Abstract
The relationship between serum 25-OH Vitamin-D level in hypothyroid patients with and without thyroid peroxidase (TPO) antibodies is controversial. There is growing evidence that the level of Vitamin-D 25-OH is related to autoimmune diseases. The study aimed to evaluate the relationship between serum Vitamin-D levels and thyroid function tests in euthyroid and hypothyroid patients from Pristina with (anti -TPO) raised. Cross-sectional analyzes were conducted at H.P Diagnostic Center, American Hospital and Olive Laboratory from February to June 2023. Fifty patients with hypothyroidism were selected. Another fifty were chosen as the control group. The tests of (TSH, FT4, Anti-TPO, Vitamin-D 25- OH) were measured using COBAS E 411 system analyzer. The results were analyzed using SPSS version. TSH was significantly increased in both hypothyroid patients with positive TPO antibodies (7.75±10.34) and negative TPO antibodies (5.01±0.79) compared to the control group (2.69±1.33), respectively, with a p -value of 0.560. The level of 25-OH Vitamin-D was lower among hypothyroid patients than in the control group. TPO-antibody-positive subjects had lower 25-OH Vitamin-D levels (10.38±4.45), than TPO antibody-negative patients (18.79±8.93) compared to controls (64.92±161.08), respectively, with the p-value value 0.045. In hypothyroid patients, women 34 (68%) were more than men 16 (32%).
Conclusion: The level of Vitamin-D 25-OH was low in patients with hypothyroidism. TPO- antibody-positive subjects had less serum 25-OH Vitamin-D compared to TPO-antibody- negative subjects.
Keywords
Vitamin-D; Autoimmune thyroiditis; Thyroid function tests
Introduction
Vitamin-D is a fat-soluble nutrient that is canonically
converted in vivo to the active hormone (calcitriol or 1,
25-dihydroxycholecalciferol) after two hydroxylation steps,
first in the liver (calcidiol or 25-hydroxy Vitamin-D) and second
in the kidneys. Circulating Vitamin-D status is assessed by the
amount of 25-hydroxy Vitamin-D in serum. Vitamin-D has two
forms Vitamin-D2 and Vitamin-D3 respectively. Some of the body
functions that Vitamin-D has been linked to include:
• The immune system
• Muscle function
• Healthy heart and circulation l Healthy lungs and airways
• Brain development
• Anti-cancer effects
• (NHS, 2020)
How much Vitamin-D is needed?
Getting the right amount of Vitamin-D does not depend on the
foods you eat. To get enough Vitamin-D, you need to expose
your skin to sunlight regularly, and you may also need to take
supplements. Different organizations recommend different
daily requirements for Vitamin-D, ranging from 200 to 1000
IU (International Units) per day. NHS guidance for adults and
children over 1 is to consider taking a daily supplement containing
10 micrograms of Vitamin-D (400 IU). This can vary depending
on skin colour, season, geographical location and clothing (NHS,
2020).
Does Vitamin-D or its lack play a role in the
development of thyroid diseases?
Some, but not all, observational studies have found low
blood levels of Vitamin-D in patients with hypothyroidism (an
underactive thyroid) as well as hyperthyroidism (an overactive
thyroid) due to Graves' disease. It is not clear from these studies
whether low Vitamin-D is a cause, a consequence, or an innocent
bystander in the development of these common thyroid
conditions [1].
The occurrence of hypovitaminosis D in populations with
hypothyroidism can be attributed to the evolution of the
Vitamin-D3 receptor and the thyroid hormone receptor from
a single primordial gene that causes a strong homology among
these receptors.
A meta-analysis looking at Vitamin-D levels in autoimmune
thyroiditis showed that both Hashimoto's thyroiditis and
Graves' disease were associated with lower levels of Vitamin-D.
Conversely, some studies have shown that there was no significant
association between Vitamin-D and autoimmune thyroiditis [2].
Thyroid disease (TD) is a quite common condition worldwide.
According to the American Thyroid Association, only in the
United States of America (USA) reported 20 million Americans
with some form of TD, and at least 12% will develop a thyroid
condition during their lifetime. According to hormonal levels, the
patients with TD can be classified into three different groups:
hypothyroidism, euthyroidism, and hyperthyroidism (ATA, 2020).
