Keywords
Clinical competence; Continuous quality improvement; Fundamentals of laparoscopy; Gynecology simulation; Maintenance of certification; Mannequins; Medical education simulation; Obstetrics simulation; Patient safety; Pelvic ultrasound simulation; Project implementation; Quality assurance; Simulation center; Surgical competence; Surgical simulation; Trainee competence
Introduction
Globally in the modern world, healthcare specialties are faced with a need to increase opportunities for trainees and practitioner exposure to skills practice situations that do not involve either real or standardized patients. The underlying rationale may vary across specialties and nations. In the United States, as resident work hour restrictions were implemented obstetrics and gynaecology (ObGyn) residents’ gynaecologic and obstetric procedure volume decreased creating a need for a continuous quality improvement (CQI) project, substantiated below. Based on a healthcare cost and utilization project (HCUP) database search, the most frequent gynaecologic procedures (excluding termination of pregnancy and dilation and curettage) in community hospitals totalled 1,649,000 in 2012, a 796,824 decline from 2,445,824 in 2007 [1]. Hysterectomies in particular decreased 247,613 from 681,234 in 2002 to 433,621 in 2010 [2]. The introduction of roboticassisted surgery further reduced resident participation in surgery [3].
Simultaneously, with the recession of 2008-2010, obstetric deliveries declined by 384,052, from a peak of 4,316,233 in 2007 to a nadir of 3,932,181 in 2013 [4,5]. However, due to an increasing primary caesarean delivery (CD) rate and a decline in the number of facilities offering trial of labor after CD, the rate of CD remains adequate at 32.8% for sufficient procedural learning. Meanwhile, obstetric patients’ age and medical morbidities increased, raising the potential for intrapartum obstetric emergencies such as abruptio placentae that require rapid team response [6-10]. These facts are consistent with an increase in the average number of cesarean sections per ObGyn resident from 191.8 in 2002-2003 to 233.4 in 2012-2013, while volumes of vaginal, forceps, and vacuum deliveries, and amniocentesis decreased [11]. Nevertheless, operative time per CD increased by a mean of 16.3 minutes from 2003-2004 to 2010-2011, p<0.001, attributable to declining trainee skill and/or increasing surgical complexity [12]. It is known that high volume surgeons can have significantly lower complication rates than low volume surgeons, p<0.001 [13]. Thus, decreasing surgical volumes raise the question of procedural patient safety in health care institutions. But, proficiency-based surgical skills simulation has been shown to improve ObGyn trainee competency, p<0.01 [14].
Meanwhile, subspecialty fellowship program directors found recent graduating ObGyn and general surgery residents lacking the surgical and academic skills necessary to maximally benefit from further training [15-17]. In fact, fellowship training is now necessary for new surgeons to attain outcomes comparable to senior surgeons [18]. Teaching institutions need a means to improve ObGyn residents’ gynecologic surgery skills despite a smaller volume of real surgical cases. Some teaching institutions have turned to international rotations in resourcelimited nations to increase American residents’ surgery volume, possibly doubling monthly surgical volume [19,20]. However, the ethics therein, akin to the ethics of medical volunteerism, are questionable, especially given that resourcelimited nations need to train and increase their indigenous health care workforce [21-23].
Simulation allows health care workers to learn and develop appropriate skill sets in a safe environment, without harming patients [24-26]. Simulation identifies knowledge, procedural, and collaborative skills requiring improvement [27]. Obstetrics simulation training has been linked with improved neonatal outcomes, medical student interest in obstetrics, and obstetrics team building [28]. Pelvic simulator training improves performance of shoulder dystocia and vaginal breech deliveries [29]. Therefore, surgical skills simulation is the ethically appropriate option for ObGyn trainee surgical skill improvement [30].
Therefore, healthcare institutions that have not established surgical skills simulation centers (SSSC), and healthcare institutions that have outdated simulation centers need to give consideration to, or reconsider surgical skills simulation. This paper provides a strategy for incorporating a SSSC into an obstetrics and gynecology department. This strategy could be used by any department simply by selecting appropriate supporting material. Readers will be shown how to evaluate stakeholder preparedness to support a continuous quality improvement project. Aspects of gynaecology and obstetrics that can be improved via simulation will be identified (as can be done for any specialty). Finally, the benefits of SSSC incorporation into medical training programs will be clarified.
