Key words
Condom, HIV/AIDS, labour migrants, overseas, paid/unpaid partner
Introduction
There is growing recognition that migration is an essential and inevitable component of the economic and social life of every State, and that orderly and properly managed migration can be beneficial for both individuals and societies. [1]
Nepal today is well recognized as the country of origin for labour migrants mainly to the Gulf Cooperation Council and Malaysia. Migrants' remittances make up about 21 per cent of GDP of Nepali economy. [2] Youth unemployment has recently become a crucial problem in Nepal—youth make up 40% of the total urban population, youth literacy is 70%, while youth unemployment is more than 11%. [3] Unable to absorb the growing labour force, the Nepalese government has been promoting overseas employment opportunities for its citizens. [4]
Globally, the epidemiology of HIV/AIDS is closely linked to the process of migration. Research from Africa and Asia has demonstrated a link between migration and multi-partner sexual networking as well as the prevalence of sexually transmitted infection (STI)/HIV infection. [5]
“Migrant populations have a greater risk for poor health in general and HIV infection in particular. This is due to the impact of socio-cultural patterns of the migrant situation on health, their economic transitions, reduced availability and accessibility of health services, and the difficulty of the host country health care systems to cope with the traditions and practices of the immigrants”. [6] When people migrate, they are exposed to behaviours and norms that tend to be different from those of their place of origin. Migration has been identified as an independent individual risk factor for the acquisition of HIV. [7] As social control in migrant communities is often limited, sexual relationships that are prohibited at home are often possible abroad. Besides continuing to belong to their home communities, migrants gradually adapt to their new communities abroad. In so doing, they adopt a so-called 'migrant identity' which can lead to a denial of certain (sexual) behaviours. All kinds of sexual behaviour seem to be possible abroad, as long as other people do not find out. [8]
Nepal’s HIV and AIDS epidemic is concentrated amongst most-at-risk populations (MARP). [9] These groups include Intravenous Drug users (IDUs), Female Sex Workers (FSWs) and their clients, and Men having Sex with Men (MSM). Migrant males, uniformed service and transport workers have also been identified as at risk groups. However, the data demonstrate that in the case of migrants this is true only when they are clients of sex workers both in country and abroad. In Nepal, hundreds of migrant workers leave country for overseas employment every day. They are vulnerable to HIV which becomes more important when they return to their country and then may transmit the infection to their family. And also an examination of perceived risk of getting AIDS may have important implications for health if the perceptions are rational and lead to a willingness to avoid risky behaviour. In addition, an understanding of the association between perception of risk and sexual behaviour may facilitate the design of AIDS-preventive measures necessary to check the spread of the disease among different population subgroups. [10] The present study attempted to identify the sexual behaviour of Nepali migrant workers in overseas and their perceived risk of HIV/AIDS.
Methods
A cross sectional study was carried out from 1st September 2009 to 28th February 2010 in different cities of Nepal. Those migrants who have worked for at least 6 months overseas and have returned from within 3 months to 2 years from the date of interview from any of the 20 countries: Qatar, Saudi Arabia, United Arab Emirates (UAE), Oman, Kuwait, Bahrain, Iraq, Israel, Maldives, Malaysia, Singapore, Hong Kong, Brunei, Macao, Saipan, South Korea, Kosovo, Latvia, the Seychelles and South Africa were interviewed using the semi-structured questionnaire to study their sexual behaviour while in overseas and their perceived risk of HIV/AIDS. Returnee migrants were identified from different recruitment agencies using purposive technique whereas snow ball technique was used to trace out returnees in different houses and hotels. The tools were prepared and finalized by incorporating the variables that were included in the related studies done by Saggurti et al., [5] Wolffer et al., [8] Akwara et al., [10] Khan et al., [11] Prata et al., [12] Tamang et al., [13] and Puri et al. [14] Informed verbal consent was taken from respondents before asking the questions. The respondents were not forced to participate in the study. Questions were not asked in a way that would hurt their dignity. The purpose of the study was explained to the participants. The respondents were assured that their answers would remain private, unanimous and confidential. Ethical approval was obtained from ethical board of School of Public Health and Community Medicine, BPKIHS, Dharan, Nepal.
Microsoft Excel 2007 was used for data entry. Descriptive statistics was used for analysis of data using frequency table, percentage, and cross tabulation. SPSS-14 and NCSS-PASS software were used for data analysis.
