Ross O Downes*
General Surgery, Laparoscopy, Doctors Hospital, Nassau, Bahamas
*Corresponding Author:
Ross O Downes
General Surgery, Laparoscopy
Doctors Hospital, Nassau, Bahamas
Tel: 12423760893
Fax: 12426760036
Email: rossdownes@yahoo.com
Received date: July 13, 2016; Accepted date: September 20, 2016; Published date: September 26, 2016
Citation: Downes RO. Single Incision Laparoscopic Peptic Ulcer Repair with the Use Extracorporeal Mishra Knot: A Case Report. J Univer Surg. 2016, 4:3.
Keywords
Laparoscopy; Single incision; Single port; Peptic ulcer; Patch repair
Introduction
Peptic ulcer disease has a perforated rate of 2% to 10% with more than 70% of PUD-related deaths being attributed to perforation [1]. Complex surgical intervention for perforated duodenal ulcers has seen a revolution and replaced by more minimalist techniques [1]. The efficacy of gastric antisecretory medication and eradication of Helicobacter pylori have improved [1-3], thus primary repair of the perforation has become the standard of care. Laparoscopy offers the possibility of diagnosis as well as treatment with laparoscopic primary repair now becoming the gold standard due to less postoperative pain, faster recovery times, and shorter hospital stays [4-10].
With advances in laparoscopic instruments and skills, SILS has been developed and adaptable to many kinds of abdominal surgical procedures [5,6,8]. This approach offers better cosmetic results and considered scarless, less incisional pain, and the capability to convert to multiport surgery if required [5-8]. The decreased risk of incisional hernias with SILS remains unsubstantiated. Making a ‘‘knot’’ when using the SILS technique was more timeconsuming and challenging than when using the conventional multiport laparoscopy. There was limited movement with SILS, which lengthened the procedure. We report a case SILS peptic ulcer repair.
Case Presentation
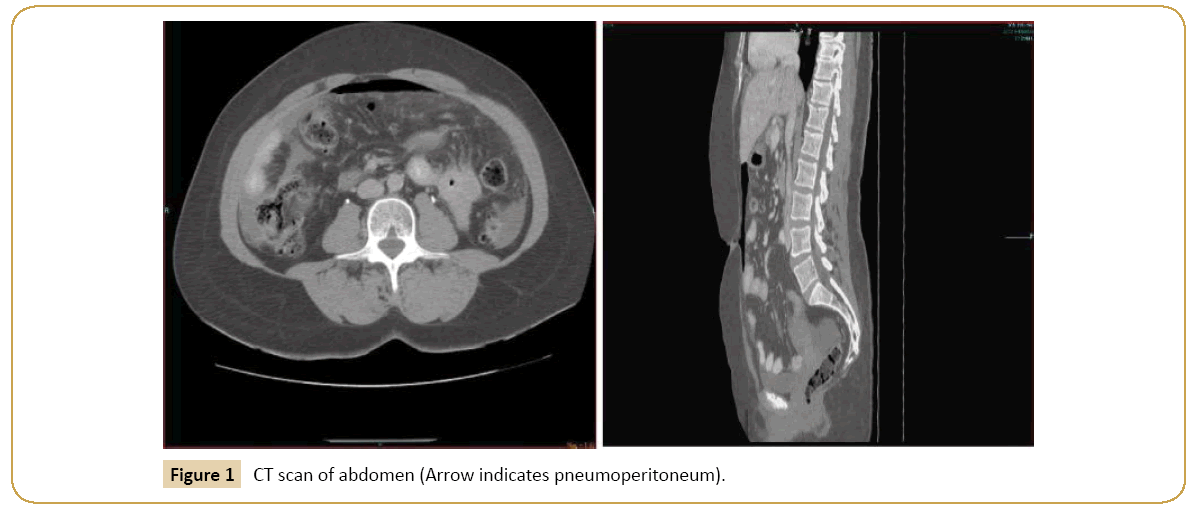
A 68-year-old woman with a body mass index of 30.3 kg/m2 was admitted to the emergency room for pain in the upper abdomen since few hours. She presented to the emergency department with a history of abdominal pain of 12 h duration that was gradual in onset, beginning epigastric then becoming generalized. The pain was associated with nausea and vomiting. She is known to have Addison’s disease and was recently placed on high dose steroids without gastric protection. Initial examination revealed a dehydrated patient with blood pressure of 130/84 and pulse rate of 54/min to 110/min. Her abdomen exhibited generalized peritonitis with increased intensity in epigastrium with guarding and rebound tenderness. Her laboratory results were all normal expect for an elevated White cell count of 17.1. Abdominal X-ray showed presence of sub-phrenic free air in the left upper quadrant and abdominal computed tomography scan confirmed pneumoperitoneum with free liquid in the hepatorenal (Morison’s) pouch and in the pelvic (Douglas’) pouch as well (Figure 1). A clinical diagnosis of perforated peptic ulcer disease was made and an emergency single port laparoscopic repair was advised. After a short period of resuscitation, the patient was taken to the operating room.
