Keywords
Central venous catheter; Complications; External jugular vein
Introduction
Central venous catheters (CVC) have a high prevalence of use in intensive care units (ICUs); According to several studies, they range from 32% to 80%. [1,2]. In the Clinic La Estancia (Popayan, Cauca) for the year 2008, the Adult Intensive Care Unit reported the use of 300 CVC in a period of 6 months [3].
In patients in critical condition it is imperative to have central venous access. Sometimes it is difficult to cannulate, not only for anatomical reasons, but because multiple pathologies can make it difficult or contraindicate their puncture, which sometimes results in technical problems and associated medical complications.
It is described that the preferred access for CVC placement is the subclavian vein (VSC) [4], and in the second option the right internal jugular vein (VJI). These techniques lead to a higher risk of complications such as pneumothorax, hemothorax, and arterial puncture, which translates into increased mortality [5-9]. In a prospective observational cohort study conducted in Clinical La Estancia (Popayan Cauca), in Adult ICUs for 2008, the association between early mechanical complications and the number of punctures used in CVC placement was documented, finding greater association and statistical significance with 3 or more puncture attempts to present these [3]. The occurrence of complications is greater in patients undergoing hemodialysis and in those with a history of previous central venous cannulations [10-12], which are why some studies suggest that both the SCV and the VJI should be avoided for the placement of the same in this type of patients. To resort when appropriate to the external jugular vein approach (VYE) for central venous cannulation, represents a relegated but alternative approach for patients in which the VJI or VSC vein approach is going to be complicated, besides, it is known that central venous cannulation by VYE leads to a lower rate of complications [13,14].
Likewise, Calvache et al. reported a rate of 4.3% of minor early mechanical complications in CVC placement by VYE, documenting as the only minor complication, the subcutaneous hematoma [3].
The aim of this study is to describe the technique used for the implantation of CVCs by VJE, and to carry out a series of case reports, characterizing the early mechanical complications in intensive care patients, who required central venous catheter placement and without the use of ultrasound guidance.
Materials and Methods
A retrospective analysis was carried out, after approval of the institutional ethics committee; the records of 70 patients admitted to the adult ICU of La Estancia Clinic were reviewed. urban health with a university agreement) from the city of Popayán (Colombia), which, due to some medical condition, required central venous cannulation via the right or left external jugular vein. During the period of 2.9 years comprised between January 2013 to September 2015; choosing only those cases where any of the external jugular veins were visible to any observer, those under 18 years of age and patients with cervical soft tissue deformities and infection were excluded.
For the collection of information, a format was designed that included: the variables: age, sex, diagnosis of admission to the ICU, APACHE II score, indication of use, type of catheter, laterality, use of mechanical ventilation, maneuvers used for the procedure, early complications, procedure time, operative personnel. The data was analyzed by descriptive statistics.
The insertion of the central venous catheters by external jugular route was performed by the medical team of the ICU; physicians specialized in intensive care, residents of anesthesiology and surgery (doctor in training), general practitioners (UCI physicians without specialization, with 3 years of clinical experience), with prior informed consent signed by the patient or, failing that, by his guardian. Both residents and general practitioners placed the catheters, always under the direct supervision of specialized personnel.
In a standardized way, the CVC insertion was done, according to the institutional protocol and using the conventional Seldinger technique. ARROW catheter mono lumens, bilumenes and trilumenes 7Fr × 20 cm, Mahurkar, and Swan Ganz shirts Arrow 8 Fr.
Anatomy of the external jugular vein
The external jugular vein begins at the level of the mandibular angle, just below this or the parotid gland, running down the neck from the mandibular angle to the middle part of the clavicle; Subsequently, the sternocleidomastoid and the subclavian triangle cross obliquely, perforating the deep Apo neurosis to empty into the subclavian vein. It is covered by the cutaneous muscle of the neck, the superficial Apo neurosis and the skin, separated from the sternocleidomastoid by the deep cervical Apo neurosis [15-17].
