Case Report - (2023) Volume 17, Issue 8
Stress Related Necrotizing Ulcerative Gingivitis: A Case Report
Boubdir Safaa*,
EL Kholti Wafa,
Rhalimi Loubna and
Kissa Jamila
Department of Periodontics, University of Hassan II of Casablanca, Casablanca, Morocco
*Correspondence:
Boubdir Safaa, Department of Periodontics, University of Hassan II of Casablanca, Casablanca,
Morocco,
Email:
Received: 21-Jun-2023, Manuscript No. IPHSJ-23-14053;
Editor assigned: 26-Jun-2023, Pre QC No. IPHSJ-23-14053 (PQ);
Reviewed: 10-Jul-2023, QC No. IPHSJ-23-14053;
Revised: 22-Aug-2023, Manuscript No. IPHSJ-23-14053 (R);
Published:
19-Sep-2023, DOI: 10.36648/1791-809X. 17.9.1056
Abstract
The basic form of necrotizing periodontal disease is
Necrotizing Ulcerative Gingivitis (NUG). It has a rapid and
aggressive start and a complex aetiology that includes
stress, nutritional deficits and immune system dysfunctions.
NUG is distinguished clinically by inflammatory interdental
papillae, gingival necrosis, gingival discomfort, bleeding and
halitosis. The therapy of NUG comprised a first phase that
should be administered immediately in order to halt disease
progression and regulate the patient's discomfort and pain.
The second phase of the preexisting condition's treatment,
followed by surgical correction of the disease's sequelae.
Following the completion of active therapy, a periodontal
maintenance programme was created. The purpose of this
case report is to present the method to diagnosis and
treatment of NUG in a male patient with no systemic
disease, as well as the likely mechanism of pathogenesis of
predisposing factors implicated.
Keywords
Diagnosis; Necrotizing Periodontal Diseases
(NPD); Necrotizing Ulcerative Gingivitis (NUG); Treatment;
Stress
Introduction
Necrotizing periodontitis is one of the most severe
inflammatory reactions of periodontal tissues caused by dental
plaque. These disorders have a quick, acute onset, as well as a
multiple and complex aetiology. Necrotizing Ulcerative Gingivitis
(NUG) is a classic example of a necrotizing periodontal disease. It
is a common kind of periodontal disease caused by bacterial
infection in people who have certain underlying risk factors
(poor dental hygiene, smoking, stress, poor nutrition, reduced
immunological function, etc).
Clinically, NUG is distinguished by high dental plaque
accumulation, quick onset of gingival discomfort, interdental
gingival necrosis, bleeding and tissue necrosis. It is also linked to
fever and lymphadenopathy. During World War II, NUG was
observed among military soldiers due to a combination of risk
factors (poor oral hygiene, significant psychological stress and
inadequate diet). NUG is seen in people with immunecompromised conditions after the conflict. According to current
data, the prevalence of NUG ranges from 6.7% in Chilean
students aged 12 to 21 years to 0.11% in the British armed
forces [1].
The periodontal therapy of NUG is aimed at remission of the
acute process's signs and symptoms, including the removal of
the local causative factors and comfort of the painful condition.
The purpose of this case study is to describe a localised form of
NUG's therapy strategy and successful outcomes.
Case Presentation
In June 2022, a 22-year-old male patient presented to the
department of periodontology, faculty of dentistry, university of
Hassan II of Casablanca, Morocco, with painful gingival
inflammation that had been present for three days. The patient
complained of sudden intense discomfort and gingival bleeding.
We observed a slender, feverish, fatigued male during the
clinical examination, but no adenopathy on the cervical ganglia
area. He was a nonsmoker with poor plaque management and
no parafunction. There was no other significant medical history
or recognised allergies [2].