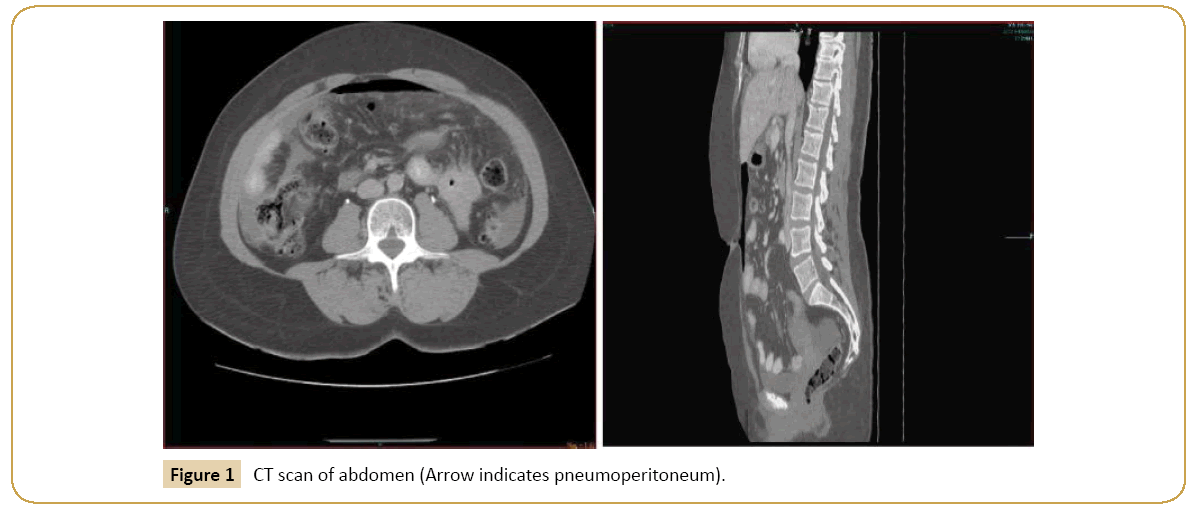
Figure 1: CT scan of abdomen (Arrow indicates pneumoperitoneum).
The patient was placed in a supine position with arms placed to the sides. A nasogastric tube was inserted, and prophylactic antibiotics were administered intravenously at the time of the incision. The surgeon was on the patient’s right and the assistant to the left of the patient.