The size of the vein varies in inverse proportion to the other veins of the neck, sometimes it is double. It has two pairs of valves, one inferior on its entry into the subclavian vein and the other superior, approximately four centimeters above the clavicle. The part between both groups of valves is often dilated and is sometimes called "sinus". The outlet of the external jugular vein in the subclavian at the confluence of Pirogoff, allows access to the central territory from a superficial puncture [18-20].
Technique used
In order to successfully achieve the insertion of the central venous catheters via the external jugular vein, first of all, all the implements required in the procedure were verified: the vital signs were evaluated, optimizing the position of the patient in supine, in such a way that the cervical anatomical structures were exposed more easily, placing in most cases textile elements in the form of an inter-scapular pillow, in the position of Trendelemburg with the head rotated towards the opposite side to that of the cannulation, prior to sustained válsalva maneuver in those awake patients who collaborated with the procedure; in addition to some additional maneuvers such as caudal traction of the ipsilateral upper limb, and / or left or right rotation movements of the neck to facilitate the passage of the guide in some cases, following the trial and error methodology.
After asepsis and antisepsis of the neck, surgical field placement, after visual recognition, in all patients by the operator and posterior palpation of the external jugular vein, infiltration of the underlying subcutaneous cellular tissue was performed, with lidocaine without 2% epinephrine, as cephalic as possible, to prevent the vein from moving, fixing it between the thumb and forefinger of the non-dominant hand, proceeding then to cannulation of the vessel; obtaining thus, the respective venous return. By means of Seldinger's technique, removing the syringe and through the needle, the J-shaped metallic guide was inserted, without forcing its way, to prevent perforations and damage thereof, thus introducing itself in a conventional manner, continuously checking the vital signs, the electrocardiographic tracing and the integrity of the metallic guide discarding possible bends. Occasionally, showing cardiac arrhythmia, as a possible indirect indicator of catheter positioning.
The needle was removed, passing the plastic dilator through the guide with controlled pressure maneuvers, thus avoiding the incision with a scalpel and then penetrating by tissue dissection to allow the subsequent passage of the catheter, entering until the stop (20 cm) in the case of the bilumenes and trilumenes catheter, given its greater anatomical route in this way, until reaching the confluent atrium cavo. After this, the venous return was verified for all its ports, washing with saline solution by these. It was fixed to the adjacent skin with silk 3 - 0 and, finally, it was covered with sterile transparent and impermeable dressing.
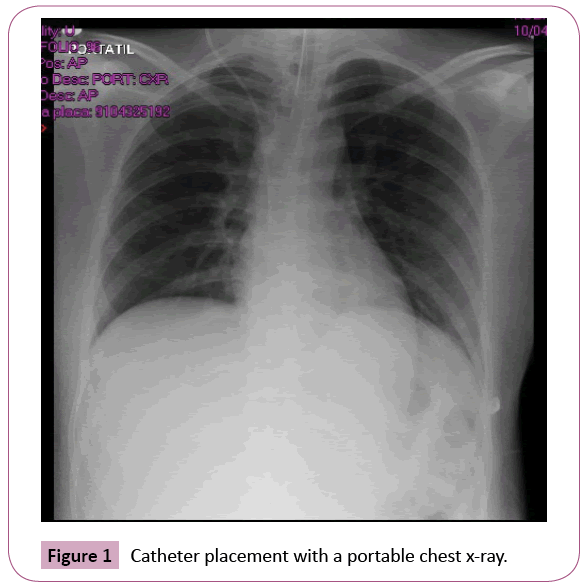
All patients, regardless of the type of catheter, were immediately checked for catheter placement with a portable chest x-ray. In the patients who were undergoing invasive mechanical ventilation, the same procedure was followed without variations in the ventilatory parameters, basically in the PEEP (Figure 1).