Results
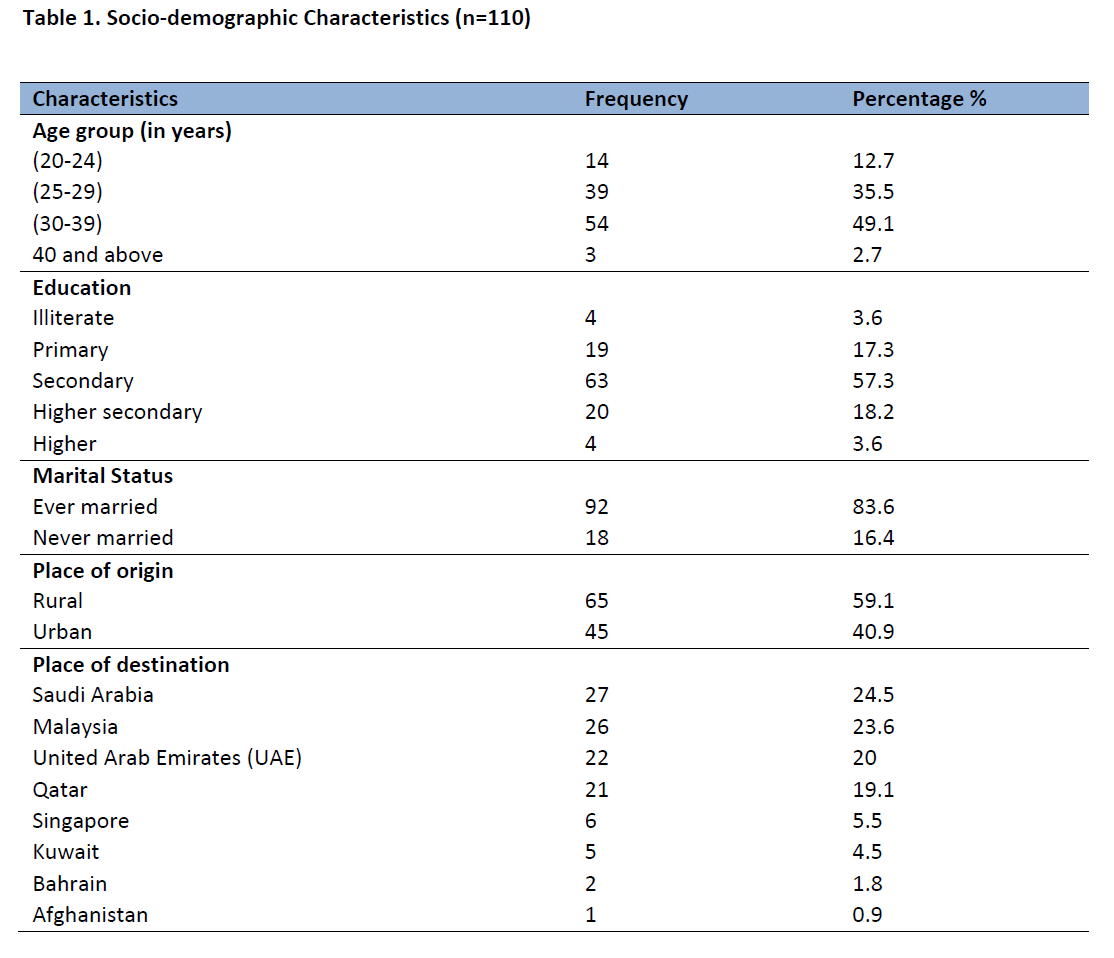
The respondents ranged from those aged 20 years to 53 years with mean age 30.27 years. Only 3.6% of the respondents were illiterate. About 85% were ever married with the average age at marriage being 22.88 years. More than half of the respondents were from rural areas in the origin country. Saudi Arabia, Malaysia, UAE and Qatar were found to be the popular countries of destination.
The median length of employment was 36 months with the range of 136 months. 17% of the respondents had worked for less than 2 years, 56% for 2-4 years, 19% for 4-6 years and 7% for more than 6 years. Complete male setting accommodation was common for workers in overseas with 88% respondents living in male only setting, 11% in male-female mixed setting and around 1% living separately (Table 1).
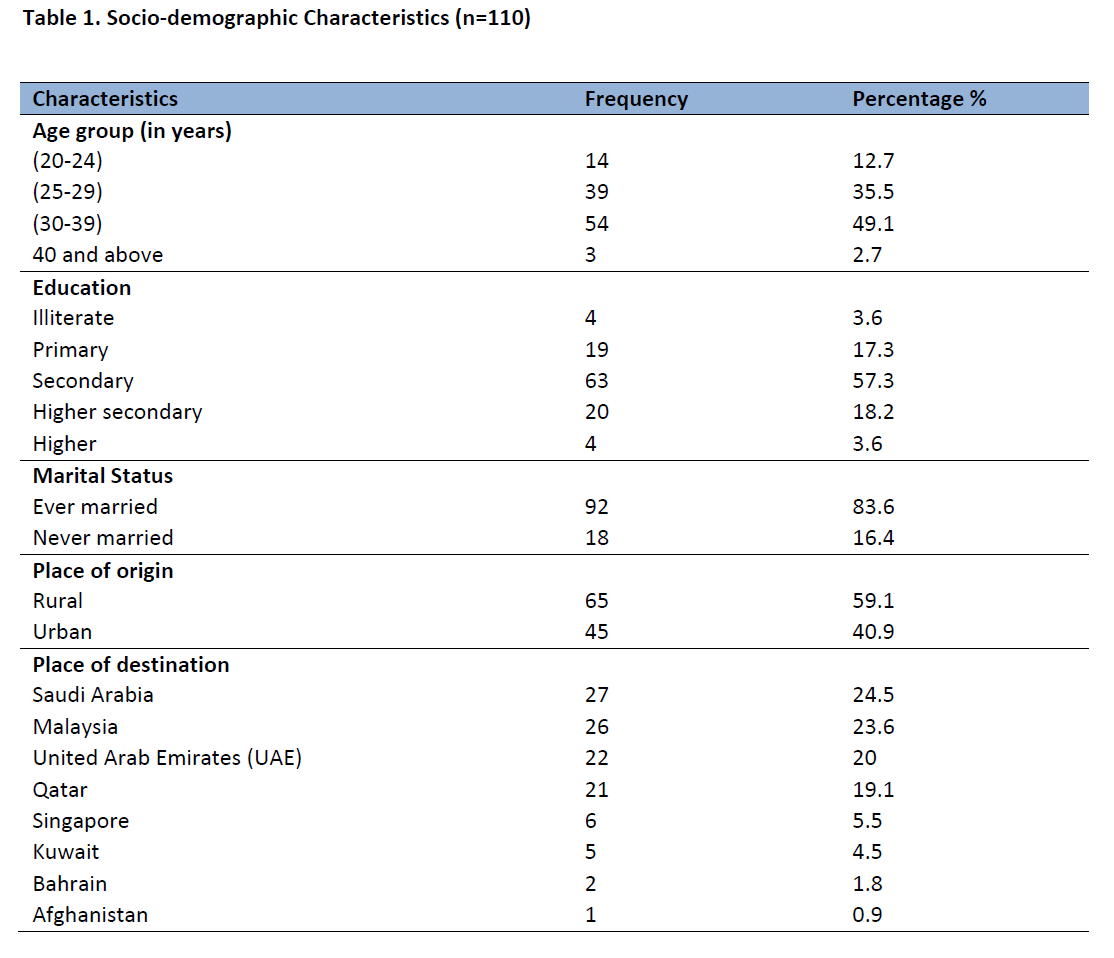
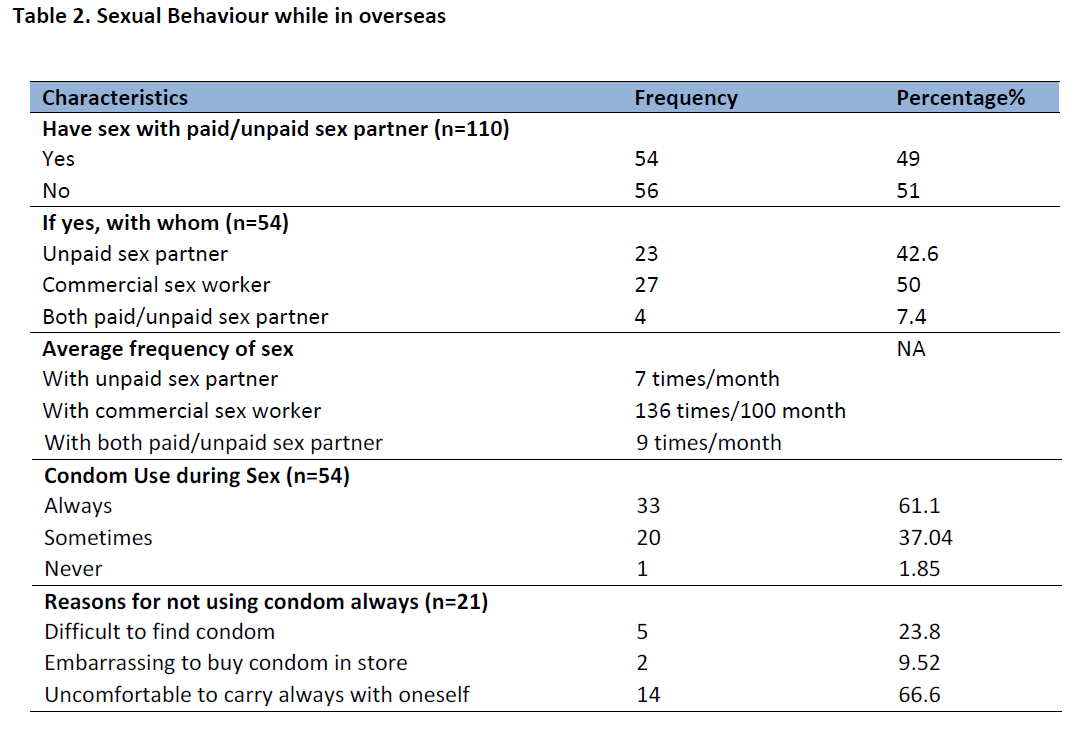
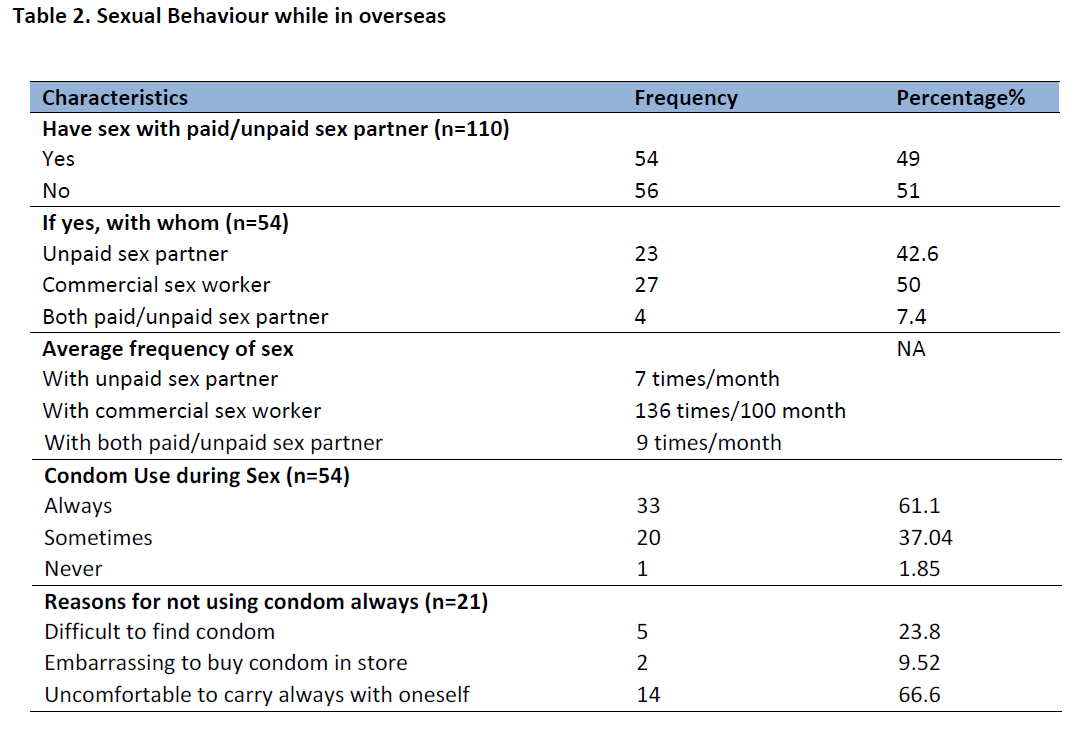
Table 2 describes the sexual behaviour of respondents while in overseas. Around 50% of the respondents had sex with paid/unpaid partner while in abroad. Among 54 respondents having sex, 23 had sex with non spousal unpaid partners, 27 with the commercial sex workers, and 4 with both paid and unpaid partners. None of the respondents reported having sexual relation with males. For majority of the respondents, co-working female friends were their unpaid sex partners. The average frequency of sex was 4 times per month. Out of 54 respondents who had sexual relation while abroad, 61.1% of them always used condom during sex, 37.04% sometimes used condom and 1.85% never used condom. Among 21 respondents who didn’t always use condom, 15 were from Gulf countries and 6 were from Non-Gulf countries. All of the respondents who mentioned difficulty in finding condom as the reason for not use of condom always were from Gulf countries.