Hypothyroidism is the condition in which thyroid hormones are
deficient. It has a higher prevalence that varies between 0.3 and
3.7% in the USA and 0.2 and 5.3% in Europe [3]. Undiagnosed
hypotyrosis, including obvious and mild cases, was estimated
to be approximately 5% in meta-analysis research conducted
in nine European countries [4]. Various epidemiological studies
have shown that women have a higher predisposition to develop
hypothyroidism than men [5]. Iodine deficiency continues to be
the leading cause of hypothyroidism worldwide, while populations
in sufficient iodine areas suffer from hypothyroidism due to
autoimmune causes (Hashimoto thyroiditis) and iatrogenic. The
wide spectrum of symptoms associated with hypothyroidism
implies that it has an impact on metabolism and systems of many
organs. The typical clinical symptoms encountered in outpatient
practice are fatigue, cold skin intolerance, dry skin, constipation,
muscle aches, sweating, skin thickening, brittle hair, hair loss,
lateral eyebrows etc [6].
Autoimmune Thyroid Diseases (AITDS)
Autoimmune thyroid diseases (AITDS), including grave disease
(GD) and Hashimoto's thyroiditis (HT), are widespread autoimmune
diseases affecting up to 5% of the total population. Aitds arise due
to the interaction between environmental and genetic factors. In
the last decade, important progress has been made in our sense of
genetic contribution to the etiology of AITDS [1].
Research question
• Do all patients with elevated Anti TPO have low
Vitamin-D levels?
• Which age group is more affected by this condition?
• Which gender is more affected by thyroid gland issues?
Hypotheses
• H1: All patients with elevated Anti TPO have low levels
of Vitamin-D.
• H2: Individuals above 40 years of age are more affected
by this autoimmune condition.
• H3: Females are more affected by thyroid gland issues
Methodology
Quantitative (quantitative) methods have been used to conduct
this research, and for the implementation of this research,
protocols from the Diagnostic Center Human Plus, as well as
those from Olive Laboratory in Prishtina were utilized, which
include values for TSH, FT4, Vitamin-D 25 OH and Anti-Tpo.
In this study, 100 participants, including individuals of different
genders and ages, were involved, in Prishtina. The sample was
randomly selected, February to June 2023. Fifty (50) of these had
hypothyroidism. From (50) hypothyroid subjects: 16 (32%) were
male, while 34 (68%) were females.
Participants were diagnosed with hypothyroidism based on
TSH levels higher than 4.3miu/l, FT4 lower than 7.2 pmol/l.
Participants are further classified in those that are positive anti-
TPO when the antibody titer is> 35iu/ml and those that are anti-
TPO negative when the antibody titer is <35 IU/ml. Vitamin-D
25-Oh levels in participants were classified as deficient when the
result is <10ng/ml, insufficient when the result varies from 10-
30ng/ml, and sufficient when the result ranges from 30-100ng/
ml. Variables were compared between hypothyroid subjects and
control groups by students' t-test, and the ANOVA method.
Results
Table 1 indicates the age and gender of the participants in the
research. 33 (34%) were male while 67 (66%) were females. It
indicates that 12 (10%) of the subjects were 18-20 years old while
51 (54%) were 31-50 years old.
| Variable |
Frekuence |
Percentage |
| Age |
|
|
| 18-30 |
12 |
10.0 % |
| 31-50 |
51 |
54.00 % |
| 51-78 |
37 |
38.00 % |
| Gender |
|
|
| Female |
67 |
66.0 % |
| Male |
33 |
34.0 % |
Table 1: Distribution of Empireers by Age and Gender
Average ± SD of TSH in the group of patients with hypothyroidism,
was (7.48 ± 9.83uiu/l) against the control group (2.69 ± 1.33uiu/l)
(p-value = 0.933), ft4 in the patient group with Hypothyroidism,
(4.67 ± 1.30pmol/l) versus control group (21.50 ± 28.10pmol/l)
(P-values = 0.071), Vitamin-D 25-OH was significantly low in the
group of patients with hypothyroidism, (17.95 ± 8.93 ng/ml)
versus the control group (19.91 ± 7.89ng/ml) (P-value = 0.767) and TPO antibodies in the group of patients with hypothyroidism,
(138.02 ± 186.82iu/ml) against the control group (64.92 ± 161.08
IU /m) (p-value = 0.882) (Table 2).
