Research Article - (2022) Volume 16, Issue 2
Staphylococcal Scalded Skin Syndrome (SEPE): Diagnosis and Treatment: Outbreak Control Presented in a Neonatal Unit at a Clinic in Monteria Colombia 2021
Rafael Chica Polo1,
Hector Rafael Pineda Roman2,
Maria Jose soto Sanchez3,
Maria Jose Vertel Argel4,
Viviana Patricia Ibarra Ramirez5,
Andrea Eloisa Ruiz Quintero6,
Soraya Escudero Hoyos7,
Jiseth Paola Avilez Aleman8 and
Carlos Mauricio Vergara Lobo9*
1Neonatologist, Universidad de Buenos Aires, Argentina
2Neonatologist, Universidad de Buenos Aires, Argentina
3Third Year Pediatric Resident, Universidad del Sinu, Colombia
4General Physician, Universidad del Sinu, Colombia
5Pediatrician, Universidad de Carabobo, Aragua, Venezuela
6General Physician, Fundación Universitaria San Martin, Colombia
7Pediatric Intensivist, Pontificia Universidade Catolica do Rio Grande do Sul, Colombia
8Nurse Epidemiologist, Universidad de Cordoba, Colombia
9Pediatric Infectologist, Universidad de Buenos Aires, Argentina
*Correspondence:
Carlos Mauricio Vergara Lobo, Pediatric Infectologist, Universidad de Buenos Aires,
Argentina,
Email:
Received: 17-Dec-2021, Manuscript No. iphsj-21-12036;
Editor assigned: 19-Dec-2021, Pre QC No. Preqc no.12036;
Reviewed: 14-Feb-2022, QC No. Qc no.12036;
Revised: 19-Feb-2022, Manuscript No. iphsj-21-12036(R);
Published:
28-Feb-2022, DOI: 10.36648/1791-809X.16.2.916
Abstract
Objective: Staphylococcal scalded skin syndrome (SEPE) is a reaction to a staphylococcal skin infection in which blisters form on the skin due to a staphylococcal toxin, which is common in infants and children. In the following observational study, the appearance of cases of a staphylococcal scalded skin syndrome (SEPE) in a neonatal intensive care unit (epidemiological outbreak) associated with health care (IAAS) is analyzed and the importance of having an infection committee in the service-providing institutions for the containment of these events is highlighted.
Materials and Methods: We reported an outbreak of scalded skin staphylococcal syndrome, over a period of 4 weeks, in a neonatal intensive care unit in the city of Montería Colombia 2021, intervention measures by the institution’s infection committee to resolve the events presented.
Results: Eight patients with suggestive characteristics of SEPE were identified between May and June 2021. The germ responsible for these events was the resistant Staphylococcus Aureus methicillin, resistant to Clindamycin, sensitive to Vancomycin, Lenezolid, identified in the blister secretion in one of these patients.
Conclusions: Staphylococcal scalded skin syndrome is a common condition in childhood, mediated by toxin-producing strains of Staphylococcus aureus. The inappropriate approach can represent complications in the child in addition to an epidemiological outbreak, which is the appearance or increase of cases in a certain population. These cases occurred in a service provider entity (IAAS), it is of great importance to have the committee of infections and the participation of senior management is fundamental to the resolution of the appearance of adverse events presented in the institutions.
Keywords
Epidemiological outbreak; Infections associated with health care; Staphylococcal scalded skin syndrome; Intervention measures
Introduction
An epidemiological outbreak is defined as the occurrence in a community, region or institution of an excessive number of cases of a disease relative to the expected values (endemic) and related to each other by deriving from a common source or from a propagated source [1] that it can be classified as localized in cases that may be circumscribed; for example, to a hospital, a building, a school, a work centre or a housing area, as evidenced in this study or diffused if there is no such delimitation [2].
