Hon-Ping Ma1,2,3, Po-Shen Chen1, Ju-Chi Ou1, Yung-Hsiao Chiang4,5,6,7, Shin-Han Tsai1,3, Wen-Ta Chiu3, Kuo-Hsing Liao8, Chung-Che Wu4,5,6,* and Kai-Yun Chen7,*
1Department of Emergency Medicine, Shuang-Ho Hospital, Taipei Medical University, Taipei, Taiwan
2Department of Emergency, School of Medicine, Taipei Medical University, Taipei, Taiwan
3Institute of Injury Prevention and Control, College of Public Health and Nutrition, Taipei Medical University, Taipei, Taiwan
4Department of Surgery, College of Medicine, Taipei Medical University, Taipei, Taiwan
5Division of Neurosurgery, Department of Surgery, Taipei Medical University Hospital, Taipei, Taiwan
6Translational Laboratory, Department of Medical Research, Taipei Medical University Hospital, Taipei, Taiwan
7Graduate Institute of Neural Regenerative Medicine, College of Medical Science and Technology, Taipei Medical University, Taipei, Taiwan
8Department of Neurosurgery, Wan Fang Hospital, Taipei Medical University, Taipei, Taiwan
*Corresponding Authors:
Chung-Che Wu
Department of Surgery, College of Medicine
Taipei Medical University, Taipei, Taiwan
Tel: 886-2-27372181#5013, 886-2-27361661#7652
Fax: 886-2-27390946
E-mail: dr.jcwu@gmail.com
Kai-Yun Chen
Graduate Institute of Neural Regenerative Medicine
College of Medical Science and Technology
Taipei Medical University, Taipei, Taiwan
Tel: 886-2-27372181#5013, 886-2-27361661#7652
Fax: 886-2-27390946
E-mail: kychen08@tmu.edu.tw
Received Date: May 18, 2017 Accepted Date: June 23, 2017 Published Date: June 27, 2017
Citation: Ma HP, Chen PS, Ou JC, et al. Significance of Balance Test in Assessing Emotional Aspect of Dizziness in Mild Traumatic Brain Injury Patients. J Neurol Neurosci. 2017, 8:3.doi: 0.21767/2171-6625.1000199
Keywords
Dizziness handicap inventory; Sway index; Stability index; Anxiety; Depression; Sleep problem; Propensity score
Introduction
Traumatic brain injury (TBI) is one of the major causes of neurobehavioral disorder [1]. The severity of TBI is categorized by the Glasgow Coma Scale (GCS) [2]. Approximately 90% of traumatic brain injuries are mild (GCS 13-15) and cannot be detected with computed tomography. Mild traumatic brain injury (mTBI) also has neurodegeneration implications leading to significant socioeconomic impact [3]. The number of reports of mTBI has increased significantly recently. While most mTBI patients recover within 3 months post-injury, approximately 15 percent of these patients have persistent post-traumatic symptoms which are grouped into three categories: (1) physical (headache, balance problems, dizziness, etc.), (2) cognitive (difficulty concentrating, etc.), and (3) behavioral /emotional (depression, anxiety, sleep problems, etc.). Several studies have made it clear that the acute phase of TBI carries the risk of depression, anxiety and sleep degradation [4,5]. Also, the problem in dizziness is one of most common complaints of mTBI patients., In general, vertigo and dizziness are typically indicative of inner-ear diseases as opposed to central nervous system diseases, and these patients with dizziness problems often suffer from depression and anxiety as well [5,6]. Additionally, Kayabasi et al. found that subjects who suffered from severe obstructive sleep apnea commonly showed abnormal vestibular responses [7]. Since patients with TBI have an increased risk of further injury [8], a focus on non-specific mTBI symptoms such as dizziness, insomnia, and anxiety may allow for predictions on the balance disorders experienced by these patients. Many studies have examined the effect of mTBI in veteran and military populations, in which comparisons between the subjective and objective measurements of balance disorders have been conducted [9,10]. In one study on patients in the aftermath of general TBI (GCS 3-15), an analysis of a total of 20 patients (10 TBI patients and 10 matched controls) showed a significant relationship between the objective changes in balance or postural equilibrium and subjective complaints of dizziness [9]. However, these symptoms are often less obvious in mTBI patients and predictions are therefore clinically difficult.
