Soubhagya Ranjan Tripathy1*, Sanjib Mishra1, Anup kumar Mahapatra2, Rabi Narayan Panda3, Harekrishna Majhi4 and Jagmohan Mishra5
1Department of Neurosurgery, SCB Medical College Hospital, Cuttack, Odisha, India
2Department of Neurosurgery, MKCG Medical College Hospital, Berhampur, Odisha, India
3Department of Neurosurgery, VSS Medical College Hospital, Burla, Odisha, India
4Department of General Surgery, VSS Medical College Hospital, Burla, Odisha, India
5Department of General Surgery, SCB Medical College Hospital, Cuttack, Odisha, India
*Corresponding Author:
Soubhagya Ranjan Tripathy
Department of Neurosurgery
SCB Medical College Hospital
Cuttack, Odisha, India
Tel: +91-9861008487
E-mail: soubhagya.tripathy@gmail.com
Citation: Tripathy SR, Mishra S, et al. Role of Single Burr-Hole and Saline Lavage in Chronic Subdural Hematoma (CSDH): The Need of another Clinical Prospective Epidemiological Study. J Neurol Neurosci. 2016, 6:4. doi: 10.21767/2171-6625.100051
Received: November 11, 2015; Accepted Date: December 15; 2015, Published Date: December 21, 2015
Keywords
Chronic subdural hematoma (CSDH); Lavage; Single burrhole; Single burr-hole and saline lavage
Introduction
One of the most gratifying experiences in neurosurgery, both for the patient and for the surgeon, is the restoration to full health of the patient by the simple surgical procedure of evacuating a chronic subdural hematoma (CSDH).
Majority of symptomatic patients need surgical evacuation. The evacuation procedures range from a simple burr-hole drainage to more complex craniotomy with membranectomy. Multiple burr-hole drainage was amongst the most favoured technique employed, at our institution. The present prospective study analyzed the results of “single burr-hole drainage with normal saline lavage”.
The aim of this study is to find out the incidence, risk factors and varieties of presentations and management with “single burr hole and drainage with saline lavage”, and complications.
Materials and Methods
The prospective study was conducted on all the patients admitted to the department of neurosurgery, Veer Surendra Sai Medical College, Burla during the period October 2010 to October 2012. All cases of chronic subdural hematoma admitted to this hospital, both unilateral and bilateral, having clinical and radiological evidence are included in this study. Post operatively patients are followed up to three months. The data were collected from the “patient proforma”, case sheets, operation theatre records and hospital discharge summaries.
Diagnosis was confirmed by cranial computed tomography scan. All the patients were operated under general anesthesia.
Inclusion criteria
CSDH at any site-frontal, parietal, hemispheric; any cause traumatic, associated with alcohol, associated with anticoagulants; patients of any preoperative GCS (Glasgow coma score), any pupillary size; mass effect on CT (computerized tomography scan) brain.
Exclusion criteria
second surgery after Extradural Hematoma (EDH) evacuation or after giving medium pressure ventriculo peritoneal (MPVP) shunt, CSDH not large enough to be operated and cases lost to follow up after surgery.
Statistical Analysis
Student t test
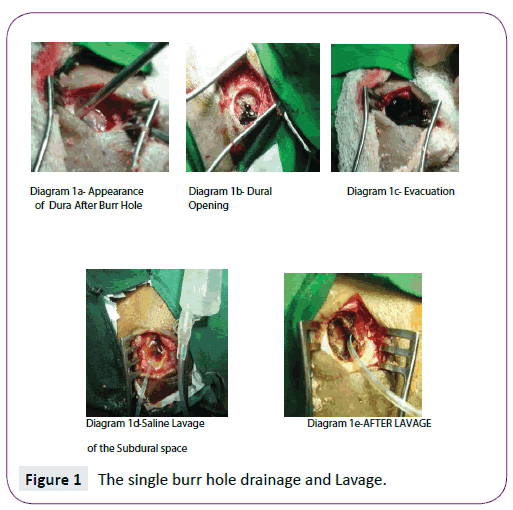
After admission routine investigations along with coagulation tests such as-BT (Bleeding time), CT (Clotting time), PTT (Plasma thromboplastin time) and INR (International normalized ration); Liver function tests (LFT) -for alcoholics, has been done and posted for surgery. The hematoma was drained through a single burr-hole placed at posterior frontal/ parietal region. Irrigation of the subdural space was done (Figure 1) with warm normal saline using a20 ml syringe. Amount of normal saline needed for irrigation ranged between1 to 2 L. On completion of the irrigation the head was elevated to 30 degree and the subdural space was slowly filled with saline so as to eliminate air to maximum possible extent before securing a single layered skin closure. A stamp sized gelfoam piece was used to plug the burr-hole opening before closure. Postoperatively the patient was adequately hydrated, allowed ambulation after 24 h and discharged after 48 h. Use of anticonvulsants was restricted only to those with a previous seizure history.
