Keywords
ISSHL; Tinnitus; Hyperbaric oxygen therapy; Tonal audiogram; Safety
Introduction
The creation and organization of Hyperbaric Medical Units along with Decompression Chambers constitute a great achievement of modern medical technology. The main objective of the Hyperbaric Medical Units is dealing with the troubleshooting of diving accidents and the clinical application of Hyperbaric Oxygen (HBO2) therapy.
Idiopathic Sudden Sensorineural Hearing Loss (ISSHL) constitutes an urgent otologic disease and is considered sudden, when installed instantly or within three days and when it exceeds 30 dB in three audio-metrically contiguous frequencies. The number of patients ranges from 5 to 20 people per population of 100.000 people. The acute onset of hearing loss is usually accompanied by tinnitus (which may be described as a feeling of continuous or intermittent sound), and by the feeling of fullness and ilingo [1,2].
Tinnitus is the perception of sound in the absence of an apparent acoustic stimulus. This disease has been afflicting people since the ancient years. However, its very first description appeared in 2500 BC in Ebers papyrus. The tinnitus must always be treated as a symptom and not as a disease, which, though, must be thoroughly investigated so that its cause can be revealed. It is estimated that over 36 million American people suffer from tinnitus. The factors associated with tinnitus are the following: age, sex, race, and hearing loss. In the majority of patients suffering from tinnitus, a certain rate of hearing loss coexists, although many other factors and clinical conditions may be responsible for this symptom. Exposure to noise constitutes a common cause of tinnitus. Other causes are: Presbycussis, Meniere’s disease, chronic otitis, otosclerosis, ISSHL, acoustic neuromas, traumatic brain injury (TBI), cervical vertebral column pathology and autoimmune diseases affecting the vestibulocochlear system [3-7].
In most cases, ISSHL is viral, since it is preceded by a viral infection at a rate of 5-65 % of cases. In 1983, Wilson et al. observed seroconversion in antibodies against cytomegalovirus, varicella (chicken pox), herpes zoster virus, bordetella pertussis, measles virus, and influenza Β virus in 63 % of 122 patients suffering from ISSHL. Viruses such as cytomegalovirus, Bordetella pertussis as well as measles virus have been identified within the inner ear of patients with ISSHL. Probably an immunological or vascular factor that contributes to the pathogenesis of this disorder, coexists [8]. Though the cause and underlying mechanisms of ISSHL are not fully understood, viral infections and vascular phenomena are the most important causes, leading to compromised vascular supply, edema and hypoxia in the inner ear [9].
Standard treatment protocols cannot be followed as the pathogenic mechanism of ISSHL is not entirely comprehensible, which could lead, as a consequence, to a wide range of treatments. Only corticosteroids have been adequately accepted and they are recommended as first line treatment by most specialists worldwide [10]. Preceding reports imply that a combination of a high dose prednisolone taper additionally to an intra-tympanic dexamethasone treatment may further accelerate hearing recovery [11].
There is a wide range of additional treatment approaches such as surgical intervention, hemorheologic regimen and hyperbaric oxygenation. HBO2 can restore altered ion exchange mechanism and can relieve hypoxia of the inner ear. The effectiveness of HBO2 treatment on ISSHL, both as a primary, adjunct and as a secondary therapy, has not been completely defined through literature. The goal of this study is to investigate the effectiveness of HBO2 on the management of ISSHL [12,13].
Methods
This study constitutes a prospective observational cohort study, carried out after the approval and the urging of the University of Athens. 56 patients, matching the ISSHL definition, were selected, who, having experienced sudden hearing loss, were under medical care at the in-patient otology clinic of two general hospitals of Athens, during a period of 14 months. After having been diagnosed by a specialist, the major percentage of patients were treated with corticosteroids and with the application of a vasodilator therapy (prednisolone -75 mg per day - tapered over 12-15 days) and were referred for hyperbaric oxygenation, as outpatients, at the Diving and Hyperbaric Unit of Athens.
The population sample consists of subjects coming from the general population of Athens and of the province, as well as from various socio-economic classes.