Staphylococcal scalded skin syndrome (SEPE or SSSS), formerly known as Ritter’s disease or neonatal pemphigus, is a potentially severe clinical syndrome mediated by toxins produced by certain strains of Staphylococcus aureus, with clinical manifestations of sudden onset with fever and irritability, and sensitive and even painful skin that includes a spectrum ranging from impetigo blistering localized form, to widespread involvement [3] that can occur with high indices, constituting an infection associated with health care (IAAS).
Infections Associated with Health Care (IAAS) are one of the main difficulties for the safety of the patient, affecting the quality of care, increased costs in institutions; hospital stay, new reinterventions, increased consumption of antibiotics, disability in patients, mortality, among others [4].
There are a number of risk factors for these infections to increase in incidence, mainly related to patient characteristics, such as in the case of children in a neonatal intensive care unit (Preterm newborns, low birth weight children, parenteral nutrition need, medical support, central catheters, use of broad spectrum antibiotics [5].
In health care institutions, there are surveillance and prevention measures for HAIs, with the aim of reducing the incidence of onset and mortality in hospitalized patients, which are supervised by the infection committee; scientific technical body at the institutional level, in charge of coordinating, executing education, promotion, prevention, surveillance strategies related to health care-associated infections and monitoring the emergence of antimicrobial resistance.
In a clinic in the city of Montería, Colombia, 8 cases of children with staphylococcal scald skin syndrome (SEPE) were reported in the neonatal intensive care unit (NICU), in a short period of 4 weeks, showing the diagnostic approach-therapeutic treatment provided, the behavior of this disease in newborns, the intervention measures used to control the outbreak of infection (IAAS), and the different areas of participation [6].
As for the pathophysiology of this syndrome, it is caused by the epidermiolytic toxins A and B of S. aureus. Any skin infectious focus (nasopharynx, conjunctiva, navel) or extra cutaneous can be the source of the disease by spreading the toxin through the blood to the skin. It is seen in the first years of life by the lack of anti-exfoliating antibodies and by the renal inability to quickly purify the toxin, as is the case of the newborn. Patients present with malaise, fever, irritability and then generalized erythematous macular rash, which in 1-2 days progresses to a painful scarlatiniform rash with flexure l and periorifice accentuation. Flaking begins 1 to 3 days later with the formation of prominent serous crusts and large flaccid blisters. The skin comes off easily with the pressure of a finger (Nicolski’s sign). Conjunctivitis may occur, but oral mucosa is never involved. In general, patients evolve favorably and mortality is less than 5%.
Materials and Methods
We performed an observational, descriptive intervention in neonatal patients with staphylococcal scalded skin syndrome, in the 4-week surveillance period, from 11-05-2021 to day 14-06- 2021. The data were collected, analyzed and later recorded in the program Microsoft Excel for registration.
Results
The institution in which the study was conducted is a maternal - child clinic located in the city of Montería, where about 2265 children are born annually and an average of 616 patients per year are admitted to the neonatal intensive care unit, representing an IT 6.1%. It has the presence of 16 neonatal beds, specialties such as neonatology, cardiology, pneumology, infectology, epidemiology, surgery, dermatology, nephrology, neurology.
The rate of device-related infections in this institution corresponds to 1) catheter-associated infection (ITS-AC) of 0.01%, 2) respirator-associated pneumonia (NAV) of 1%, 3) urinary tract associated infections (UTI-AC) 0.01%. An average of 23 deaths of neonates with weight less than 1000 gr, 11 deaths between the weight of 1000 to 1500 gr and more than 2000gr 17 deaths per year.