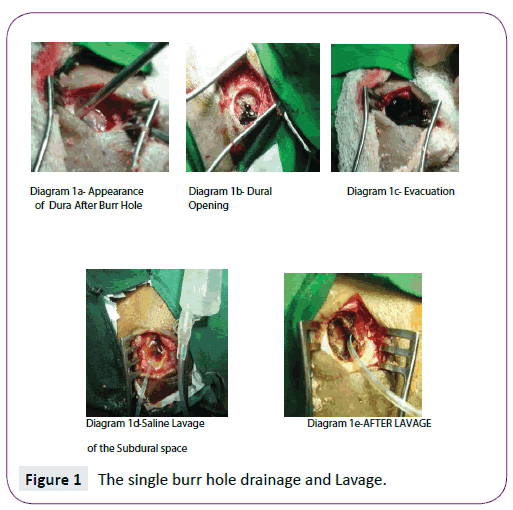
Figure 1: The single burr hole drainage and Lavage.
Clinical status at admission and outcome was assessed in terms of the Glasgow outcome score scale (GOS) at three weeks following discharge.
Proforma
The proforma is as depicted in Table 1.
| SN |
Name/ Age/Sex |
H/O Trauma |
Anticoa
Gulants/
Antiplates |
Alcohol |
GCS |
Clinical
Features:- |
Side/
Site |
Midline
Shift:- |
CT:-CSDH Thickness
(mm) |
Recovery |
Complications:- |
| |
PupilSigns/
Headache/
Seizure/
Hemiparesis |
|
>5mm/
<5mm |
|
Complete/
Partial/
Death |
(TP)/(SDE)/ (ICH)/(C/L) Hematoma and Recurrence |
[TP: Tension Pneumocephalus; SDE: Sub Dural Empyema; ICH: Intra Cranial Hemorrhage, C/L: Contralateral.]
Table 1: Proforma
Results
Total number of traumatic brain injury cases admitted during the study period is 687. Out of this 36 cases are with clinical and radiological features of CSDH. Thus the incidence in our study is 5.24%.
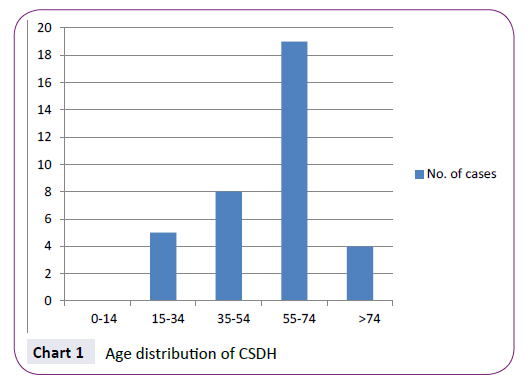
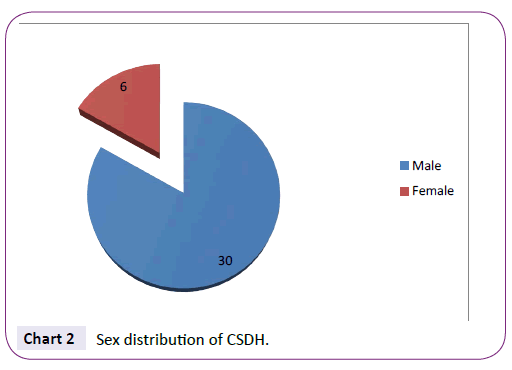
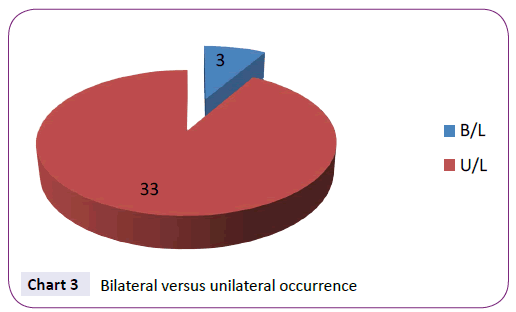
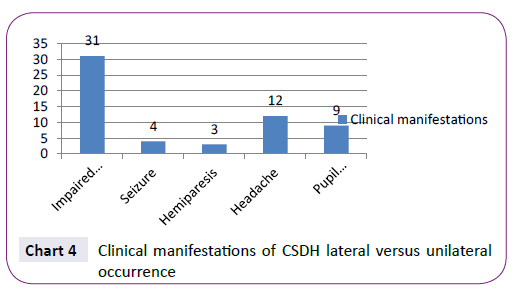
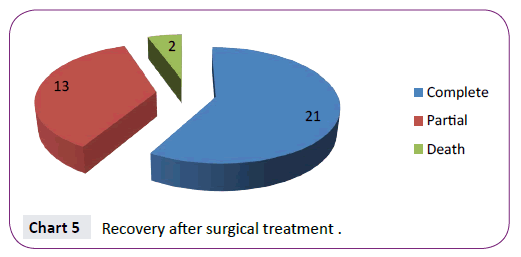
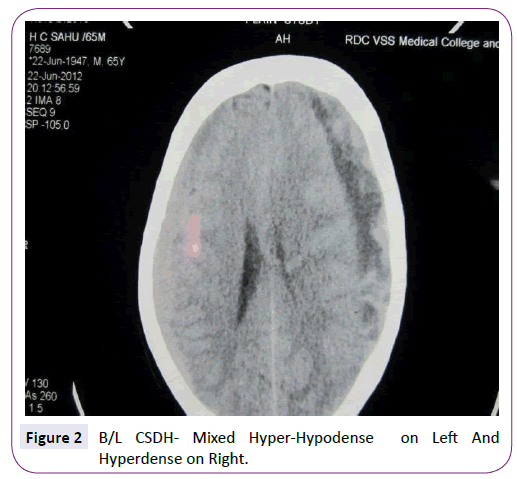
52.8% belong to 55-75 yr age group [1,2] (Chart 1) with male predominance [3] (5:1) (Chart 2), trivial trauma m/c mode (83.3%). Chronic anticoagulant/ antiplatelet (Aspirin) [2,4] uses are responsible as a risk factor in 19.4% cases. Alcohol abuse present in 25%, 91.7% cases were unilateral (Chart 3), 44.4% were hemispheric. Altered