Ming-Hung Tsai1,2,3, Chi-Ming Wu3,4, Ming-Hong Lin1, Ching-Zong Wu5,6, Han-Yi Cheng3,4,7 and Keng-Liang Ou3,4,7,8*
1Department of Mechanical Engineering and Graduate Institute of Mechanical and Precision Engineering, National Kaoshiung University of Applied Sciences, Kaoshiung 807, Taiwan
2Department of Dentistry, Chang Yin dental clinic, No.46-1, Yangming St., Banqiao City, Taipei County 220, Taiwan
3Research Center for Biomedical Devices and Prototyping Production, Taipei Medical University, Taipei 110, Taiwan
4Graduated Institute of Biomedical Materials and Tissue Engineering, College of Oral Medicine, Taipei Medical University, Taipei 110, Taiwan
5School of Dentistry, College of Oral Medicine, Taipei Medical University, Taipei 110, Taiwan
6Department of Dentistry, Taipei Medical University Hospital, Taipei 110, Taiwan
7Research Center for Biomedical Implants and Microsurgery Devices, Taipei Medical University, Taipei 110, Taiwan
8Department of Dentistry, Taipei Medical University-Shuang Ho Hospital, Taipei 235, Taiwan
Corresponding Author:
Keng-Liang Ou
Research Center for Biomedical Devices and Prototyping Production
Taipei Medical University, Taipei 110, Taiwan
Tel: 886-2-27361661
Fax: +886-2-27395524
Email: klou@tmu.edu.com
Citation: Ming-Hung T, Chi-Ming W, Ming-Hong L, et al. Research on Biomechanical Behavior of Temporomandibular Joint Disorders Using Occlusal Splint Treatment: Computed-Aided Analysis. J Biomedical Sci. 2015, 4:2. doi:10.4172/2254-609X.10008
Copyright: © 2015 Ming-Hung T. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Keywords
Biomechanical behavior; Finite element analysis; Splint therapy; Temporomandibular joint; Von Mises stress
Introduction
Temporomandibular joint disorders (TMDs) are common in adults, and one-third of adults report having one or more symptoms, which include joint pain, headache, and clicking or grating within the joint [1-3]. It is referred to as a cluster of conditions characterized by pain in the temporomandibular joint (TMJ) during motion. Despite the wide use of oral splints in the treatment of TMDs and bruxism, their mechanisms of action remain unclear and controversial [4]. Splint treatment is worth investigating, although occlusal adjustment is not an accepted treatment in all parts of the world. The material of the splint is widely investigated, focusing on wear resistance [5-7]. This technique has been discouraged as a treatment, in contrast to the author’s statement [8,9]. Nevertheless, some patients suffering from a TMJ syndrome will improve or become cured when occlusal splint treatments are used [10-12]. There are several kinds of therapies commonly used for the treatment of TMJ disorders. Noninvasive therapies should be considered before pursuing invasive, permanent, or semi-permanent treatments that have the potential to cause irreparable harm.
Finite element analysis is a useful tool that can be applied to quantify the stress distribution in the TMJ and surrounding tissues, and it has been previously used in the study of biomechanical behavior of orthopedic devices, including hip, knee, and spinal implants, under various loading conditions [13-15]. Until today, no literature has reported on the use of a three-dimensional (3D) model for comparison of the TMJ to understanding the stress fields of TMDs before and after occlusal splint treatment, although numerous finite element simulations of the TMJ have been performed [16,17].
To examine the biomechanical behavior of TMDs, one must focus on the magnitude and location of the maximum stresses under physiological loading. Therefore, the aim of this study was to develop 3D finite element models reconstructed from in vivo image data, to quantify the stress distribution in the mandibular condyle, disc, and articular eminence, and to further investigate the von Mises stresses of the models during jaw closing and maximum opening before and after occlusal splint treatment.
Materials and Methods
Patient selection and therapeutic intervention
Six patients (mean age ± SD: 37.45 ± 5.81 years; range: 34 to 41 years) suffering from anterior disc displacement without reduction in the TMJ were enrolled in this study. The objectives were to investigate the stress distributions of TMJ models before and after splint treatment, and then to further compare the six symptom free TMJ models (control group). The patients received an occlusal splint treatment, which covered the entire upper dental arch. They were advised to wear the splint day and night, excluding mealtimes for six months. Regular check-ups were performed and adjustments made once every two months to ensure that the close contacts of the occlusal splint were balanced. No additional drugs or manual therapies in this study were adopted or performed.