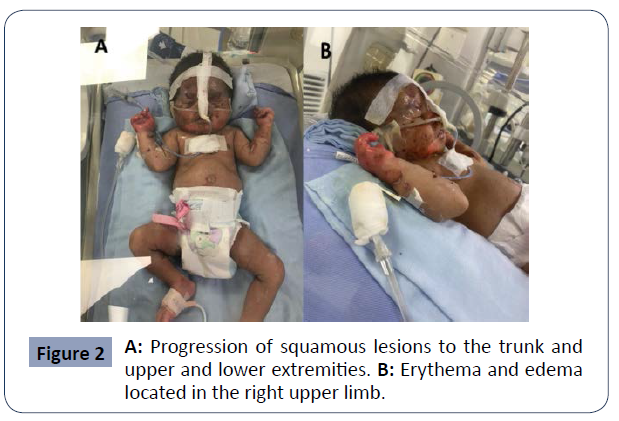
In the second week of May, patients with the following clinical characteristics began to be identified; children with blistering, crusty lesions, skin lesions with the appearance of burns, compromising the face as seen in Figure 1, however, lesions that progressed rapidly were also identified on the trunk and extremities, as seen in Figure 2 and 3. Inclusive, most of the patients showed systemic compromise, evolution requiring critical support and some had a fatal outcome. Eight children were identified (4 female and 4 male), with a 1: 1 ratio, the cases occurred in a period of 4 weeks between May and June 2021 (05- 11-2021 at day 06-14-2021). The median gestational age of these patients was 29 weeks and the average onset of symptoms was 34 days after birth.
Figure 1 Patient admitted with blistering and crusty lesions with
the appearance of a burn in the area of the face.
Figure 2 A: Progression of squamous lesions to the trunk and
upper and lower extremities. B: Erythema and edema
located in the right upper limb.
Figure 3 Peeling skin on the trunk and upper and lower
extremities secondary to progression of skin lesions.
87.5% of the children had received previous antibiotics due to the identification of maternal risk factors for sepsis in the newborn such as (PROM, chorioamnionitis, colonization by sgb) and ampicillin + gentamicin is the scheme used in these patients by the institution's protocols, coupled to national and international. 12.5% of patients had received a different antibiotic regimen due to the appearance of late sepsis after birth, a regimen consistent with the usual microbiota of the neonatal unit, the most widely used was Cefepime, Vancomycin. 12.5% were stable at the time of diagnosis and 87.5% had critical support.
37.5% died, which is equivalent to 3 deaths, 100% had used adequate antibiotics, the antibiotics initially proposed were, Vancomycin + cefepime, vancomycin + amikacin, Clindamycin as monotherapy. Subsequently, the infectology, epidemiology, and infection committee team optimized the antibiotic scheme in orientation to the antibiogram of a secretion culture of one of the bullous lesions of these patients, identifying staphylococcus aureus resistant to methicillicin, resistant to clindamycin, sensitive to linezolid, vancomycin, proposing the use of lenezolid as a toxin-inhibiting antibiotic in this condition mediated by toxins produced by staphylococcus aureus, controlling the pathology and therefore, avoiding death.
To control the outbreak, the following interventions were carried out
The institution has pediatric emergency services, 3 pediatric care rooms, 1 pediatric intensive care unit, 1 intermediate room, 1 neonatal intensive care unit, operating room, delivery room, and other areas for the care of adults, each area has the attention of different specialties. At the time of the appearance of SEPE cases in the neonatal unit, the alert was given in the institution, the competent body in charge of coordinating and executing the strategies to be used to contain the appearance of these infectious intercurrences was informed In the kids. The infection committee is made up of the nursing, epidemiology, neonatology, pediatric infectious disease, medical coordination team, and senior management.
Its functions include
• Carry out the Institutional Committee for the prevention, surveillance and control of IAAS with the participation of the different actors that allow the socialization of progress and results.
• Implement the national guidelines for the prevention, surveillance and control of HAI.
• Lead and participate in the formulation and implementation of institutional infection prevention and control initiatives.
• Carry out the implementation, monitoring and adherence of the technical annexes protocolized in the institutions.
• Periodically socialize the behavior of infections that require precautions and the percentage of adherence to it.
• Periodically socialize the behavior of infection outbreaks in the institution and the actions generated for containment.