| Parameters |
Patients with hypothyroidism (Mean ±SD) |
Control group l (Mean ±SD) |
P-value |
| TSH uIU/L |
7.48±9.83 |
2.69±1.33 |
0.933 |
| FT4 pmol/l |
4.67±1.30 |
21.50±28.10 |
0.071 |
| 25-OH Vitamin D ng/ml |
17.95±8.93 |
19.91±7.89 |
0.767 |
| Anti-TPO IU/mL |
138.02±186.82 |
64.92±161.08 |
0.882 |
Table 2: Comparison of Vitamin D 25 Oh levels of TSH, FT4, FT3, TPO among patients with hypothyroidism and control group
Average ± SD of TSH in the group of patients with hypothyroidism,
in the group of TPO positive antibodies was significantly high
(7.75 ± 10.34uiu/l) compared to TPO antibodies in the negative
group (5.01 ± 0.79uui/l), of Both mean are significantly higher
than in the control group (2.69 ± 1.33uui/l) (p-values = 0.560).
Average ± SD FT4 in the group of patients with hypothyroidism,
in the group of TPO positive antibodies was (4.67 ± 1.34pmol/l)
and the average in the negative TPO antibodies was (0.56 ±
0.19pmol/l) which was significantly lower than us Control group
(4.67 ± 1.07pmol/l) (p-value = 0.999). Average ± SD of Vitamin-D
level 25-OH in the group of patients with hypothyroidism in the
group of TPO positive antibodies was (10.38 ± 4.45ng/ml) and
in the group of negative antibodies was (18.79 ± 8.93ng/ml)
compared to The control group (64.92 ± 161.08ng/ml) were
significantly lower (p-value = 0.045) (Table 3).
| Parameters |
Mean ±SD |
P-value |
| Anti-TPO Negative(<35IU/ml) |
Anti-TPO Positive(>35IU/ml) |
Control group |
| TSH uIU/L |
5.01±0.79 |
7.75±10.34 |
2.69±1.33 |
0.560 |
| FT4 pmol/l |
4.67±1.07 |
4.67±1.34 |
21.5±28.10 |
0.999 |
| 25-OH Vitamin D ng/ml |
18.79±8.93 |
10.38±4.45 |
64.92±161.08 |
0.045 |
Table 3: Average comparison ± SD of TSH, FT4, FT3 and 25-OH vitamin D levels in anti-TPO patients with hypothyroidism (positive and negative) versus control group
Average ± SD of TSH in patients with Vitamin-D 25-Oh was
significantly higher (7.78 ± 10.70 uui/ml) than in patients with
insufficient Vitamin-D 25-OH (5.89 ± 1.78 Uui /ml) (P-values
0.624). FT4 was also lower in patients with Vitamin-D 25-OH
(4.67 ± 1.35pmol/l) compared to patients with insufficient
Vitamin-D 25-OH (4.70 ± 1.12pmol/l) (p-value 0.945 Average
antibodies TPO in Vitamin-D 25-Oh in patients with Vitamin-D
25-Oh was (151.47 ± 200.04iu/ml) higher compared to patients
with insufficient Vitamin-D 25-Oh (67.40 ± 56.17 IU/ml) with (a
value of 0.247) (Table 4).
| Parameters |
(Mean ±SD) |
P-value |
| Insuficient 25-OH VitaminD (10-30 ng/ml) |
Deficient 25-OH VitaminD (<10ng/ml) |
Control group |
| TSH uUI/mL |
5.89±1.78 |
7.78±10.70 |
2.69±1.33 |
0.624 |
| FT4 pmol/l |
4.70±1.12 |
4.67±1.35 |
21.5±28.10 |
0.945 |
| Anti-TPO IU/mL |
67.40±56.17 |
151.47±200.04 |
64.92±161.08 |
0.247 |
Table 4: Comparison of TSH antibodies, FT4, FT3 and TPO by vitamin D level 25-OH
Figure 1 Indicates the distribution of groups of patients with
hypothyroidism by gender: 16 (32%) were male while 34 (68%)
were females.
