Keywords
Mental practice; Mental imagery; Motor imagery; Stroke; Cerebrovascular accident; Hand function; Functional training; Mental practice; Hemiplegic; Dexterity; Arm; Upper extremity
Introduction
Up to 85% stroke survivors experience hemi paresis resulting in impaired movement of the arm, and hand as reported by Nakayama et al. Loss of arm function adversely affects quality of life and functional motor recovery in affected upper extremity.
Sensorimotor deficits in the upper limb, such as weakness, decreased speed of movement, decreased angular excursion and impaired temporal coordination of the joints impaired upper-limb and trunk coordination.
Treatment interventions such as materials-based occupations constraint-induced movement therapy modified constraint-induced movement therapy and task-related or task-specific training are common training methods for remediating impairments and restoring function in the upper limb.
For the improvement of upper and lower functions, physical therapy provides training for functional improvement and fine motor. For most patients such rehabilitation training has many constraints of time, place and expense, accordingly in recent studies, clinical methods such as mental practice for improvement of the upper and lower functions have been suggested.
Mental practice is a training method during which a person cognitively rehearses a physical skill using motor imagery in the absence of overt, physical movements for the purpose of enhancing motor skill performance. For example, a review of the duration of mental movements found temporal equivalence for reaching; grasping; writing; and cyclical activities, such as walking and running.
Evidence for the idea that motor imagery training could enhance the recovery of hand function comes from several lines of research: the sports literature; neurophysiologic evidence; health psychology research; as well as preliminary findings using motor imagery techniques in stroke patients.
Much interest has been raised by the potential of Motor Practice of Motor task, also called “Motor Imagery” as a neuro rehabilitation technique to enhance Motor Recovery following Stroke.
Mental Practice is a training method during which a person cognitively rehearsals a physical skill using Motor Imagery in the absence of Physical movements for the purpose of enhancing Motor skill performance.
The merits of this intervention are that the patient concentration and motivation can be enhanced without regard to time and place and the training is possible without expensive equipment.
Researchers have speculated about its utility in neurorehabilitation. In fact, several review articles examining the impact of mental practice have been published. Two reviews examined stroke outcomes in general and did not limit their review to upper-extremity–focused outcomes. Both articles included studies that were published in 2005 or earlier.
Previous reviews, however, did not attempt to rate the studies reviewed in terms of the level of evidence. Thus, in this review, we determined whether mental practice is an effective intervention strategy to remediate impairments and improve upper-limb function after stroke by examining and rating the current evidence.
Methods
Sources
Independent searches of electronic databases including Medline, PubMed, the Cochrane Database, from 1995 to 2016 was performed. Search terms included mental practice, mental imagery, motor imagery, stroke, cerebrovascular accident, Hand function, functional training, mental practice, hemiplegic, dexterity, arm, and upper extremity. The search was limited to journals published in English.
Study selection
Published and completed studies were included in this review if they met the following criteria: The participant’s primary diagnosis was a stroke, mental practice was used as part of the intervention plan either in isolation or in conjunction with other therapies, and mental practice was used to reduce upper-extremity impairment or improve upperextremity function.
Inclusion criteria
• Articles published in time period between 1995 to 2016.
• All levels of evidence were considered for this review.
• Primary diagnosis – stroke.
• Mental Practice – either as sole treatment or in combination.
Data extraction
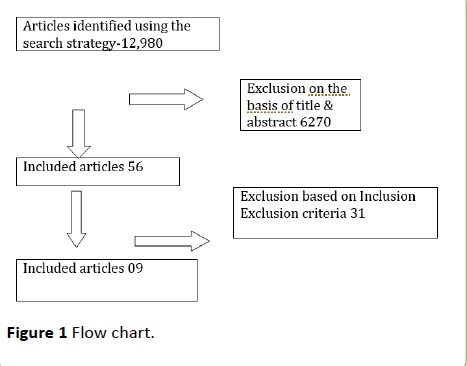
Study objectives, level of evidence and design, description of participants (e.g., age, time since stroke, lesion sites), intervention description, outcome measures, and dimension of the outcome measures based on the International Classification of Functioning, Disability and Health (World Health Organization, 2001) For this review, we used the following levels of evidence: Level I (systematic reviews, metaanalyses, RCTs), Level II (nonrandomized controlled trials, case control trials), Level III (pretest–posttest designs, crosssectional designs), Level IV (single-subject designs, case series), and Level V (case reports, narrative literature reviews). Additionally, assessed the quality of the included studies using the Critical Review Form – Quantitative studies (Figure 1).