consciousness (86.1%) followed by headache (33.3%) are m/c presenting s/s (Chart 4). Recurrence was seen in 5.5% (Chart 5). Complete recovery in 58.3% on postop follow up with another 36.1% showing partial recovery, immediate postop follow up 80% were hypodense on CT. Mixed density denotes acute bleed into CSDH. Visual disturbances in CSDH patients are mostly due to raised intra cranial pressure and the resulting papilledema. But CSDH patients with altered consciousness fail to give details of loss of their visual acuity. Complete recovery was seen in 58.3% of cases on postoperative follow up; with 36.1% showing partial recovery post-surgery. 80% CSDH are hypodense on CT scan. Mixed density (Figure 2) implicates acute bleed into a chronic hematoma. Isodense CSDH are the most difficult to diagnose plain CT scan and may need CECT (Contrast enhanced CT scan) or MRI (Magnetic resonance imaging) for it Impaired consciousness [5] was noted in 31 (86.1%) cases, seizures in 4 (11.1%), hemiparesis [5] in 3 (8.3%), features of raised intra cranial pressure i.e. headache in 12 (33.3%) and pupillary abnormality [5] in 9 (25%) of cases. Maximum patients of CSDH are of GCS scoring “8-12” i.e. 25 (69.4%). Patients with very poor GCS status (3-7) at presentation were 5 (13.9%). CSDH are mostly unilateral in our study i.e. 33 (91.7%) [2,6]. Almost 3/5th (58.3%) of the patients displayed midline shift of more than 5 mm, which is an urgent indication for surgery. Complete recovery [7,8] is seen in 21 (58.3%) cases.