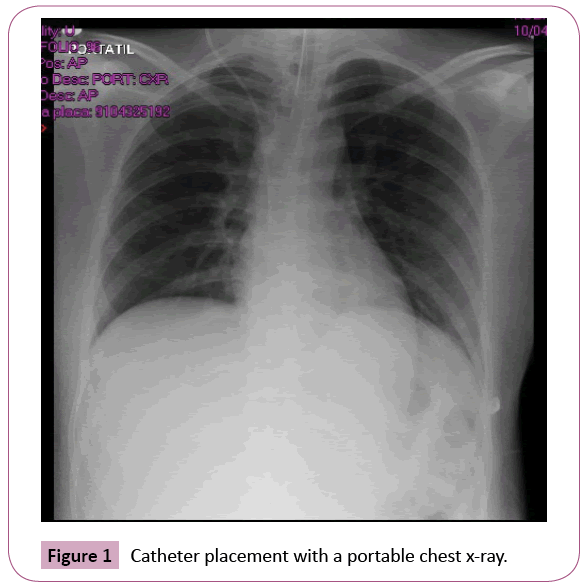
Figure 1: Catheter placement with a portable chest x-ray.
Results
Seventy consecutive patients were collected who required insertion of the CVC in the ICU, of which 63 were successfully performed by VJE (90%). In 7 patients, insertion of the catheter by this technique was not possible. The general characteristics of the patients and the procedure are presented in Table 1.
| Average age |
57-years-old (16-90) |
| Gender |
Five Enino 41 (59.4%) |
| Diagnostics principles |
| Shock |
30 (47.6%) |
| Others |
11 (17.4) |
| Abdominal Pathology |
5 (8) |
| Trastor no Hidroelectrolitos |
4 (6.35%) |
| Pulmonary Pathology |
4 (6.35%) |
| Trauma |
3 (4.76%) |
| Cardiac Conduction Disorder |
3 (4.76%) |
| Kidney Pathology |
2 (3.2%) |
| Metabolic Pathology |
1 (1.58%) |
| Patients in mechanical ventilation |
| Mechanic ventilation |
33 (52.3%) |
| Central venous catheter insertion site |
| Right external jugular vein |
50 (79.3%) |
| Left external jugular vein |
13 (20.7%) |
| Characteristics of the insertion |
| Use of trilumen catheter |
54 (85.7%) |
| Use of catheter swan ganz |
2 (3.2%) |
| Use of mahurkar catheter |
4 (6.34%) |
| Use of pacemaker |
3 (4.76 %) |
| Insersion during day (7 AM-7 PM) |
36 (57.14%) |
| Operator training level |
| Medical specialist / intensivist |
42 (66.6%) |
| General practitioner |
15 (23.8%) |
| Resident doctor in training |
6 (9.6%) |
| an=63 |
Table 1: The general characteristics of the patients and the procedure.
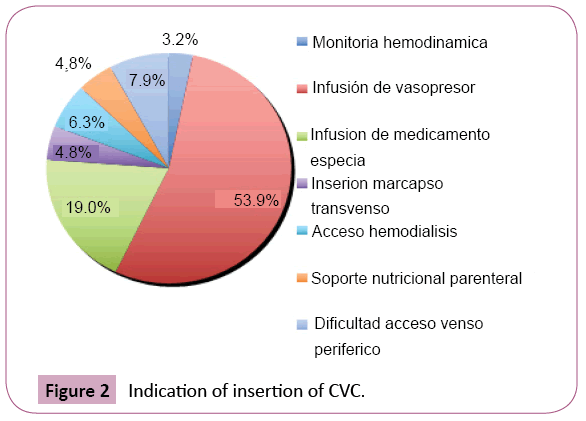
In most patients, the main diagnosis was indiscriminately shock, including all types of this entity (47.6%). The main indication for insertion of the catheter was the requirement for vasopressor support (53.9%) (Figure 2).