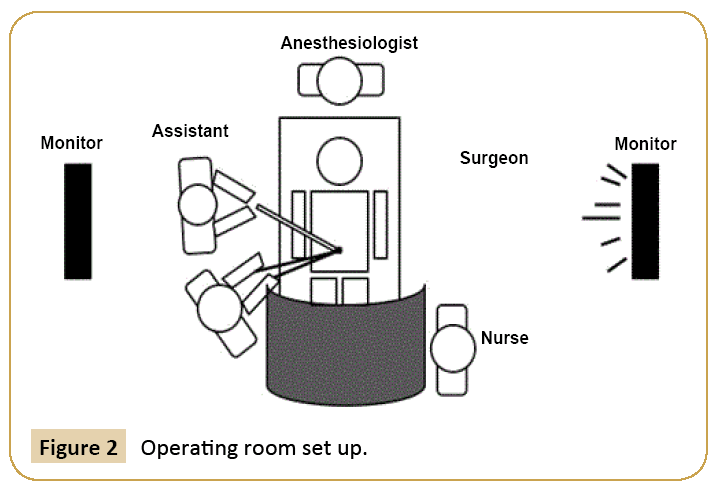
After the abdomen was entered, they both stood on the patient’s right with the assistant to the surgeon’s left. A television monitor and the insufflator system Karl Storz HD were placed to the left side of the patient. A 2.0 cm vertical trans-umbilical skin incision was made and directed down into the peritoneum. An S-retractor was introduced into the incision to facilitate the ease of port insertion. A special single incision port (GelPOINT™ port) was placed through the incision (Figure 2).
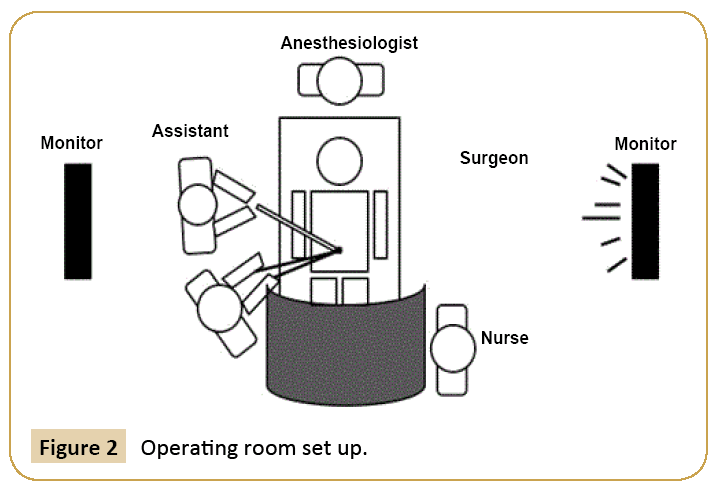
Figure 2: Operating room set up.
After pneumoperitoneum was established using 15 mmHg of carbon dioxide, a 10/12 mm trocar and 2 mm × 5 mm trocars were then inserted through the GelPOINT™ in a triangular fashion. The platform was positioned to place the 10/12 mm port at the 7 O’clock with other ports at 12 O’clock and 5 O’clock respectively. After port access had been achieved, the operating table was tilted to the right and was placed in the reverse Trendelenberg position at angles of 15° and 25° respectively. We used a standard length 10 mm 30° laparoscope placed in the 7 O’clock position. Exploration of the abdominal cavity showed the presence of free purulent liquid in the hepato-renal (Morison’s) pouch and in the pelvic (Douglas) pouch as well. A perforated 1 cm duodenal ulcer on the anterior surface of the first part of the duodenum, covered in part by fibrin was evidenced. We used standard disposable instruments for the procedure. There was bacteriological sampling of the free liquid and irrigation of the cavity with 4 L of warm saline solution. The duodenum ulcer was closed by 2/0 silk × 2 using Mishra’s knot technique. Omentoplasty was performed as well using 2/0 silk sutures. Mishra knot allowed us to quickly tie the sutures in the absence of the classic laparoscopic working triangulation established inside as in multi-trocar laparoscopy. Due to this patient’s ASA score of 4 we thought it imperative to place a drain. A 5 mm trocar was inserted in the right lower quadrant and a 10 F Jackson Pratt drain inserted and snaked along the right paracolic gutter to the Morison’s pouch. The instruments and trocar were removed under vision, and a meticulous closure of the umbilical fascia and loose approximation of the skin performed.