A Strategy for Surgical Skills Simulation Center Implementation
First delineate a CQI need. The aforementioned status of ObGyn trainees’ skills supports a needs statement for surgical skills continuous quality improvement (CQI) via skills simulation in ObGyn. Second, acquire suggestions to address the need: Brainstorming is a viable option. Third, select the most appropriate solution that addresses the need, which can also be done by brainstorming. Fourth, implement the chosen solution. Eight factors that affect SSSC implementation outcome will be reviewed: Science, staff, supplies, space, support, systems, success, and sustainability [31]. These factors come into play at different stages of SSSC implementation.
Continuous Quality Improvement Project Needs Delineation
The baseline CQI needs as identified above provide a starting point to which future successes can be compared. The following gynaecologic, obstetric, and ultrasound skills simulation programs provide a basis upon which a SSSC can be developed. Existing international simulation systems can be drawn upon to facilitate streamlined, cost-effective initial SSSC operation.
The Fundamentals of Laparoscopic Surgery (FLS) web- and simulation-based training program, developed to address quality and safety of surgical resident training, is requisite for American Board of Surgery residency program completion [32]. Completion of FLS is also a component of board certified surgeons’ maintenance of certification (MOC). Simulation programs are also accepted as annual improvement in medical practice modules for board certified ObGyns’ MOC. FLS incorporation into gynaecologic residency program training has been recommended [33]. Structured robotic simulation may become a mandatory component of surgical specialty residency programs [34]. Following suggestions that Canada adopt a standardized national ObGyn resident simulation program, a Canadian gynecologic laparoscopy simulation program was developed and validated [35-37]. The Canadian gynecologic laparoscopic simulation program may form the basis for global gynecologic laparoscopic simulation, use of which would complement FLS. Medical student, physician assistant, midwife, ObGyn resident and attending obstetrics training and L&D obstetric emergency team training needs may be met by a surgical skills simulation center (SSSC).
Ultrasound is an integral part of obstetrical and gynecological evaluation, and essential for performance of some specialty specific procedures including amniocentesis and oocyte retrieval. Gynecologic emergencies may initially present to the Emergency Department, where rapid disposition hinges on emergency physicians’ performance of transvaginal pelvic ultrasound [38]. However, emergency physicians may only spend 4 weeks of their residency on Labor and Delivery, with vaginal delivery performance being the priority. Similarly, if only to competently supervise ultrasonographers, radiology residents benefit from ultrasound simulation [39]. ObGyn resident ultrasound efficacy following clinical training is less than after simulation-based transvaginal ultrasound training, p<0.001 [40]. Dyad training reduces training costs by reducing instructor, training facility, and participant time [41]. Based on the objective structured assessment of ultrasound skills (OSAUS) dyad obstetrics simulation training has been shown to be statistically significantly better than individual simulation training, p=0.05 [42].
Given the above, the next step is to develop organizational buy-in for resolution of declining ObGyn trainee skills set. The need to satisfy mandated trainee competencies cannot be overlooked [36]. Concurrently, skills simulation provides a means for practitioners to satisfy MOC requirements [43]. Awareness that ObGyn attending physicians can also maintain and improve their skill sets via SSSC use further supports the case for a SSSC CQI implementation project.
Brainstorming
CQI option analysis brainstorming with at most 30 facility wide representatives is a method to consider options for Ob- Gyn resident skills improvement. Facility wide representatives should be drawn from anaesthesia, emergency medicine, human resources (or the department responsible for nursing on boarding), internal medicine, neurosurgery, ObGyn, orthopaedics, paediatrics, and radiology. These are all departments proven to benefit from surgical skills simulation [28,29,38-40,44].
The brainstorming process should include an icebreaker, CQI need presentation, idea collection, review and selection for CQI project implementation. This entire process can be completed within a few hours, depending on the volume of ideas generated.
An icebreaker should be used at the brainstorming session onset even if all the participants are known to each other. A novel icebreaker is for each participant to find the answers to a jeopardy game style question sheet from their colleagues at the brainstorming session. The icebreaker should not take more than 10 minutes. After the icebreaker, all participants should be seated. The need for ObGyn trainee skill improvement should be presented. Thereafter, participants will be given five minutes to write down their initial thoughts for a solution on a provided paper.
