Simon B N Thompson1,2*
1Clinical Neuropsychology Research Centre, Faculty of Science & Technology, Bournemouth University, Talbot Campus, Poole House (P305), Poole, BH12 5BB, UK
2International Scientific Council for Research, Université Paris X Ouest Nanterre La Défense, 200 avenue République, 92001 Nanterre, Francea
*Corresponding Author:
Simon B N Thompson
Associate Professor, Faculty of Science and Technology
Bournemouth University, Talbot Campus
Poole House (P302), Poole, BH12 5BB, UK
Tel: +441202 961558
E-mail: simont@bournemouth.ac.uk
Citation: Thompson SN. Retinoblastoma: How Advancements in Neurology and Neuroscience Can Help. J Neurol Neurosci. 2016, 6:4. doi: 10.21767/2171-6625.100050
Received Date: December 01, 2015; Accepted Date: December 01; 2015; Published Date: December 14, 2015
Keywords
Artificial eyes; CHECT; Childhood eye cancer; Diagnosis; Neurology; Neuroscience; Prevalence; Prognosis; Retinoblastoma
Editorial
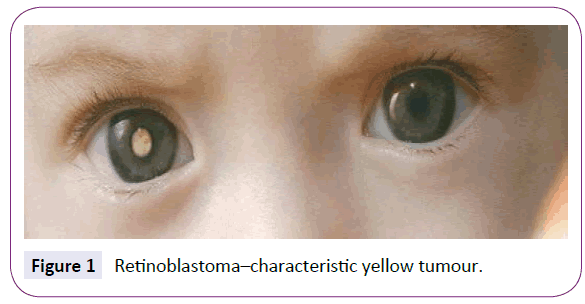
Retinoblastoma is a significant cause of childhood eye cancer world-wide with prognosis dependent upon early diagnosis and treatment but also upon accurate classification of tumours [1]. Unilateral incidence (Figure 1) [2] is normally non-hereditary compared with bilateral incidence.
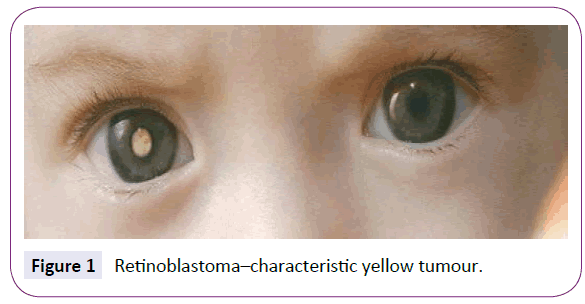
Figure 1: Retinoblastoma–characteristic yellow tumour.
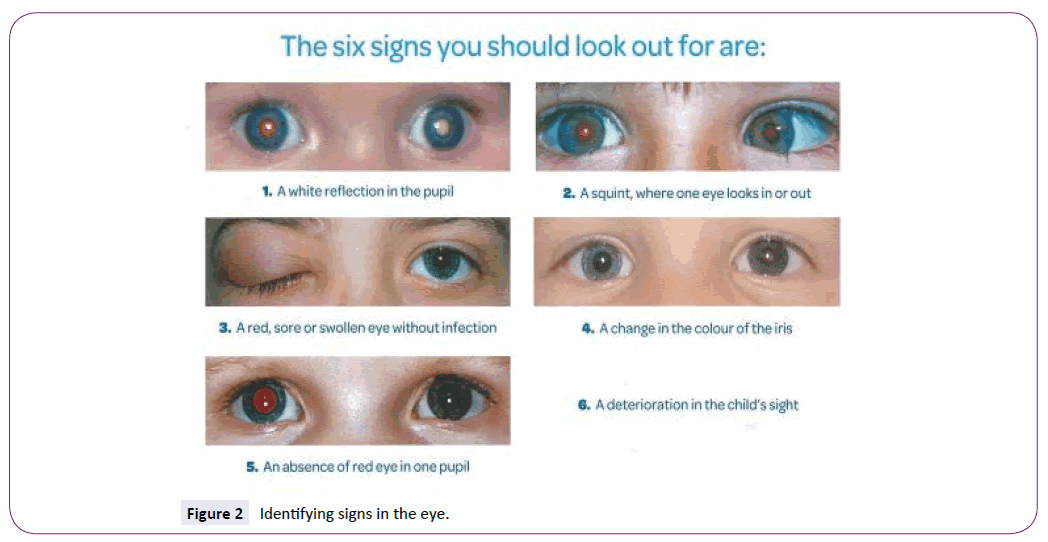
Survivorship is much better for unilateral compared with bilateral and trilateral retinoblastoma but the early signs are important to detect and photography can assist in identifying no return of “red-eye” during flash photography or a distinctive white or yellow appearance of the tumour (Figure 2) [2].