The study has the approval of the Institution’s Bioethical Committee of the General Hospital where the research took place, as well as the consent of the participants in this study, after their having been appropriately informed of the fact that all the data reported in the questionnaires would remain strictly personal and would be confidential.
This study includes an assessment of main and secondary points. More specifically, the main assessment criteria concern changes in auditory function according to tone audiogram for the acoustic acuity measurement and the secondary assessment criteria concern changes in the intensity and quality of tinnitus, as well as the tinnitus-related quality of life.
The exclusion criteria concerned patients under the age of 15, patients suffering from infectious diseases, such as mumps, patients with traumatic brain injury (TBI) and acute acoustic trauma, acute otitis media, or damage of the tympanic membrane, Meniere’s disease, acoustic neuromas, Multiple Sclerosis, embolic or thrombotic stroke and patients to whom HBO2 should not be provided as they suffer from spontaneous pneumothorax, heavy emphysema occurring after being poisoned by CO2, upper respiratory infection with inability to equation ear infection (Valsava maneuver), patients with a history of middle ear surgery for treatment against otosclerosis, a history of seizures, uncontrolled high fever, congenital spherocytosis, psychotic illness, myocardial or pregnancy as well as hemodynamically unstable patients.
Key and important information was collected and compiled from the completion of a questionnaire given to patients by the chief nurse on their admission to the Hyperbaric Unit. The medical and nursing staff was responsible for the completion, the assessment and the evaluation of the questionnaire as well as for any further clarification. The main data concerning the evaluation of the patient’s history included demographic data (age, gender, occupation, home address, etc.), general oto-rhynologist History (allergic rhinitis, otitis, nasal congestion, Meniere's disease, etc.), general medical history (including History of vascular disease, of autoimmune and endocrine diseases), history of injury (acoustic injury, TBI, etc.), history of neoplasia (acoustic neuroma, etc.), history or reference of some habits / addictions (smoking, alcohol, etc.), medication during the week before the episode of sudden hearing loss, history of recent sudden hearing loss accompanied with the description of symptoms (vertigo, tinnitus, dizziness, etc.), the report of infection symptoms of the upper or lower respiratory tract, the activities (exposure to noise, intense stress, climbing, etc.), the nature and the type of the medication taken (which was classified into categories and doses, such as corticosteroids, vasodilators, or anticoagulant treatment in low, medium or high dose) and the previous history of hearing loss.
The level of hearing was evaluated with the use of pure tone audiogram and was considered normal when 0 to 20 dB, or was rated at a mild loss of hearing acuity when 21 to 30 dB, at a moderate loss of hearing acuity when 31 to 70 dB, at a severe loss of hearing acuity when 71 and 90 dB and at a clear loss of hearing acuity (deafness) when 91 to 110 dB.
Assessment of hearing in audiogram is carried out in four frequencies 500, 1000, 2000 and 4000 Hz. If, according to the audiogram, the level of hearing is <0, the value is placed at 0 and if it is > 100, the value is placed at 100. Then, the sum of all scores of frequencies is rated and the amount of loss of acoustic acuity is deduced. Zero is considered to be the lower score and 400 the higher score [14].
Folmer and Griest’s questionnaire, Tinnitus Severity Index (TSI), constituted the basis for the assessment of tinnitus in two theoretical levels, the first one being related to the severity of tinnitus concerning the quality of life [15,16]. The questionnaire includes 12 questions. At the end of the questionnaire there is the visual analogue scale (VAS), which refers to the intensity of the tinnitus, ranging from 0 to 10. Barely perceptible intensity of tinnitus is characterized by grade 1 whereas 10 corresponds to very high tinnitus intensity. The second theoretical level of the evaluation of tinnitus was based on a research study corresponding to the possibility of evaluating subjective idiopathic tinnitus and it relied on Glorig questionnaire (according to American Medical Association –AMA guidelines for permanent balance and impairment of equilibrium), which classifies the severity of tinnitus from minor to severe [17,18].