Since the increased risk of subsequent falls may correlate with dizziness or imbalance, the relationship between dizziness and balance in mTBI patients requires additional investigation. In this study, the non-military mTBI patients were studied with regard to the relationship between the subjective measurement of DHI and the objective clinical measure of balance impairment.
Methods
Subjects
The patients were recruited from three hospitals (Taipei Medical University Hospital, Wan Fang Hospital, and Shuang-Ho Hospital) between June 2012 and June 2014. This study was approved by the Taipei Medical University Joint Institutional Review Board (No.201003008, 201302027). A total of 1,157 mTBI patients were recruited for our study, and 286 (24.72%) patients enrolled with written informed consent. Among these 286 patients, 210 (73.43%) completed the questionnaires and all balance tests within one month of experiencing an mTBI. Upon protocol approval, 89 men and 121 women, aged older than 20 years, who had an mTBI as documented by their medical records through the following criteria: Glasgow coma score (GCS) of 13-15, and negative Computer Tomography (CT). Exclusion criteria included history of previous traumatic brain injury, cerebrovascular disease, and severe systemic medical illness.
Stability index and Sway index
The stability index, the average position of the subject from the center, and the sway index, the standard deviation of the stability index, were evaluated using a Biodex Balance System (Biodex Medical Systems, Inc., Shirley, NY, USA) [11]. Postural stability was assessed based on the overall stability index (OSI), anteroposterior stability index (APSI), and mediolateral stability index (MLSI). These indices include standard deviations used to assess fluctuations from the horizontal plane along the anteriorposterior and medial-lateral axes. For testing sway indices, participants were asked to stand on firm (IS) and foam surfaces (OS) and performed the test with eyes open (EO) and eyes closed (EC) for 30 seconds. There four tests were as follows: Eyes open firm surface (EOI), eyes closed firm surface (ECI), eyes open foam surface (EOO), and eyes closed foam surface (ECO).
Dizziness handicap inventory
The Dizziness Handicap Inventory (DHI) is a 25-item instrument used to evaluate individual handicap results from dizziness symptoms, composed of physical, emotional and functional aspects [12]. There are three possible scores: 0 for never, 2 for sometimes and 4 for always. The total score ranges from 0 to 100, with the emotional, physical and functional aspects contributing 36, 28 and 36 points, respectively.
The Chinese version of the DHI (Intraclass correlation coefficient 0.64, Cronbach alpha coefficient>0.7) was used [13]. A higher score indicates a greater degree of impairment.
BAI, BDI, PSQI
Anxiety and Depression were assessed using the Beck anxiety inventory and Beck depression inventory, respectively [14,15]. Both inventories consisted of 21 items and each item score ranged from 0 to 3, with the total score ranging from 0 to 63. The PSQI is a self-report questionnaire which contains a global sleep quality score and seven components: sleep latency, sleep efficiency, sleep disturbance, sleep medication, daytime dysfunction, sleep quality, and sleep duration [16]. The score for each of these components also ranges from 0 to 3, and the global score ranges from 0 to 21. For all three questionnaires, higher score indicated more severe problems. The Chinese version of BAI, BDI, and PSQI were used for all the patients in our study [17,18].
Data Analysis
Demographic data were showed and the psychometric data, as well as balance index data between two groups were compared by the student T-test and a nonparametric method, Mann-Whitney U test, for normal and abnormal continuous data, respectively.
A chi-square test was used to compare categorical data. The relationships among psychometric data and balance indices were assessed using the Pearson correlation coefficient and stepwise regression analysis. In addition, a propensity score model was included in the model in order to reduce the bias caused by confounders [19]. The Box-Cox Transformations was used for skewed outcomes [20], and the level of statistical significance was set at p<0.05. Statistical analyses were performed using R 3.1.2 (R Foundation for Statistical Computing, Vienna, Austria).