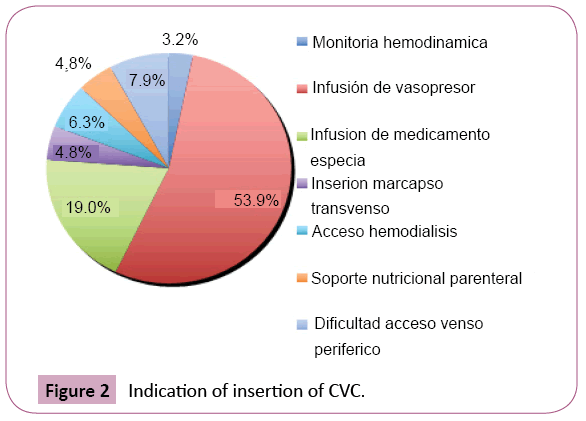
Figure 2: Indication of insertion of CVC.
More than half of the patients required invasive ventilatory support at the time of insertion of the CVC, the most chosen site by the operator was the right side in 79.3% of the patients, the most used catheter was the trilumen in In 85.7% of the cases, 57.1% of the catheters were inserted during the hours of the day. The highest proportion of CVC insertion was performed by the operator with the highest level of training, in this case the critical care specialist.
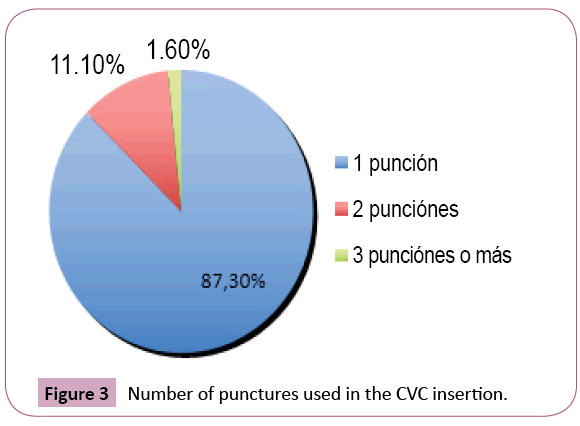
The proportion of catheters inserted successfully on the first attempt was 87.3% (Figure 3).
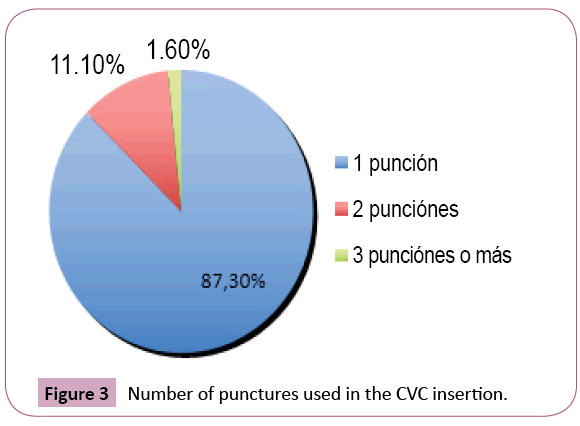
Figure 3: Number of punctures used in the CVC insertion.
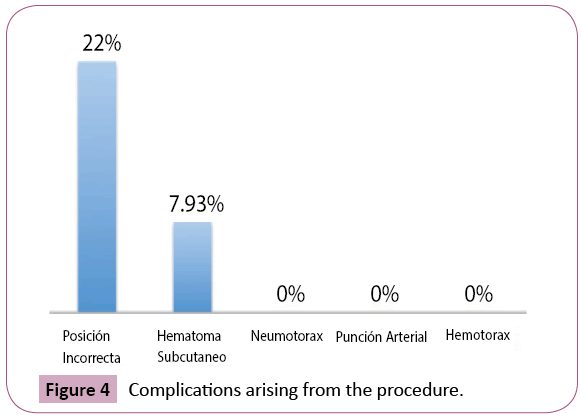
Mechanical complications related to CVC insertion are described in Figure 3. The only complication associated with the procedure was subcutaneous hematoma in 7.93% of the patients, and the incorrect position was observed in 22.2%, in no case were they presented pulmonary complications. It is understood as the correct position the location of the catheter tip in a wide diameter vessel, ideally outside the cardiac cavity, parallel to the axis of the vein to reduce the probability of injury [21] (Figure 4).