The brainstorming session facilitator will collect all suggestion papers and post these on a board for all participants to view. The participants will then anonymously vote on all the initial solutions. Computer programs such as ADoodle, CloudVOTE, DirectPoll, Engagenow, Gooru, Kwik Surveys, Live Vote, MeetingPulse, Micropoll, Obsurvey, Opinion Stage, Participoll, Polldaddy, Poll Everywhere, Slido, SMSPoll, TurningPoint, Voxvote, Wooclap, Yarp, YawnBuster Connect, and Yorn can be used to perform the initial solutions vote. The top seven solutions should be selected for further discussion. To facilitate this participants will break into no more than seven sub-groups. Each sub-group should have at least four participants assigned to work on one of the initial top seven solutions. The sub-groups will be directed to discuss costs, logistics, and support for their assigned top seven initial solution. Sub-group discussion should take 10 minutes. The brainstorming facilitator may have prepared pro and con sheets for the most likely options that can be given to the subgroups to assist their discussions.
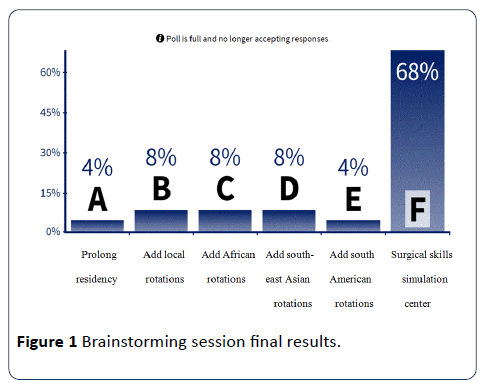
After the 10-minute sub-group discussion period each subgroup will present their assigned initial solution to the main group. Five minutes per sub-group should be sufficient, after which a final anonymous vote is taken. Poll Everywhere or other selected computer program can also be used for the final vote, in which case the outcome may be projected for all participants to see, as in Figure 1. Following the final vote, the facilitator will establish the first CQI project implementation meeting at which the concept and parts needed to achieve the concept will be reintroduced [45]. An overview of the CQI project implementation process follows.
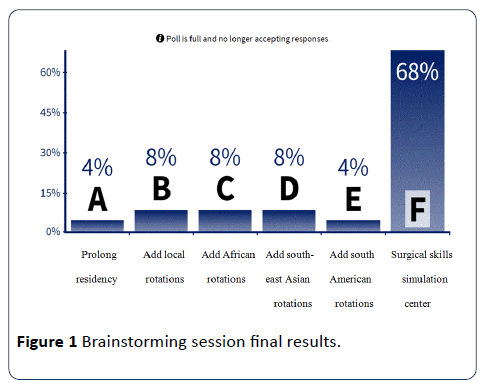
Figure 1: Brainstorming session final session.
The CQI project implementation committee will determine if any parts of the CQI project can be established as standalone processes. CQI project implementation illustrations including documentary films can be sought. These illustrations can be used for a movie and lunch showing. The CQI project implementation committee will need to determine how to keep track of before and after outcomes. Identified barriers will be addressed. The method by which the CQI project will be introduced to affected staff and departments will be determined. If available, implementation films should be reshown. Provision for coaching should be made. A go-live date must be determined. Once live, the CQI project implementation committee should hold monthly reviews for 1 year. Pre- and post-implementation data should be reviewed at each monthly meeting. Plan-do-study-act cycles should be performed as necessary. Finally, determination should be made as to when the CQI project may be implemented in facility-wide departments. Throughout the course of the CQI project implementation committee meetings, eight factors that affect SSSC implementation must be addressed.
Surgical Skills Simulation Center Implementation Considerations
Eight factors that affect SSSC implementation outcome are science, staff, supplies, space, support, systems, success, and sustainability [31]. These factors come into play at different stages of SSSC implementation. Each factor is reviewed to provide an understanding of what is needed to follow through with a SSSC implementation project.
Staff
Seek, cultivate, achieve, and maintain project buy-in from all current intended users within the primary department: Medical and nursing students, residents, nurses, midwives, nurse practitioners (NP), physician assistants (PA), and physicians should be secured. Nurse and physician champions should be sought and cultivated [31]. Include a representative presence in stakeholder discussions from potential user departments including anesthesiology, emergency medicine, human resources, pediatrics, neurosurgery, orthopedics, radiology, surgery and urology. Human resources may consider using the SSSC as part of new employee onboarding. Simulation presentations throughout the facility may be necessary to garner support [31].
Staff to support the SSSC must be put in place. This may be a minimum of a medical simulation fellow (who may also be a part-time attending) and a support person. The SSSC should be staffed at least during normal office hours for training environment and posture issues [46]. Teaching hospitals have a median of 2 and an average of 3.4 full time equivalent staff for a SSSC [47]. Medical schools have a median of 5 and an average of 8.1 FTE staff for a SSSC [47]. SSSC implementation also creates leadership and leadership training opportunities within the health care facility.