Figure 1:Distribution of patients of patients with hypothyroidism
by gender.
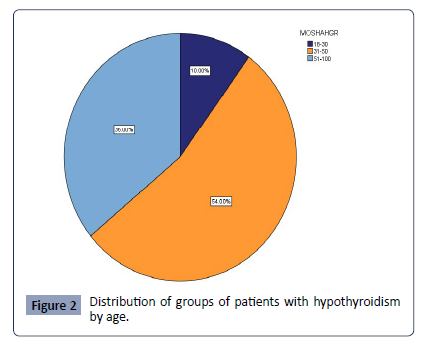
Figure 2 Indicates the distribution of groups of patients with
hypothyroidism by age: 5 (10%) were 18-20 years old while 27
(54%) were aged 31-50 and: 18 (36%) were 51-78 year old.
Figure 2:Distribution of groups of patients with hypothyroidism
by age.
Discussion
During this research we have been more focusing to the link
between serum of Vitamin-D levels and thyroid function tests
in patients with eutiroids and hypothyroids. In this study there
were a total of one hundred (100) subjects. Fifty (50) of these had
hypothyroidism. From (50) hypothyroid subjects: 16 (32%) were
male, while 34 (68%) were females. This value indicates that the
prevalence of the disease is greater in women than in men (graph
1). This matches [7]. Their study stated that hypothyroidism is a
widespread disease of specific organs and affects 2 - 5% of the
population with significant variability between sex (ie, female
5-15% and Men 1-5%).The same finding was confirmed by [8], who reported that the prevalence of hypothyroids is common
in women. This may be due to the fact that women are more
susceptible to autoimmune diseases than men. As it had been
recently reported, many autoimmune disorders tend to affect
women during long periods of stress, such as pregnancy, or
during a hormonal change.
Also from (50) hypothyroid entities: 5 (10%) were 18-20 years old
while 27 (54%) were 31-50 years old and: 18 (36%) were 51-78
years old. Recent results and data from observation studies can
be said that serum TSH levels increase in older people. However,
very mild TSH rising in older individuals may not reflect subclinical
thyroid dysfunction, but be more than a normal consequence of
aging [9].
An analysis from the Longitudinal Baltimore Aging study has found
that changes in thyroid function tests are common, especially in
older age groups, and medium regression is partially responsible
for this finding. Importantly, changes in TSH and FT4 over a
7-year period were accompanied by increased mortality [10]. The
results of the thyroid function indicate that the TSH in the group
of patients with hypothyroidism has increased significantly,
especially in the TPO-antibodies-positive than in the negative
TPO antibodies compared to the control group. FT4 has been
significantly reduced in TPO positive antibodies than in negative
TPO antibodies compared to the control group. This matches the
study done by [11], which found that autoimmunity is closely
linked to thyroid function and an increase in autoimmunity is
directly linked to the deterioration of thyroid function as they are
seen increasing TSH levels in Positive anti-TPO patients.
In contrast, vitamin 25-oh D levels in the group of patients with
hypothyroidism, in the positive TPO antibodies was (10.38 ±
4.45ng/ml) and in the group of negative TPO antibodies was
(18.79 ± 8.93ng/ml) while compared with the control group (64.92
± 161.08ng/ml) were significantly lower. This is compatible with
the study done by (Idiculla J et al, 2018) that the level of vitamin
25-Oh D in patients with hypothyroidism was significantly lower
than in eutroid controls and that anti-TPO positive patients had
lower levels of Vitamin-D25- Oh compared to the negative group
to anti-Tpo.
This study compares subjects that have Vitamin-D 25-Oh and
those with insufficiency, thus showing an increase in TSH and
anti-tpo among those with Vitamin-D 25-Oh. In contrast, the FT4
was lower in the group with Vitamin-D deficiency 25-OH than in
the group with Vitamin-D 25-Oh. This relationship is confirmed by
the findings of (Richards B, 2008) in its experimental study that
explored the effect of Vitamin-D deficiency on the thyroid gland.
In this study, he reported that Vitamin-D deficiency contributed
to the possibility of lowering thyroid hormones.
The study done by [12-18], suggests that Vitamin-D deficiency is
more linked to the antitroid antibody titrine than thyroid function
itself in humans.