Ingestion and transformation of TMJ numerical images
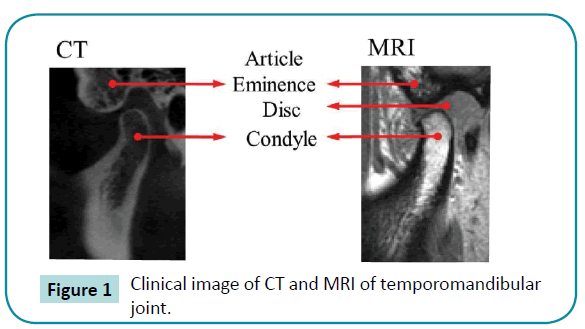
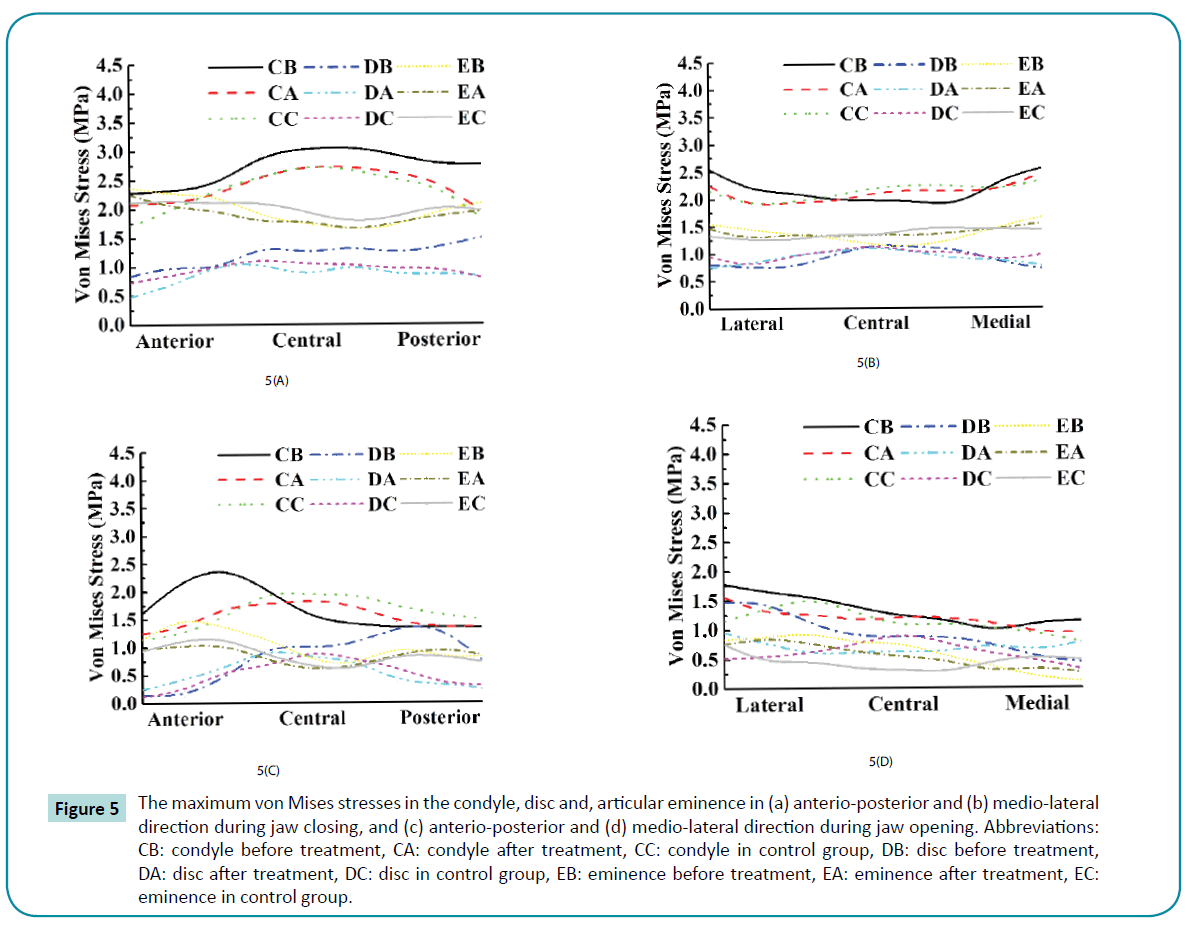
For the reconstructed model, magnetic resonance imaging (MRI, slices at 1 mm intervals; HDx 3.0T, Signa, USA) and computed tomography (CT, slices at 1 mm intervals; High Speed CT1, General Electrics, USA) examinations were conducted with closed and maximum open mouth positions in the parasagittal section, as shown in Figure 1.
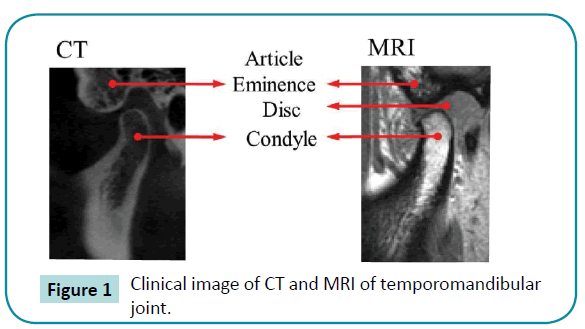
Figure 1: Clinical image of CT and MRI of temporomandibular joint.
