Keywords
Childhood-onset Systemic lupus erythematosus; Clinical manifestation; Laboratory finding; Management
Introduction
Systemic Lupus erythematosus (SLE) is a severe, chronic autoimmune disease, that results in inflammation and eventual damage in a broad range of organ systems; kidney, joint, skin, heart, pulmonary, hematology, Neurological system and Blood vessels [1]. It is likely that lupus is a multifactorial disease of unknown etiology in which significant immunological abnormalities have been identified. Hormonal, genetic and environmental factors have been implicated in its etiology [1].
SLE is a relatively rare disease in childhood, approximately 20% of individuals with SLE will have their disease onset prior to the age of 16 years [1].
SLE generally presents between the age of 5-15 years, rare in children younger than 5year [1-4]. Females are most commonly affected with female-to-male of 4.5-5:1 prior to puberty, raised to 9-10:1 after puberty [1-9].
There is no specific diagnostic test for cSLE, and diagnosis is notoriously difficult due to protean clinical symptoms and signs. Physicians have commonly relied on the American college of rheumatology (ACR) criteria for the classification of SLE [10]. These criteria were preliminary developed in 1971, revised in 1982 and updated in 1997 [11]. A child can be classified as having SLE if at least four of the 11 criteria are present in order to address the limitations of ACR criteria, the systemic lupus international collaborating clinics (SLICC) developed SLICC criteria in 2012 [12], which exhibited higher sensitivity and lower specificity than ACR criteria. The SLICC criteria include 11 clinical and 6 immunologic items. It requires 4 items with at least one clinical and one immunologic item or biopsy proven nephritis compatible with lupus in presence of a ANA or Anti ds-DNA. The SLICC criteria has been validated in children, showing better sensitivity and fewer mis-classifications than the ACR criteria [12,13]. Of note, both criteria are classification rather than diagnostic criteria and some patients need treatment despite not fitting these classification criteria.
Because of its protean manifestations, lupus must be considered in the differential diagnosis of many conditions including fever of unknown origin, arthritis, anemia and new onset kidney disease [14].
The clinical manifestations of SLE have been extensively described from different geographical parts of the word, the prevalence and severity of the disease differs among ethnic groups [2-9,14].
The disease has variable presentations including conditional symptoms, cutaneous, cardiac, pulmonary, musculoskeletal and renal. The disease course is characterized by periods of remission and flares and children with cSLE have more active disease at presentation and over time than do adults with SLE, especially active renal disease [15].
The long-term prognosis for SLE has improved markedly in recent years because of earlier diagnosis and optimized treatment [16], although children with SLE suffering extensive morbidity because of the longer duration of disease activity causing cumulative damage as well as the side effects from medication [17].
The aim of this study is to evaluate disease characteristics; clinical manifestations, laboratory characteristics, and treatment in patients with SLE following at Rheumatology department, Tripoli children hospital.
Methods
In this retrospective, descriptive study, we reviewed the medical files of children with diagnosis of cSLE who are following at Tripoli children hospital, rheumatology department over the last 7 years (January 2011- April 2018).
The diagnosis of SLE was based on 1997 updated criteria for the classification of SLE. All children fulfilled at least 4 of the American college criteria and had been diagnosed at least 6 months. All patients files were reviewed for demographic, clinical and laboratory finding, the following parameters were collected; age at onset of the disease, age at diagnosis, gender, Initial diagnosis (diagnosis at referral), disease duration (time from the disease onset until the present time), diagnosis time interval (period between disease onset to diagnosis), clinical manifestations at the onset and during the evolution of the disease. Disease activity was determined using British Isles lupus assessment group (BILAG) index. BILAG is recording clinical disease activity in 8 different organ systems for a total of 86 items [18], each item is measured qualitatively by clinical observation (yes, no, improvement, same, worse, new) or quantitatively by measuring hematological and renal values. Based on these items, each of the 8 organ system is allocated an alphabetical score of A (most active), B (moderate activity), C (minor activity) D (stable) or E (never present). Normally total score is not calculated. Laboratory abnormalities were defined according to ACR classification criteria for SLE. Immunological parameters recorded include antinuclear antibody (ANA), anti-double strand DNA (Anti ds DNA), Antiphospholipid antibodies (lupus anticoagulant, Anticardiolipin), Extractable nuclear antibodies (ENA), Serum complement, C3, C4. Pathological evaluation includes renal biopsy; renal biopsies were classified according to WHO classification for lupus nephritis [19].
SPSS 16 software was used for of data analysis, the result is expressed as means for continuous variable and frequencies/ percentages for categorical variables.
