Review - (2022) Volume 13, Issue 2
Reproductive Health, Social and Financial Impact of Valproic Acid Withdrawal for Childbearing Epileptic Saudi Woman
Neveen Fathi2,
Miraven Mupas1,
Said Moussa1,
Assem Mustafa3,
Tamir Abdeljawad4,
Bashir Ighle2 and
Hassen Al Dawssary5
1Department of CQI & PS, Armed Forces Hospital Wadi Al Dawassir, Saudi Arabia
2Department of Internal Medicine, Armed Forces Hospital Wadi Al Dawassir, Saudi Arabia
3Laboratory Department, Armed Forces Hospital Wadi Al Dawassir, Saudi Arabia
4Department of Radiology, Armed Forces Hospital Wadi Al Dawassir, Saudi Arabia
5Department of Surgery, Armed Forces Hospital Wadi Al Dawassir, Saudi Arabia
Received: 09-Feb-2022, Manuscript No. ipjnn-22-12493;
Editor assigned: 11-Feb-2022, Pre QC No. P-12493;
Reviewed: 04-Mar-2022, QC No. Q-12493;
Revised: 07-Mar-2022, Manuscript No. R-12493;
Published:
14-Mar-2022
Abstract
Epilepsy complicates a woman`s reproductive life. The physiological modification of the woman and the effects of antiepileptic drugs are generally the cause. Several complications may be added during treatment that requires careful monitoring. The risks in women of childbearing age associated with prenatal Valproic Acid Drug (VPA) exposure are becoming established, and updated recommendations are being made internationally for restrictions to (VPA) use and enhanced preconception counseling in this patient group.
To minimize these complications we implement same protocol in the different hospital departments to assure high quality of care for childbearing age women. As a result we remark a decrease number of patients using (VPA) and improvement of the quality of reproductive health and per consequence reducing hospital and societal costs.
Keywords
Childbearing age women; Epilepsy; Valproic acid; Depakin complication;
Hospital and social cost
Introduction
Being a woman with epilepsy is not the same as being a man
with epilepsy. Epilepsy affects sexual development, menstrual
cycle, aspects of contraception, fertility, and reproduction.
Epilepsy causes significant medical and social costs, and places an
economic burden on society and individuals by causing increases
in healthcare costs, as well as losses in employment, wages and
household work [1-3]. (VPA) interferes with the endocrine system
at multiples levels causing several reproductive and sexual
dysfunctions in women with epilepsy [2,4].
It is now not recommended that (VPA) should be prescribed
routinely for women with child-bearing potential. If (VPA) use
is inevitable, then recommendations are for a clinical discussion
involving teratogenic risk, pregnancy planning, and contraception
advice [5-7].
NICE 2021 advice a special consideration for women and girls
with epilepsy and prepare a special pathway to manage during
the child-bearing period [8]. The main objective of our study
is to provide health promotion, screening and interventions
to epileptic women of childbearing age using (VPA) before
conception and thereby improve pregnancy-related outcomes.