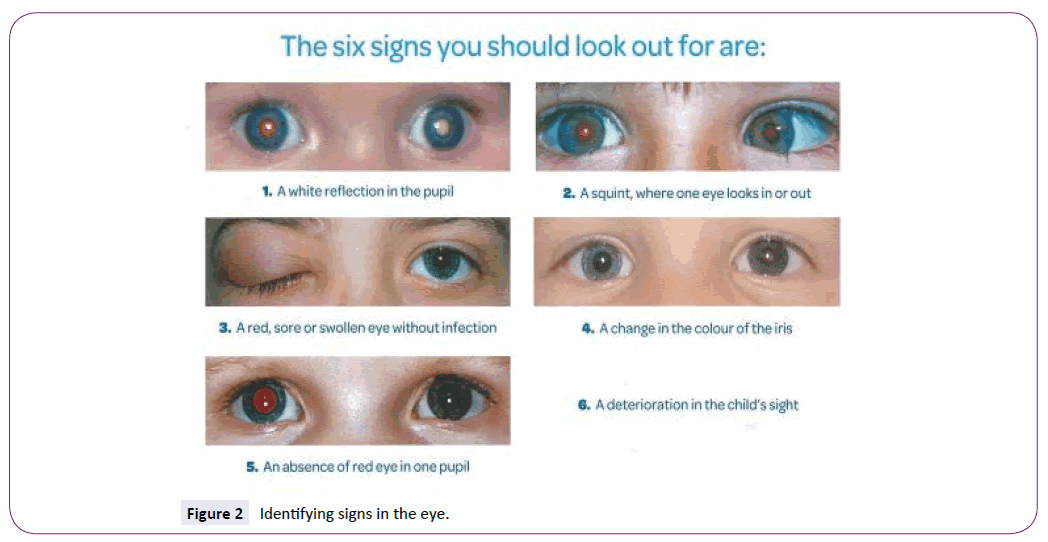
Figure 2: Identifying signs in the eye.
In the UK, it affects between 40-50 children every year [3] and occurs because of errors or mutations to a gene we all possess called the RB1 gene [2]. Five-year survivorship in developed countries averages at 95 per cent compared to 50 per cent worldwide [4,5] and 100 per cent in the UK for the period 2006- 2010 [2]. Delay in diagnosis and access to qualified professionals and resources are the most common explanations for these differences [6].
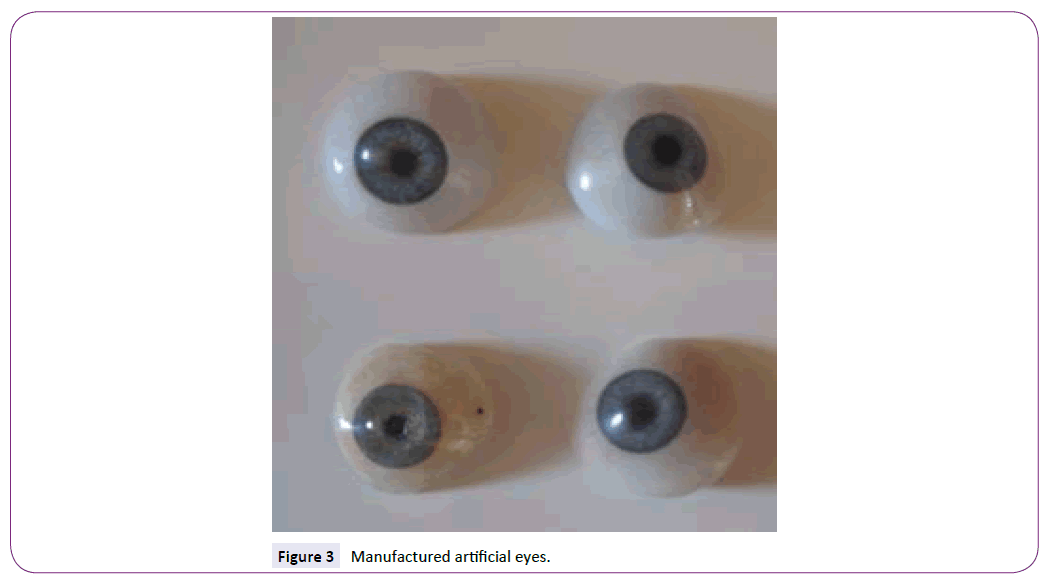
Tragically, it is common for children diagnosed with unilateral retinoblastoma to lose one eye due to the progress of the tumour resulting in enucleation and replacement by an artificial eye (Figure 3). They are often of higher than average intelligence possibly due to their early awareness of mortality and inner strength [7].