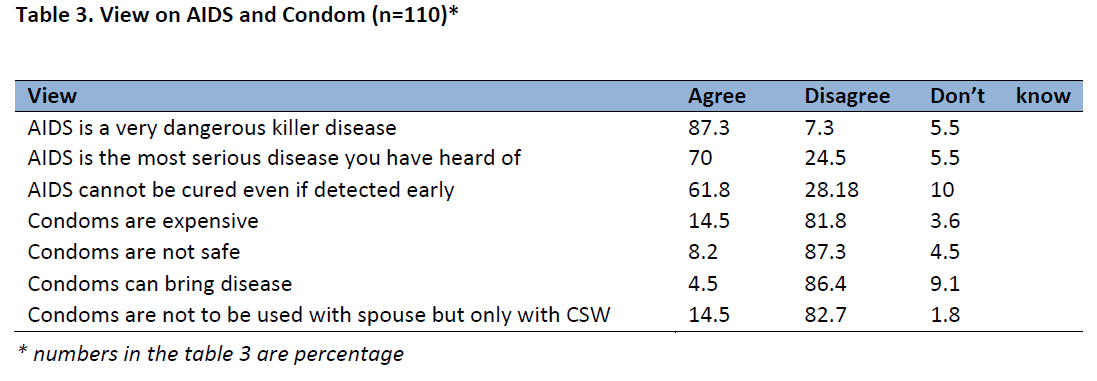
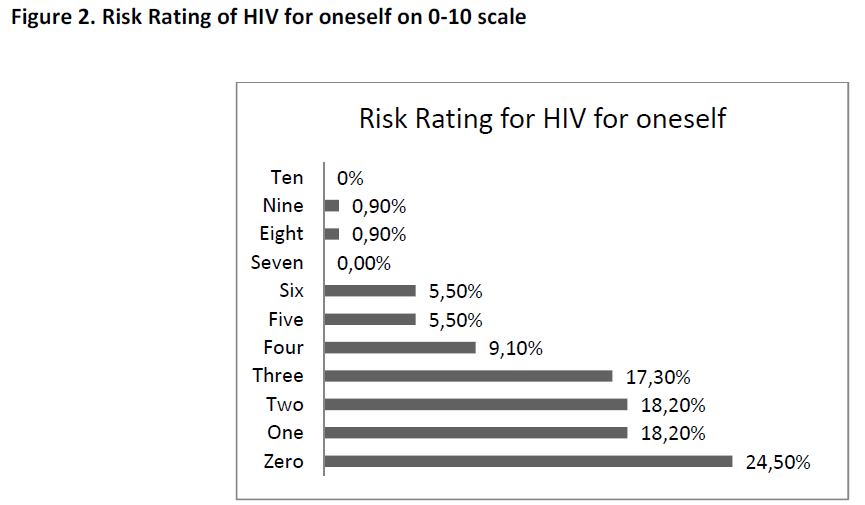
The majority of the respondents disagreed with the view that condoms are not to be used with spouse but only with Commercial Sex Worker (CSW) whereas only 14.5% agreed the view. (Table 3) More than half of the respondents (57.3%) perceived themselves to be at no risk of HIV. However, in case of their friends, only 21.8% perceived their friends to be at no risk of HIV (Figure 1). When respondents were given to rate their risk of HIV on scale from 0-10, only 24.5% rated their risk of HIV at zero (Figure 2).
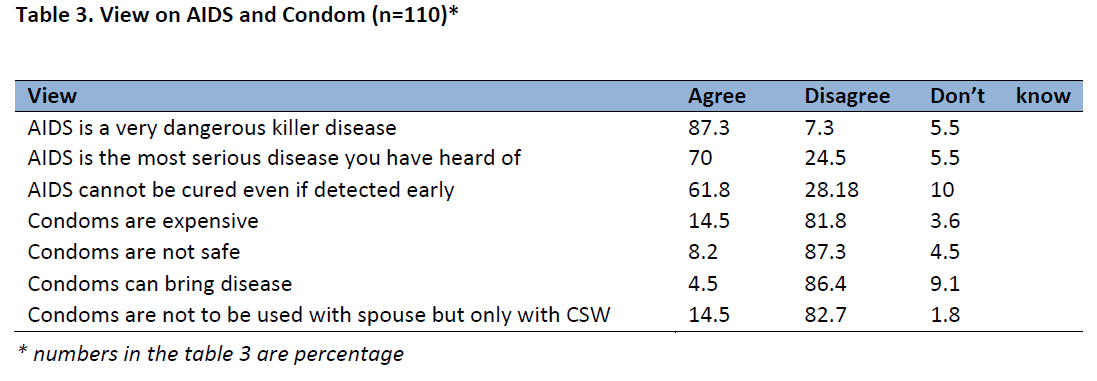

Figure 1: Perceived risk of HIV for oneself and for their friends
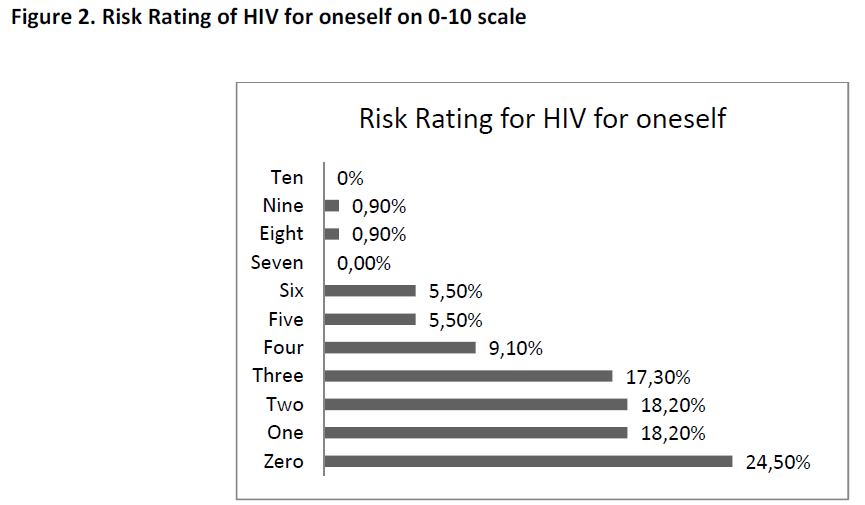
Figure 2: Risk Rating of HIV for oneself on 0?10 scale
The risk perception of HIV for oneself was found higher with increase in educational status. Out of 4 respondents with no formal education, 3 (75%) kept themselves at no risk of HIV/AIDS whereas among 19 respondents with primary education, 10 (53.62%) kept them at some risk of HIV. Similarly, 36 (41%) out of 87 respondents with secondary and higher studies combined kept themselves at some risk of HIV.