Results
The total number of SLE patients diagnosed in Rheumatology department, Tripoli children hospital in the period from January 2011 to April 2018 was 12 cases. 10 were Females (83.3%), 2 were males (16.7%) with F:M of 5:1. Age at onset ranged from 5-15 year with mean of 11.6 years. Mean age at diagnosis was 12.5 years. Disease duration was 6 months to 14 years.
Only two patients referred with initial diagnosis of SLE while 10 patients referred with different diagnosis. Diagnosis at referral was Henoch Schonlein purpura in 3 patients, idiopathic thrombocytopenic purpura in one patient, Evans syndrome in one patient, acute Rheumatic fever in one patient, systemic onset juvenile idiopathic arthritis in one patient, inflammatory bowel disease in one patient and tow patient suspected to have leukemia.
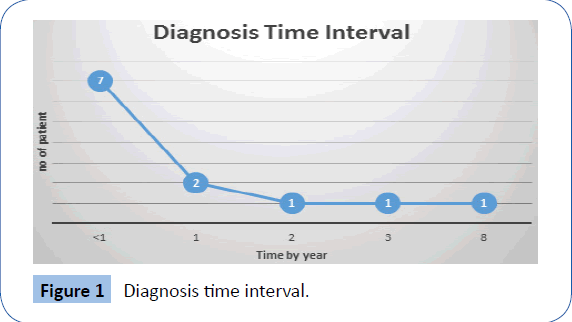
Diagnosis time interval ranged from 6 months to 8 years, with 7 patients diagnosed within the first year after disease onset. One patient during 2nd year, one patient during 3rd year and one patient diagnosed after 8 years of disease onset (Figure 1).
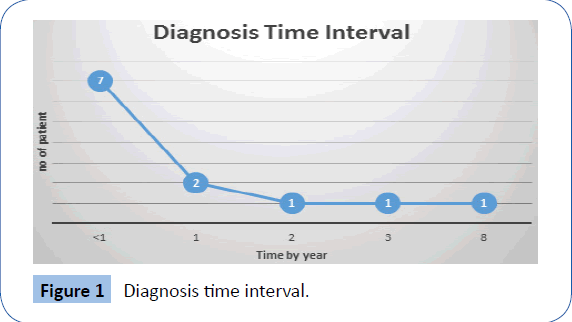
Figure 1: Diagnosis time interval.
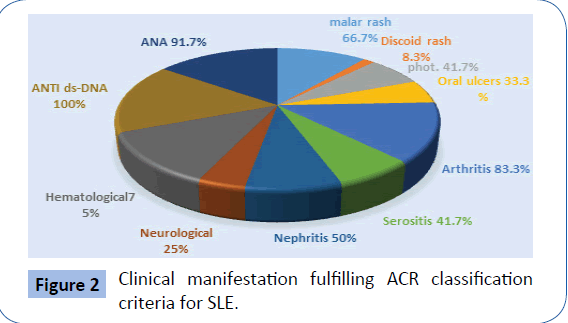
The main clinical manifestations of our patients that’s full filling ACR classification criteria are shown in Figure 2, the most common clinical manifestations seen were articular in 83.3%, followed by hematological manifestations in 75%, skin in 66.7% [20] and renal manifestations in 50% of patients. Other manifestations are listed in Table 1.
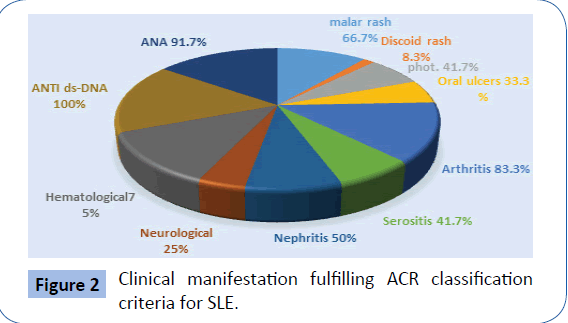
Figure 2: Clinical manifestation fulfilling ACR classification criteria for SLE.
| Clinical presentation |
No of patient |
| fever |
6 (50) |
| Fatigability |
5 (41.7) |
| Arthralgia |
2 (16.7) |
| Dyspnea |
4 (33.3) |
| Palpitation |
4(33.3) |
| Abdominal pain |
1 (8.3) |
| Anorexia |
1 (8.3) |
| Alopecia |
2 (16.7) |
| Raynaud’ phenomena |
0 |
| Other skin manifestation |
4 (33.3) |
| Lymphadenopathy |
1 (8.3) |
| Hepatosplenomegaly |
1 (8.3) |
Table 1: Other clinical manifestations.