Space
Given the size and layout of medical centers, for convenient 24/7 accessibility multiple SSSC, and/or a mobile SSSC may be viable for a single medical center. If the facility has a space allocation committee, the SSSC implementation project needs to be presented to the committee as early as possible [31]. The physical space for the SSSC may need to be developed, entailing renovating existing spaces, new construction, or temporary facilities [31,48].
Given a USD 4.204 million capital investment for a 800 to 1,200 square feet SSSC renovation with initial capital equipment stocking, and USD 476,000 annual operating budget in 2011, all health care facility departments that could benefit from the SSSC need to be onboard to share SSSC implementation and operating costs [48]. The annual operating budget for 75% of teaching hospital and 43% of medical school SSSC is less than USD 500,000 [47]. If the SSSC includes standardized patient exam rooms, median space requirements are 2,100 to 4,650 square feet, with average space requirements of 4,973 to 6,401 square feet [47]. These spaces and budgets can accommodate an average of 1,500 individual learners annually in an average of 700 to 822 total sessions annually. Budget differences between medical schools and teaching hospitals are partially attributable to medical schools having fewer but longer sessions, while teaching hospitals have more but briefer sessions [47].
Systems
Low and high-fidelity simulation equipment, mannequins, ultrasound machines, and other capital equipment, and disposables have to be procured [48]. The facility and equipment should be sufficient to provide each resident with 40 hours of simulation training per 3 months or about 80 hours in the intern year before clinical procedural exposure [48,49]. Equipment electrical, network, and internet needs should be considered [31]. Equipment warranties and maintenance, which may cost up to 15% of capital equipment costs, must be included in the annual operating budget [48].
Unless the institution only has rare training requirements initial investments should focus on the broadly applicable systems. The McGill Inanimate System for Training and Evaluation of Laparoscopic Skills (MISTELS), FLS, and Southwestern video trainer stations all have proven face, construct, and predictive validity [46]. While Lap Mentor and Xitact LS 500 virtual simulators have construct and predictive validity, haptic feedback, basic skills, and procedural task ability, neither has a validated teaching curriculum or team training ability [46]. However, Lap Sim with haptics does have all the above listed VRS capabilities. The selected simulator system(s) may include scheduling software. SimManager simulation scheduling software provides public view only and interactive user scheduling options. SimManager also tracks space and simulator use over time.
Supplies
Disposable supplies factor into both initial setup and annual operating costs. Expired supplies should be requested from all facility departments including Biomedical Equipment, Facilities Engineering, and the pharmacy [31]. This may yield audiovisual recording systems, examination tables, fluid management systems, injectable medications, intravenous kits, prefilled syringes, scopes, single use instruments, suture, and wound care items. When expired, single-use, or sterilized single-use supplies are used for simulation-based training, it must be explicitly stated that such use is only allowed in the simulation environment [31]. If the SSSC may be converted into a rapid response center, consideration should be given as to how expired or non-sterile supplies will be kept separate from supplies that may be used to treat living patients.
Science
The surgical skills curricula should be determined. The curricula should include cognitive knowledge development, technical skill associative development, and autonomous demonstration of adequate judgment [46]. Institutional procedural checklists should be incorporated into the curricula as appropriate [31]. A dedicated bulletin can publicly announce desired behaviors [31].
The FLS, obstetrics, and pelvic ultrasound simulation programs must be introduced to residents, nurses, midwives, NP, PA, and physicians. Departments must determine the logistics of incorporating the SSSC program into the residents’ schedules [49]. Residency FLS programs require 24-hour access SSSC [33]. Plan-do-study-act (PDSA) cycles may be necessary to determine which equipment, curricula, learners, and learning schedule should be introduced, and the manner in which this occurs. Users, departments, and funding may determine if SSSC programs are introduced sequentially or all at once.
