Case Report - (2017) Volume 9, Issue 1
Successful Treatment of Lung Abscess with Pigtailed Catheter after Failure with
Antibiotics and Surgical Debridement
Dalvir Gill1*, Kamalpreet Mann2, Sharanpreet Kaur1, Vanessa Goyes Ruiz1, Ryan Dean1 and Samana Zaidi1
1Department of Internal Medicine, SUNY Upstate Medical University, 750 East Adams Street, Syracuse, NY, USA
2The University of Medicine and Health Sciences, Basseterre, St. Kitts
- *Corresponding Author:
- Dalvir Gill
Department of Internal Medicine
SUNY Upstate Medical University, 750 East Adams Street, Syracuse, NY, USA
Tel: 3158028394
E-mail: gillda@upstate.edu
Received date: January 23, 2017; Accepted date: February 06, 2017; Published date: February 13, 2017
Citation: Gill D, Mann K, Kaur S, Ruiz VG, Dean R, et al. Successful Treatment of Lung Abscess with Pigtailed Catheter after Failure with Antibiotics and Surgical Debridement. Arch Med. 2017, 9:1. doi: 10.21767/1989-5216.1000193
Copyright: © 2017 Gill D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Necrotizing pneumonia is a rare complication of pneumonia as it could lead to lung abscess, septic shock and respiratory failure. 80%-90% of lung abscess are successfully treated with antibiotics, however surgical intervention is required in refractory cases1. Mortality rates are high despite thoracotomy and lobectomy, ranging from 15%-20% [1]. An alternative therapy is percutaneous tube drainage.
Keywords
Pneumonia; Antibiotics; Pulmonary gangrene
Case Report
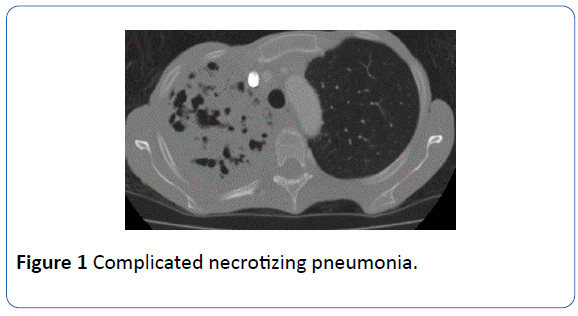
We present a summary of events in a case of complicated necrotizing pneumonia (Figure 1). Our patient is a 58-year-old female with past medical history significant for COPD, who initially presented with productive cough, fever, chills, and shortness of breath. Her vitals remained stable and physical exam was remarkable for dullness on percussion and decreased breath signs of the right upper lung fields. Chest X-ray showed right apical consolidation and follow up CT thorax showed large cavitary mass that involved the upper lobe of the right lung and the superior segment of the right lower lobe.
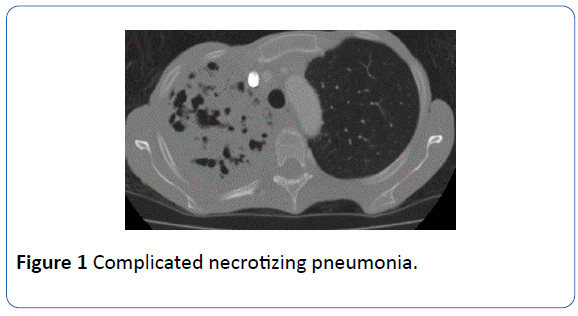
Figure 1: Complicated necrotizing pneumonia.