Results
This study consisted of 94 mTBI patients with complaints of dizziness and 116 mTBI without complaints (Table 1). The percentage of females in the dizziness group was significantly higher than that in the non-dizziness group. Additionally, the average age in the dizziness group was less than that of the nondizziness group, though the dizziness group did show a higher number of years of education. A high percent of subjects in the dizziness group also experienced headache. Neither height nor weight was significantly different between the two groups. From the results of all four self-reported questionnaires we found that anxiety, depression, sleep problems, DHI subscores, and DHI total scores were significantly different between the dizziness and non-dizziness groups. The total scores of the dizziness and non-dizziness groups were 40.43 ± 24.14 and 20 ± 21.75 out of a maximum possible score of 100, respectively. All questionnaire scores of the dizziness group were higher than those of the nondizziness group. However, none of the stability indices and sway indices were significantly different between the dizziness and non-dizziness groups.
| |
Dizziness |
Non-dizziness |
P value |
| Sample size (n) |
94 |
116 |
|
| Age, year (mean) |
37.47±12.54 |
42.71±14.27 |
0.009# |
| Male/Female (n) |
30 / 64 |
59 /57 |
0.009+ |
| Education (y) |
14.81±3.057 |
12.95±3.115 |
0.002# |
| Smoker (N/Y) |
59/35 |
68/48 |
0.639+ |
| Drinker (N/Y) |
44/49 |
57/59 |
0.520+ |
| Headache (N/Y) |
25/69 |
84/32 |
<0.001+ |
| Height, cm(mean) |
162.85±8.50 |
163.84±9.41 |
0.453# |
| Weight, kg (mean) |
60.96±11.87 |
63.91±13.93 |
0.173# |
| Questionnaires (mean) |
|
|
|
| BAI |
13.52±10.92 |
4.87±4.87 |
<0.001# |
| BDI |
13.32±10.19 |
6.13±6.51 |
<0.001# |
| PSQI |
9.59±4.52 |
7.33±3.85 |
<0.001# |
| DHI-physical |
12.94±7.64 |
6.60±6.45 |
<0.001# |
| DHI-emotional |
12.17±8.88 |
5.71±6.84 |
<0.001# |
| DHI-functional |
15.32±9.97 |
8.66±8.66 |
<0.001# |
| DHI-total |
40.43±24.14 |
20.97±21.75 |
<0.001# |
| Stability index |
|
|
|
| Overall |
0.49±0.27 |
0.49±0.28 |
0.998# |
| AP |
0.36±0.19 |
0.38±0.24 |
0.779# |
| ML |
0.22±0.16 |
0.21±0.13 |
0.367# |
| Sway index |
|
|
|
| Eye open firm surface |
0.51±0.28 |
0.51±0.28 |
0.865# |
| Eye closed firm surface |
1.15±0.60 |
1.07±0.51 |
0.774# |
| Eye open foam surface |
0.96±0.47 |
0.92±0.46 |
0.464# |
| Eye closed foam surface |
2.96±0.96 |
3.12±1.26 |
0.611# |
| Mechanisms of Injury(n) |
|
|
0.291? |
| Transportation accident |
26 (0.28) |
44(0.38) |
- |
| Falls |
49(0.52) |
55(0.47) |
- |
| Other |
19(0.20) |
17(0.15) |
- |
Values are means ± SD or n
#: Mann-Whitney U test
+: chi-square test
Table 1: Baseline characteristics.
There was a significant relationship between the emotional aspects of the DHI and the Sway index in the eye closed on firm surface condition (Table 2). There was no statistically significant association between the physical, functional, or total DHI score and the balance indices. All sway indices were significantly related to anxiety, and the sleep quality score affected the sway indices in both ECO and ECI conditions. The depression score (BDI) was related to the sway indices in the condition of standing on the foam surface. Age was weakly to moderately positively correlated with the stability and sway indices. That is, the stability and sway indices increased as age increased. Height also showed a significant mild to moderate relationship with all stability and sway indices, except the sway index of ECI. As the height decreased, the balance indices increased.