Method
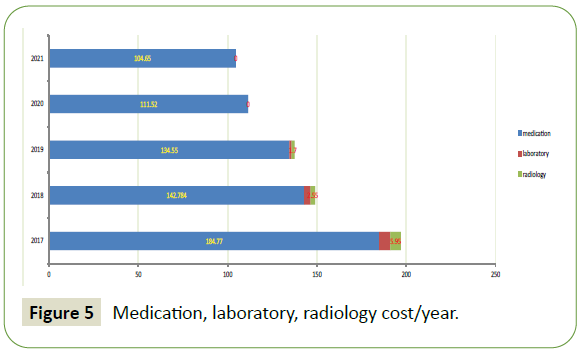
This study was carried out after the establishment of a similar
management protocol in all the departments that take care of
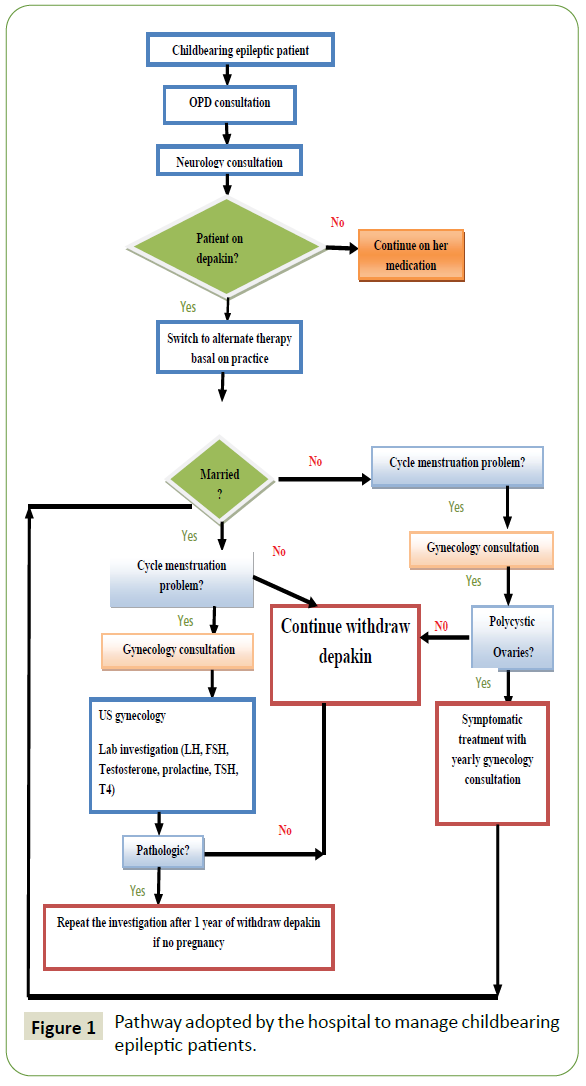
epileptic patients of childbearing age (Figure 1).
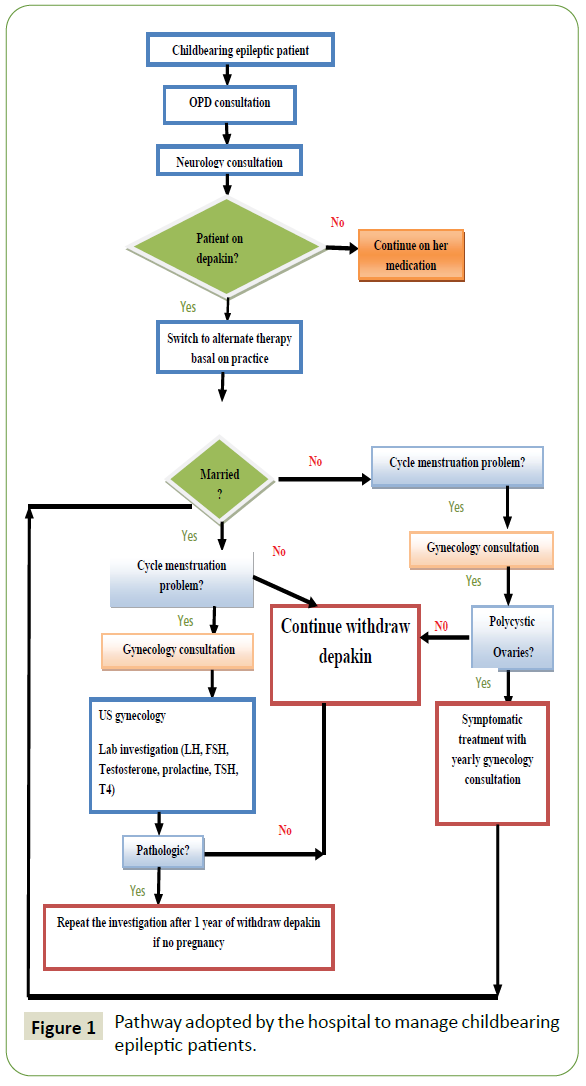
Figure 1: Pathway adopted by the hospital to manage childbearing
epileptic patients.
We are interested in calculating only the cost of laboratory
tests and radiological examinations necessary to investigate
the potential indisputable effects of (VPA) and the costs of
pharmaceuticals as preliminary project. The cost of admissions, visits by general practitioners and specialists, have not been
calculated on the one hand because it is a preliminary study and
on the other hand these management are offered free of charge
in our hospital.