Proton pump inhibitors were intravenously injected during the fasting periods and then orally administered after starting a meal. When the patient complains of pain at the operation site, 50 mg of pethidine was injected intravenously. The patient resumed oral intake after passing the first flatus and was discharged when they were able to tolerate an oral diet. A Proton pump inhibitors was prescribed as long as she remained on steroids. The patient was prophylactically treated with triple therapy, including a proton pump inhibitor, amoxicillin, and clarithromycin.
Discussion
Laparoscopic surgery has become the standard of care for treatment in a variety of gastrointestinal pathologies. Laparoscopic surgery illustrated superior outcomes with respect to less postoperative pain, shorter hospital stays, better comesis, and early recovery [4-11]. Nathanson et al. [12] reported the first laparoscopic management of a perforated duodenal ulcer. Since then perforated duodenal ulcers have been managed laparoscopically with ulcer over-sewing and Graham’s patch.
One caveat is ulcers with diameter greater than 3 cm usually required formal resection [13], which could also be accomplished laparoscopically in skilled hands.
Single incision laparoscopic surgery or deduced port laparoscopic surgery offers the benefit of less parietal trauma. This can augment reduction in the acute stress response, which already is heightened in the patient with peritonitis. With advances in instrumentation and surgical experience, SILS has become more commonplace for complicated abdominal pathology. The list of surgical procedures been performed with SILS has steadily grown and has the added advantages of being virtually scarless, have less incisional pain, with less parietal trauma [14-17]. Another trocar can be easily inserted to perform multiport surgery [5- 8]. Conversion should never be seen as failure and should be prompt when required. Advances such as energy devices (LigaSure™, Harmonic); and dedicated single access platforms (e.g. GelPOINT™, TriPORT™, SILS, etc) have eliminated many of the hidden pitfalls earlier seen with limited resources.