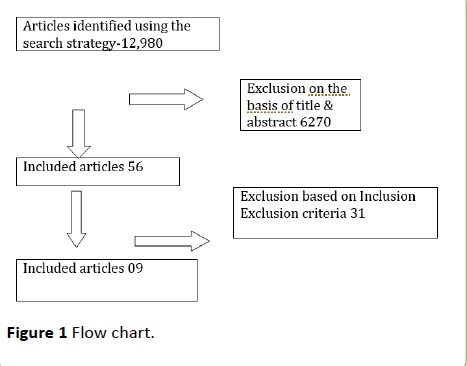
Figure 1 Flow chart.
Results
Eleven articles were originally located using the previously mentioned key words and study selection criteria. Of those articles, 2 were excluded because they were not completed studies Therefore, a total of nine articles were reviewed and classified according to the criteria described earlier. The results are summarized in Table 1 [1-5].
| Author |
Participants |
Duration |
Outcome measure |
Results |
Conclusion |
Evidence |
Juhyung Park
et al. [1] |
29 participants, hemiplegia for over 6 months, |
10 min per session, once a day, 5 times a week, for 2 weeks |
ARAT,
FMA,
Modified Bathel Index |
The mental practice showed significant improvement p<0.05 in ARAT, MBI, and FMA-UE of the affected side. |
MP intervention is effective at improving stroke pt’s UE function and daily activity performance |
Level 1 |
| Hua Liu et al. [2] |
20 participants, first stroke with neurological deficit in the affected UE ( nadir hand function level beyond brunnstrom 3rd) |
Once a day for 45 min, 5 days a week for 4 weeks |
ARAT |
ARAT score increased significant difference in the ARAT. P=0.04 |
Combining MP with may be a more effective treatment strategy for improvement in Hand function |
Level 1 |
| Annick A et al. [3] |
160 participants, First stroke, were 2 to 6 weeks after stroke at inclusion, were clinically diagnosed with a central paresis of the arm-hand |
3 times per day for 6 weeks |
Fug- Meyer Test, Wolf Motor Function Test, Barthel Index, Frenchay activities Index |
No significant difference in training effects between groups was demonstrated. Training effects were demonstrated after MP training in pts with sub-acute stroke. |
The results of this study do not corroborate the hypothesis that the use of MP in addition to therapy as usual in pts with sub-acute stroke has an additional effect over Neuro developmental therapy. |
Level 1 |
| Magdalena et al. [4] |
Participants- 41, a history of stroke 1-6 months, ARAT score of between 3 and 51, no severe cognitive impairment |
45min supervised sessions 3 times a week for 4 weeks, independent session twice a week |
ARAT |
P=0.77 MP with motor imagery does not enhance motor recovery in pts early post stroke |
Only pts with preserved motor ability stand to benefit from MP, pts with limited cognitive resources are also unlikely to gain from this treatment |
Level 1 |
| Stephen J et al. |
30 Participants, stroke experienced>12 months prior to study enrollment, a score >70 on the MMSE, Only have experiences one Stroke |
60 min sessions 3days/week for 10 weeks |
ARAT, FMA |
Subjects administered MP exhibited markedly larger score changes |
60min of MP appears to most significantly reduce affected arm impairment |
Level 1 |
| Katharina et al. [5] |
17 Participants, first ever stroke, only one brain lesion in MRI, severe hemiparesis with complete paralysis of the affected arm at the acute stage of stroke |
30min 5days/week for 4 weeks |
Jebsen-test,
Barthel Index |
Mental training resulted in an increase in the peak force of the pinch grip and generalized in a better functionality of the upper extremity. |
The control of finger movements benefits from mental training of sequential finger movements . |
Level 1 |
| Stephen J et al. |
32 Participants, history of no more than one stroke, a score >69 on the MMSE, age >18 and <80 years |
30min 2 days/week for 6 weeks. |
ARAT,
FMA |
Subjects receiving MP showed significant reductions in affected hand impairment and significant increases in daily arm function. P= <0.0001 |
Supports the efficacy of programs incorporating MP for rehabilitating affected arm motor function. These changes are clinically significant. |
Level 1 |
| Magdalena et al. [4] |
135 Participants, a history of stroke one to six months prior to participation, ARAT score of between 3 and 51, no severe aphasia, MMSE score of 7 or more. |
45min daily/week for 5 weeks |
ARAT,
Grip strength (dynamometer), Barthel Index |
Patients engaging in mental rehearsal of variety of UL movements showed enhanced motor recovery and improvement in hand function. |
The idea of enhancing motor recovery through the use of MP rehab techniques is important with potential implications for clinical practice. |
Level 1 |
| Stephen J et al. |
11 Participants, 10* or more of active flexion in the more affected wrist, MMSE score 70 or higher, MAS score of 3 or lower, score of 4 or lower on VAS |
30min 2days/week for 6 weeks |
Motor Activity Log, ARAT |
ARAT scores revealed significantly P= .004 greater changes in the MP’s group scores |
Participation in an MP protocol may increase a stroke patient’s use of his/her more affected limb. |
Level 1 |
Table 1 Summary of evidence on use of mental practice to improve hand function in stroke survivors.