A same protocol has been implemented in the different
departments involved in the management of a child-bearing
epileptic patient (since the age of 9 years to 45 years old) (Figure
1). All female patients with diagnosis of epilepsy (OPD, pediatric
clinic and gynecology clinic) are referred to neurology clinic.
Once the patient visits a neurology clinic the neurologist will
take from history some focus information’s (general information,
questions about treatment given for epilepsy, problems related
to period, sterility problem, planning for pregnancy). The patient
switched to another antiepileptic progressively if the patient is
initially was on (VPA). The patient who are on (VPA) and they plan
for pregnancy or have problem to get pregnant should be seen by
gynecology for laboratory investigation and pregnancy planning.
Each year we calculated the number of patient using (VPA),
endocrinology problems resolved and the cost of treating
reproductive health problems. We chose as direct cost only the
blood tests and the radiological exams requested to explore the
side effects of (VPA). Investigations done to have diagnosis are
the same for all epileptic patients in our hospital that is why we
did not include these parameters in our study. Drug costs were
based on the year 2017 acquisition cost of drugs by the hospital.
Total drug costs were then calculated using the unit prices and
duration of prescriptions.
Ethical considerations
Ethics committee review was not required for this project as it
was a quality improvement project for already existing practices
and treatments in the hospital.
Results
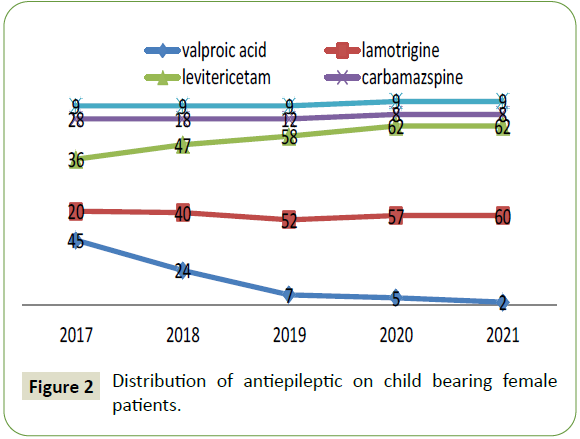
Between November 2017 and October 2021, the total number
of female epileptic patients was 269. Patients who are on childbearing
period (9-45) were 125. Initially on 2017, 45 Patients
were on (VPA) (36%), the others patient were on Lamotrigine (20)
16%, Carbamazepine (28) 22.4%, Leviterecitam (36) 28.8% and
(9) 7.2% on Phenytoin (Figure 2).
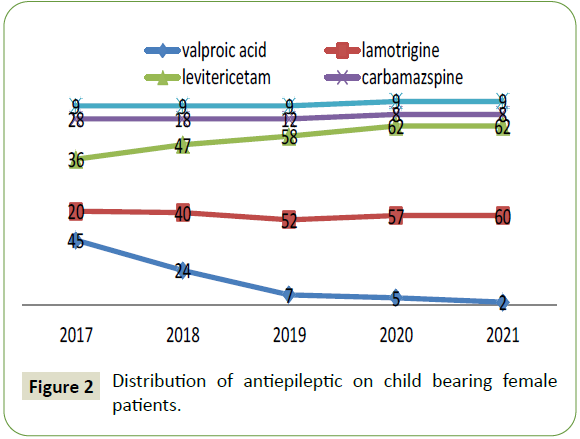
Figure 2: Distribution of antiepileptic on child bearing female patients.