The images were segmented for data extraction to describe the surfaces of the condyle, disc, and articular eminence. An edge detection algorithm was used with AVIZO 6.2 (Internet Securities, Inc., USA) to distinguish cortical bone from cancellous bone and to detect the various boundary components of the mandible.
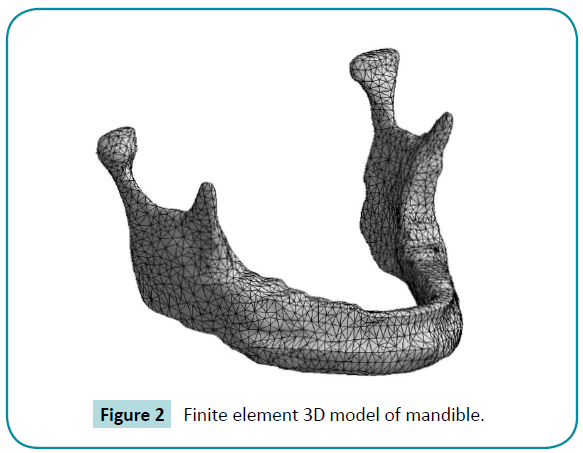
The 3D image reconstruction and solid modeling were conducted using ANSYS Workbench 12.1 (ANSYS, Inc., USA) finite element software. Upon reconstruction of the condyle hard tissue and articular eminence from CT data, the soft tissue of the disc was detected using MRI data. A condyle cartilage layer with a uniform thickness of 0.2 mm was added to the bony surface of the mandibular condyle [18], and the friction coefficient inside the TMJ was assumed to be 0.01 [19]. The structures of the condyle, disc, and articular eminence were regarded as a continuous integer. In order to obtain accurate results from the finite element method, converging and reinforcing the mesh are one of the major important processes that allow the model to approach the actual conditions. Through five convergence processes, we could assume a reliable mesh, and the final 3D model consisted of approximately 280,000 nodes and 160,000 solid elements. The elements adopt tetrahedral features with 10 nodes, i.e., each side had a mid-side node, and three degrees of freedom, as shown in Figure 2.
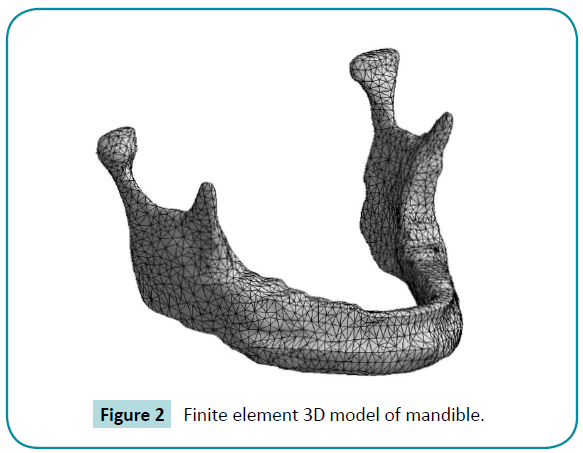
Figure 2: Finite element 3D model of mandible.
The properties of the cortical bone, cancellous bone, and articular disc of the TMJ were defined in previous literature [20,21]. The condyle surface is defined by the properties of the cortical bone, whereas internal nodes were assigned to the cancellous bone. However, due to the elastic modulus of the condyle cartilage layer, which is similar to that of hyaline cartilage of several other synovial joints, the condyle cartilage layer was defined as a nonlinear material to better mimic in vivo properties of the mandibular condyle [22].
Mathematical model
The mastication muscles on the TMJ are complex and transmit functional chewing forces during jaw movement [23]. The three muscles used during mastication, masseter, medial pterygoid, and temporalis, are activated to close the mouth, while the lateral pterygoid is used for mouth opening. It is necessary to know the cross-sectional area (CSA) to determine the maximum muscle force via the following mathematical function [24]. This method integrates the CSA of the muscles for accuracy and reliability. The maximum muscle forces of each are as follows: masseter, left side: 176.86 N, right side: 161.32 N; temporalis: 104.71 N, 125.80 N; medial pterygoid: 87.69 N, 79.18 N; and lateral pterygoid: 107.67 N, 95.46 N.
Fimax = K × CSA (1)
Equatation (1) estimated the maximum muscle forces possible based on the CSA, where K = 37 N cm-2.
Statistical analysis
The nonparametric Kruskal-Wallis test was used to calculate statistical significance among the groups, and all data were stored and processed with Excel. The mean and standard deviations of each group were compared using analysis of variance. For all statistical analyses, values of p < 0.05 were considered statistically significant.
