Sushil Kumar*, Amit Handa and Ravi Tiwari
Department of Neurosurgery, St. Stephens Hospital, Delhi, India
*Corresponding Author:
Sushil Kumar
Department of Neurosurgery, St. Stephens Hospital
Tis Hazari, Delhi-110054, India
Tel: 9810471753
Email: sushilneuro@rediffmail.com
Received Date: July 05, 2017; Accepted Date: July 19, 2017; Published Date: July 24, 2017
Citation: Kumar S, Handa A, Tiwari R (2017) Spontaneous Cervical Intramedullary Hematoma. J Neurol Neurosci Vol. 8 No. 4:210 DOI: 10.21767/2171-6625.1000210
Keywords
Intramedullary hemorrhage; Spontaneous; Magnetic Resonance Imaging (MRI)
Introduction
Spontaneous intramedullary hematoma is a rare entity. Spinal trauma is the most common cause of intramedullary hematoma. Early surgery is to be performed for pain relief and restoration of neurological functions [1-9]. Recently we came across a case of spontaneous cervical intramedullary hematoma with atypical pattern of presentation, hence being reported.
Case Report
A 35-year-old male patient was admitted to medicine department with complaints of sudden onset of tingling and weakness of right shoulder which progressed to involve the whole of right upper limb. Two days later the weakness spread to right lower limb and subsequently it involved left upper limb and lower limb. Two days prior to admission he developed urinary retention and fever. Also he complained of loss of warm and cold sensations on the left side of one-day duration. On examination he was afebrile, Pulse was 86/min and BP 110/80 mmHg, respiratory rate was 16/min and breath holding time was 27 seconds. On neurological examination there was hypertonia in the limbs more on right side. Power was grade I in all group of muscles on right side, gr IV on left side. All deep tendon jerks were exaggerated. Plantar was extensor on the right side. Sensations were impaired up to C5 level.
Investigations
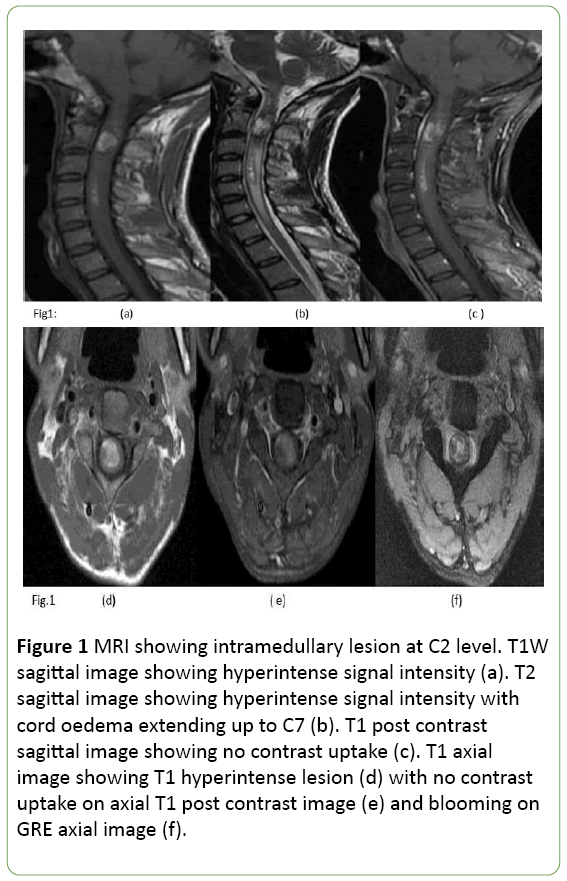
Hemogram, urinalysis was normal. Lumbar puncture revealed clear CSF without any cells. Protein was 37 mg% and sugar 72 mgm%. MRI revealed hyperintense lesion on T1WI and T2WI with peripheral hypointense rim, without any contrast uptake, (Figures 1a-1e). Gre sequence revealed blooming (1f). There were multiple small similar lesions opposite C4 and cord oedema extending up to C7.