HBO2 therapy was performed in a multiplace hyperbaric chamber. The HBO2 protocol included five phases, each consisting of five sessions. In each session 100 % O2 was being provided at pressure of 2 ATA for 120 minutes, once daily, during five consecutive sessions per week. As far as it concerns the 1st phase, in the beginning patients were examined with an audiogram, whereas regarding the second phase they were examined at the end of it and if the evaluation of the results showed no improvement to the patients’ condition, they continued the therapy for 5 more sessions. Moreover, a month after the end of the sessions, in the third phase they were submitted at 5 more sessions with HBO2, at the end of each they repeated the examination of acoustic acuity with audiogram. Finally, during the 5th phase of the study, the patients returned three months later for the therapy and after its completion the acoustic acuity was counted.
Statistical analysis
Statistical analysis was performed with the statistical program SPSS 15.0. The continuous variables were expressed by the average (mean), standard deviation (SD) and 95 % confidence Intervals (95 % CI). The dichotomy and categorical variables were expressed by frequencies. The regularity of the variables with more than fifty cases was checked with Kolmogorov-Smirnov test and of those ones with less than fifty cases with Shapiro-Wilk test. The parametric t-test and One Way ANOVA were used for continuous variables with normal distribution in order to compare averages between independent samples and the Paired t-test was used for comparison among the same sample. As for the variables without normal distribution the nonparametric Mann-Whitney U Test was used to compare averages between independent samples and the Wilcoxon Rank test was used for comparison among the same sample. The degree of correlation between two consecutive variables was checked through the correlation coefficient Spearman's rho correlation. The bisectors and categorical variables were checked through the statistical test Chi-square test and Fisher's exact test. All cases were checked at the significant statistical level p<0.05.
Conditions of HBO2 therapy
HBO2 therapy took place in a multiplace hyperbaric chamber in a general hospital of Athens. There are three chambers all communicating between them and working through computers. They can have the maximum compression at 50 meters with 6 ATA and room for 24 people. The nursing approach of the patients in the hyperbaric chamber was according to the clinical condition, the age and the ability of each patient to adapt to a place and to the conditions of high ambient pressure. The effective and safe conduct of the treatment was based mainly on prevention which was achieved through acquisition of a detailed medical history, presentation of the place where the treatment would take place and accurate information of the patient regarding the HBO2 effect, the Changes of pressure, the temperature and the volume within the chamber, as well as the procedure and the way of equalization (valsava maneuver) of the necessary data for the initial compression.
The nurse in charge, in collaboration with the person accompanying the patient, were responsible for taking down the patient’s history, as well as for pointing out the essential differentiation points during the session. He/She recommended that the patient wear appropriate, cotton, non-synthetic clothes and noted out that, after the session, the patient should not smoke for at least 2 hours, should not take a flight, nor get to some altitude for some time, depending on the pressure and the time of exposure to the hyperbaric environment.
After completing the preparation of the patients outside the chamber, the inner attendant, along with the physician, were responsible for their examination, mostly paying attention to clinical symptoms, so that any changes of the clinical status can be reported and compared, throughout the whole duration of the treatment. In the meantime, during the initial compression, the attendant reminded the patient the process of Valsava maneuver, and other alternative maneuvers, while paying attention to avoiding ear barotrauma. Furthermore he/she was taking care of the patient position, whether he should be sitting or be horizontal with a slight elevation of the head. The inner attendant was also responsible for the maintenance of adequate ventilation – oxygenation, the connection with monitor and the frequent check of the function of human organs, particularly during the first treatments, as well as for the maintenance of relatively constant temperature for the patient, which may occur due to changes in the parameters (pressure-volume-temperature) of the hyperbaric environment. Finally, he/she had to monitor and beware of signs of CNS oxygen toxicity, such as vision disorders, tubular vision, amblyopia, hearing disorders, vertigo, dizziness, nausea and possible vomiting, muscle contractions on the face (lips) and hands as well as myoclonus jerks – convulsions and behavior changes, anxiety, restlessness, confusion and fatigue.