| |
Stability index |
Sway index |
| DHI components |
OSI |
APSI |
MLSI |
EOI |
ECI |
EOO |
ECO |
| |
|
|
|
|
|
|
|
| Physical |
<0.01 |
<0.01 |
-0.01 |
0.02 |
0.07 |
0.04 |
0.02 |
| Emotional |
0.08 |
0.06 |
0.06 |
0.09 |
0.13* |
0.1 |
0.11 |
| Functional |
<0.01 |
-0.01 |
0.01 |
0.03 |
0.08 |
<0.01 |
0.02 |
| Total |
0.03 |
0.02 |
0.02 |
0.05 |
0.11 |
0.05 |
0.05 |
| |
|
|
|
|
|
|
|
| Questionnaires |
|
|
|
|
|
|
|
| |
|
|
|
|
|
|
|
| BAI |
0.1 |
0.09 |
0.11 |
0.15* |
0.19* |
0.21* |
0.13* |
| |
|
|
|
|
|
|
|
| BDI |
0.01 |
<0.01 |
0.03 |
0.05 |
0.12 |
0.15* |
0.15* |
| |
|
|
|
|
|
|
|
| ESS |
-0.05 |
-0.04 |
-0.07 |
0.1 |
0.01 |
-0.01 |
-0.01 |
| |
|
|
|
|
|
|
|
| PSQI |
0.05 |
0.06 |
0.04 |
0.03 |
0.14* |
0.12 |
0.19* |
| |
|
|
|
|
|
|
|
| Other predictors |
|
|
|
|
|
|
|
| |
|
|
|
|
|
|
|
| Age |
0.35* |
0.40* |
0.17* |
0.31* |
0.29* |
0.34* |
0.45* |
| Height |
-0.26* |
-0.25* |
-0.15* |
-0.24* |
-0.1 |
-0.27* |
-0.23* |
| Weight |
-0.13* |
-0.11 |
-0.1 |
-0.13* |
-0.02 |
-0.12 |
-0.13 |
*: p-value <0.05
Table 2: Correlations (p-value) for the stability and sway indices (*: significant p-value <0.05).
The association between the DHI components and other mental problem scores are shown in Table 3. All three questionnaires were self-reported and showed a significant mild to moderate correlation with each DHI component, especially for the BAI. As the anxiety score increased, so did the emotional aspect score of the DHI (correlation coefficient 0.616), in addition to other aspects of the DHI. For depression, the BDI score showed a significant moderate relationship with the emotional aspect of the DHI.
| DHI components |
Age |
BAI |
BDI |
PSQI |
| Physical |
-0.025 |
0.514* |
0.434* |
0.337* |
| Emotional |
0.016 |
0.616* |
0.555* |
0.416* |
| Functional |
0.013 |
0.524* |
0.417* |
0.356* |
| Total |
0.003 |
0.603* |
0.511* |
0.400* |
*: significant (P-value <0.05)
Table 3: Correlations (p-value) among DHI components, BAI, and BDI (*: significant).
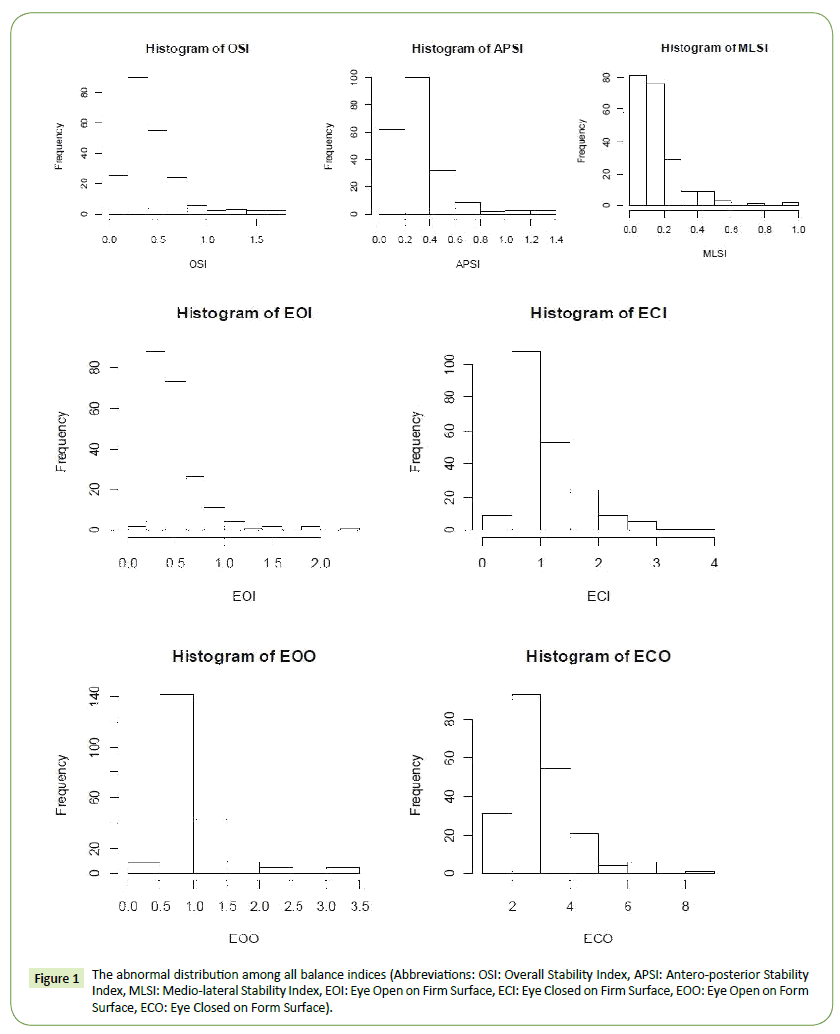
The propensity scores model, including the BAI, BDI, and PSIQ, were assessed and considered in the final model because all three mental problems were correlated with DHI components. Figure 1 shows that all of the indices were abnormally distributed. Therefore, all regression analyses required the Box-Cox transformation to correct for residuals, and the corresponding transferred coefficients (λ) are shown in Table 4.