The majority of the respondents (93.6%) had never been diagnosed with a Sexually Transmitted Infection (STI). Only 6.4% were diagnosed with any STI till the date of interview. Similarly 68.2% of the respondents had ever knowingly had an HIV test and 50.9% had planned to do HIV test after returning from abroad. Among the total respondents, only 7% had ever used Voluntary Counselling and Testing (VCT) service. Those 93% respondents who had never used VCT service had also not heard of the service. A slightly higher percentage of those who had ever done HIV test by themselves (52%) than those who had never done HIV test by themselves(23%), kept them at some risk of HIV for themselves whereas around 77% of the respondents who had never done HIV test knowingly by themselves kept themselves at no risk of HIV.
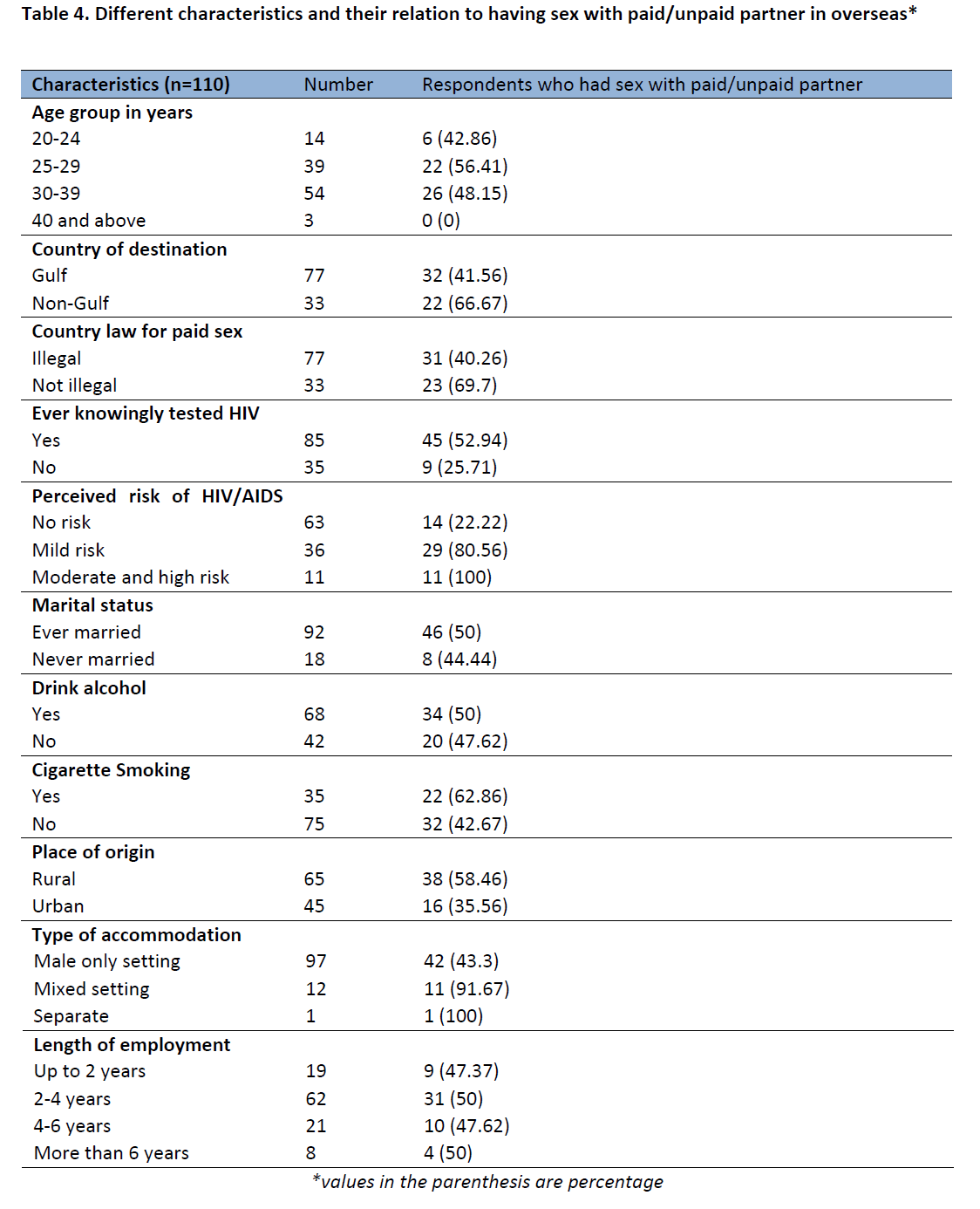
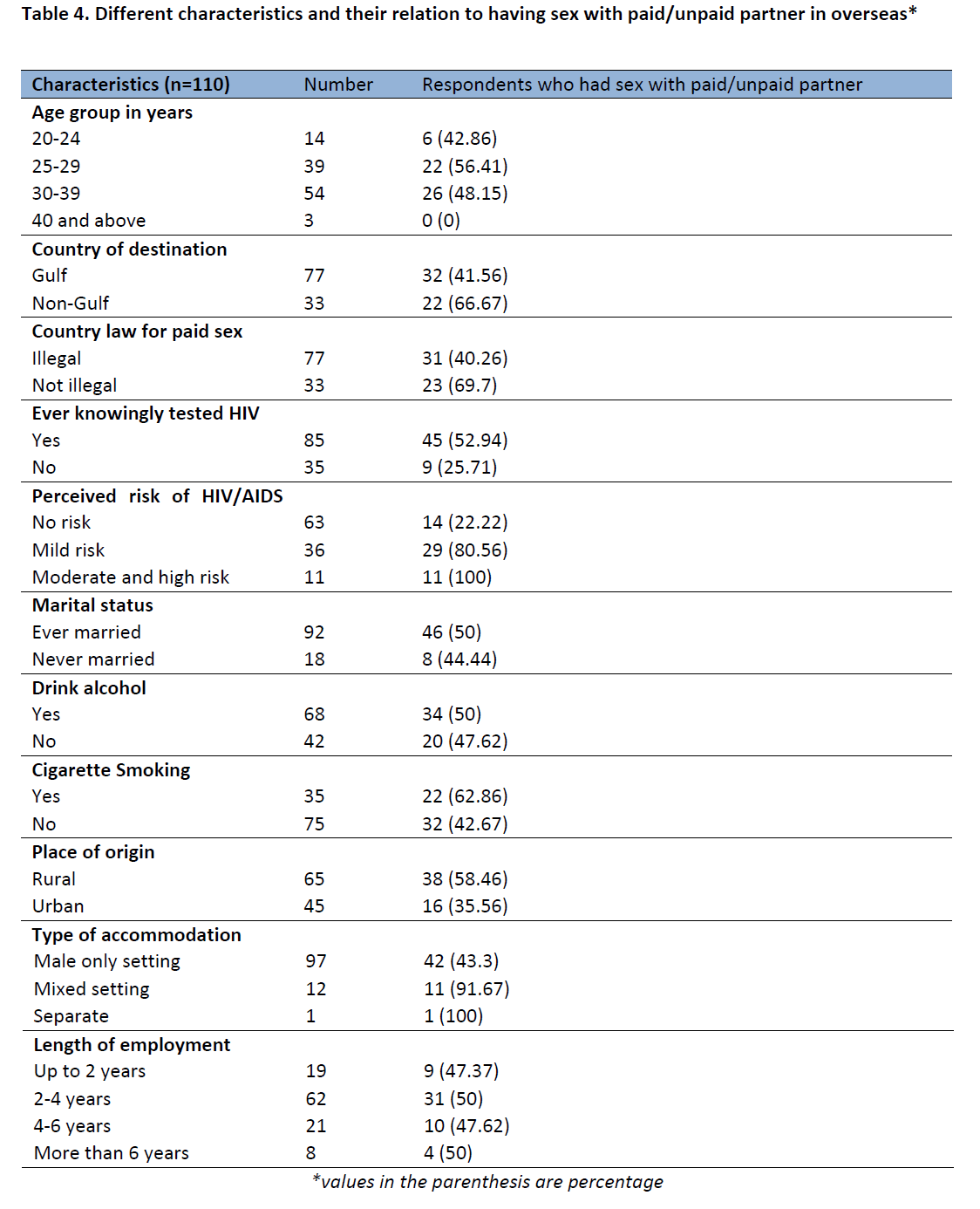
Out of total respondents in the age group 25-29 years, 56.4% had sexual intercourse with non-spousal paid/unpaid partners while in abroad. Similarly, this was 48% for respondents in the age group 30-39 years (Table 4). There is not much difference in the pattern of sexual activities being performed regardless of the country law. Among the respondents who had sexual relation abroad, 83.3% had knowingly done HIV test. Less percentage of respondents (22.22%) who perceived themselves at no risk had sexual relation in abroad whereas majority of those who perceived themselves at some risk (mild, moderate and high), had sex with paid/unpaid partner in abroad. Similarly, it was found that respondents were almost equally likely to be involved in having sex in overseas despite their marital status and their status of drinking alcohol. However, 62.8% of smokers had sex while 42.7 non smokers had sex. Those having mixed setting accommodation were more likely to have sex with paid/unpaid partner compared to those living in complete male setting.
Discussion
There is growing recognition of the need to address migrants’ HIV and related vulnerabilities but the knowledge on this issue is very limited in the Asian countries. [15] This study is aimed at identifying the sexual behaviour of the Nepali migrant workers while in the overseas and their risk perception of HIV/AIDS.
The findings from different studies revealed that unsafe sexual habits (based on sex with paid/unpaid partner, non use of condom, frequency of sex) are prevalent among migrant workers going overseas. [16,17]
A study in Bangladesh also revealed that most of the migrants had sexual relationship while staying abroad with causal partners or went to CSWs and due to lack of information and knowledge migrant workers engaged themselves to the risky sexual behaviour. [11] Migrants may get involved in risky sexual behaviour with other migrants also as a means of recreation. [15] Risky sexual behaviours such as premarital sex, extramarital sex, and commercial sex are increasingly observed among rural-to-urban migrants. [18]
The findings reveal that the migrants going to Gulf countries are more vulnerable to HIV/AIDS as compared to migrants going to Non-Gulf countries. According to a study some West Asian countries do not allow migrants to carry condoms as they believe it is against the tenets of Islam. [15] Similar to this among 15 respondents out of 21 who did not always use condom and for whom the reason behind non use of condom was “difficult to find condom” were from Gulf countries.