Results
Fifty six patients enrolled in the study (35 males/21 females). Subjects’ mean age was 42.7 years (SD ± 13.4, 95 % CI 39.1-46.3), and there was no age difference between males and females (p=0.739 t (54) =-0.334). Most of the patients (42/56) were civilians and (14/56) were military personnel. Hearing loss and tinnitus were presented initially as main symptoms in 50 % of the patients.
Vertigo, dizziness, tinnitus, heaviness-clogged ear, headache and numbness (Table 1), were the initial symptoms, about which the patients were questioned before initiating the treatment. As shown, the majority of patients experienced tinnitus (80.4 %) and a sense of heaviness-clogged ear (66.1 %).
Table 1: Initial symptoms.
| Initial symptoms |
| Symptoms |
YES % (n/N) |
NO % (n/N) |
| Tinnitus |
80.4 % (45/56) |
19.6 % (11/56) |
| Heaviness-clogged ear |
66.1 % (37/56) |
33.9 % (19/56) |
| Dizziness |
30.4 % (17/56) |
69.6 % (39/56) |
| Vertigo |
25 % (14/56) |
75 % (42/56) |
| Headache |
10.7 % (6/56) |
89.3 % (50/56) |
| Numbness |
5.4 % (3/56) |
94.6 % (53/56) |
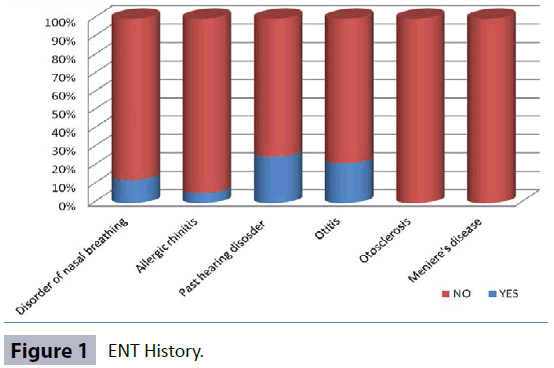
Regarding the ENT history, nearly a quarter of the total number of patients reported hearing disorders (14/56) and otitis (12/56) in the past, while the majority of patients did not face any other serious ENT diseases, such as otosclerosis and Meniere’s disease (Figure 1).
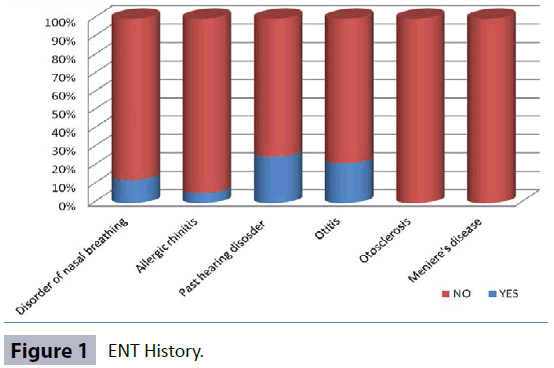
Figure 1: ENT History.
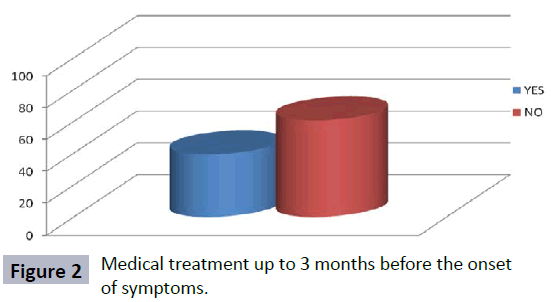
The patients at a percentage of 39.3 % (22/56) had been under some kind of medication for various health problems, up to three months before the onset of symptoms (Figure 2). More specifically, as far as it concerns corticosteroids, which are regarded as the basic traditional therapy in ISSHL, a percentage of 88.2 of the patients (45/56) were provided with them during HBO2.