2021 only two patients were on VPA. One of them was Down
syndrome and she is on bi-therapy the other one is cerebral
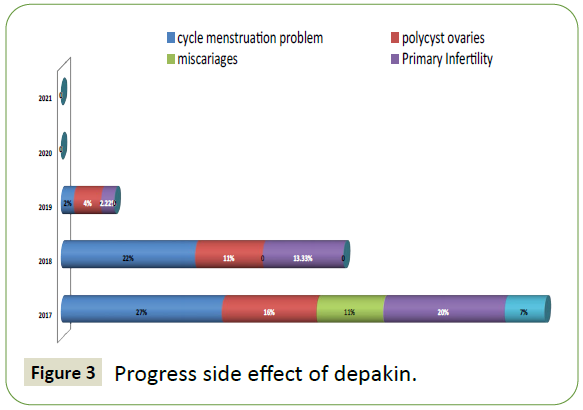
palsy. The following diagram (Figure 3) summarizes the various
undesirable effects observed in epileptics patients treated with
VPA. In our study we are only interested in the cost directly
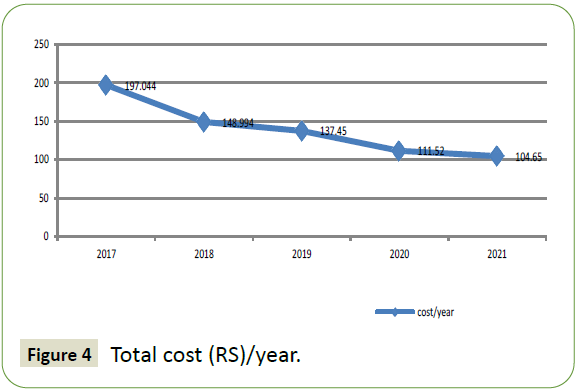
related to the side effects caused by VPA (Figures 4 and 5).
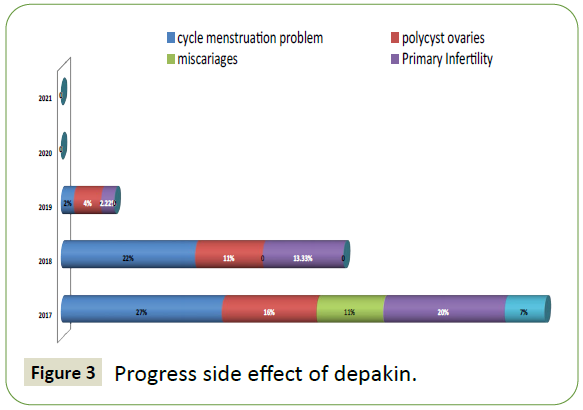
Figure 3: Progress side effect of depakin.
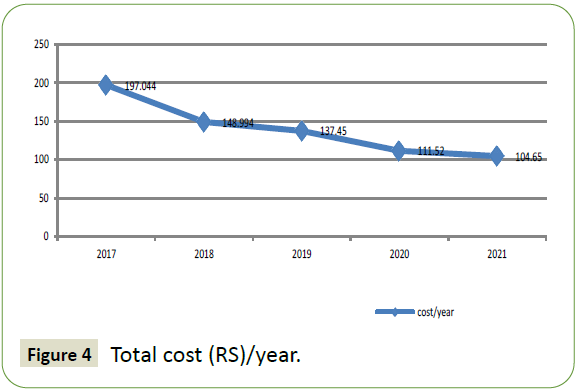
Figure 4: Total cost (RS)/year.
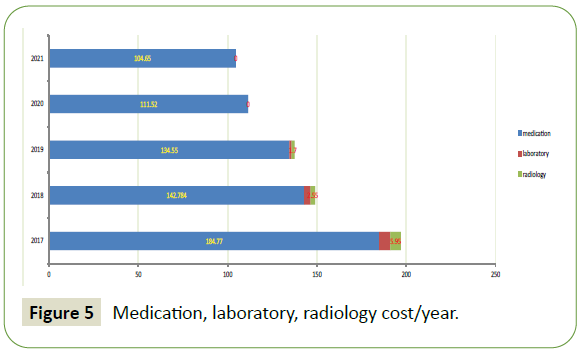
Figure 5: Medication, laboratory, radiology cost/year.
Discussion
Epilepsy is an important public health issue in many countries.
The prevalence of this disease is estimated between 5 and
9.3/1,000, with a predominance feminine of the period from
10 to 14 years [5]. Sub fertility and sexual disorders in epileptic
patients are known and have been described for the first time in
1954 by Gastaut and Collomb Epilepsy causes significant medical
and social costs, and places an economic burden on society and individuals by causing increases in health care costs, as well as
losses in employment, wages and household work [8].