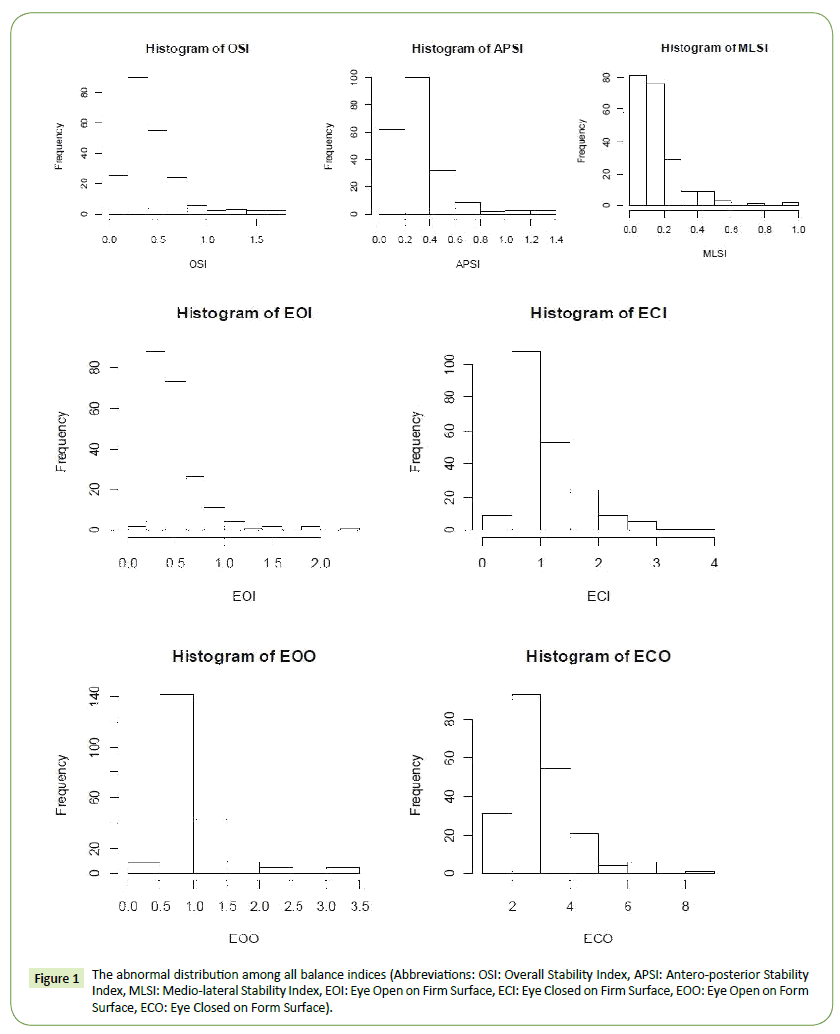
Figure 1: The abnormal distribution among all balance indices (Abbreviations: OSI: Overall Stability Index, APSI: Antero-posterior Stability Index, MLSI: Medio-lateral Stability Index, EOI: Eye Open on Firm Surface, ECI: Eye Closed on Firm Surface, EOO: Eye Open on Form Surface, ECO: Eye Closed on Form Surface).