Discussion
The results of the studies reviewed were positive indicating the potential benefits of mental practice in the recovery of upper limb motor performance following a stroke, however, the limited number of studies and small sample sizes must be noted when considering the strength of results.
Studies differed with respect to patient characteristics, intervention protocols and outcome measures. It remains unclear what the optimal dosing is regarding the amount of Mental Practice or the ratio of Mental to Physical practice needed to obtain a positive effect. Most studies have shown that mental practice reduces impairments and improves functional recovery of the upper limb. Future research should explore the dosage, factors affecting the use of Mental Practice, effects of Mental Therapy alone without in combination with other interventions.
Several studies have shown support for the notion that mental practice can reduce upper-limb impairments and increase functional use of the affected limb [5,6], return to the occupational performance after Mental Practice is yet to be found.
According to Stevens, a motor representation contains both the kinesthetic and the biomechanical constraints associated with the action, as well as the spatial coordinates of the action. Therefore, the visual imagery modality (i.e., “seeing” your hand move) may be used to represent the spatial coordinates (i.e., distance and location), and the kinesthetic imagery modality (i.e., “feeling” your hand move) may be used to represent the biomechanical constraints.
Moreover, it would be of interest to determine whether one type of instruction is more beneficial to facilitating imagery than another and to what extent imagery training before engagement in mental practice is beneficial [7] (Table 2).
| Strength |
Weakness |
| Study design of the articles was randomized controlled trial. |
Different evaluation methods were used in the various articles. |
| The similarity and differences between the groups were mentioned clearly. |
Sample size was small in three articles. |
| Attention Bias and Measurement Bias was present in two articles. |
| Intervention was described in detail. |
| Contamination of treatment was avoided. |
Might be the patients did not adhere to the intervention. |
| Results were reported in terms of statistical significance. |
| The length of the interventions and number of practice hours varied. |
Table 2 Strengths and weaknesses.
Although the benefits of mental practice in post stroke rehabilitation appear promising, general conclusions are difficult to make. Future research should investigate whether mental practice promotes return to occupational performance as perceived by the participants engaged in treatment.
Conclusion
The evidence presented in this review indicates the potential mental practice has for the improvement of upper extremity function in stroke survivors, but general guidelines inclusive of practice hours are difficult to conclude at this stage, future research should investigate the optimize duration and sole benefits of mental practice to improve hand function in stroke survivors.
Conflict of Interest
None.
Source of Funding
Self-funding.
Ethical Clearance
Ethical clearance was obtained from the JSS College of Physiotherapy, Mysore.
Acknowledgement
The author would like to thank Dr Kavitha Raja for her guidance and assistance regarding this study.
18614
References
- Park J, Lee N, Cho M, Kim D, Yang Y (2015) Effects of mental practice on stroke patients upper extremity function and daily activity performance. Journal of Physiotherapy Science 27: 1075-1077.
- Liu H, Song LP, Zhang T (2014) Mental practice combined with physical practice to enhance hand recovery in stroke patients. Behavioural Neurology 1-9.
- Timmermans A, Verbunt J, Woerden R, Monnekens M, Pernot D, et al. (2013) Effect of mental practice on the improvement of function and daily activity performance of the upper extremity in patients with sub-acute stroke- A randomized clinical trial. JAMDA 14: 204-212.
- Letswaart M, Johnston M, Dijkerman C, Joice S, Scott C, et al. (2011) Mental practice with motor imagery in stroke recovery- A randomized controlled trial of efficacy. Brain - A Journal of Neurology 134: 1373-1386.
- Page JS, Levin P, Leonard A (2007) Mental practice in chronic stroke - Result of randomized placebo controlled trial. Stroke 38: 1293-1297.
- Page JS, Dunning K, Hermann V, Leonard A, Leving P (2011) Longer versus shorter mental practice sessions for affected upper extremity movement after stroke- A randomized controlled trial. Clinical Rehabilitation 25: 627-637.
- Hall C, Pongrac J (1983) Movement Imagery Questionnaire. London, ON: University of Western Ontario.