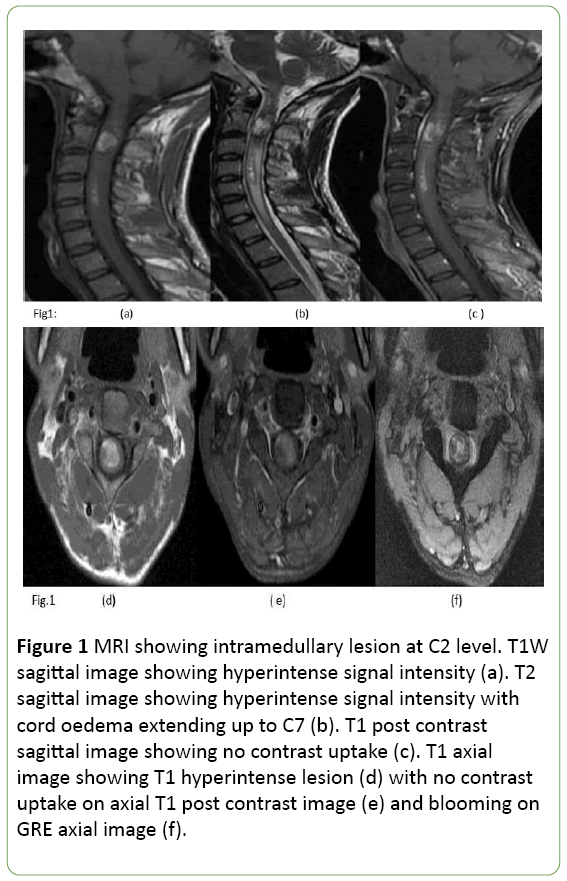
Figure 1: MRI showing intramedullary lesion at C2 level. T1W sagittal image showing hyperintense signal intensity (a). T2 sagittal image showing hyperintense signal intensity with cord oedema extending up to C7 (b). T1 post contrast sagittal image showing no contrast uptake (c). T1 axial image showing T1 hyperintense lesion (d) with no contrast uptake on axial T1 post contrast image (e) and blooming on GRE axial image (f).
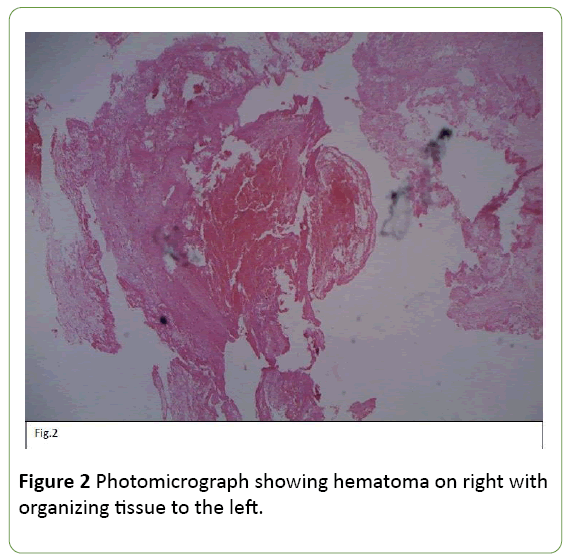
C2-C3 laminectomy revealed xanthochromia of right dorsal roots with cord bulge. Midline myelotomy revealed organized blood clot with pseudo-capsule adherent to cord tissue. Clot was removed gently and histopathology confirmed it to be organizing hemorrhage without any evidence of vascular malformation (Figure 2).
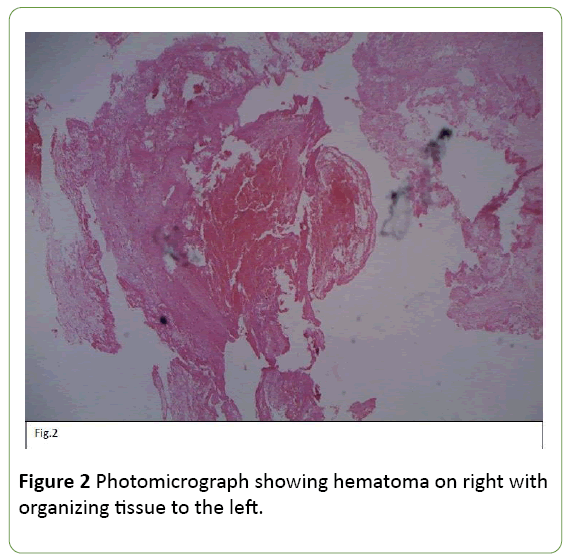
Figure 2: Photomicrograph showing hematoma on right with organizing tissue to the left.