Clinical findings and diagnostic assessment
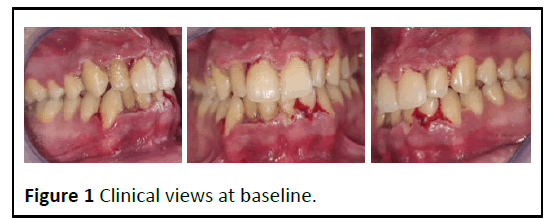
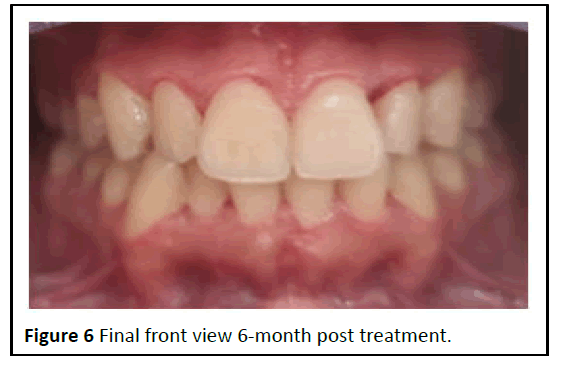
Clinical examination indicated a pseudo membrane formation
along the gingival edges, as well as headless ulcerated papillae,
particularly on the upper anterior teeth and lower central
incisors (Figure 1). In rare cases, the papilla did not completely
fill the interproximal area. On the teeth surfaces, there was a
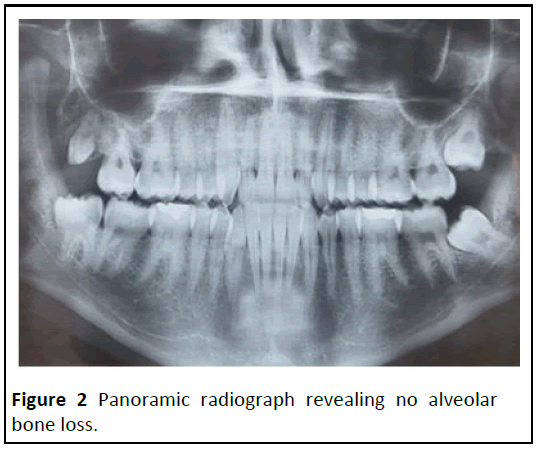
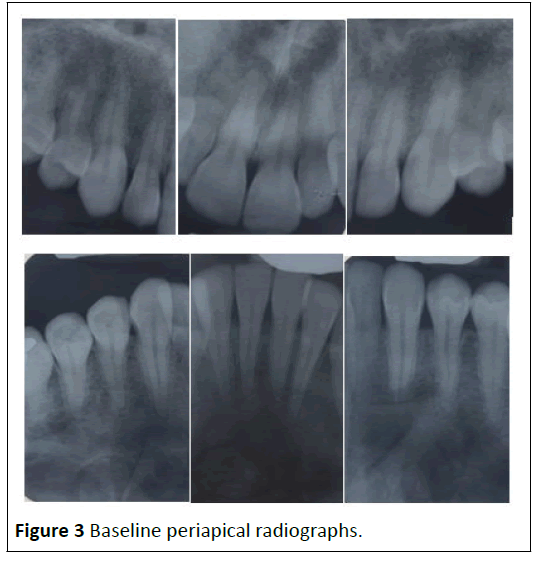
generalised and extensive deposit of dental plaque. X-rays
revealed periodontal ligament expansion in the lower central
incisors but no alveolar bone loss (Figures 2 and 3). During the
physical examination, no systemic condition that could
predispose the patient to NUG was discovered. However, the
patient indicated that he had been under considerable stress
and psychological pressure at school as a result of a period of
academic probation. Based on the clinical data obtained at the
examination, NUG was diagnosed [3].
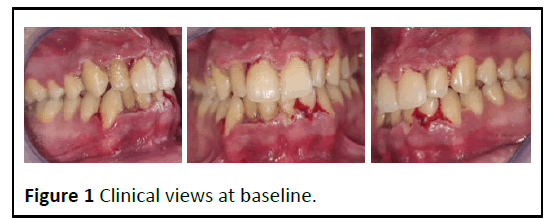
Figure 1: Clinical views at baseline.