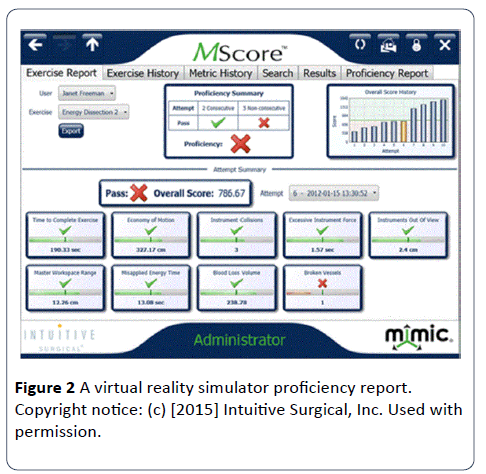
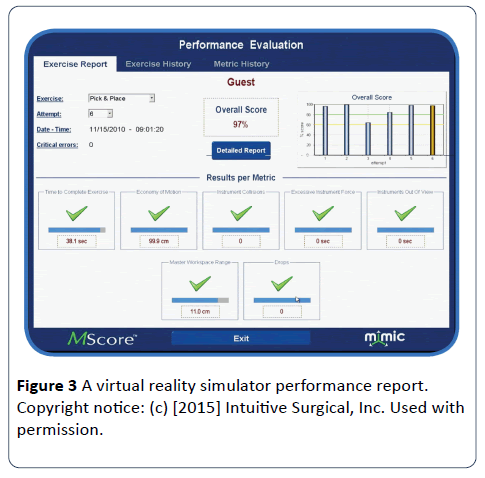
Evaluation metrics need to be determined. Pre-SSSC metric scoring must be done for baseline control statistics. A metrics outcome tracking mechanism will need to be determined and implemented. Outcomes tracking may factor into which simulation equipment is chosen for the SSSC, as integrated, computer-generated scorecards (Figures 2 and 3) and the capabilities thereof may vary across simulation equipment. Teaching staff will learn and use debriefing following obstetric team simulations [25,50]. Once ObGyn staff have completed their initial simulation programs, the medical and nursing students can be introduced to the SSSC.
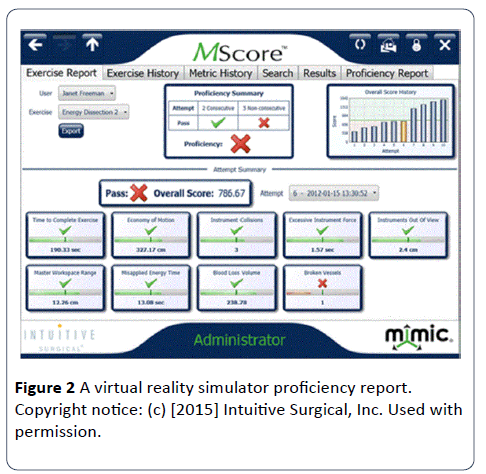
Figure 2: A virtual reality simulator proficiency report. Copyright notice: (c) [2015] Intuitive Surgical, Inc. Used with permission.
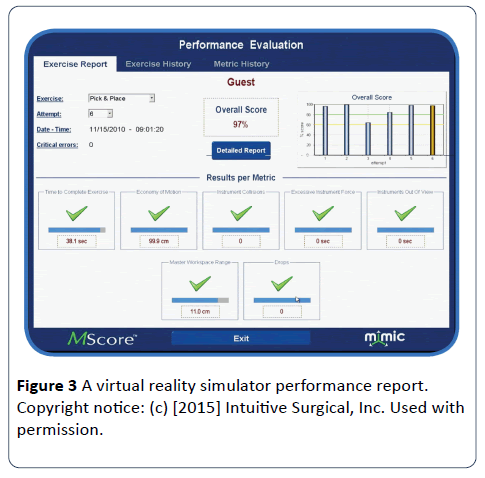
Figure 3: A virtual reality simulator performance report. Copyright notice: (c) [2015] Intuitive Surgical, Inc. Used with permission.
Success
User performance assessment at the end of each obstetrics or gynecology rotation will form the basis of periodic adjustments in the course of academic years. Each individual’s performance over time forms the individual’s CQI project. Training program, institutional, state, national, and international quality and safety benchmark scoring changes with time form the department CQI project, including the United Nations’ Millennium Development Goals 4 and 5 – reduction of maternal and infant, including neonatal mortality [51]. Annual quality and safety outcome changes may indicate the need for SSSC fine tune-ups or overhauls.
Support
SSSC achievements may be communicated to the entire health care facility via the employee newsletter or equivalent communication medium [31]. Simulation achievements relative to existing quality and safety benchmarks and resultant cost-effectiveness should be publicized, demonstrating the value of the SSSC [31]. The facility administrators and board members should be invited to simulation briefings and team simulations to kindle organizational support. The SSSC training schedule should be publicly posted informing staff when there are training sessions they may wish to join, and when equipment needed for individual, dyad, or team practice may be available. An equipment and space scheduling system should be established.