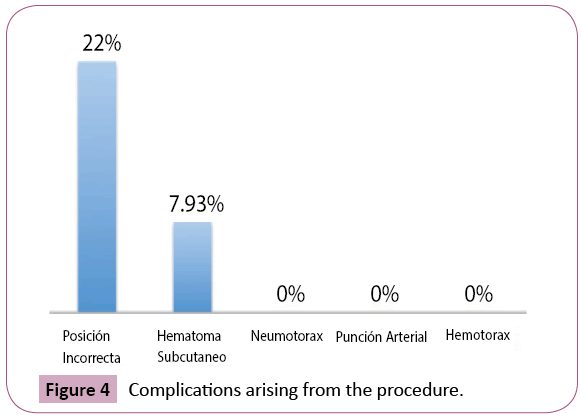
Figure 4: Complications arising from the procedure.
Discussion
Reviewing the medical literature, we found the first reports of CVC placement by VYE towards the 1970s [22] The focus on the use of this technique has not been very popular due to the low success rate reported by some authors [23], mainly attributed to anatomical considerations that make the passage of the CVC difficult in this way.
The technique is well described in the literature consulted, there are few available data and studies in which the potential use of VYE for the insertion of CVC in critically ill patients is addressed and described.
The benefits inherent in the use of VYE include its large size, which allows greater capacity to accommodate large or multilumen catheters more easily than many peripheral insertion sites; the superficial location facilitates the ability to visualize the VYE without image technology. The above are properties that make this technique attractive; in addition, it has a very low rate of complications derived from the insertion of the CVC.
Although certain studies on this relegated technique are emerging today, such as that written by Kazuya Kato et al. [24] prospective cohort study, which describes the insertion of CVCs by VYE, prior preoperative estimation of the orientation Detailed anatomical study of the cervical venous plexus, using computed tomography venography, our technique does not involve performing any previous imaging studies to achieve the corresponding anatomical description of the vein, this is due to the fact that the external jugular vein in all patients selected for the insertion of the CVC in this way was always visible to the observer.
There is also a prospective randomized cohort study conducted by Calin I. Miter et al. [25] in which two groups of patients were compared, to whom the CVC was inserted by VJE, without the use of ultrasound guidance and another with the use of the same, documenting a success rate of CVC insertion of 42% and 27% for each of the groups; With our technique we obtained success in the insertion of the CVC in 90% of the cases, this attributed to the condition that the objective of choosing and performing the procedure was met only in those patients, where the previous macroscopic visualization was possible of VJE, aspect not taken into account in the previous study. Regarding the complications reported by the previous ones, the only one was the formation of subcutaneous hematoma at the puncture site in 36.6% and 43.3% respectively, while in our report it was also the only one observed, and it was presented in 7.93% of the cases.
The attractiveness of our approach, used in the implementation of the CVC by VYE, as previously mentioned, does not require any imaging study for the insertion of the same, except for a single requirement, vein observation by the operator, in addition to the maneuvers described in our technique, it is possible to overcome the angulation between the VYE and the subclavian vein, which often makes it difficult to pass the CVC.
Conclusion
This study obtains its expression with the preliminary work that was reported in 2008, carried out in the health center, where a technique was applied to a group of patients with a minimum of complications; it is interesting the duly planned execution of a study with a different methodology that allows the comparative statistical analysis that could yield other results.
In conclusion, this is a technique, with minimal complications, to be considered in critically ill patients, to whom the external jugular vein is visible by the observer, in which the use of more invasive traditional techniques could generate greater complications.
Conflict of Interests
None of the authors declares to have a conflict of interest.
23250
References
- National Nosocomial Infections Surveillance (2002) NNIS: System Report. Am J Infect Control 30: 458-475.