According to the AIDS risk reduction model, knowledge of AIDS is a prerequisite to recognizing risky behaviour and taking action to change it. [19] A study conducted among youths in Zambia found that knowledge on HIV/AIDS is associated with a reduced probability of sexual experience and an elevated level of condom use among boys. [20] The association between higher educational attainment and increased knowledge of HIV risk factors as well as education and HIV risk perception has been well documented across studies in most developed countries. [21] In the same way, among returnee migrants from overseas in Nepal, the risk perception of HIV/AIDS for oneself is higher with increase in educational status. However despite their knowledge on severity of disease i.e. majority of the respondent (87.3%) agreed that HIV/AIDS is the dangerous killer disease, 42.7% kept them at some risk of HIV. A similar finding was shown by a study among five high risk groups in Uganda [22] that despite the HIV/AIDS epidemic, awareness and perception of people with multiple sexual partners as being highly vulnerable to contracting HIV, these groups had only changed their sexual behaviour a little, and they reported to be continuing with multiple sexual partners for a variety of reasons. Among men, the constant desire to have sexual pleasure, which was greatly facilitated by their financial status, was the force behind their reckless sexual behaviour. [22]
The study found that those who did not have sex with paid/unpaid partner in overseas put them at no risk of HIV and very few of those who had sex put themselves at no risk. The majority of those with sexual relation while overseas perceive themselves to be at some risk (mild, moderate or high) of HIV. Only 24.5% rated themselves at zero risk for HIV/AIDS based on their sexual behaviour. This finding differ from the finding of Puri M. and Cleland J [14] in a study done among young migrant factory workers in Nepal, where no significance difference was found in perceived risk between those who did and did not have a non regular sex partner in previous 12 months.
According to UNAIDS report of July 2010, among the countries which have been included in the study, Afghanistan, Bahrain, Kuwait, Qatar, Saudi Arabia and UAE have the country law that deem sex work as illegal whereas Singapore and Malaysia have the country law that do not deem sex work as illegal. [23] Among the respondents who were in country where sex work was illegal, 40.3% had sex with paid/unpaid partner. Similarly among the respondents who were in country where sex work was not illegal, 69.7% had sex with paid/unpaid partner. This shows that there is no more difference in the pattern of sex trade regardless of country law.
Finding of a study done by He et al., [24] about sexual behaviour of male rural migrants in China, shows that risk taking behaviour increased with decreasing age. Younger men initiated sexual intercourse earlier and had premarital sex and sexual partner as well as more frequent sexual encounters.
The present study result shows similarity to this finding to some extent. This has found that the risk taking behaviour is higher in the lower age range like 20-24 years, 25-29 years and 30-39 years that among the respondents in the higher age range like 40 years and above.
As found by Halli et al., [25] this study also found that there is no difference in the risky behaviour between ever married and never married migrant workers. Findings of this research show that risky behaviours were higher among those with mixed setting accommodation which is similar to the finding of Puri and Cleland [14] that boys who were currently living in a mixed gender hostel were more likely to be sexually involved than others. Workers working abroad for more than 4 years up to 6 years were more likely to get involved in having sex with paid/unpaid sex partner which was unlike to the finding Puri and Cleland that those young workers who are working in their present job for less than 1 year were more likely to report non regular sexual relationship than those working more than 1 year. However, Htoo and Panza [26] in a study among Myanmar migrant fishermen in Thailand found that longer duration of stay (1-4) years, negative attitude towards HIV/AIDS and condom use were statistically associated with practice of unsafe sex with sex workers.
Only 61.1% of those who had sex with paid/unpaid partner always used condom and remaining 38.9% which is still a high proportion sometimes or never used condom though 87.3% of the respondents disagreed the view that ‘condoms are not safe’. 52.7% of the respondents disagreed that condoms are not to be used with spouse but only with wife however 44.5% agreed and 2.7% didn’t know about it representing those who had never used condom. This finding is important because the sexual habit of workers while in overseas directly affects the wives when they return back, in the context when, still around 50% of the total respondents have the attitude that condoms are not to be used with wife but only with sex workers. In connection to this, 92.7% of the respondents said that condom prevent from STDs/HIV which might represent their view that only sex workers are the sources of HIV/AIDS.
Regarding the use of preventive behaviour, those respondents who have been involved in risky sexual behaviour while abroad are more likely to ever knowingly do HIV test by them and also plan to do HIV test after returning from abroad. A similar result has been found by Kevin et al., [27] that, those who have been HIV tested were more likely to have been previously diagnosed with an STI or perceived themselves to be at increased risk of acquiring HIV suggesting that the uptake of HIV testing among the migrant communities may be driven by actual or perceived HIV risk.
The study found that more respondents from rural areas in the country of origin were found to have sex with paid/unpaid partner than those from urban areas. This finding might be associated with the finding of Regmi [28], in a study of barriers to sexual health services for young people in Nepal that, for sexual and reproductive health services, rural people have to rely on government health services which are not youth friendly and include very few sexual health services which decreases their access to information related to sexual and reproductive health as compared to urban youths who have access to more sources of information.
Conclusion
Migration is an independent individual risk factor for unsafe sexual behaviour and vulnerability to HIV/AIDS. Findings showed that unsafe sexual habits are prevalent among Nepali labour migrants in the overseas. For the majority of those having sex while in abroad, co-working female friends were the non spousal unpaid partners. This represents that female migrant labours are also equally involved in risky sexual behaviour.