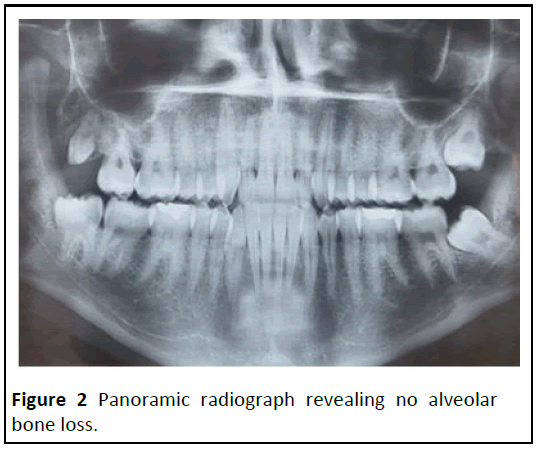
Figure 2: Panoramic radiograph revealing no alveolar
bone loss.
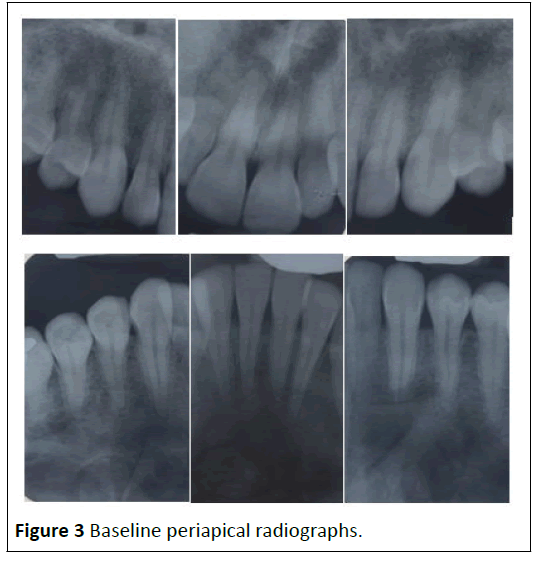
Figure 3: Baseline periapical radiographs.
Therapeutic approach
The primary clinical treatment goal was to shorten the acute
period of NUG. Using sterile swabs and appropriate ultrasonic
supragingival debridement, we administered diluted hydrogen
peroxide to the necrotic pseudomembranous lesions. The
patient was given an oral antibiotic (250 mg metronidazole
every 8 hours for 7 days) as well as an oral mouth rinse (0.12%
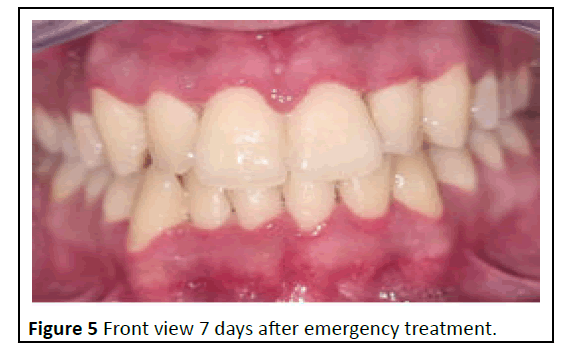
chlorhexidine twice day for 10 days). The gingiva condition was
assessed two days and seven days after therapy. The clinical
examination revealed that the patient's condition was improving, with less erythema and swelling. A subgingival
debridement was performed two days following the emergency
therapy [4].
A reinforcement of the oral hygiene instructions was realised
in order to change the patient's oral hygiene behaviour with
regular and effective oral hygiene habits maintenance. Within
two weeks, the inflammatory clinical state was corrected and
periodontal health was noted. The patient was seen once a
month on a regular basis. There was no tissue squealing, thus
the evolution was positive (Figures 4-6) [5].

Figure 4: Clinical views 2 days after emergency treatment.
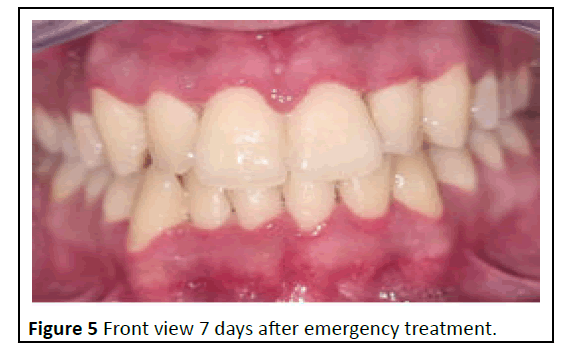
Figure 5: Front view 7 days after emergency treatment.
