in students and obese individuals. Appetite 115: 54-61.
- VanderBroek-Stice L, Stojek MK, Beach SR, MacKillop J (2017) Multidimensional assessment of impulsivity in relation to obesity and food addiction. Appetite 112: 59-68.
- Steward T, Mestre‐Bach G, Vintró‐Alcaraz C, Lozano‐Madrid M, Agüera Z, et al. (2018) Food addiction and impaired executive functions in women with obesity. European Eating Disorders Review 26: 574-584.
- Ivezaj V, White MA, Grilo CM (2016) Examining binge‐eating disorder and food addiction in adults with overweight and obesity. Obesity 24: 2064-2069.
- Mies GW, Treur JL, Larsen JK, Halberstadt J, Pasman JA, et al. (2017) The prevalence of food addiction in a large sample of adolescents and its association with addictive substances. Appetite 118: 97-105.
- Schulte EM, Jacques-Tiura AJ, Gearhardt AN, Naar S (2018) Food addiction prevalence and concurrent validity in African American adolescents with obesity. Psychol Addict Behav 32: 187-196.
- Hsu JS, Wang PW, Ko CH, Hsieh TJ, Chen CY, et al. (2017) Altered brain correlates of response inhibition and error processing in females with obesity and sweet food addiction: A functional magnetic imaging study. Obesity research & clinical practice 11: 677-686.
- Imperatori C, Innamorati M, Lamis DA, Farina B, Pompili M, et al. (2016) Childhood trauma in obese and overweight women with food addiction and clinical-level of binge eating. Child Abuse Negl 58: 180-190.
- Masheb RM, Ruser CB, Min KM, Bullock AJ, Dorflinger LM (2018) Does food addiction contribute to excess weight among clinic patients seeking weight reduction? Examination of the Modified Yale Food Addiction Survey. Compr Psychiatry 84: 1-6.
- Meule A, Hermann T, Kübler A (2015) Food addiction in overweight and obese adolescents seeking weight‐loss treatment. European Eating Disorders Review 23: 193-198.
- Rodrigue C, Ouellette AS, Lemieux S, Tchernof A, Biertho L, et al. (2018) Executive functioning and psychological symptoms in food addiction: a study among individuals with severe obesity. Eat Weight Disord 23: 469-478.
- Stice E, Yokum S (2016) Gain in Body Fat Is Associated with Increased Striatal Response to Palatable Food Cues, whereas Body Fat Stability Is Associated with Decreased Striatal Response. J Neurosci 36: 6949-6956.
- Lennerz B, Lennerz JK (2018) Food Addiction, High-Glycemic-Index Carbohydrates, and Obesity. Clin Chem 64: 64-71.
- Fletcher PC, Kenny PJ (2018) Food addiction: a valid concept? Neuropsychopharmacology 43: 2506-2513.
- Loos RJ (2011) The genetic epidemiology of melanocortin 4 receptor variants. European journal of pharmacology 660: 156-164.
- Farooqi IS, Keogh JM, Yeo GS, Lank EJ, Cheetham T, et al. (2003) Clinical spectrum of obesity and mutations in the melanocortin 4 receptor gene. N Engl J Med 348: 1085-1095.
- Obregon AM, Oyarce K, Santos JL, Valladares M, Goldfield G (2017) Association of the melanocortin 4 receptor gene rs17782313 polymorphism with rewarding value of food and eating behavior in Chilean children. Journal of physiology and biochemistry 73: 29-35.
- van der Klaauw AA, von dem Hagen EA, Keogh JM, et al. (2014) Obesity-associated melanocortin-4 receptor mutations are associated with changes in the brain response to food cues. The Journal of clinical endocrinology and metabolism 99: E2101-E2106.
- Moubarac J-C, Parra DC, Cannon G, Monteiro CA (2014) Food classification systems based on food processing: significance and implications for policies and actions: a systematic literature review and assessment. Curr Obes Rep 3: 256-272.
- Gearhardt AN, Davis C, Kuschner R, Brownell KD (2011) The addiction potential of hyperpalatable foods. Current drug abuse reviews 4: 140-145.
- Poti JM, Braga B, Qin B (2017) Ultra-processed Food Intake and Obesity: What Really Matters for Health—Processing or Nutrient Content? Current obesity reports 6: 420-431.
- Martins APB, Levy RB, Claro RM, Moubarac JC, Monteiro CA (2013) Increasing participation of ultra-processed products in the Brazilian diet (1987-2009) Public Health Journal 47: 656-665.
- Burrows T, Kay-Lambkin F, Pursey K, Skinner J, Dayas C (2018) Food addiction and associations with mental health symptoms: a systematic review with meta-analysis. J Hum Nutr Diet 31: 544-572.