Table 4 shows that there was no difference in the dizziness group when adjusted with propensity scores, but gender and age were significant predictors. In addition, we found that the emotional aspect of the DHI was a significant predictor for all stabilities and sway indices, except the MLSI. Moreover, the functional aspect of the DHI was also a significant predictor of the sway index in the EOO condition.
| |
λ |
Age |
Male |
Height |
Emotional |
Function |
| Stabilityindex |
| OSI |
-0.1818 |
0.013(<0.01) |
-0.238(<0.01) |
- |
0.009(0.03) |
- |
| APSI |
-0.101 |
0.015(<0.01) |
-0.207(<0.01) |
- |
0.009(0.03) |
- |
| MLSI |
- |
- |
- |
- |
- |
- |
| |
|
|
|
|
|
|
| Sway |
|
|
|
|
|
|
| index |
|
|
|
|
|
|
| |
|
|
|
|
|
|
| EOI |
-0.5051 |
0.016(<0.01) |
-0.276(<0.01) |
- |
0.011(0.02) |
- |
| ECI |
-0.2626 |
0.011(<0.01) |
- |
- |
0.009(<0.01) |
- |
| EOO |
-0.93 |
0.013(<0.01) |
- |
-0.011(<0.01) |
0.014(<0.01) |
-0.008(0.043) |
| ECO |
-0.2626 |
0.007(<0.01) |
- |
- |
0.004(0.06) |
- |
λ: Box-Cox transformation parameter
- : Not selected variable after stepwise
Table 4: Results of stepwise regression with propensity scores.
Discussion
It is important for clinicians to assess the physical conditions of mTBI patients through periodic clinical follow-ups, so they can assess the need for medical intervention. The strongly impaired balance in postural stability and sensory integration of mTBI patients were studied in comparison with healthy control participants [21]. The main goal of this study was to determine whether a more objective method of measurement could quantify the subjective complaints of dizziness. For the analysis of subjective complaints, the relationship between DHI scores and balance indices were assessed.
A higher level of handicap due to dizziness was anticipated for older people with physical degeneration, but there was no significant correlation between age and each aspect of the DHI in mTBI participants. Anxiety, depression and sleep problems were significantly related to the three aspects of the DHI and the total scores. The greatest correlation was found with the emotional aspect of the DHI when compared with other aspects of the DHI. In addition, all DHI components were highly related to anxiety.
In a study on general TBI involving 10 patients with GCSs between 3-15 and 10 matched control patients, Kaufman et al. showed that the relationship between the posturography and the physical aspects of the DHI was significant [9]. In our study, the emotional aspect of the DHI was a significant predictor for all stability and sway indices. Moreover, the functional aspect of the DHI was a significant predictor for the sway index in the EOO condition. Height was a significant predictor for most indices, except sway indices in both the ECI and ECO conditions.
The correlations between height and balance scores were significant when assessed directly. Interestingly, as body height increased, the balance indices increased and balance problems became worse. One possible explanation is that the effect of age and the one-by-one correlation coefficients did not consider other factors. Additionally, subjects of elderly age might have shorter heights overall.
The correlation between Sway indices and several psychologicallyassociated indices was significant. The psychologically-associated indices included the emotional component of the DHI, PSQI, BAI, and BDI. Based on our data, the BAI was significantly correlated with all components of the Sway indices. Additionally, the BDI was associated with the Sway indices involving standing on foam surface. Furthermore, PSQI scores were correlated with the Sway indices involving closed eyes. The emotional component of DHI was only significantly correlated with the ECI. The associations between anxiety, depression, sleep, and the emotional component of the DHI with certain components of the Sway indices were intriguing, and consideration of propensity scores may be beneficial for further analyses.
The propensity scores of the emotional component of the DHI and the results of many components of the balance test showed a significant association. When age, gender and height were accounted for, all components of the Sway indices demonstrated a significant association with the emotional component of the DHI. Moreover, the overall stability index showed a significant relationship with the emotional aspect of the DHI. Although after adjusting for confounders, only anteroposterior stability correlated significantly. There was no association between mediolateral stability and the emotional component of the DHI. While the relationships were significant, the scores were low and the correlation was weak.
There are other limitations to our study besides weak correlations. Firstly, there was no longitudinal observation. A 6 month or 1 year study would have been preferable for the assessment of changes in dizziness and balance for mTBI participants.