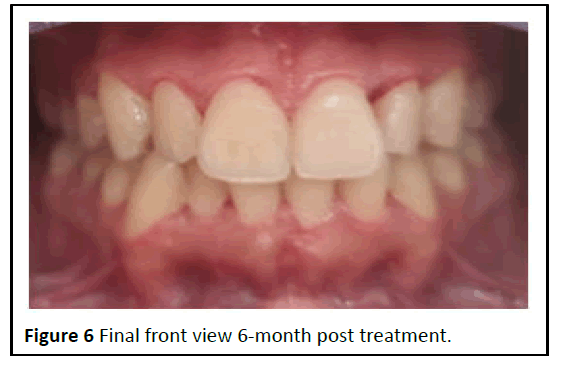
Figure 6: Final front view 6-month post treatment.
Results and Discussion
Necrotizing ulcerative gingivitis is limited to the gingival tissue
and does not impact other periodontal tissues. The World
Health Organisation (WHO) designated NUG, along with
Necrotizing Ulcerative Periodontitis (NUP) and linear gingival
erythema, as periodontal disease-related diseases in HIVpositive
patients in 1993. Later, according to the American
academy of periodontology's 1999 categorization scheme, NUG
was classed as necrotizing periodontal disease (NUP).
Necrotizing Gingivitis (NG), Necrotizing Periodontitis (NP) and Necrotizing Stomatitis (NS) are severe inflammatory periodontal
diseases caused by bacterial infection in patients who have
certain risk factors (poor dental hygiene, smoking, stress, poor
diet, reduced immunological function and so on [6].
In the present case report, systemic clinical symptoms indicate
the less severity of the case. The typically histopathological
aspect of NUG is described on four different layers from the
most superficial to the deepest layers of the lesion:
• The bacterial area with a superficial fibrous mesh composed of
degenerated epithelial cells, leukocytes, cellular rests and a
wide variety of bacterial cells, including rods, fusiforms and
spirochetes.
• The neutrophil rich zone composed of a high number of
leukocytes, especially neutrophils and numerous spirochetes
of different sizes and other bacterial morphotypes located
between the host cells.
• The necrotic zone, containing disintegrated cells, together with
medium and large size spirochetes and fusiform bacteria.
• The spirochetal infiltration zone, where the tissue components
are adequately preserved but are infiltrated with large and
medium size spirochetes. Other bacterial morphotypes are not
found [7].
The diagnosis of NUG can be confused with some viral
infections (acute herpetic gingivostomatitis and infectious
mononucleosis…), bacterial infections (gonococcal or
streptococcal gingivitis) and also some mucocutaneous
conditions (desquamative gingivitis, multiform erythema,
pemphigus vulgaris). The risk factors play a significant role in
NUG by suppressing the host immune response and enhancing
bacterial pathogenicity. Psychological stress, low sleep and poor
diet are among these variables. In this case, two NUG risk factors
were suspected: Poor diet and psychological stress caused by
tests. The proposed mechanisms to explain the relationship
between psychological stress and NUG are based on reductions
in gingival microcirculation and salivary flow, as well as increases
in adrenocortical secretions, which are associated with changes
in the function of polymorphonuclear leukocytes and
lymphocytes. NUG therapy modalities are organised in three
steps: First, treat the acute phase; second, treat the previous
condition; and last, treat the illness sequelae [8]. Then comes
the supportive or maintenance phase. The goal of acute phase
treatment is to stop the disease process and tissue
deterioration, as well as to regulate the patient's general sense
of discomfort and pain, which may interfere with nutrition and
oral hygiene practises. These goals can be met through careful
superficial ultrasonic debridement and chemical deterrence of
necrotic lesions with oxygen-releasing chemicals, referred to as
"local oxygen therapy." Metronidazole (250 mg, every 8 hours) is
the primary choice of medicine for systemic antimicrobials due
to its active action against stringent anaerobes. Other systemic
medications with acceptable results in the literature include
penicillin, tetracyclines, clindamycin, amoxicillin or amoxicillin
with clavulanate. Locally delivered antimicrobials are not
recommended for the huge number of bacteria present in
tissues, where the local medication will not acquire acceptable
concentrations. Antifungal drugs are especially useful in
immunocompromised patients receiving antibiotics [9]. Once the acute phase is under control, treatment of the previous
chronic illness, such as chronic gingivitis, should begin, which
may include professional prophylaxis and/or scaling and root
planing. Instructions on oral hygiene and motivation should be
strengthened. Overhanging restorations and interdental open
areas, for example, should be addressed as predisposing local
variables. Systemic risk factors such as smoking, insufficient
sleep and stress reduction should be addressed and controlled.