Little information is available with regards to epilepsy and
antiepileptics drugs (VPA) complication in Saudi women
with epilepsy. The particularity of our study is to show the
improvement of the reproductive health of epileptic patients
under (VPA) after the gradual withdrawal of this antiepileptic in
patients of childbearing age and then calculate the cost saving
to the hospital after adequate management from the onset of
the disease of patients with epilepsy. The current study found
a decline in the rate of prescription of (VPA) between 2017 and
2021 from 36% to 1.6%.
On 2017, 26% of our patients who are on (VPA) have experience
abnormalities in menstrual cycle, 26% have problems to get
pregnant and 15% of them have the diagnosis of Polycystic Ovary Syndromes (PCOS). One study reports that ovulation was delayed
in women with epilepsy [9]. Another study published on 2012
conclude that there is an increased incidence of PCOS in Chinese
women with epilepsy at reproductive ages, by more than 2 times
of that in the general population. Risk factors include seizures
starting at a young age and (VPA) therapy [10].
Actually is well known that antiepileptic Drugs, particularly VPA, may change serum concentrations of reproductive hormones in
patients with epilepsy, thus contributing to the development of
reproductive dysfunction [5]. In our study 26% of our patients
have problems to get pregnant and 41% (5 patients) of them the
hormonal check-up was pathologic.
Endocrine problems were clear in our population. A Filnandan
study followed 35 epileptics women aged 12-25 years for an
average of 5.8 years who received (VPA). All of these women had
hyper-endrogenia, 63% had (PCOS), increased blood levels of
prolactin, hormones secreted by the pituitary and hypothalamus
[11].
Laboratory measurements include serum levels of PRL, LH, FSH,
testosterone, GnHR and thyroid hormones are indicated to
epileptic women on (VPA) with irregular menstrual or difficulty
to get pregnant [5]. Two of our patients were switched to
Lamotrigine and 2 years after they have their first baby. One
of them was programmed to an artificial insemination but she
get pregnant spontaneously only by withdraw (VPA). The same
result was found in another study when they switch from (VPA) to
Lamotrigine. They remarked reversal of hyper-androgenism, and
normalization of ovarian morphology [12].
Once improving reproductive health in women of childbearing
age remains the primary goal of any health system, it becomes
necessary to identify and address the various obstacles. This is
why economic analysis is an indispensable tool in the promotion
and production of preventive therapies and effective strategies
for different diseases and in particular those with a heavy social
and economic burden such as epilepsy.
We study only the direct cost of (VPA) complications in child
bearing epileptic female patients. We found that when we shift
patients from (VPA) to another safe treatment we gain 90.000 RS
(only for 45 patients) that is mean 2.000 RS per patient and per
years.
We should know that our cost include only cost of medication,
laboratory and gynecologic ultra sound requested to investigate
gynecologic problems. We have chosen to study the treatment
cost in childbearing age patient because this age range is
important in the improvement of reproductive health.
The majority of publications talk about the undesirable effects
of (VPA) and its cost on pregnancy and newborns [13], but the possibility of preventing these damages from an early age in
epileptic women of childbearing age is not clearly mentioned in
literature.
The gain was significant despite the fact that our patients were
put on the new antiepileptic which is more expensive than the
old antiepileptic. This shows that an early catch can prevent
this burden [14]. The cost of hospitalization, visits by specialists
and family doctors have not been calculated because they are
provided free of charge to our hospital.
The indirect cost that is not calculated in our study and has
been mentioned in other studies [15], such as lost days of work,
psychological and family comfort felt by our patients. These
studies looking at the direct and indirect cost of epilepsy have
shown that the indirect cost is at least 58% of the total cost [3,16].
In addition, the majority of our patients were students or women
working. We have seen an improvement in their productivity and
a clear decrease in demand for sick leave during consultation.
Conclusion
This preliminary study provides the cost data for the treatment of child bearing female patient in Saudi Arabia. The results can
help not only the institution concerned, but also the country as
a whole in the appropriate and efficient distribution of health
care resources. The results can also provide a useful basis for
pharmaco-economic evaluations of interventions, such as those
of the new antiepileptic, despite being more expensive than the
old antiepileptic (VPA) but providing better protection for this
category in terms of reproductive health, quality of life and social
and hospital cost.