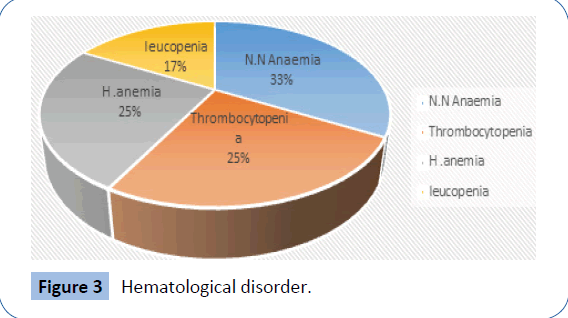
The most common hematological manifestations in our patient was normocytic normochromic anemia of chronic illness in 33% of patient, followed by hemolytic anemia in 25%, thrombocytopenia in 25% and leucopenia in 17% of patients Figure 3.
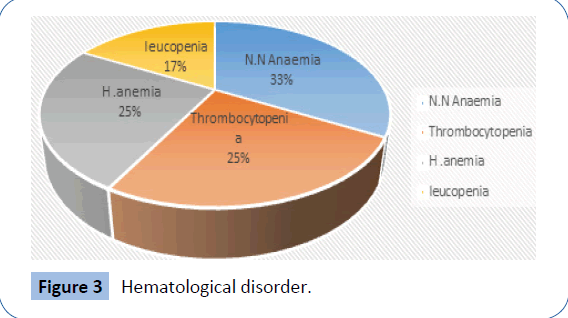
Figure 3: Hematological disorder.
Renal involvement occurred in 6 (50%) of our patients, tow patients at the time of diagnosis other 4 patient developed renal disease within the first year of follow up. 5 of them had renal biopsy with histopathological evaluation classified according to modified world Health Organization classification (Figure 4).

Figure 4: Renal biopsy findings according to WHO Classification.
The immunological parameters are show in Table 2. 91.7% of our patients had positive ANA titer, and one patient had SLE despite negative ANA titer. Anti-ds- DNA was positive in 100% of patients. Complement was low in 33.3% of patients (Table 2).
| Investigations |
No of patient (%) |
| ANA |
11 (91.7) |
| Anti-ds-DNA |
12 (100) |
| ENA |
5 (41.7) |
| C3 |
4 (33.3) |
| C4 |
4 (33.3) |
| CRP |
4 (33.3) |
| ESR |
5 (41.7) |
Table 2: Laboratory results.
All of our patients treated with corticosteroids for the disease control, 2nd most commonly used drug was hydroxychloroquine in 10 (83.3%) of patients. Immunosuppressive medications were used in 10 (83.3%) including Azathioprine in 5 (41.7%) patients, 5 (41.7%) patients treated with pulses cyclophosphamide followed by Mycophenolate mofetil (Table 3).
| Medications |
No of patient (%) |
| Steroid |
12 (100) |
| Hydroxychloroquine |
10 (83.3) |
| Enaloprile |
6 (50) |
| MMF |
5 (41.7) |
| Cyclophosphamide |
5 (41.7) |
| Azathioprine |
5 (41-7) |
| Ritoxamab |
2 (16.7) |
| Warfarin |
1 (8.3) |
| Heparin |
2 (16.7) |
| Asprin |
4 (33.3) |
Table 3: Medication used in treatment of cSLE.
The clinical features of SLE in our patient population were then compared to other childhood SLE series from other Arabic countries such as Saudi Arabia, Egypt, Jordan, Sultanate of Oman.
Discussion
This is a retrospective single center study carried out in department of rheumatology at Tripoli children hospital. The total number of SLE patients diagnosed in the period from January 2011 to April 2018 was 12 patients. This small number of patients may be due to that many cSLE patients are followed by adult rheumatologist due to adolescent predilection of this disease. Only two patients referred with initial diagnosis of SLE while 10 patients referred with different diagnosis as Henoch Schonlein purpura, idiopathic thrombocytopenic purpura, Evan syndrome, Acute rheumatic fever, Inflammatory bowel disease, Systemic onset juvenile idiopathic arthritis and malignancy, this indicate that SLE have a great variability in disease presentation and course [5,6]. Therefore, Knowledge of general pediatric diseases that can mimic SLE is very important in making the accurate diagnosis. Age at onset ranged from 5-15 year with mean of 11.6 years.
The clinical and laboratory findings of childhood SLE patients in our series were compared to other childhood SLE series from other Arabic countries; Egypt, Jordan, Tunisia, Oman, Saudi Arabia, and Kuwait to identify any variation. The mean age at diagnosis was 12.5 years which is higher than other Arab pediatric SLE series. Taking in consideration the marked delay in diagnosis in one of our cases that diagnosed as Evan syndrome for 8 years.