The first strategy used to control the outbreak was to identify if there were reports of other cases of SEPE in other areas of the institution such as pediatric ward, pediatric intensive care unit, intermediate, among others, to identify if the cause was external to the unit neonatal, identifying the neonatal intensive care unit as the only place of reported cases. (Control of the chain of contagion).
As a second strategy, the request for cultures in these children was expanded to identify the causative germ of the reported cases because many of the antibiotic regimens used had no therapeutic response, managing to identify a methicillin-resistant Staphylococcus aureus, resistant to clindamycin, optimizing an effective scheme for the management of the disease and thus avoid mortality in children.
Finally, as a third strategy, standard measures in infection prevention were indicated, avoiding the appearance of new cases, which included:
• Hand higiene
• Use of gloves
• Use of personal protection elements (PPE)
• Care for the management of the environment, clothing, waste, solutions and equipment.
• Respiratory hygiene
• Cleaning, disinfection of biomedical devices and equipment. • Cleaning and disinfection of surfaces in the operating room, laundry room, delivery room, neonatal unit, etc.
• Culture of blisters in children (methicillin-resistant Staphylococcus aureus, clindamycin resistant
• Catheter change at 7 days in all patients
In general, the strategy was used to identify the cause and evaluate the behavior of human talent that would be allowing the appearance of this event, as seen in Tables 1 and 2.
| Causes of the Identified Event |
Brand (You cam check more than one) |
| |
Yes |
No |
| Brand (You can check more than one) |
|
|
| Outbreak due to a virulent microorganism |
|
|
| Outbreak due to a resistant microorganism |
|
|
| Changes in patient care |
|
|
| Due to the entry of residents or students |
|
|
| Change in the ratio of the number of nurses/patients |
|
|
| Change in the use of prophylactic or empirical antibiotics |
|
|
| Decreased adherence to prevention measures (bundles) |
|
|
| Related to a single health service or professional |
|
|
| Change in data handling |
|
|
| Changes in infection control personnel |
|
|
| Variations in the intensity of surveillance |
|
|
| Changes in the personnel who upload the data |
|
|
| Changes in definitions of hospital infection |
|
|
| Changes in laboratory procedures or in% of samples cultured |
|
|
| Changes in demographic characteristics of patients |
|
|
| Temporary increase in high-risk patients |
|
|
| Increased incidence of a particular pathology |
|
|
Table 1. Strategy implemented to identify the cause of the event.
| Measures Implemented to Control the Increase in Cases |
Brand (You cam check more than one) |
| |
Yes |
No |
| Assessment of infection control standards |
|
|
| Review of infection control standards |
|
|
| Identification of standards not met |
|
|
| Development of new standards |
|
|
| Application of insulation measures |
|
|
| Increase in the number of staff |
|
|
| Staff training |
|
|
| Review of laboratory practices |
|
|
| Data handling review |
|
|
| Identification of high-risk patients |
|
|
Table 2. Strategy used to evaluate the behavior of human talent that would be allowing the appearance of this event.
Discussion
As could be observed in the study, this pathology presents as a rapidly evolving toxic shock that can trigger death, as occurred in 37.5% of patients, therefore the approach must be timely, identifying the pathology, its possible cause to finally implement proper handling.
Antibiotics such as clindamycin, linezolid have the mechanism of action to act at the intracellular level of Staphylococcus aureus and act as inhibitors of toxins produced by this germ. Other antibiotics proposed by the literature is the use of vancomycin, so the doctor in charge of the patients must know the current resistance profiles of both community-acquired infections and those acquired at the hospital level, offering adequate management to each patient.
Therefore, authors such as Chacín and others, who present a case report of Staphylococcal Scalded Skin Syndrome in a younger infant, conclude that early evaluation and a timely diagnosis to start early parenteral antibiotics has shown to reduce complications, and guarantee the success of the procedure. Treatment; Cephalosporins and Betalactamase inhibitors are the most frequently used, obtaining good results, from the experience of our department the use of glycopeptides in view of the increased frequency of methicillin-resistant Staphylococcus aureus infections in our population has also proven to be a valid option in the treatment of this disease. In addition to antibiotics, there are also general measures such as controlling the environment where the patient is and improving the general conditions of the skin, in order to ensure the prompt recovery of turgor, pigmentation or gross appearance of the skin.