Secondly, anxiety or depression occurs more often in patients with post-traumatic stress disorder (PTSD) or PTSD with mTBI than in those who only had mTBI [22]. In our study, we did not evaluate PTSD and the problem of dizziness in mTBI with PTSD might be more serious than that in mTBI without PTSD.
Conclusion
In conclusion, the clinical application of the balance test for assessment of post-mTBI patients confirms emotional consequences of patients with dizziness. Additional information obtained through other tests and/or biomarkers [23] may be required for an adequate objective assessment of patient conditions.
Acknowledgements
We would like to express our appreciation to Taipei Medical University Hospital, Wan Fang Hospital, and Shuang-Ho Hospital for their helps in patient recruitment; all patients for their participation. This study was supported by grants from the Ministry of Science and Technology MOST 104-2314-B-038-031, Taipei Medical University TMU102-AE1-B27, TMU105-AE1-B03, Yuan's General Hospital 106YGH-TMU-09 and Taipei Medical University –Shuang Ho Hospital 103 TMU-SHH-24.
19676
References
- McInnes K (2017) Mild Traumatic Brain Injury (mTBI) and chronic cognitive impairment: A scoping review. PLoS One 12: e0174847.
- Teasdale G, Jennett B (1974) Assessment of coma and impaired consciousness. A practical scale. Lancet 2: 81-84.
- DeKosky ST, Ikonomovic MD, Gandy S (2010) Traumatic brain injury--football, warfare, and long-term effects. N Engl J Med 363: 1293-1296.
- Ma HP (2014) Recovery from sleep disturbance precedes that of depression and anxiety following mild traumatic brain injury: a 6-week follow-up study. BMJ Open 4: e004205.
- Katz DI, Cohen SI, Alexander MP (2006) Mild traumatic brain injury. Handb Clin Neurol 127: 131-156.
- Maskell F, Chiarelli P, Isles R (2006) Dizziness after traumatic brain injury: overview and measurement in the clinical setting. Brain Inj 20: 293-305.
- Kayabasi S (2015) Vestibular functions were found to be impaired in patients with moderate-to-severe obstructive sleep apnea. Laryngoscope 125: 1244-1248.
- Bazarian JJ (2009) Long-term neurologic outcomes after traumatic brain injury. J Head Trauma Rehabil 24: 439-451.
- Kaufman KR (2006) Comparison of subjective and objective measurements of balance disorders following traumatic brain injury. Med Eng Phys 28: 234-239.
- Akin FW, Murnane OD (2011) Head injury and blast exposure: vestibular consequences. Otolaryngol Clin North Am 44: 323-334.
- Shumway-Cook A, Woollacott MH (1995) Motor control: theory and practical applications. Lippincott Williams & Wilkins.
- Jacobson GP, Newman CW (1990) The development of the Dizziness Handicap Inventory. Arch Otolaryngol Head Neck Surg 116: 424-427.
- Poon DM (2004) Translation of the dizziness handicap inventory into Chinese, validation of it, and evaluation of the quality of life of patients with chronic dizziness. Ann Otol Rhinol Laryngol 113: 1006-1011.
- Beck AT (1988) An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol 56: 893-897.
- Beck AT (1996) Comparison of Beck Depression Inventories -IA and -II in psychiatric outpatients. J Pers Assess 67: 588-597.
- Buysse DJ (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28: 193-213.
- Zheng YP (1988) Applicability of the Chinese Beck Depression Inventory. Compr Psychiatry 29: 484-489.
- Tsai PS (2005) Psychometric evaluation of the Chinese version of the Pittsburgh Sleep Quality Index (CPSQI) in primary insomnia and control subjects. Qual Life Res 14: 1943-1952.
- Rubin DB (2007) The design versus the analysis of observational studies for causal effects: parallels with the design of randomized trials. Stat Med 26: 20-36.
- Han C, Kronmal R (2004) Box-Cox transformation of left-censored data with application to the analysis of coronary artery calcification and pharmacokinetic data. Stat Med 23: 3671-3679.
- Lin LF (2015) Balance function and sensory integration after mild traumatic brain injury. Brain Inj 29: 41-46.
- Pineau HA Marchand, Guay S (2015) Specificity of cognitive and behavioral complaints in post-traumatic stress disorder and mild traumatic brain injury. Behav Sci 5: 43-58.
- Chen KY (2015) Worsening of dizziness impairment is associated with BMX level in patients after mild traumatic brain injury. J Neurotrauma.