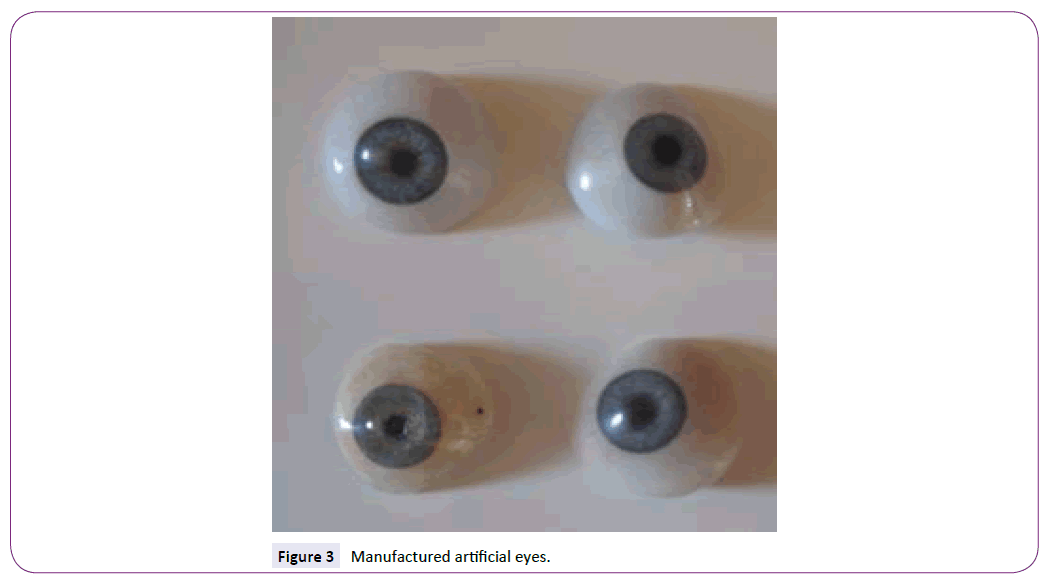
Figure 3: Manufactured artificial eyes.
The manufacture of artificial eyes has advanced considerably with the preferred material in the UK being polymethyl methacrylate (PMMA) which is a rigid plastic that is shatterproof and may be matched to the colour of the iris and covered in a clear coating like the stroma of the cornea.
Often they are hand-painted by a trained occularist. The eye stays in place by the muscles of the upper and lower eyelids but is easily removed for cleaning and regular replacement as the child grows. The fitting procedure is often trial-and-error and dependent upon the skill of the prosthetist, taking an impression of the eye implant with a material similar to dental putty and creating a wax moulding before PMMA manufacture.
Neurological knowledge of the eye and advancement in neuroscience and physics technology provides potential for developing improved fitting procedures. For example, computerassisted LED (Light Emitting Diode) or laser scanning of the implant is possible to collect accurate data about the contours of the implant to inform manufacture of the artificial eye and to ensure better comfort and fitting of the prosthetic.
Research by the author and his team at Bournemouth University, is exploring improved techniques towards more accurate production and fitting of the artificial eye using a soft bonded interface at the back of the prosthetic that provides increased comfort for the wearer and still allows the important growth and stretching of the eyelids in young children.
Informed by the UK’s National Artificial Eye Service and a track record of research in prostheses and cancer [8,9], it is hoped that progress can be made in this field of neurology after decades of exploration by scientists across the world from technology, chemistry, and neurology backgrounds, in search of the ultimate comfortable prosthetic eye.
If this provides our very courageous young children who have this disease with a brighter and more normal prospect in life, then this pursuit is wholly worthwhile.
7893
References
- Thompson SBN, Chinnery HL, Noroozi S, Dyer B, Barratt K (2015) Retinoblastoma: identifying the diagnostic signs for early treatment. Int J Neurorehab 2:1-11.
- Childhood Eye Cancer Trust. About retinoblastoma (2015) Accessed: 02.12.2015. https://www.chect.org.uk/cms/index.php/about-rb
- Children with Cancer UK. Retinoblastoma (2014) Accessed: 02.12.2015. https://www.childrenwithcancer.org.uk/Rb
- Meel R, Radhakrishnan V, Bakhshi S (2012) Current therapy and recent advances in the management of retinoblastoma. Ind J Med Paed Onc 2: 80-88.
- Moll AC, Imhof SM, Cruysberg JRM, Schouten-van Meeteren AYN, Boers M, van Leeuwen FE (2003) Incidence of retinoblastoma in children born after in-vitro fertilization. Lancet 9354:309-310.
- Ramirez-Ortiz MA, Ponce-Castaneda MV, Cabrera-Munoz ML, Medina-Sanson A, Liu X, et al. (2014) Diagnostic delay and sociodemographic predictors of stage at diagnosis and mortality in unilateral and bilateral retinoblastoma. Cancer Epidemiology, Biomarkers & Prevention 5: 784-792.
- Chinnery HL, Thompson SBN (2015) Sensory compensation in children following vision loss after trauma and disease. J Clin Res Ophthal4:049-053.
- Abbey G, Thompson SBN, Hickish T, Heathcote D (2014)A meta-analysis of prevalence rates and moderating factors for cancer-related post-traumatic stress disorder. Psycho-Onc23: 1-12.
- Dyer, B, Noroozi S, Sewell P (2015)Sprinting with an amputation: Some race-based lower-limb step observations. ProsthetOrthotInt 4:300-306.