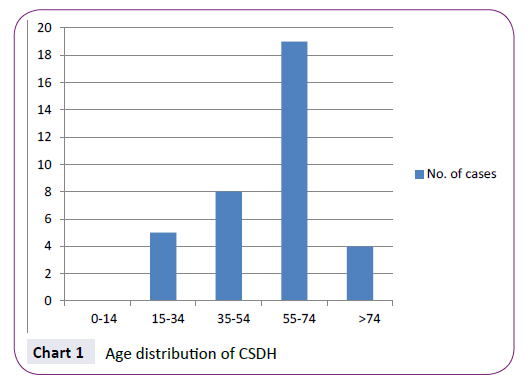
Chart 1: Age distribution of CSDH
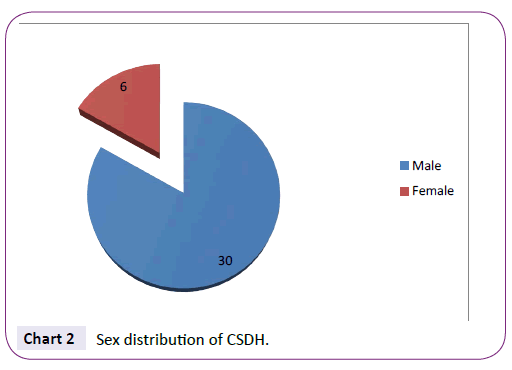
Chart 2: Sex distribution of CSDH.
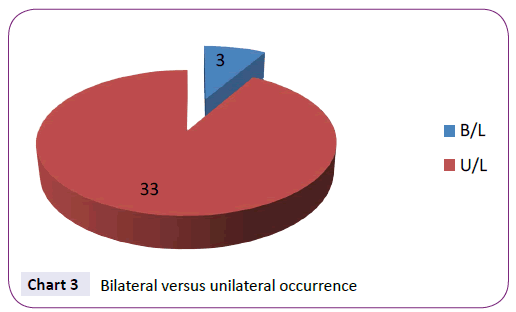
Chart 3: Bilateral versus unilateral occurrence
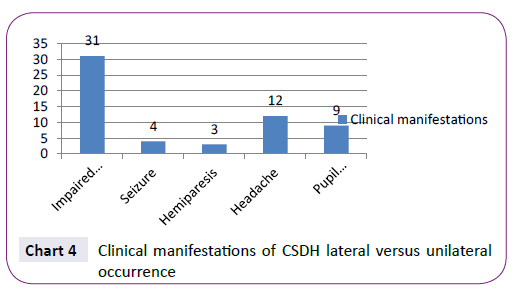
Chart 4: Clinical manifestations of CSDH lateral versus unilateral occurrence
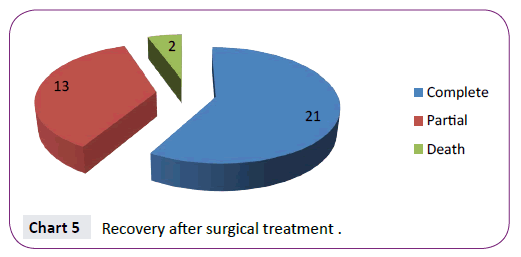
Chart 5: Recovery after surgical treatment .
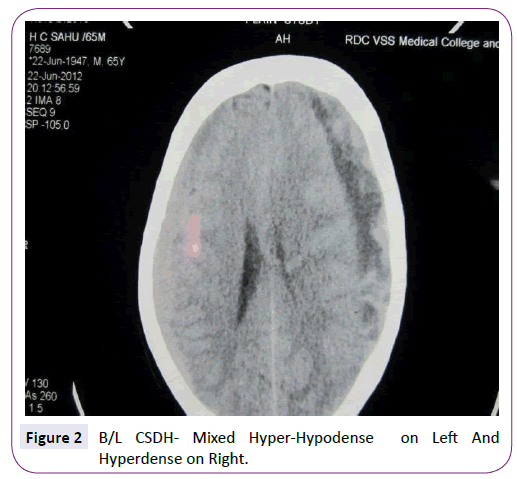
Figure 2: B/L CSDH- Mixed Hyper-Hypodense on Left And Hyperdense on Right.
Death occurred in 2 cases (5.6%); who were admitted with low general condition, having electrolyte abnormalities; because of prolonged treatment for ‘erroneous CVA diagnosis’ elsewhere. Out of the complications post operatively intra cranial hematoma [9] constitute the major part (11.1%). Contralateral hematoma and subdural empyema [2] are rare (2.7% each).
Discussion
A chronic subdural hematoma (CSDH) typically consists of darkish red liquefied blood and blood breakdown products with an associated neomembrane and is located in the subdural space. In strict anatomic sense, there is no true space called ‘subdural space’; rather it is a potential space that is created by the rupture of the bridging veins and expansion of the hematoma that gradually separates the layers of the dura and creates the “virtual” subdural space [9]. The space that the CSDH occupies is technically the intradural space. It is a disruption of the dural border cell layer from the deep pachymeninges. Blood in this space provokes an inflammatory reaction, which results in an enveloping membrane surrounding the blood.