Treatment success is dependent not only on biofilm control
approaches, but also on patient behaviour change and
adherence to treatment regimens. In the current clinical
example, patient compliance was a beneficial aspect in the
clinical situation's favourable evolution. He has good plaque
control, follows control appointments and is still in the
maintenance phase [10].
Conclusion
NUG is a form of periodontal necrotizing disease. Different
clinical and systemic symptom and risk factors are behind the
diagnostic assessment. Treatment should be organized on
successive stages and the acute phase treatment should be
provided immediately to prevent sequelae and craters in soft
tissues that could lead to new relapses. Finally, a good
compliance with the oral hygiene practices and maintenance are
the guarantee of successful outcomes.
Conflict of Interest
The authors declare that they have no competing interest.
References
- Ardila CM, Guzman IC (2016) Association of P orphyromonas gingivalis with high levels of stress-induced hormone cortisol in chronic periodontitis patients. J Investig Clin Dent 7: 361-367.
[Crossref] [Google Scholar] [PubMed]
- Dufty J, Gkranias N, Petrie A, McCormick R, Elmer T et al. (2017) Prevalence and treatment of Necrotizing Ulcerative Gingivitis (NUG) in the British armed forces: A case-control study. Clin Oral Investig 21: 1935-1944.
[Crossref] [Google Scholar] [PubMed]
- Folayan MO (2004) The epidemiology, etiology and pathophysiology of acute necrotizing ulcerative gingivitis associated with malnutrition. J Contemp Dent Pract 5: 28-41.
[Google Scholar] [PubMed]
- Herrera D, Alonso B, de Arriba L, Santa Cruz I, Serrano C et al. (2014) Acute periodontal lesions. Periodontol 65: 149-177.
[Crossref] [Google Scholar] [PubMed]
- Holmstrup P, Westergaard J (2003) Necrotizing periodontal disease. Clinical Periodontology and Implant dentistry, Oxford: Blackwell, pp. 243-259.
[Google Scholar]
- Holmstrup P, Plemons J, Meyle J (2018) Non-plaque-induced gingival diseases. J Clin Periodontol 45: 28-43.
[Crossref] [Google Scholar] [PubMed]
- Hu J, Kent P, Lennon JM, Logan LK (2015) Acute necrotising ulcerative gingivitis in an immunocompromised young adult. BMJ Case Rep 2015: bcr2015211092.
[Crossref] [Google Scholar] [PubMed]
- Lopez R, Fernandez O, Jara G, Aelum VB (2002) Epidemiology of necrotizing ulcerative gingival lesions in adolescents. J Periodontal Res 37: 439-444.
[Crossref] [Google Scholar] [PubMed]
- Malek R, Gharibi A, Khlil N (2017) Necrotizing ulcerative gingivitis. Contemp Clin Dent 8: 496.
[Crossref] [Google Scholar] [PubMed]
- Martos J, Ahn Pinto KV, Feijo Miguelis TM, Cavalcanti MC, Cesar Neto JB (2019) Clinical treatment of necrotizing ulcerative gingivitis: A case report with 10-year follow-up. Gen Dent 67: 62-65.
[Google Scholar] [PubMed]
Citation: Safaa B, Kholti W, Loubna R, Jamila K (2023) Stress Related Necrotizing Ulcerative Gingivitis: A Case Report. J Health Sci. Vol. 17 No. 09
1056.