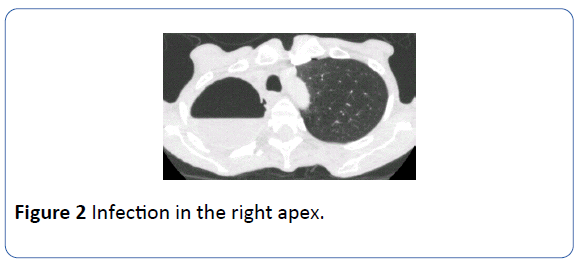
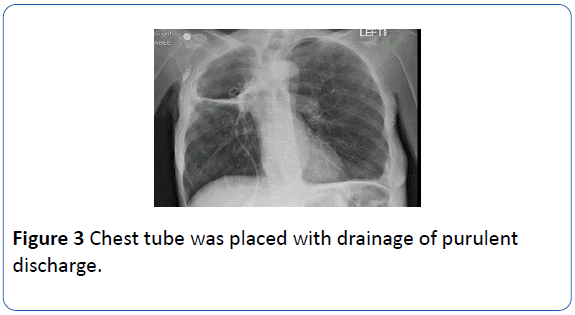
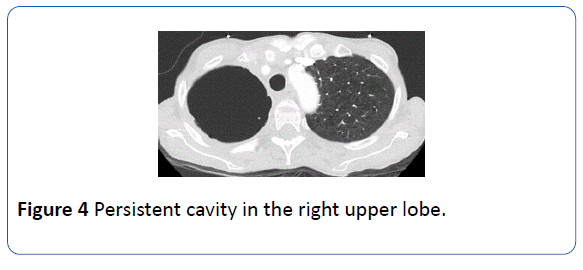
Bronchoscopy with biopsy was consistent with necrotizing pneumonia and patient was treated with IV antibiotics. However her symptoms did not resolve and surgery was consulted. Patient got decortication of the right upper lobe. Nonetheless, surgical intervention did not help and she was readmitted. Compared with prior CT thorax, now there was a substantial complex fluid within the cavity, suspicious for a superimposed infection in the right apex (Figure 2). She was started on IV antibiotics again, but her symptoms persisted. Chest tube was placed with drainage of purulent discharge (Figure 3). The cultures grew pan-sensitive Klebsiella pneumoniae, which was treated with antibiotics. Repeat CT thorax in 2 months showed persistent cavity in the right upper lobe but the air/fluid level had resolved (Figure 4) [1].
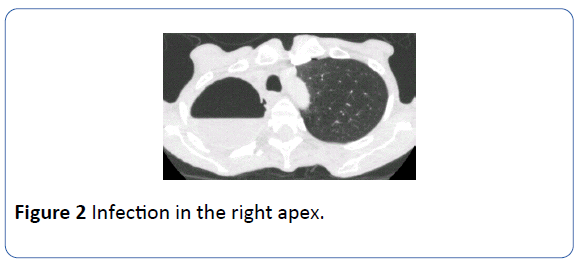
Figure 2: Infection in the right apex.
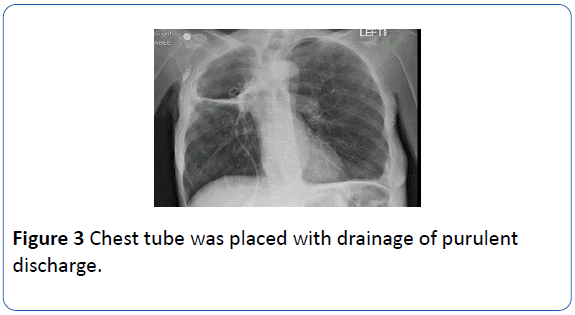
Figure 3: Chest tube was placed with drainage of purulent discharge.
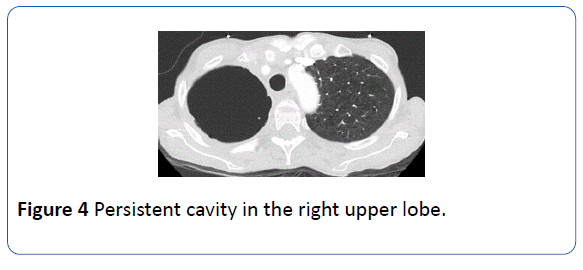
Figure 4: Persistent cavity in the right upper lobe.
Necrotizing pneumonia is a complication of pneumonia and it could be fatal if not treated appropriately. Klebsiella pneumoniae is a common cause of necrotizing pneumonia and is often complicated by lung abscess, which usually appears as cavities. One case series demonstrated multiple small cavities ranging from 1 mm to 3 cm in 48% patients by CT thorax [2]. The most feared complication is massive pulmonary gangrene, which could develop from lung abscess from Klebsiella pneumoniae, and it can destroy an entire section of a lung. Although pulmonary gangrene is a rare condition, but over one-half of cases are attributable to Klebsiella pneumonia [2]. On imaging, pulmonary gangrene starts with lung consolidation, which then leads to multiple small cavities that coalesce into one large cavity. After a 10 to 14 days period of conservative medical therapy without clinical improvement, percutaneous tube drainage should be considered.
Necrotizing pneumonia secondary to Klebsiella pneumoniae could lead to fatal pulmonary gangrene. Percutaneous tube drainage is a safe and effective method for treating lung abscesses, and it should be strongly considered in complicated patients who have failed trial of antibiotics. The evidence for such therapy is derived from uncontrolled case series, and the need for randomized trials cannot be emphasized enough.
18356
References
- Wali SO (2016) An Update on the Drainage of Pyogenic Lung Abscesses. Ann Thorac Med 7: 3-7.
- Beth GL, Stout JE (2008) Cavitary Pulmonary Disease. Clin Microbiol Rev 21: 305-333.