Results
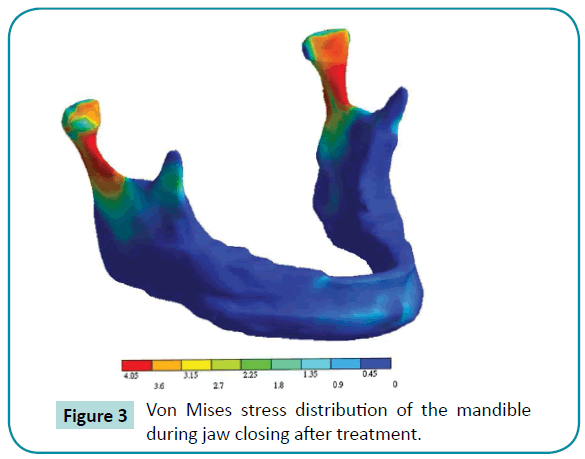
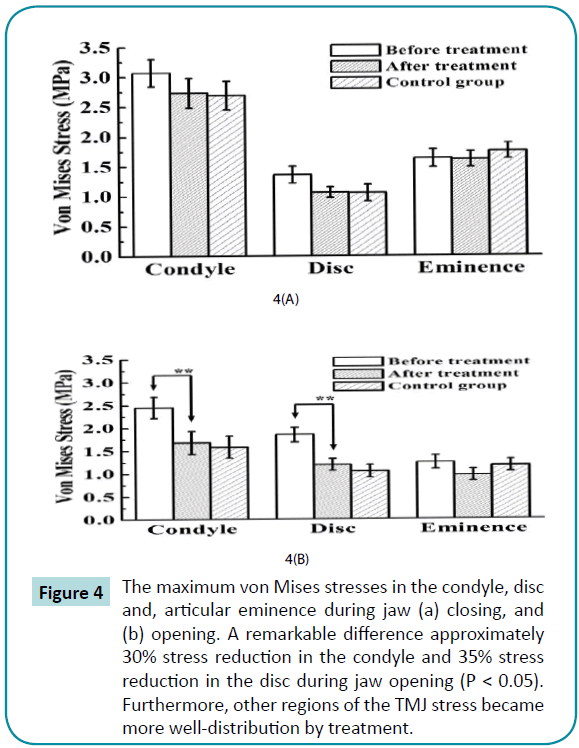
For successful occlusal splint treatment, it is highly recommended to reduce the von Mises stresses of the mandibular condyle, disc, and articular eminence. Figure 3 displays the stress distribution of one model during jaw closing, showing the interface between condyle, disc, and eminence after treatment. For the entire TMJ model, the highest von Mises stress varied from 0.74 MPa to 3.34 MPa (Figure 4). An approximately 30% stress reduction in the condyle and 35% stress reduction in the disc were found during jaw opening (p < 0.05), a remarkable difference. Furthermore, stress in other regions of the TMJ became well distributed after treatment. The maximum stresses were usually in the anteriorposterior directions in all regions.
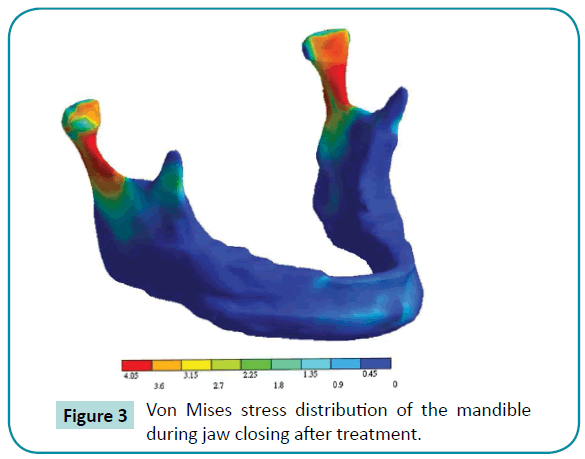
Figure 3: Von Mises stress distribution of the mandible during jaw closing after treatment.