- VanderBroek-Stice L, Stojek MK, Beach SRH, vanDellen MR, MacKillop J (2017) Multidimensional assessment of impulsivity in relation to obesity and food addiction. Appetite 112: 59-68.
- Loeber S, Grosshans M, Korucuoglu O, et al. (2012) Impairment of inhibitory control in response to food-associated cues and attentional bias of obese participants and normal-weight controls. Int J Obes (Lond) 36: 1334-1339.
- Jasinska AJ, Yasuda M, Burant CF, et al. (2012) Impulsivity and inhibitory control deficits are associated with unhealthy eating in young adults. Appetite 59: 738-747.
- Brunault P, Ducluzeau PH, Courtois R, Bourbao-Tournois C, Delbachian I, et al. (2018) Food Addiction is Associated with Higher Neuroticism, Lower Conscientiousness, Higher Impulsivity, but Lower Extraversion in Obese Patient Candidates for Bariatric Surgery. Subst Use Misuse 53: 1919-1923.
- Meule A, de Zwaan M, Muller A (2017) Attentional and motor impulsivity interactively predict 'food addiction' in obese individuals. Compr Psychiatry 72: 83-87.
- Benzerouk F, Gierski F, Ducluzeau PH, Bourbao-Tournois C, Gaubil-Kaladjian I, et al. (2018) Food addiction, in obese patients seeking bariatric surgery, is associated with higher prevalence of current mood and anxiety disorders and past mood disorders. Psychiatry Res 267: 473-479.
- Blume M, Schmidt R, Hilbert A (2019) Executive Functioning in Obesity, Food Addiction, and Binge-Eating Disorder. Nutrients 11: 54.
- Ceccarini M, Manzoni GM, Castelnuovo G, Molinari E (2015) An evaluation of the Italian version of the Yale Food Addiction Scale in obese adult inpatients engaged in a 1-month-weight-loss treatment. J Med Food 18: 1281-1287.
- Chao AM, Shaw JA, Pearl RL, Alamuddin N, Hopkins CM, et al. (2017) Prevalence and psychosocial correlates of food addiction in persons with obesity seeking weight reduction. Compr Psychiatry 73: 97-104.
- Davis C, Curtis C, Levitan RD, Carter JC, Kaplan AS, et al. (2011) Evidence that ‘food addiction’is a valid phenotype of obesity. Appetite 57: 711-717.
- Eichen DM, Lent MR, Goldbacher E, Foster GD (2013) Exploration of “food addiction” in overweight and obese treatment-seeking adults. Appetite 67: 22-24.
- Filgueiras AR, de Almeida VBP, Nogueira PCK, Domene SMA, da Silva CE, et al. (2019) Exploring the consumption of ultra-processed foods and its association with food addiction in overweight children. Appetite 135: 137-145.
- Gearhardt AN, White MA, Masheb RM, Grilo CM (2013) An examination of food addiction in a racially diverse sample of obese patients with binge eating disorder in primary care settings. Compr Psychiatry 54: 500-505.
- Guzzardi MA, Garelli S, Agostini A, Filidei E, Fanelli F, et al. (2018) Food addiction distinguishes an overweight phenotype that can be reversed by low calorie diet. European Eating Disorders Review 26: 657-670.
- Imperatori C, Innamorati M, Contardi A, Continisio M, Tamburello S, et al. (2014) The association among food addiction, binge eating severity and psychopathology in obese and overweight patients attending low-energy-diet therapy. Compr Psychiatry 55: 1358-1362.
- Imperatori C, Fabbricatore M, Innamorati M, Farina B, Quintiliani MI, et al. (2015) Modification of EEG functional connectivity and EEG power spectra in overweight and obese patients with food addiction: An eLORETA study. Brain imaging behav 9: 703-716.
- Imperatori C, Innamorati M, Lester D, Continisio M, Balsamo M, et al. (2017) The association between food addiction and early maladaptive schemas in overweight and obese women: a preliminary investigation. Nutrients 9: 1259.
- Ouellette AS, Rodrigue C, Lemieux S, Tchernof A, Biertho L, et al. (2017) An examination of the mechanisms and personality traits underlying food addiction among individuals with severe obesity awaiting bariatric surgery. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity 22: 633-640.
- Tompkins CL, Laurent J, Brock DW (2017) Food addiction: A barrier for effective weight management for obese adolescents. Child Obes 13: 462-469.
- Gearhardt AN, White MA, Masheb RM, Morgan PT, Crosby RD, et al. (2012) An examination of the food addiction construct in obese patients with binge eating disorder. Int J Eat Disord 45: 657-663.