Limitation of our Study
A limit of our study is that it is menu on a small population.
The indirect cost that we did not calculate has a large effect on
reproductive health outcomes, with a large effect on reducing
hospital and social costs.
It is time to pay more attention to this category and to develop a
program at the level of the Kingdom to improve the reproductive
health of childbearing women because of its repercussions on the
economic and the well-being of future mother and descendants.
REFERENCES
- Lemahafaka GJ, Fenomanana SM, Tehindrazanarivelo AD (2019) Epilepsy and reproductive health: challenges and prospects. Pan Afr Med J 34: 81.
Google Scholar, Crossref, Indexed at
- Bonnet D, Guillaume A (2004) La santé de la reproduction: une émergence des droits individuels. Centre Population et Developpement (CEPDE) Google Scholar pp: 11-20.
Google Scholar
- Al-Zakwani I, Hanssens Y, Deleu D, Cohen A, et al. (2003) Annual direct medical cost and contributing factors to total cost of epilepsy in Oman. Seizure 12: 555-560.
Google Scholar, Crossref, Indexed at
- Baldwin D, Wieck A (2018) Withdrawal of, and alternatives to valproate containing medicines in girls and women of childbearing age. RCPsych pp: 4-18.
- Mohamed HTE, Alanazi AOZ, Alshammari TMM, Alshammari ANM, Alenezi OML, et al. (2020) Epilepsy in Saudi Arabia: prevalence in different regions, causes, risk factors, and management: A systematic review. Int J Pharmaceut Phytopharmacol Res 10: 92-99.
- Witchel SF, Oberfield SE, Peña AS (2019) Polycystic ovary syndrome: pathophysiology, presentation, and treatment with emphasis on adolescent girls. J Endocr Soc 3: 1545-1573.
Google Scholar, Crossref, Indexed at
- Verrotti A, Greco R, Latini G, Chiarelli F (2005) Endocrine and metabolic changes in epileptic patients receiving valproic acid. J Pediatr Endocrinol Metab 18: 423-430.
Google Scholar, Crossref, Indexed at
- Special considerations for women and girls with epilepsy. NICE 2021.
- Gastaut H, Collomb H (1954) Étude du comportement sexuel chez les épileptiques psychomoteurs. Ann Med Psychol 2: 657-696.
Google Scholar
- Herzog AG (2016) Current concepts of catamenial epilepsy. Epilepsi 22: 75-85.
Google Scholar
- Zhou JQ, Zhou LM, Chen LJ, Han JD, Wang Q, et al. (2012) Polycystic ovary syndrome in patients with epilepsy: A study in 102 Chinese women. Seizure 21: 729-733.
Google Scholar, Crossref, Indexed at
- Acide valproique pertuebeur endocrinien. la revue prescrire, janvier 41: 25-30.
- Svalheim S, Sveberg L, Mochol M, Taubøll E (2015) Interactions between antiepileptic drugs and hormones. Seizure 28: 12-17.
Google Scholar, Crossref, Indexed at
- Melkamu P, Animut Y, Minyihun A, Atnafu A, Yitayal M (2021) Cost of illness of epilepsy and associated factors in patients attending adult outpatient department of university of gondar referral hospital northwest Ethiopia. Risk Manag Healthc Policy 14: 2385-2394.
Google Scholar, Crossref, Indexed at
- Koba CM, Bashizi PB, Kongolo CM, Bora BK (2018) Evaluation du cout du traitement antiepileptique a lubumbashi. IOSR J Dental Med Sci 17: 76-80.
Google Scholar, Crossref, Indexed at
- Shin J (2016) Direct and indirect cost of epilepsy: latest estimates from the medical expenditure panel survey. The University of Texas School of Public Health. Pro Quest Dissertations Publishing pp: 1013-1761.
Google Scholar
Citation: Mokni N, Fathi N, Mupas M, Moussa S, Mustafa A, et al. (2022) Reproductive Health, Social and Financial Impact of Valproic Acid Withdrawal for Childbearing Epileptic Saudi Woman. J Neurol Neurosci Vol.13 No.2:413.