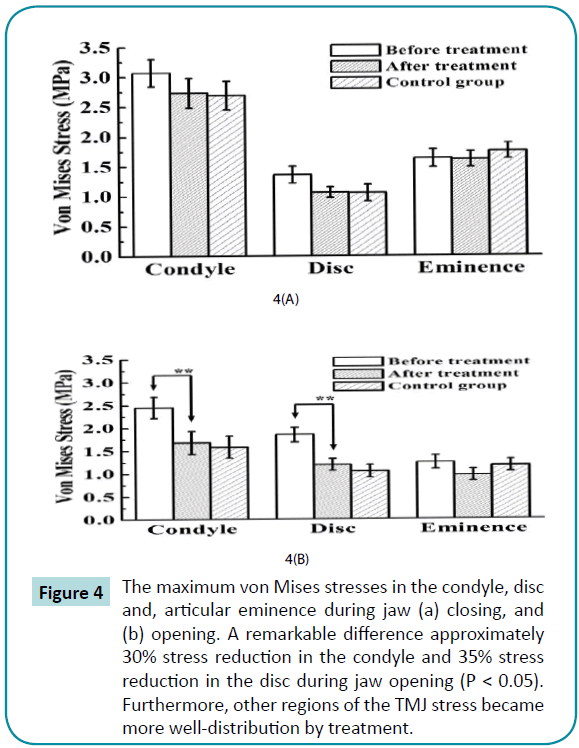
Figure 4: The maximum von Mises stresses in the condyle, disc and, articular eminence during jaw (a) closing, and (b) opening. A remarkable difference approximately 30% stress reduction in the condyle and 35% stress reduction in the disc during jaw opening (P < 0.05). Furthermore, other regions of the TMJ stress became more well-distribution by treatment.
Magnitude and location of the highest stress
In the mandibular condyle region, the highest stress varied from 1.35 to 3.34 MPa, and the highest stress was observed in the central mandibular condyle. It was observed that the highest Von Mises stress changes after treatment, and the decrease in stress after treatment in the central region shows no statistically significant differences (p > 0.05). The maximum stresses varied from 0.98 to 1.93 MPa in the articular disc region, whereby the highest stress observed was an abnormal stress focusing on the posterior region during jaw opening before treatment, and its stress distribution after treatment became well distributed. For the articular eminence, the highest von Mises stress varied from 0.93 to 1.82 MPa, and there were no significant differences among the groups before and after treatment (p > 0.05).
Stress distributions analysis
There were similar tendencies in the stress simulation among the six patients; therefore, one model was selected on which to perform the following stress distribution analysis in the anterioposterior and medio-lateral directions (Figure 5). It was found that the stress is reduced and the stress curve approaches that of the control group after treatment. The stress distribution of the condyle increased in the central region, and the stress value increased slightly in the posterior articular eminence during jaw closing, as shown in Figure 5a. During jaw opening, significantly abnormal stresses are observed in the anterior condyle and posterior disc of TMD patients due to anterior disc displacement without reduction (Figure 5c). However, in the medio-posterior direction, differences among groups were not able to be determined (Figure 5b, d). In addition, for the condyle stress and disc release during the course of treatment, the stress curves after treatment displayed similar tendencies to that of the control group.
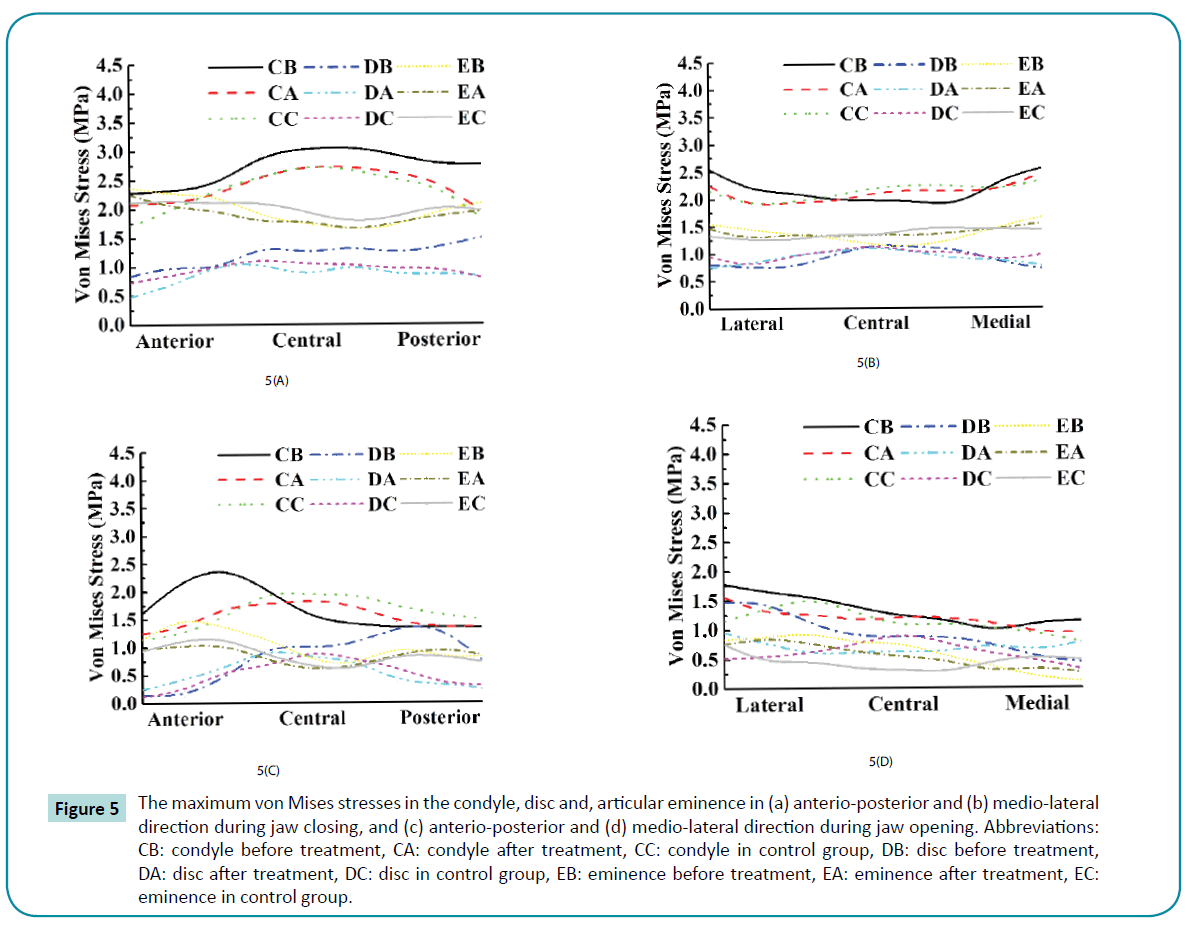
Figure 5: The maximum von Mises stresses in the condyle, disc and, articular eminence in (a) anterio-posterior and (b) medio-lateral direction during jaw closing, and (c) anterio-posterior and (d) medio-lateral direction during jaw opening. Abbreviations: CB: condyle before treatment, CA: condyle after treatment, CC: condyle in control group, DB: disc before treatment, DA: disc after treatment, DC: disc in control group, EB: eminence before treatment, EA: eminence after treatment, EC: eminence in control group.
As part of the contact region, the load transferred from the mandibular condyle to the disc and articular eminence during function is established. It was observed that the maximum stress was generated at the contact points. The applied stress is considered the most important factor for long-term success of TMD treatment. Furthermore, the bone response will depend on the applied stress because of the overload stress in most cases. This is highlighted during overloading, showing the condyle stresses in jaw closing, the condyle and disc during opening before treatment, the well-distributed stresses, and the release after occlusal splint therapy.