In turn, in its retrospective, descriptive and observational study, in which the medical records of patients diagnosed with SEPE seen between May 2000 and May 2010, treated in the Pediatric Dermatology Section of the Ramos Mejía Hospital, were reviewed, and between May 2005 and May 2010 in the Dermatology Service of the German Hospital, Losada et al. concluded that the timely recognition of SEPE and the early initiation of treatment with antibiotics resistant to ß-lactamases reduces the extent of the condition. On the contrary, the use of corticosteroids could aggravate it. The clinical evolution of SEPE is very good in pediatric age and does not leave sequelae or scars.
For its part, thorough hand washing continues to be the fundamental pillar to prevent the spread of infections at the nosocomial level and the rational use of antibiotics in all institutions should be a priority, the infection committee, the team in charge of caring for patients must have the support of senior management to be able to identify and implement measures to prevent events that put patients' lives at risk, unnecessarily high consumption of antibiotics, increased hospital stays, increased costs , as well as resistance profiles difficult to handle.
The institution must constantly update the protocols with the personnel in charge of health care in order to reduce the incidence of infections associated with health care, hand washing, use and care of catheters, preventive measures in pneumonia associated with the ventilator, while the microbiology laboratory has to periodically update the resistance profiles of the institution so that the infection committee offers a rational use of antibiotics through its doctors to each pathology to present.
Conclusion
Staphylococcal skin scald syndrome is a rare skin disease that is clinically manifested by the presence of erythema, blisters and scaling, as well as pain to the touch in the patient, which is a frequent pathology in childhood, mediated by toxin-producing strains of staphylococcus aureus, so its inappropriate approach can represent complications in the child and in some cases cause mortality rates.
Regarding the treatment established for this, clindamycin and linezolid are antibiotics with activity against staphylococcus aureus, which act by binding the 50s subunits of bacterial ribosomes, inhibiting the synthesis of toxins, which is why they are useful in strains that produce these.
At the same time, periodic updates of protocols for surveillance and prevention of infections related to health care such as hand washing, device care (catheter, endotracheal tubes, bladder catheters) and the constant participation of senior management on issues are essential. of patient care by providing the necessary tools to prevent infections, safeguarding their integrity and reducing unnecessary expenses to the institution.
REFERENCES
- Outbreak investigation (2021) Approach to nosocomial infections. Bogotá Mayor's Office.
Google Scholar
- García GJJ (2002) Basis for the epidemiological study of an outbreak. Rev Mex Pediatr 69: 208-211.
Indexed at, Google Scholar, Crossref
- Sánchez-Saldaña LA (2020) Síndrome Estafilocócico de la piel escaldada. Dermatol Perú 30.
Google Scholar, Crossref
- Promotion and Prevention Directorate (2018) Programa de prevención, vigilancia y control de infecciones asociadas a la atención en salud-IAAS y la resistencia antimicrobiana. Ministry of Health and Social Protection.
Google Scholar, Crossref
- Chacín M, Bermúdez V, Bucete B, Rojas J (2018) Staphylococcal Scalded Skin Syndrome In A Young Infant: A Case Report. Venezuelam Archives Pharmacol Ther 37.
Google Scholar
- Sanclemente L, Kamelia María LSK, Alexia DM, Javier SJ, Verónica L, et al. (2011) Staphylococcal scalded skin syndrome (SSSS). Our 10-year experience. Dermatol Argent 17: 193-197.
Google Scholar, Crossref
Citation: Lobo CMV (2022) Staphylococcal Scalded Skin Syndrome (SEPE): Diagnosis and Treatment: Outbreak Control Presented in a Neonatal Unit at a Clinic in Monteria Colombia 2021. Health Sci J. Vol. 16 No. 2:916.