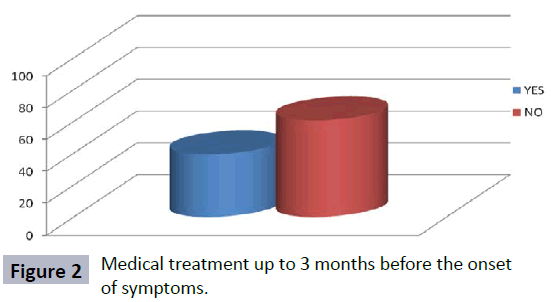
Figure 2: Medical treatment up to 3 months before the onset of symptoms.
In order to investigate the role of the use of corticosteroids in the final outcome, there was a comparison between the final audiogram and the final evaluation of the tinnitus, among patients who were receiving corticosteroids and those who were not being under corticosteroids while being in the HBO2 treatment. This comparison showed that the first group were experiencing improvement, which was characterized as mild, both in the audiogram and in the final evaluation of the tinnitus. However, this difference was not statistically significant (p=0.989 audiogram, p=0.324 final evaluation of tinnitus) (Tables 2 and 3).
Table 2: Comparison between data of those taking corticosteroids and those who don’t.
| Data of the final audiogram from patients taking corticosteroids and those who don’t |
| Final Audiogram |
Mean value |
SD |
95 % CI |
p |
| Taking corticosteroids |
164.7 |
93.0 |
136.7-192.6 |
0.989 |
| Not taking corticosteroids |
168.3 |
129.9 |
32.0-304.6 |
Table 3: The final evaluation of tinnitus after the end of the treatment between those taking corticosteroids and those who don’t.
| The final evaluation of tinnitus after the end of the treatment between those taking corticosteroids and those not receiving corticosteroids |
| Intensity of Tinnitus |
Mean value |
SD |
95 %CI |
p |
| Taking corticosteroids |
7.5 |
2.3 |
6.8-8.2 |
0.324 |
| Not taking corticosteroids |
8.7 |
3.1 |
5.4-11.9 |
The majority of patients 41.1 % (23/56) had experienced severe stress before the onset of the symptoms, while 7.1 % (4/56) and 14.3 % (8/56) had been exposed to diving or to echogenic environment respectively (Table 4).
Table 4: Activities of patients before the onset of symptoms.
| Activities of patients before the onset of symptoms. |
| Activities |
YES % (n/N) |
NO % (n/N) |
| Intensive stress |
41.1 % (23/56) |
58.9 % (33/56) |
| Exposure to sound |
14.3 % (8/56) |
85.7 % (48/56) |
| Physical activity |
8.9 % (5/56) |
91.1 % (51/56) |
| Diving |
7.1 % (4/56) |
92.9 % (52/56) |
| Mountain Climbing |
0 % (0/56) |
100 % (56/56) |
Through the comparison between the professions and the stress experienced by patients before the onset of symptoms, it was revealed that civil servants were experiencing more stress. However, this difference was not statistically significant.
The time of the symptoms’ onset before the beginning of HBO2 treatment was estimated to be 17 days (SD ± 12.5, CI: 13.7-20.4) on average. The protocol of therapy with HBO2 consisted of five phases all of which are described in the part of methodology. All 56 patients completed phase 1 and 2 of HBO2 therapy, 43 patients completed phase 3, 13 patients completed phase 4, and 6 patients completed all 5 phases. The acoustic acuity was measured, for the first time, with audiogram at the beginning of phase 1. Then, it was measured at the end of second phase, as no significant change was expected during the first phase and subsequently it was also measured at the end of every phase.
Overall, significant improvement was noted between initial and final audiogram after the application of HBO2 treatment (Mean value 239.7 vs. 164.2, p<0.001). Table 5 shows the improvement of audiogram before and after each HBO2 treatment phase.