Discussion
Although occlusal adjustment is not an accepted in all parts of the world, there are many successful cases documented in previous studies. TMJ pain and dysfunction were treated with stabilization splints in a one-year follow-up in 2005. Joint noise was observed to be reduced, and it is concluded that occlusal splint therapy is beneficial for the management of intra-articular pain and dysfunction. Furthermore, there are no risks of irreversible occlusal changes [11]. Forty patients with three different kinds of disorders were treated with splint therapy for eight weeks. Eighty percent of the patients were free of joint noise and pain at the end of the treatment period, and each patient’s TMJ returned to ordinary function. The patients were reevaluated 2.5 years later, and 75% of the patients had no joint pain. Sixty-six percent of the patients did not seek additional treatment for jaw pain and dysfunction [25]. Two different types of splint stabilization methods, splint therapy and pivot splint therapy, which are used in patients with painful anterior disc displacement of the TMJ, were compared (n = 20). There was a significant increase in the maximum jaw opening and a significant reduction of pain in both therapy groups. However, the differences between the groups were not statistically significant (p > 0.05). It was determined that both types of splints provided effective therapy in patients with anterior disc displacement [12].
In contrast to the author’s statement, this technique has been discouraged as a therapy. Occlusal splint therapy was compared to other therapies in the treatment of 20 patients with internal TMJ derangement with reduction. Flat plane occlusal splint treatment produced no significant changed in the dysfunction level of patients with internal joint derangements with reduction [8], and Hateta demonstrated that therapeutic exercise contributed to earlier recovery of jaw function compared with splints [9].
Data analysis indicates that the condyle and eminence are more precisely modeled with CT than MRI images. Nevertheless, MRI could generate the disc component that could not be tracked by CT. Therefore, using CT to reconstruct hard tissue and MRI to reconstruct soft tissue produces the most precise model of the TMJ.
The von Mises stresses in the mandibular condyle were considerably reduced by approximately 10% and 5% in the central and medial regions, respectively, and by approximately 15% in the anterior regions. The anterior, central, and medial regions of the mandibular condyle are considered important functional regions that sustain masticatory loading [26]. Treatment could release abnormal focusing stresses on these important regions. In the posterior and lateral regions, there is a stress-shielding problem before treatment. Decreasing the load would lead to severe resorption, while a mechanical stimulus or stress in the skeleton is one of the major factors in the maintenance of a normal balance between the dynamic processes of bone formation and resorption [27]. The abnormal effects of stress shielding are known to persist. This could promote the stressshielding problem in the posterior and lateral regions as a result of treatment.