- Vincent JL, Bihari DJ (1995) The prevalence of nosoco-mial infection in intensive care units in Europe. Results of the European prevalence of infection in intensive care (EPIC) study. J Am Med Assoc 274(8): 639-644.
- Calvache JA, Rodrguez MV, Trochez A, Klimek M, Stolker RJ, et al. (2014) Incidence of mechanical complications of central venous catheterization using landmark technique: Do not try more than 3 times. J Intensive Care Med 31(6): 397-402
- Mgarbane B, Mira JP, Kalfon P (2015) Intravascular complications of central venous catheterization by insertion site. N. Engl. J. Med 373(13): 1220-1229.
- Bermard RW (1971) Subclavian vein catheterizations: A prospective study. I. Non-infectious complications. Ann Surg 173: 184-190.
- Mansfield PF, Hohn DC, Forange BD, Gregurich MA (1994) Complications and failures of subclavian-vein catheterization. N Engl J Med 29: 1735-1738.
- Trerotola SO (1997) You are asked to place a dialysis access catheter in a patient. What is your preferred access site, and why?. J Vasc Interv Radiol 8: 75-76.
- Macdonald S, Watt AJB, McNally D, Edwards RD (2000) Comparison of technical success and outcome of tunneled cath- eters inserted via the jugular and subclavian approach. J Vasc Interv Radiol 11: 225-231.
- Schillinger F, Schillinger D, Montagnac R (1991) Post catheterization vein stenosis in haemodialysis: comparative angiographic study of 50 subclavian and 50 internal jugular access. Nephrol Dial Transplant 6: 722-724.
- Beaulieu Y (2005) Bedside ultrasonography in the ICU. Chest 128: 1766-1781.
- Ked DF (2007) Ultrasound guided internal jugular access. Chest 132: 302-309.
- Bond DM, Champion LK (1989) Real-time ultrasound imaging aids jugular venipuncture. Anesth Analg 68: 700-701.
- Segura-Vasi AM, Suelto MD (1999) External jugular vein cannulation for central venous access. Anesth Analg 88: 692-693.
- Byth PL (1985) Evaluation of the technique of central venous catheterisation via the external jugular vein using the J-wire. Anaesthesia and intensive care 13: 131-133.
- Caballero L A (2002) Cateterizacin venosa profunda. En: Terapia intensiva. La Habana Editor Ciencias Mdicas 31-60.
- Vorger G (2002) Cateter intervenosos e infecciones. MedClin 82: 846-848.
- Blitt CD (1974) Central venous catheterization via the external jugular vein. A technique employing the J. Wire. JAMA 229: 817-818.
- Prez Almenares D, Parte Prez L, Prez P©rez I (1995) Cateterismo de la vena yugular externa en el cardipata. Rev Cuba Pediatr 67(2): 103-106.
- Blitt CD, Carlson GL (1982) Wire versus straight wire for central venous system cannulations via the external jugular vein. Anesth Analg 61: 536-537.
- Richet H, Hubert B, Nitemberg G, Andreamont A, Bou-Hoy A, et al. (1990) Prospective multicenter study of vascular catheter related complications and risk factors for positive central catheter culture in intensive care unit patients. J Clin Microbiol 28: 2520-2525.
- Nawa WS (2001) Unconventional venous access. Teach vas interv radiol 5: 114-120.
- Malatinsky J, Kadlict P, Majek MSM (1976) Misplacement and loop formation of central venous catheterst. Acta Anaesth scand 20: 237-247.
- Kato K, Taniguchi M, Iwasaki Y, Sasahara K, Nagase A, et al. (2014) Computed Tomography (CT) venography using a multidetector CT prior to the percutaneous external jugular vein approach for an implantable venous-access port. Ann Surg Oncol 21: 1391-1397.
- Mitre CI, Golea A, Acalovschi I, Mocan T, Caea AM (2010) Ultrasound-guided external jugular vein cannulation for central venous access by inexperienced trainees. European Journal of Anaesthesiology 27: 300-303.