The most common clinical manifestations seen were articular in 83.3%, followed by hematological manifestations in 75%, skin in 66.7% and renal manifestations in 50% of patients. Cutaneous manifestations observed in 66.7% of our patients compared with 70% in Omani patients, 52% in Jordanian patients, 51% in Kuwait patients and much higher than the Egyptian patients. Musculoskeletal manifestations was observed in 83.3% of our patients, which is higher than all comparable studies in which MSK manifestations ranged from 36% in Egyptian patients to 76% in Omani patient.
Renal involvement was found in 50% of our patients, nothing that renal manifestation occurs in 29% to 83% in comparable studies.
Conclusion
SLE has a highly variable presentation, a high index of suspicion should be maintained in order to make an early diagnosis. Better recognition of the age-specific manifestations of this disease is required to improve its outcome.
22698
References
- Petty RE, Laxer RM, Lindsley CB, Wedderburn LR (2016) Text book of pediatric rheumatology (7th Ed.): 285-317.
- Rahman SA, Islam MI, Talukder MK, Islam M, Huque SS, et al. (2015) Presentation of childhood systemic lupus erythematoosis in a tertiary care hospital. Bangladesh J Child Health 38: 124-129.
- Ben Amer HM (2015) Clinical presentation of pediatric SLE at outpatient clinic. MOJ Orthoped Rheumatol 2: 00032.
- Abu-Shukair M, Habahbeh Z, Almutereen M, Zyoud R, Alwahadneh A, et al. (2014) Spectrum of pediatric systemic lupus erythematosus at queen rania al-abdullah hospital for children. J Royal Med Serv 21: 12-18.
- Thabet Y, Mankai A, Achour A, Sakly W, Trabelsi A, et al. (2014) Systemic lupus erythematosus in children: A study about 37 tunisian cases. J Clin Cell Immunol 5: 192.
- Muzaffer MA, Al-Mayouf SM (2011) Clinical and laboratory variables of childhood systemic lupus erythematosus in western province of saudi arabia. Rheumatol Int 31: 23-26.
- Abdwani R, Rizvi SG, El-Nour I (2008) Childhood systemic lupus erythematosus in sultanate of oman: Demographics and clinical analysis. Lupus 17: 683-686.
- Alsaeid K, Kamal H, Haider MZ, Al-Enezi HM, Malaviya AN (2004) Systemic lupus erythematosus in Kuwaiti children: Organ system involvement and serological findings. Lupus 13: 613-617.
- Kumar S, Nair S, Rajam L (2010) Case series of pediatric systemic lupus erythematosus from kerala: Comparison with other Indian series. Int J Rheumatic Dis 13: 391-395.
- Tan EM, Cohen AS, Fries JF, Masi AT, McShane DJ, et al. (1982) The (1982) revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 25: 1271-1277.
- Hochberg MC (1997) Updating the american college of rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 40: 1725.
- Petri M, Orbai AM, Alarcón GS, Gordon C, Merrill JT, et al. (2012) Derivation and validation of the systemic lupus international collaborating clinics classification criteria for systemic lupus erythematosus. Arthritis Rheum 64: 2677-2686.
- Inês L, Silva C, Galindo M, López-Longo FJ, Terroso G, et al. (2015) Classification of systemic lupus erythematosus: Systemic lupus international collaborating clinics versus american college of rheumatology criteria. A comparative study of 2,055 patients from a real-life, international systemic lupus erythematosus cohort. Arthritis Care Res 67: 1180-1105.
- Gottlieb B, NormanT (2006) Lupus erythematosus in children and adolescent. Pediatr Rev 27: 323-330.
- Brunner HI, Mina R, Pilkington C, Beresford MW, Reiff A, et al. (2011) Preliminary criteria for global flares in childhood-onset systemic lupus erythematosus. Arthritis Care Res (Hoboken) 63: 1213-1223.
- Thong B, Olsen NJ (2017) Systemic lupus erythematosus diagnosis and management. Rheumatol 56: i3–i13.
- Olowu W (2007) Childhood-onset systemic lupus erythematosus. J Natl Med Assoc 99: 777-784.
- Hay EM, Bacon PA, Gordon C, Isenberg DA, Maddison P, et al. (1993) The BILAG index: A reliable and valid instrument for measuring clinical disease activity in SLE. QJM 86: 447-558.
- Weening JJ, Agati VD, Schwartz MM, Seshan SV, Alpers CE, et al. (2004) The classification of glomerulonephritis in systemic lupus erythematosus revisited. J Am Soc Nephrol 65: 521-520.
- Kuhn A, Landmann A (2014) The classification and diagnosis of cutaneous lupus erythematosus, Reviewing the Recommendations for Lupus in Children. J Autoimmun 49: 14-19.