Several researchers have attempted to assess or measure the mechanical loads directly in the TMJ during jaw movement by a strain gauge technique, which indicates that substantial forces are induced and, hence, the TMJ is acting as a load-bearing member [28]. However, these experimental approaches have shortcomings, such as surgical invasion of the TMJ structures. On the other hand, the analytical techniques of the finite element method have been used to investigate stresses and forces in the TMJ by mathematical models for a long time [29]. Researchers in the biomechanics field have successfully used these analytical techniques, which posses the following advantages [30]. These techniques measure the internal stresses in the model and can easily simulate conditions with different magnitude forces or bone densities. Another important factor, which governs the results of the analyses, is the mechanical and physical properties of the model compared with the actual object. In this study, there were four main materials, cortical bone, cancellous bone, condyle cartilage layer, and articular disc. The condyle cartilage layer is composed of mainly large proteoglycans, such as aggrecan and versican [31,32]. In general, large proteoglycans are more suited for resisting compressive forces than the articular disc, which is composed mainly of collagen fibers [33]. Accurate representation of the condyle cartilage layer in the TMJ finite element model is of great importance. The nonlinear material of the condyle cartilage layer is likely to more accurately mimic the in vivo properties of the mandibular condyle. The elastic modulus of the condyle cartilage layer is similar to that of hyaline cartilage in other joints. The addition of the condyle cartilage layer to the model was found to be the primary cause of the reduction in the loading of the mandibular condyle, as opposed to the disc or articular eminence. These findings led to the hypothesis that the mandibular condyle is more likely to function as a shock absorber than the disc [34].
Our present study provides us with useful information related to stress distribution and the probability of locating areas that may be most likely to experience TMDs. The limitations of our study are as follows: (1) it adopted uniform muscle forces; (2) the viscoelasticity of bone was not taken into account; and (3) this study was based on a theoretical analysis.
Conclusion
The present results proposed that TMDs could be cured using occlusal splint treatments, which promote the stress problem. There are many controversial issues surrounding occlusal splint treatment for the management of TMDs; nevertheless, splint therapy was able to release the overloading stress in this study. An approximately 30% stress reduction in the condyle and 35% stress reduction in the disc were found during jaw opening (p < 0.05), a remarkable difference. Furthermore, other regions of stress in the TMJ became well distributed after treatment. The maximum stresses were usually in the anterior-posterior direction in all regions. The present data demonstrated the potential benefits of using occlusal splint treatments for providing superior biomechanical behavior to the TMJ.
Acknowledgements
The authors would like to thank the Department of Health, Executive Yuan, Taiwan for financially supporting this research under contract No. MOHW103-TDU-N-211-133001 and No. MOHW103-TD-B-111-01 (Health and welfare surcharge of tobacco products).
7213
References
- Buescher JJ (2007) Temporomandibular Joint Disorders. Am Fam Physician 76: 1477-1482.
- Kalpakci KN, Willard VP, Wong ME, Athanasiou KA (2010) An Interspecies Comparison of the Temporomandibular Joint Disc. J Dent Res 90: 193-198.
- Durham J, Steele JG, Wassell RW, Exley C (2010) Living with uncertainty: temporomandibular disorders. J Dent Res89:827-830.
- Dao TT, Lavigne G(1998) Oral Splints: the Crutches for Temporomandibular Disorders and Bruxism? Crit Rev Oral Biol Med9:345-361.
- Schulte JK, Anderson GC, Sakaguchi RL, DeLong R (1987) Wear resistance of isosit and polymethyl methacrylate occlusal splint material. Dent Mater3:82-84.
- Ye X, Tse ZTH, Tang G, Song G(2014) Effect of electroplastic rolling on deformability, mechanical property and microstructure evolution of Ti–6Al–4V alloy strip. Materials Characterization98:147-161.
- Ye X, Liu T, Ye Y, Wang H, Tang G, Song G(2015) Enhanced grain refinement and microhardness of Ti–Al–V alloy by electropulsing ultrasonic shock. Journal of Alloys and Compounds621:66-70.
- Anderson GC, Schulte JK, Goodkind RJ (1985) Comparative study of two treatment methods for internal derangement of the temporomandibular joint. J Prosthet Dent53:392-397.
- Haketa T, Kino K, Sugisaki M, Takaoka M, Ohta T (2010) Randomized Clinical Trial of Treatment for TMJ Disc Displacement. J Dent Res89:1259-1263.
- Conti PC, dos Santos CN, Kogawa EM, de Castro Ferreira Conti AC, de Araujo Cdos R (2006) Conti ACdCF, de Araujo CdRP. The treatment of painful temporomandibular joint clicking with oral splints. J Am Dent Assoc137:1108-1114.