The etiology of CSDH is not fully understood. Traumatic subdural effusion is widely accepted as a preliminary stage in the development of CSDH [10]. Traumatic subdural effusion is a result of arachnoid tearing caused by head injury and this fluid with or without blood in subdural space facilitates the formation of the so called “outer membrane”. This membrane then forms internal capillaries or sinusoids. These fenestrated blood vessels allow plasma fluid leakage into the subdural space. This phenomenon results in progressive expansion of subdural space [10]. Bleeding occurs repeatedly from capillaries with degenerative endothelium and is accompanied by local hyperfibrinolysis which is one of the causes for the growth of effusions into CSDH. Fluid ingress driven by osmotic gradient generated by the fibrinolytic products in the hematoma further helps in the genesis of CSDH.
Bleeding diathesis, blood dyscrasias and dural metastases may result in chronic subdural haematoma. In infants and children, infection as well as dehydration leading to hypernatremia may result in a subdural haematoma. Vitamin B1 deficiency has been blamed as a cause.
Reduction in intracranial pressure like after shunt surgery for hydrocephalus in infants and children plays a role in the production of both subacute and chronic subdural haematoma. Reduction of intracranial contents due to cerebral atrophy in the elderly favours the formation of chronic subdural haematoma. In such cases even minor trauma is sufficient to initiate the process.
Risk factors for CSDH: chronic alcoholism, epilepsy, coagulopathy, arachnoid cysts, anticoagulant therapy (including aspirin), cardiovascular disease (hypertension, arteriosclerosis), thrombocytopenia, and diabetes, In younger patients, alcoholism, thrombocytopenia, coagulation disorders, and oral anticoagulant therapy have been found to be more prevalent. Arachnoids cysts are more commonly associated with patients younger than 40 years with chronic SDH (subdural hematoma). In older patients, cardiovascular disease and arterial hypertension are found to be more prevalent.
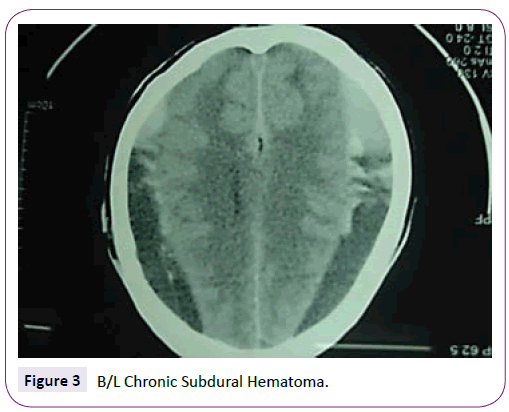
The aetiologies considered are trauma, coagulopathy, arachnoid cysts, vascular malformations, metastatic cancer, meningioma, or other neoplastic/ inflammatory lesions. People generally do well after surgical drainage of the CSDH, but the optimal surgical management is still debated. Chronic SDHs are 21 days (3 wk) or older and are hypodense (Figure 2) compared with the brain on CT scan. However, SDHs may be mixed in nature (Figure 3), such as when acute bleeding has occurred into a chronic SDH [9].
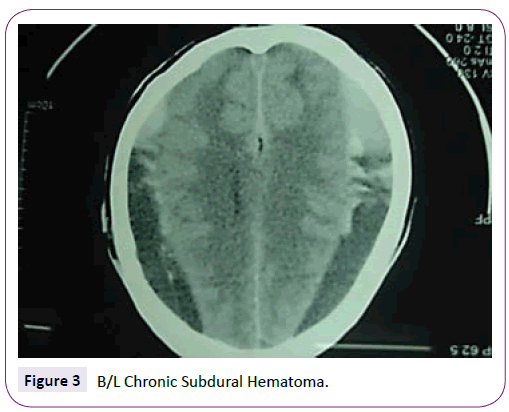
Figure 3: B/L Chronic Subdural Hematoma.
There are arrays of surgical procedures on offer in the treatment of CSDH. These include:
1) one or two burr-hole craniostomy; with or without saline irrigation and closed-system drainage; 2) twist drill craniostomy with or without drainage; 3) craniotomy and excision of the subdural membranes; 4) percutaneous needle trephination and open system drainage with repeated saline rinsing; 5) replacement of the haematoma with oxygen via percutaneous subdural tapping without irrigation and drainage; 6) Craniotomy with membranectomy and 7) continuous subgaleal suction drainage. The procedures most commonly resorted to are twist drill--drainage, burr-hole drainage and craniotomy.