Sustainability
Residency and nursing program directors and coordinators will need to learn to extract and analyze integrated computer generated simulation scorecards, adjusting simulation training as needed. A simulation committee may be necessary. Simulation contests, including mannequin naming contests may be held [31].
Central venous catheter insertion (a required internal medicine procedure) simulation training for residents yields a 7 to 1 return on training costs versus the cost of treating catheter-related bloodstream infections [48]. Simulation-based training for bedside paracentesis is mathematically modeled to result in 80% cost savings based on interventional radiology paracentesis costs [52]. For laparoscopic procedures, part task simulation training (PT) can be more effective than whole task simulation training (WT). Laparoscopic inguinal hernia repair PT requires less time (p=0.02), USD 121 less material per learner, and is more likely to be retained 1-month later (p=0.03) than WT [53]. Therefore, sustainability must factor into initial simulation systems selection.
For revenue generation the SSSC should operate as close to a 24-hour per day, 7-days per week schedule as possible. Intravenous infusion therapy continuing medical education courses will appreciate having use of a center that does not require mannequin transportation, setup, and take down. Nursing schools, medical reserve corps volunteers, paramedics and emergency medical services also need SSSC services. The SSSC may house ACLS, ATLS, BLS, CPR, NRP, and PALS certification programs on the weekends.
In the United States, funding support is also available from the Agency for Healthcare Research and Quality, the Alliance for Academic Internal Medicine, the Comprehensive Emergency Management Program, the Telemedicine & Advanced Technology Research Center, and the United States Departments of Defense and Veterans Affairs [31]. Sample funding request applications and donor appeals are available through Internet searches.
Conclusion
Brainstorming allows an organization to choose the best fit solution. Simulation can safely and cost-effectively improve health care workers’ skills and patients’ outcomes. Improved health care quality and safety, which can be tracked as a CQI project, should be the result of SSSC implementation. Constant evaluation of simulation curricula, as well as individual, team, departmental, and facility outcomes scoring maintains CQI. To this end, PDSA cycles should occur at least as frequently as equipment upgrades are considered.
17869
References
- Wier LM, Steiner CA, Owens PL (2015) Surgeries in hospital-owned outpatient facilities, 2012. Agency for Healthcare Research and Quality: Rockville, Maryland, USA.
- McLeod JB, Cao J, Spiryda LB (2015) Introduction of laparoscopic hysterectomy approach: Decreasing the abdominal hysterectomy approach or replacing vaginal hysterectomy. Surg Res Open J 2: 36-42.
- Jeppson PC, Rahimi S, Gattoc L, Westermann LB, Cichowski S, et al. (2015) Impact of robotic technology on hysterectomy route and associated implications for resident education. Am J Obstet Gynecol 212: 196 -196.
- Hamilton BE, Martin JA, Osterman MJK, Curtin SC (2015) Births: Preliminary data for 2014. National Vital Statistics Reports.
- Lockwood CJ (2012) Washington’s political failures and your practice. Implications for ob/gyns. Contemporary OB/GYN.
- Callaghan WM, Creanga AA, Kuklina EV (2012) Severe maternal morbidity among delivery and postpartum hospitalizations in the United States. Obstetrics Gynecol 120: 1029-1036.
- Ibrahim M, Ziegler C, Klam SL, Wieczorek P, Abenhaim HA (2014) Incidence, indications, and predictors of adverse outcomes of postpartum hysterectomies: 20-year experience in a tertiary care center. J Obstet Gynaecol Can 36: 14-20.
- Janoudi G, Kelly S, Yasseen A, Hamam H, Moretti F, et al. (2015) Factors associated with increased rates of cesarean section in women of advanced maternal age. J Obstet Gynaecol Can 37: 517-526.
- Mehrabadi A, Liu S, Bartholomew S, Hutcheon JA, Kramer MS, et al. (2014) Temporal trends in postpartum hemorrhage and severe postpartum hemorrhage in Canada from 2003 to 2010. J Obstet Gynaecol Can 36: 21-33.
- Mhyre JM, Bateman BT, Leffert LR (2011) Influence of patient comorbidities on the risk of near-miss maternal morbidity or mortality. J Am Soc Anesthesiol 115: 963-972.
- Gupta N, Dragovic K, Trester R, Blankstein J (2015) The changing scenario of obstetrics and gynecology residency training. J Grad Med Educ 7: 401-406.
- Smrtka MP, Gunatilake RP, Harris B, Yu M, Lan L, et al. (2015) Increase in cesarean operative time following institution of the 80-hour workweek. J Grad Med Educ 7: 369-375.