Inline viewing is a concept, which evolved following the development of natural orifice transluminal endoscopic surgery. All instruments occupied one line of sight. Conventional laparoscopy advocates triangulation around a central optical instrument and thus SILS is thought to be contrary to this. Newer port systems (SILS™, GelPOINT™, TriPORT™) allow a combination of inline viewing and triangulation to accomplish the surgery. Thus clashing of instruments was minimized. These factors decreased the complexity and technical challenges of the operation.
We developed our SILS skills and techniques using as many standard instruments as possible. From our earlier accounts we were able to demonstrate that SILS was not more time consuming than multiport surgery [18]. Traditional laparoscopic skills were easily adaptable to this application. Thus, it shouldn’t take much time for surgeons to acclimate themselves to this new technique.
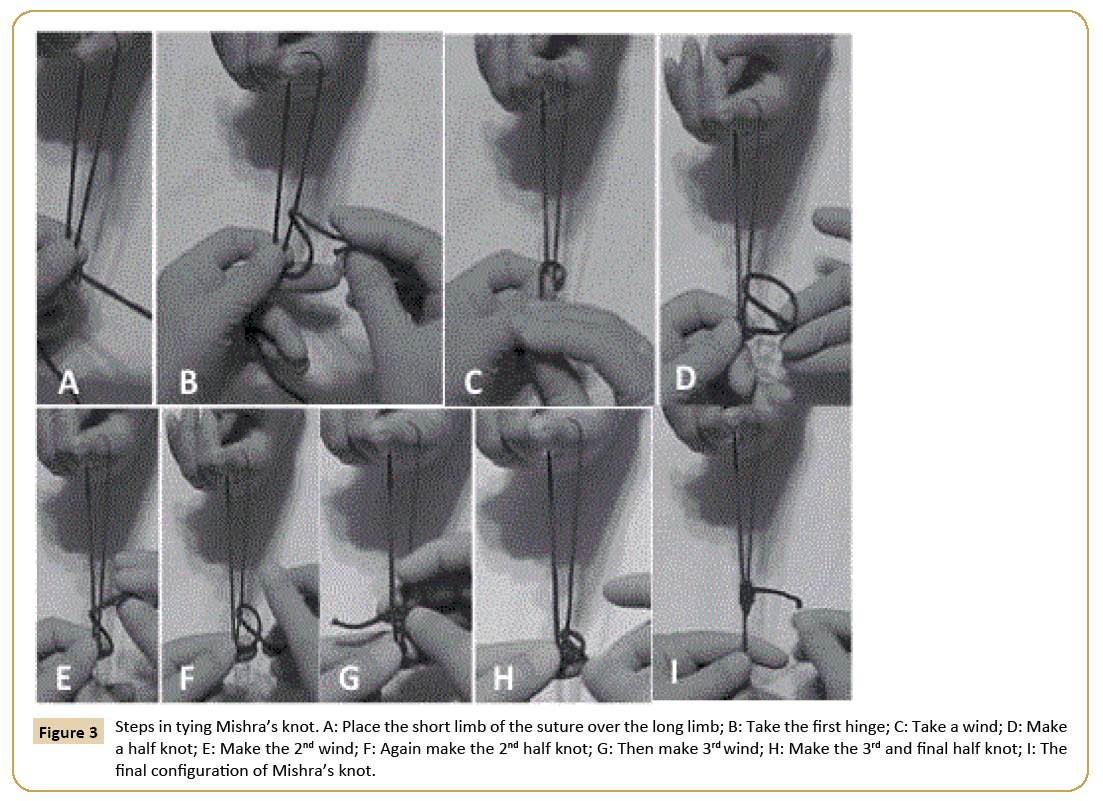
Even in the face of these advances, we found that the degree of triangulation was still not sufficient enough to comfortably suture. The Mishra’s knot was chosen as a simple and less time consuming technique. There are many variants of the extracorporeal slipknot. These knotting techniques are variations of turns around the axis or the number of reversed half hitches. The Mishra’s knot uses 3 half hitches in the completed knot. Extracorporeal Mishra's Knots can tolerate better distraction forces than other slipknot variants [20]. The major advantage in this technique is that any number of additional knots may be tied extracorporeally and pushed into the abdomen in a single maneuver (Figure 3). These knots slide down with equal ease, thus minimizing the risk of traction-induced trauma and of risk of stitches cutting through [19,20]. We used #0 silk for our repair.
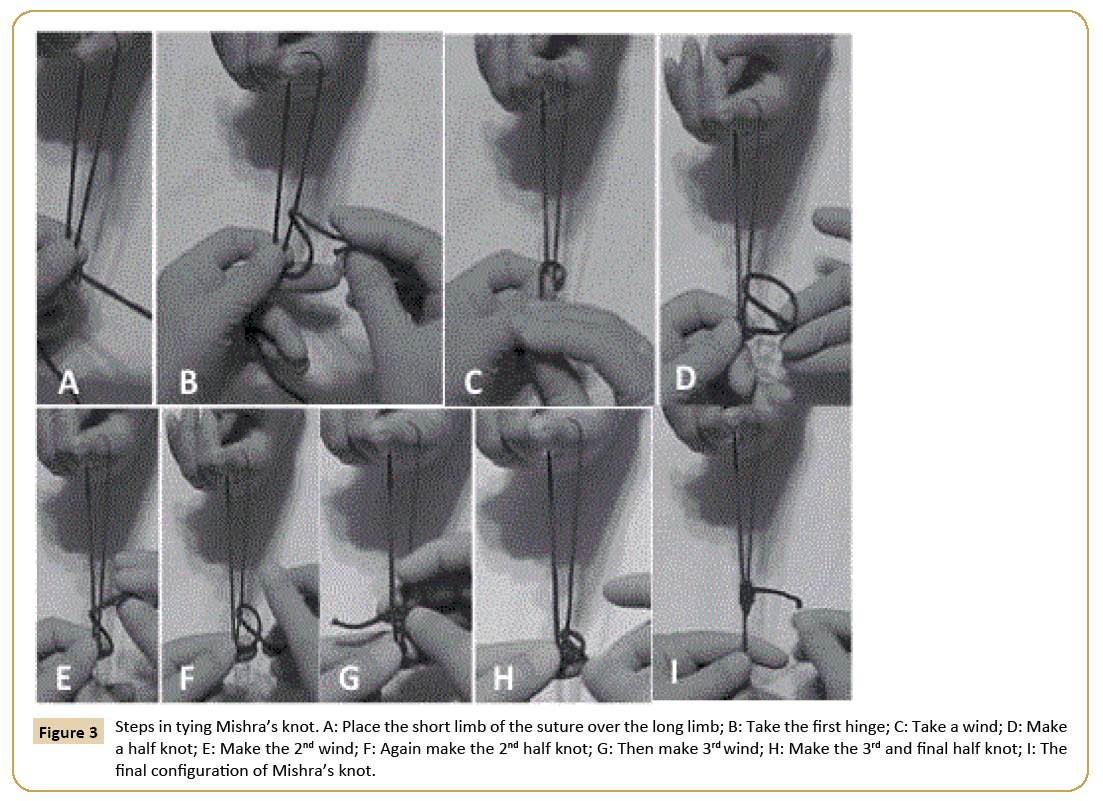
Figure 3: Steps in tying Mishra’s knot. A: Place the short limb of the suture over the long limb; B: Take the first hinge; C: Take a wind; D: Make a half knot; E: Make the 2nd wind; F: Again make the 2nd half knot; G: Then make 3rd wind; H: Make the 3rd and final half knot; I: The final configuration of Mishra’s knot.