Post-operatively he improved and could walk with support within 3 weeks of surgery and regained bladder control. 3 years after surgery his power has improved to grade V in all group of muscles except short muscles of right hand which are minimally weak.
Discussion
Spontaneous intramedullary hematoma is rare condition and there have been case reports only in the literature [1-6]. The most common etiology for this entity is spinal trauma, others being vascular malformation, cavernoma, tumor, syrinx, bleeding disorders and use of anticoagulants. In our patient none of the above etiologies could be attributed for the development of intramedullary hematoma, hence being labelled as idiopathic.
Patients may present with acute, subacute or chronic myelopathy. In our patient, though onset was acute but progression was slow and stepwise. Pain was conspicuously absent and bladder involvement was also late feature unlike that of a typical intramedullary lesion.
Other atypical presentation like mimicking a myocardial infarction or Brown-Sequard Syndrome have also been reported [9,10]. Surgical removal of the hematoma is the treatment of choice, whether course of hematoma is acute, subacute or chronic. Early surgery improves the prognosis.
Conclusion
Although patient reported to our department many days after the symptoms, yet we performed immediate surgery after coming to the diagnosis of intramedullary hematoma based on magnetic resonance imaging (MRI). In the long run our patient has shown good recovery although no recovery after evacuation of hematoma has been reported as well [6]. Most important prognostic factor is preoperative neurological status of the patient. Usually spinal angiography is not necessary if MRI suggests hemorrhage without any evidence of abnormal vessels [11]. We feel that high index of suspicion with accurate diagnosis by MRI and proper treatment can improve the prognosis.
20080
References
- Chao CH, Tsai TH, Huang TY, Lee KS, Hwang SL (2013) Idiopathic spontaneous intraspinal intramedullary hemorrhage: A report of two cases and literature review. ClinNeurolNeurosurg115: 1134-1136.
- Hwang JH, Sung JK, Hwang SK, Hamm IS, Park YM, et al. (2000) Spontaneous hematomyelia: Acase report.J Korean Neurosurg Soc. 29: 411-419.
- Lee DH, Choi YH (2014) Spontaneous intramedullary hematoma initially mimicking myocardial infarction. Am J Emerg Med 32: 1294-E3-1294-E4.
- Leep HA, Wijdicks EF (2008) Intramedullary spinal cord hemorrhage (hematomyelia). Rev Neurol Dis 6: E54-E61.
- Kumar S, Jaiswal AK, Singh H, Papo I (2005) Spontaneous intramedullary hematoma: A case report. J NeurolSci 49: 21-23
- Akpnar A, Celik B, Canbek I, Karaveliolu E (2016) Acute paraplegia due to thoracic hematomyelia. Case Rep Neurol Medp. 3.
- Choi BS, Lee S (2015) Idiopathic spontaneous intramedullary hemorrhage: A report of a rare case of repeated intramedullary hemorrhage with unknown etiology. Korean J Spine 12: 279-282.
- Leech RW, Pitha JV, Brumback RA (1991) Spontaneous haematomyelia: A necropsy study. J NeurolNeurosurg Psychiatry 54: 172-174.
- Toda H, Okamoto T, Nishida N, Yuba Y, Iwasaki K (2014) Idiopathic hematomyelia as a rare cause of epiconus syndrome. ClinNeurolNeurosurg125: 75-77.
- Madhusudhan BK, Mahendra JV, Rohan M, Srinivasa R ( 2014) Hematomyelia as a cause of brown-sequard's syndrome in a hypofibrinogenemic patient. Neurol India 62: 473-473.
- Karavelis A, Foroglou G, Petsanas A, Zarampoukas T (1996) Spinal cord dysfunction caused by non-traumatic hematomyelia. Spinal Cord 34: 268-271.