- Wallenstein MR, Ananth C, Kim JH, Burke WM, Hershman DL, et al. (2012) Effect of surgical volume on outcomes for laparoscopic hysterectomy for benign indications. Obstetrics Gynecol 119: 709-716.
- Gala R, Orejuela F, Gerten K, Lockrow E, Kilpatrick C, et al. (2013) Effect of validated skills simulation on operating room performance in obstetrics and gynecology residents: a randomized controlled trial. Obstetrics Gynecol 121: 578-584.
- Doo DW, Powell M, Novetsky A, Sheeder J, Guntupalli SR (2015) Preparedness of Ob/Gyn residents for fellowship training in gynecologic oncology. Gynecol Oncol Rep 12: 55-60.
- Guntupalli SR, Doo DW, Guy M, Sheeder J, Omurtag K, et al. (2015) Preparedness of obstetrics and gynecology residents for fellowship training. Obstetrics Gynecol 126: 559-568.
- Mattar S, Alseidi A, Jones D, Jeyarajah DR, Swanstrom LL, et al. (2013) General surgery residency inadequately prepares trainees for fellowship: results of a survey of fellowship program directors. Ann Surg 258: 440–449.
- Johnston MJ, Singh P, Pucher PH, Fitzgerald JE, Aggarwal R, et al. (2015) Systematic review with meta-analysis of the impact of surgical fellowship training on patient outcomes. Br J Surg 102: 1156-1166.
- Henry JA, Groen RS, Price RR, Nwomeh BC, Kingham TP, et al. (2013) The benefits of international rotations to resource-limited settings for U.S. surgery residents. Surgery 153: 445-454.
- Kolkman P, Soliman M, Kolkman M, Stack A, Rao TS, et al. (2015) Comparison of resident operative case logs during a surgical oncology rotation in the United States and an international rotation in India. Indian J Surg Oncol 6: 36-40.
- Coors ME, Matthew TL, Matthew DB (2015) Ethical precepts for medical volunteerism: Including local voices and values to guide RHD surgery in Rwanda. J Med Ethics 41: 814-819.
- Melby MK, Loh LC, Evert J, Prater C, Lin H, et al. (2016) Beyond medical “missions” to impact-driven short-term experiences in global health (STEGHs): Ethical principles to optimize community benefit and learner experience. Acad Med 91: 633-638.
- Stone GS, Olson KR (2016) The ethics of medical volunteerism. Medical Clinics of North America 2016: 237-246.
- Argani CH, Eichelberger M, Deering S, Satin AJ (2011) The case for simulation as part of a comprehensive patient safety program. Am J Obstet Gynecol 206: 451-455.
- Ennen CS, Satin AJ (2010) Training and assessment in obstetrics: The role of simulation. Best Pract Res Clin Obstet Gynaecol 24: 747-758.
- Rall M, Gaba DM, Dieckmann P, Eich CB (2015) Patient simulation. In: Miller RD, Eriksson LI, Fleischer L, Wiener-Kronish JP, Cohen NH (eds) Miller’s Anesthesia (8th edn). Elsevier, Waltham, Massachusetts, United States. pp: 167-209.
- Maslovitz S, Barkai G, Lessing JB, Ziv A, Many A (2007) Recurrent obstetric management mistakes identified by simulation. Obstetrics Gynecol 109: 1295-1300.
- Rosen KR (2008) The history of medical simulation. J Crit Care 23: 157-166.
- Alici F, Buerkle B, Tempfer CB (2014) Objective structured assessment of technical skills (OSATS) evaluation of hysteroscopy training: A prospective study. Eur J Obstet Gynecol Reprod Biol 178: 1-5.
- Ziv A, Wolpe PR, Small SD, Glick S (2006) Simulation-based medical education: An ethical imperative. Simulation in Healthcare: J Soc Simul Healthc 1: 252-256.
- Lazzara EH, Benishek LE, Dietz AS, Salas E, Adriansen DJ (2014) Eight critical factors in creating and implementing a successful simulation program. Jt Comm J Qual Patient Saf 40: 21-29.
- Scott DJ, Hafford M, Willis RE, Gugliuzza K, Wilson TD, et al. (2013) Ensuring competency: Are fundamentals of laparoscopic surgery training and certification necessary for practicing surgeons and operating room personnel? Surg Endosc 27: 118-26.