Even if the surgeon was somewhat lacking in experience with SILS, moderate laparoscopic experience allows this technique to be performed without any challenges. Exposure of perforation site may occasional be inhibited by the liver bed or gallbladder, making the repair process more difficult [21-23]. The Mishra’s knot allowed us to use one hand to elevate the liver/gallbladder to expose the operative field, while we drove the suture through the tissues and delivered externally. This technique allowed us to confidently suture inflamed, friableness tissue in a satisfactory closure. To strengthen the weak point, we extended the omentum over the perforated site. As a result, this would reduce leakage at the perforation site or need for conversion to multiport surgery. We believed this patient required a drain because of her comorbidities. We placed a 5 mm port in the right lower quadrant and introduced a Jackson Pratt drain, which was then snaked along the right paracolic gutter. This port was placed in the lower abdominal crease for optimal cosmesis [24]. We believe placing the drain through the umbilicus has the risk for incisional hernia formation and increase wound infection rates, thus it is avoided. Although costly, we prefer to use a special single access platform. This avoids the direct puncture technique used by some authors that we believe directly increases port site hernia rates [20].
Conclusion
In conclusion, SILS for the treatment of a perforated duodenal ulcer using the Mishra’s knot technique can be performed successfully without technical challenges and does not require any specialized instruments. Extracorporeal Mishra's Knot and Tayside Knot can tolerate better distraction forces and thus have higher median Knot Quality Score scores compared with Roeder's knots.
17143
References
- Bertleff ME, Lange JF (2010) Perforated peptic ulcer disease: a review of history and treatment. Dig Surg 27: 161-169.
- Chung SC, Li AK (1997) Helicobacter pylori and peptic ulcer surgery. Br J Surg 84: 1489-1490.
- Hopkins RJ, Girardi LS, Turney EA (1996) Relationship between Helicobacter pylori eradication and reduced duodenal and gastriculcer recurrence: a review. Gastro J 110: 1244-1252.
- Kathouda N, Mouiel J (1998) Laparoscopic treatment of peptic ulcer disease. McGraw-Hill, New York, USA. pp. 123-130.
- Lunevicius R, Morkevicius M (2005) Systematic review comparing laparoscopic and open repair for perforated peptic ulcers. Br J Surg 92: 1195-1207.