Hence, the HIV prevention programs need to target both male and female labour migrants in the work site in the country of destination. Irregular use of condom despite affordability and knowledge that condoms can prevent from HIV and STD shows that there is need of counselling and positive attitude building towards condom use. Around 15% of the respondents said that condoms are to be used with commercial sex workers and not with wives and this attitude might put their wives and family at the country of origin at risk of HIV. Therefore, awareness raising activities on HIV/AIDS, Behaviour Change Communication (BCC) program for helping them change their risky sexual behaviours and other preventive actions like promotion of condom use, easy access to condom; counselling and testing services need to be taken in the country of origin, addressing both male and female prospective and returnee migrants.
3017
References
- About migration: International Organisation for Migration. https://www.iom.int/jahia/Jahia/about-migration/lang/en, (accessed on 1st September 2010).
- Nepal facts and figures: International Organisation for Migration, Nepal. https://www.iom.int/jahia/Jahia/about-migration/lang/en, (accessed on 1st September 2010).
- Unleashing economic growth, Region based urban development strategy for Nepal: ADB, 2010.
- Gurung G. Patterns in foreign employment and vulnerabilities in HIV: Nepal Institute of Development Studies, 2000.
- Saggurti N, Verma RK, Jain A, RamaRao S et.al., HIV risk behaviours among contracted and non-contracted male migrant workers in India: potential role of labour contractors and contractual systems in HIV prevention. AIDS 2008;22(5): S127-S136.
- Migrant population and HIV/AIDS, The development and implementation of programmes: Theory, methodology and practice: UNESCO/UNAIDS, 2000 June.
- Gurung, G. An overview paper on overseas employment in Nepal, 2004, ILO, Nepal.
- Wolffers I, Farnandez I, Verghis S, Vink M. Sexual behaviour and vulnerability of migrant workers for HIV infection. Culture, Health & Sexuality 2002; 4(4): 459 -473.
- HIV and migration country profile, Nepal. 2009. (https://aidsdatahub.org/en/regional-profile/hiv-and-migration/cat_view/207-regional-profiles/208n-asia-pacific-region/211-regional-reviews/221-hiv-and-migration-?limit=5&order=hits&dir=ASC&start=10, (accessed on September 3, 2010)
- Akwara PA, Madise NJ, Hinde A. Perception of risk of HIV/AIDS and sexual behaviour in Kenya. Journal of Biosocial Science 2003 ;35(3):385-411.
- Khan MS, Sakiul MM, Shaon HI. HIV/AIDS knowledge and vulnerable factors of overseas migrant workers of Bangladesh. IntConf AIDS 2000 July 9-14.
- Prata N, Morris L, Mazive E, Vahidnia F, Stehr M. Relationship between HIV risk perception and condom use: Evidence from a population based survey in Mozambique. IntFam Plan Perspect 2006;32(4):192-200.
- Tamang A, Nepal B, Puri M, Shrestha D. Sexual behavior and risk perception among young men in border towns of Nepal.Asia Pac Pop J.2001.
- Puri M, Cleland J. Sexual behavior and perceived risk of HIV/AIDS among young migrant factory workers in Nepal. Journal of Adolescent Health. 2006; 38:237-246.
- No safety signs here: Research study on migration and HIV vulnerability from seven South and North East Asian Countries: UNDP/APMRN 2004;17.
- Carballo M, Nerurkar A. Migration, Refugees, and Health Risks. Emerg Infect Dis. 2001. https://dx.doi.org/10.3201/eid0707.017733, (accessed on October 9, 2012)
- He N. Socio-demographic characteristics, sexual behaviour, and HIV risks of rural-to-urban migrants in China. Biosci Trend 2007;1(2):72-80.
- Catania JA, Kegeles SM, Coates TJ. Towards an understanding of risk behaviour: an AIDS Risk Reduction Model (ARRM). Health Education Quarterly 1990;17(1):53-72.
- Magnani RJ, Karim AM, Weiss LA, Bond KC, Lemba M, Morgan TG. Reproductive health risk and protective factors among youth in Lusaka, Zambia. Journal of Adolescent Health 2002; 30(1):76-86.
- Brown LK, Lourie KJ, Flanagan P, High P. HIV-related attitudes and risk behavior of young adolescent mothers. AIDS Education Preview 1998;10: 565-73.
- Ntozi JP, Najjumba IM, Ahimbisibwe F, Ayiga N, Odwee J. Has the HIV/AIDS epidemic changed sexual behaviour of high risk groups in Uganda? African Health Science 2003;3(3):107-16.
- Making the law work for the HIV response. A snapshot of selected laws that support or block universal access to HIV prevention, treatment, care and support: UNAIDS, 2010 July.
- He N, Detels R, Chen Z, Jiang Q, Zhu J, Dai Y, et al., Sexual behaviour among employed male rural migrants in Shangahi, China. Aids EducPrev 2006; 18(2);176-86.
- Halli SS, Blanchard J, Satihal DG, Moses S. Migration and HIV transmission in rural South India: An ethnographic study. Culture, Health & Sexuality 2007;9(1): 85-94.
- Htoo K.M and Panza A. Factors associated with unsafe sex behaviors for prevention of HIV/AIDS transmission among Myanmar migrant fisherman in Ranong, Thailand. Journal of Health Research 2009; 23: 43-47.
- Kevin M, Cock D, Low N. HIV and AIDS, other sexually transmitted diseases, and tuberculosis in ethnic minorities in United Kingdom: is surveillance serving its purpose? British Medical Journal 1997; 314: 1747-51.
- Regmi PR. Barriers to sexual health services for young people in Nepal. Journal of Health, Population and Nutrition. 2010 December. (Accessed from https://www.faqs.org/periodicals/201012/2198154391.html).