- Conti PC, Miranda JE, Conti AC, Pegoraro LF, Araújo Cdos R (2005) Partial time use of anterior repositioning splints in the management of TMJ pain and dysfunction: a one-year controlled study. J Appl Oral Sci13:345-350.
- Stiesch-Scholz M, Kempert J, Wolter S, Tschernitschek H, Rossbach A (2005) Comparative prospective study on splint therapy of anterior disc displacement without reduction. J Oral Rehabil32:474-479.
- Morra EA, Greenwald AS (2005) Polymer Insert Stress in Total Knee Designs During High-Flexion Activities: A Finite Element Study. J Bone Joint Surg Am 87:120-124.
- Goel VK, Panjabi MM, Patwardhan AG, Dooris AP, Serhan H (2006) Test Protocols for Evaluation of Spinal Implants. J Bone Joint Surg Am88:103-109.
- Poggie RA, Turgeon TR, Coutts RD (2007) Failure Analysis of a Ceramic Bearing Acetabular Component. J Bone Joint Surg Am89:367-375.
- Beek M, Koolstra JH, Van Ruijven LJ, Van Eijden TMGJ (2001) Three-dimensional Finite Element Analysis of the Cartilaginous Structures in the Human Temporomandibular Joint. J Dent Res 80:1913-1918.
- Koolstra JH, van Eijden TMGJ (2007) Consequences of Viscoelastic Behavior in the Human Temporomandibular Joint Disc. J Dent Res 86:1198-1202.
- Pullinger AG, Baldioceda F, Bibb CA (1990) Relationship of TMJ Articular Soft Tissue to Underlying Bone in Young Adult Condyles. J Dent Res 69:1512-1518.
- Tanaka E, del Pozo R, Tanaka M, Asai D, Hirose M, et al. (2004) Three-dimensional finite element analysis of human temporomandibular joint with and without disc displacement during jaw opening. Med Eng Phys 26:503-511.
- Donzelli PS, Gallo LM, Spilker RL, Palla S (2004) Biphasic finite element simulation of the TMJ disc from in vivo kinematic and geometric measurements. J Biomech 37:1787-1791.
- Tanaka E, Tanne K, Sakuda M (1994) A three-dimensional finite element model of the mandible including the TMJ and its application to stress analysis in the TMJ during clenching. Med Eng Phys 16:316-322.
- Hu K, Radhakrishnan P, Patel RV, Mao JJ (2001) Regional structural and viscoelastic properties of fibrocartilage upon dynamic nanoindentation of the articular condyle. J Struct Biol 136:46-52.
- Kashi A, Chowdhury AR, Saha S (2010) Finite element analysis of a TMJ implant. J Dent Res 89:241-245.
- Weijs A, Hillen B (1984) Relationship between the physiological cross-section of the human jaw muscles and their cross-sectional area in computer tomograms. Acta Anat (Basel) 118:129-138.
- Okeson JP (1988) Long-term treatment of disk-interference disorders of the temporomandibular joint with anterior repositioning occlusal splints. J Prosthet Dent 60:611-616.
- Scapino RP, Canham PB, Finlay HM, Mills DK (1996) The behaviour of collagen fibres in stress relaxation and stress distribution in the jawjoint disc of rabbits. Arch Oral Biol 41:1039-1052.
- Kennady MC, Tucker MR, Lester GE, Buckley MJ (1989) Histomorphometric evaluation of stress shielding in mandibular continuity defects treated with rigid fixation plates and bone grafts. Int J Oral Maxillofac Surg 18:170-174.
- Brehnan K, Boyd RL, Laskin J, Gibbs CH, Mahan P (1981) Direct Measurement of Loads at the Temporomandibular Joint in Macaca arctoides. J Dent Res 60:1820-1824.
- Smith RJ (1978) Mandibular biomechanics and temporomandibular joint function in primates. Am J Phys Anthropol 49:341-349.
- Tanaka E, Tanne K, Sakuda M (1994) A three-dimensional finite element model of the mandible including the TMJ and its application to stress analysis in the TMJ during clenching. Med Eng Phys 16:316-322.
- Mao JJ, Rahemtulla F, Scott PG (1998) Proteoglycan Expression in the Rat Temporomandibular Joint in Response to Unilateral Bite Raise. J Dent Res 77:1520-1528.
- Nakai H, Niimi A, Ueda M (1998) The influence of compressive loading on growth of cartilage of the mandibular condyle in vitro. Arch Oral Biol 43:505-515.
- Berkovitz BKB, Robertshaw H (1993) Ultrastructural quantification of collagen in the articular disc of the temporomandibular joint of the rabbit. Arch Oral Biol 38:91-95.
- Hu K, Qiguo R, Fang J, Mao JJ (2003) Effects of condylar fibrocartilage on the biomechanical loading of the human temporomandibular joint in a three-dimensional, nonlinear finite element model. Medical Engineering & Physics 25:107-113.