- Hur H-C, Arden D, Dodge LE, Zheng B, Ricciotti HA (2011) Fundamentals of laparoscopic surgery: A surgical skills assessment tool in gynecology. J Soc Laparoendoscopic Surg 15: 21-26.
- Vogell A, Gujral H, Wright KN, Wright VW, Ruthazer R (2015) Impact of a robotic simulation program on resident surgical performance. Am J Obstet Gynecol 213: 874-875.
- Sanders A, Wilson RD (2015) Simulation training in obstetrics and gynaecology residency programs in Canada. J Obstet Gynaecol Can 37: 1025-1032.
- Cundiff GW (2016) At last, a standardized laparoscopy curriculum for gynecology residents. Am J Obstet Gynecol 215: 137-139.
- Shore EM, Grantcharov TP, Husslein H, Shirreff L, Dedy NJ, et al. (2016) Validating a standardized laparoscopy curriculum for gynecology residents: A randomized controlled trial. Am J Obstet Gynecol 215: 204.e1-204.e11.
- Girzadas DV, Antonis MA, Zerth H, Lambert M, Clay L, et al. (2009) Hybrid simulation combining a high fidelity scenario with a pelvic ultrasound task trainer enhances the training and evaluation of endovaginal ultrasound skills. Acad Emerg Med 16: 429-435.
- Ahmad R, Alhashmi G, Ajlan A, Eldeek B (2015) Impact of high-fidelity transvaginal ultrasound simulation for radiology on residents’ performance and satisfaction. Acad Radiol 22: 234-239.
- Tolsgaard MG, Ringsted C, Dreisler E, Nørgaard LN, Petersen JH, et al. (2015) Sustained effect of simulation-based ultrasound training on clinical performance: A randomized trial. Ultrasound Obstet Gynecol 46: 312-318.
- Bjerrum AS, Morcke AM (2015) Dyad training: Effective, efficient and transferable. What are we waiting for? Med Educ 49: 242-246.
- Tolsgaard MG, Madsen ME, Ringsted C, Oxlund BS, Oldenburg A, et al. (2015) The effect of dyad versus individual simulation-based ultrasound training on skills transfer. Med Educ 49: 286-295.
- Smith ML, Foley MR (2016) Transforming clinical education in obstetrics and gynecology. Obstet Gynecol 127: 763-767.
- Gardner R, Raemer DB (2008) Simulation in obstetrics and gynecology. Obstet Gynecol Clin North Am 35: 97-127.
- Lilaonitkul M, Kwikiriza A, Ttendo S, Kiwanuka J, Munyarungero E, et al. (2015) Implementation of the WHO Surgical Safety Checklist and surgical swab and instrument counts at a regional referral hospital in Uganda – a quality improvement project. Anaesthesia 70: 1345-1355.
- Schreuder HWR, Oei G, Maas M, Borleffs JCC, Schijven MP (2011) Implementation of simulation for training minimally invasive surgery. Neth J Med Educ 30: 206-220.
- Passiment M, Sacks H, Huang G (2011) Medical simulation in medical education: Results of an AAMC survey. Association of American Medical College, Washington, DC, USA.
- Danzer E, Dumon K, Kolb G, Pray L, Selvan B, et al. (2011) What is the cost associated with the implementation and maintenance of an ACS/APDS-based surgical skills curriculum? J Surg Educ 68: 519-525.
- Krajewski A, Filippa D, Staff I, Singh R, Kirton OC (2013) Implementation of an intern boot camp curriculum to address clinical competencies under the new accreditation council for graduate medical education supervision requirements and duty hour restrictions. JAMA Surgery 148: 727-732.
- Johnston MJ, Paige JT, Aggarwal R, Stefanidis D, Tsuda S, et al. (2015) An overview of research priorities in surgical simulation: What the literature shows has been achieved during the 21st century and what remains. Am J Surg 211: 214-225.
- Fransen AF, Banga FR, Ven VDJ, Moi BWJ, Oei SG (2015) Multi-professional simulation-based team training in obstetric emergencies for improving patient outcomes and trainees’ performance (protocol). The Cochrane Library.
- Barsuk JH, Cohen ER, Feinglass J, Kozmic SE, McGaghie WC, et al. (2014) Cost savings of performing paracentesis procedures at the bedside after simulation-based education. Simul Healthc 9: 312-318.
- Hernández-Irizarry R, Zendejas B, Ali SM, Farley DR (2016) Optimizing training cost-effectiveness of simulation-based laparoscopic inguinal hernia repairs. Am J Surg 211: 326-335.