Conclusion and Recommendations
From the research results we can conclude as follows:
Vitamin-D levels 25-OH were significantly reduced in patients
with hypothyroidism. Patients with anti-TPO positive suffered
more from hypovitaminosis D than those with negative anti-
TPOs. Vitamin-D deficiency was associated with the presence of
autoantibody of the thyroid and abnormal thyroid functions.
Considering the importance of Vitamin-D, we recommend:
Further research fully illuminate the role of Vitamin-D levels in
autoimmune thyroiditis, and provide knowledge of Vitamin-D
efficiency and safety as a therapeutic tool for Aitd.
Acknowledgement
We would like to acknowledge the contribution of proofreading
the article of Prof. Ass.Dr. Mulaim Kacka from the Heimerer
College, for the critical review of this manuscript.
Statement of Interests
The authors declare no conflict of interest.
References
- Stathatos N, Daniels GH (2012) autoimmune thyroid disease. Curr Opin Rheumatol 24:70–5.
Indexed at, Google Scholar, Crossref
- Wang J, Lv S, Chen G, Gao C, He J, et al. (2015) Meta-analysis of the association between vitamin D and autoimmune thyroid disease. Nutrients 7:2485–2498.
Indexed at, Google Scholar, Crossref
- Chaker L, Bianco AC, Jonklaas J, Peeters RP (2017) hypothyroidism. Lancet 390:1550–1562.
Indexed at, Google Scholar, Crossref
- AG Madariaga, Santos PS, Guillén GF, Galofré JC (2014) the incidence and prevalence of thyroid dysfunction in Europe a meta-analysis. J Clin Endocrinol Metab 99:923-931.
Indexed at, Google Scholar, Crossref
- Vanderpump MP (2011) the epidemiology of thyroid disease.Br Med Bull 99:39-51.
Indexed at, Google Scholar, Crossref
- Almandoz JP, Gharib H (2012) Hypothyroidism etiology diagnosis and management. Med Clin North Am 96:203-221.
Indexed at, Google Scholar, Crossref
- Amaya AJ, Rojas-Villarraga A, Anaya JM (2014) cardiovascular disease in the antiphospholipid syndrome. Lupus 23:1288-91.
Google Scholar, Crossref
- Meng, Zhaowei (2015) Gender and age impacts on the association between thyroid function and metabolic syndrome in Chinese. Medicine 94: e2193.
Indexed at, Google Scholar, Crossref
- Aggarwal N, Razvi S (2013) Thyroid and aging or the aging thyroid? An evidence-based analysis of the literature. J Thyroid Res 2013:481287.
Indexed at, Google Scholar, Crossref
- Mammen JS, McGready J, Ladenson PW, Simonsick EM (2017) Unstable thyroid function in older adults is caused by alterations in both thyroid and pituitary physiology and is associated with increased mortality. Thyroid 27:1370–1377.
Indexed at, Google Scholar, Crossref
- Calcaterra V, Montalbano C, Miceli E, Luinetti O, Albertini R, et al. (2020) Antigastric parietal cell antibodies for autoimmune gastritis screening in juvenile autoimmune thyroid disease. J Endocrinol Invest 43:81-86.
Indexed at, Google Scholar, Crossref
- Tamer G, Arik S, Tamer I, Coksert D (2011) Relative vitamin D insufficiency in Hashimoto's thyroiditis. Thyroid 21:891-896.
Indexed at, Google Scholar, Crossref
- A Gil, Plaza-Diaz J, Mesa MD (2018) Vitamin D Classic and Novel Actions. Ann Nutr Metab 72:87-95.
Indexed at, Google Scholar, Crossref
- Doohe Kim (2017) The Role of Vitamin D in Thyroid Diseases. Int J Mol Sci 18:1949.
Indexed at, Google Scholar, Crossref
- General Information/Press Room [Internet]. American Thyroid Association.
- Idiculla J, Prabhu P, Pradeep R, Khadilkar K, Kannan S (2018) Vitamin D and primary hypothyroidism: Is there an association? Thyroid Res Pract 15:34.
Google Scholar
- National Health Service (NHS). Vitamin D. 2022.
- Richards B (2008) Low vitamin D contributes to thyroid problems. Health news.
Google Scholar