Burr-hole drainage is the most favoured and practised technique and usually done through the placement of two burr-holes. Re expansion of the brain after hematoma evacuation is the most important guiding factor for good outcome. The reexpansion of the brain is inhibited by presence of residual clots and membrane, air in subdural space, and high brain surface elastance.
A single burr-hole is sufficient for drainage of the hematoma. The irrigation of the subdural space that follows helps in the evacuation of residual clots and membrane shreds, dilution of profibrinolytic compounds and elimination of air from subdural space. The controlled pressure and circumferential syringe irrigation may help in breaching of membrane and removal of far off clots along with membrane shreds. Using controlled pressure syringing irrigation is a necessary precaution to minimize the possible pressure injury to the cortical vessels by the saline jet.
Conclusion
CSDH is a common neurosurgical entity which mimics many neuropsychiatric conditions; patients are mostly elderly hence prone to the social neglect by attributing the patient’s condition to senile neurological changes. Hence a high degree of suspicion and CT scan is necessary wherever suspicion arises. Outcome of surgery is good; so urgent surgical intervention should be contemplated. Our prospective study confirms that “single burr-hole with saline lavage” technique is an adequate and safe treatment; having a very low recurrence and mortality rate. A short operating time, ease and simplicity of the procedure are also it’s advantages. This study in the South Asian nation also provides with the epidemiological data of this common neurosurgical entity, however a better designed, double blind randomized trial with more number of participants will be needed to reinforce our findings.
Patient Consent
The patients/guardian (children) have consented to the submission of the case report to the journal.
Competing Interests
We have no financial/non-financial (political, personal, religious, ideological, academic, intellectual, commercial or any other) competing interests.
Author’s Contribution
1-SRT, RNP, AKM carried out the investigation, data keeping.
2-SRT drafted the manuscript.
3- SRT, AKM, RNP, SM helped in preparation of the patient preoperatively and followed up the patient postoperatively.
4-SRT, AKM, RNP, SM participated in the surgical procedures.
5-SRT, SM, RNP, HKM participated in the design of the study and reviewed the literature.
6-SRT, RNP, SM, HKM conceived of the study, and participated in its design, coordinated and scrutinized the manuscript.
7-SRT, SM, HKM, JM overviewed the study.
8-All authors read and approved the final manuscript.
Acknowledgement
All the patients/ guardians of dept of Neurosurgery, VSS Medical College, Burla, Odisha, India for generously participating in the study; all staffs and faculties of dept of Neurosurgery/ dept of General Surgery, VSS Medical College, Burla, Odisha, India for their active support throughout.
7915
References
- Kudo H, Kuamura K, Izawa I (1992)Chronic subdural hematoma in the elderly: Present status on Awaji Island and epidemiological prospect. Neurol Med Chir (Tokyo) 32:207-209.
- Stanisic M, Lund JM, Mahesparan R (2005) Treatment of chronic subdural hematoma by burr holecraniostomy in adults: Influence of some factors on postoperative recurrence. ActaNeurochir (Wien) 147: 1249-1256.
- Gonogunta V, Buxton N (2001) Warfarin and chronic subdural hematomas. Br J Neurosurg 15: 514-517.
- Ikada K (1990) Relation of regional cerebral blood flow to hemiparesis in chronic subdural hematoma. Surg Neurol 33:87-95.
- Drake ME (1993) Mozart’s; chronic subdural hematoma. J Neurology (Minneap) 48:2400.
- Weigel R, Krauss J K (2004) Concepts of neurosurgical management of chronic subdural hematoma: Historical perspectives. Br J Neurosurg18: 8-18.
- Prabhu SS, Zauner A (2004) Surgical management of traumatic brain injuries. Winn R, Editor, Youman’s Neurological Surgery: W.B Saunders Co 5145-5180.
- Marike Z, Muizelaar JP (2004) Clinical pathophysiology of traumatic brain injury, chapter 324, Youman’sNeurolSurg fifth ed., pg. 667.
- Kumar P, Kiran U (2013) Management of chronic subdural haematoma: Single burr-hole drainage and irrigation using the technique of “syringing”: The Indian journal of Neurotrauma 10: 105-108.