- Bertleff ME, Halm JA, Bemelman WA, van der Ham AC, van der Harst E, et al. (2009) Randomized clinical trial of laparoscopic versus open repair of the perforated peptic ulcer: the LAMA Trial. World J Surg 33: 1368-1373.
- Siu WT, Leong HT, Law BB, Chau CH, Fung KH, et al. (2002) Laparoscopic repair for perforated peptic ulcer: a randomized controlled trial. Ann Surg 235: 313-319.
- Lau WY, Leung KL, Kwong KH, Davey IC, Robertson C, et al. (1996) A randomized study comparing laparoscopic versus open repair of perforated peptic ulcer using suture or sutureless technique. Ann Surg 224: 131-138.
- Lau H (2004) Laparoscopic repair of perforated peptic ulcer: a meta-analysis. SurgEndosc 18: 1013-1021.
- Bhogal RH, Athwal R, Durkin D, Deakin M, Cheruvu CV (2008) Comparison between open and laparoscopic repair of perforated peptic ulcer disease. World J Surg 32: 2371-2374.
- Nelson H, Sargent DJ, Wieand HS, Fleshman J, Anvari M (2004) A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 350: 2050-2059.
- Nathanson LK, Easter DW, Cushieri A (1990) Laparoscopic repair peritoneal toilet of perforated duodenal ulcer. SurgEndosc 4: 232-233.
- Montalvo-Javé EE, Corres-Sillas O, Athié-Gutiérrez C (2011) Factors associated with postoperative complications and mortality in perforated peptic ulcer. Cirugía Y Cirujanos 79: 141-148.
- Merchant AM, Cook MW, White BC, Davis SS, Sweeney JF, et al. (2009) Transumbilicalgelport access technique for performing single incision laparoscopic surgery (SILS). J GastrointestSurg 13: 159-162.
- Hong TH, You YK, Lee KH (2009) Transumbilical single-port laparoscopic cholecystectomy: scarless cholecystectomy. SurgEndosc 23: 1393-1397.
- Pappalepore N, Tursini S, Marino N, Lisi G, Lelli Chiesa P (2002) Transumbilical laparoscopy-assisted appendectomy (TULAA): a safe and useful alternative for uncomplicated appendicitis. Eur J PediatrSurg 12: 383-386.
- Castellucci SA, Curcillo PG, Ginsberg PC, Saba SC, Jaffe JS, et al. (2008) Single port access adrenalectomy. J Endourol 22: 1573-1576.
- Downes RO, Farlane M, Diggiss C, Iferenta J (2015) Single incision cholecystectomy using a clipless technique with LigaSure in a resource limited environment: The Bahamas experience. Int J Surg Case Rep 11: 104-109.
- Akindele RA, Fasanu AO, Mondal SC, Komolafe JO, Mishra RK (2014) Comparing Extracorporeal Knots in Laparoscopy using Knot and Loop Securities. World J Lap Surg 7: 28-32.
- Dapri G, Himpens J, Evola G, Marsili L, Cadière G (2012) Transumbilical single-access laparoscopic perforated gastric ulcer repair. Surg Inn 19: 130-133.
- Tan S, Wu G, Zhuang Q, Xi Q, Meng Q, et al. (2016) Laparoscopic versus open repair for perforated peptic ulcer: A meta analysis of randomized controlled trials. Int J Surg 5: 124-132.
- Alemrajabi M, Safari S, Tizmaghz A, Alemrajabi F, Shabestanipour G (2016) Laparoscopic Repair of Perforated Peptic Ulcer: Outcome and Associated Morbidity and Mortality. Electron Physician. 8: 2543-2545.
- Mishra RK (2009) Text book of Practical Laparoscopic Surgery. 3rd edn, Jaypee Brothers Medical Publishers, New Delhi, India.
- Sun JY, Sun DJ, Li XJ, Jiao K, Zhai ZW (2016) Laparoscopic treatment experience of severe acute pancreatitis complicated by peptic ulcer perforation. Eur Rev Med PharmacolSci 20: 285-290.