Table 5: Initial and final audiogram data regardless of the phase of HBO2 therapy. The lower the value in the audiogram the higher the hearing acuity and vice versa.
| Data from the initial and last audiogram regardless of the phase of HBO2 Therapy |
| Audiogram |
Mean value |
SD(95%ΔΕ) |
P |
| Initial |
239.7 |
±95.6(95 % ΔΕ:214.8-264.7) |
<0.001 |
| Final |
164.2 |
±93.5(95 % ΔΕ:139.9-188.6) |
Before the therapy onset, 30.5 % of patients had normal auditory acuity and a rate of 22 % suffered from a clear hearing loss (Table 6). At the end of all treatments the above rates were at 59.3 % for the normal auditory acuity and 6.8 % for the clear hearing loss (Table 6).
Table 6: Change in the auditory acuity before and after treatment.
| Change in the auditory acuity before and after treatment |
| Classification |
Before treatment |
After treatment |
| % (n/N) |
% (n/N) |
| Normal |
30.5 % (18/56) |
59.3 % (35/56) |
| Mild loss |
11.9 % (7/56) |
10.2 % (6/56) |
| Moderate loss |
10.2 % (6/56) |
8.5 % (5/56) |
| Moderately severe loss |
13.6 % (8/56) |
10.2 % (6/56) |
| Severe loss |
11.9 % (7/56) |
5.1 % (3/56) |
| Explicit loss |
22 % (13/56) |
6.8 % (4/56) |
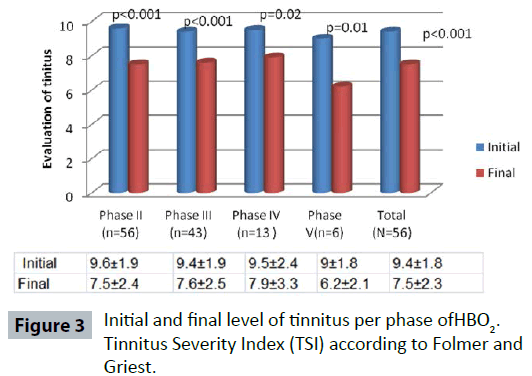
It was also noticed that after HBO2 treatment, tinnitus evaluation score, tinnitus intensity, as well as tinnitus associated problems decreased significantly (p<0.001). Overall, by comparing the initial score 9.6 (±1.9 95 % CI: 8.8-9.9) to the final score 7.5 (±2.4 95 % CI: 6.8-8.1), it was obvious that tinnitus improved significantly (p<0.001). The fact that after the end of each therapy phase a statistically major improvement was accomplished, was revealed by the internal comparison of the initial and the final score of the tinnitus per phase. Particularly, after the termination of the therapy (per phase), patients ranked tinnitus with lower score than the one existing at the initial rating (Figure 3).
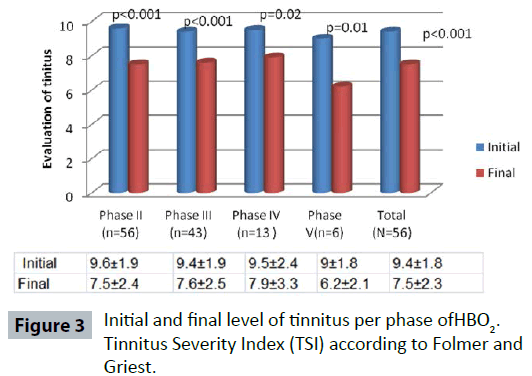
Figure 3: Initial and final level of tinnitus per phase of HBO2. Tinnitus Severity Index (TSI) according to Folmer and Griest.
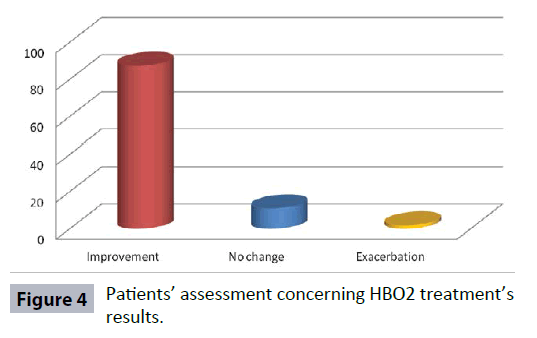
After the completion of all phases of HBO2 therapy, patients were asked to evaluate the final outcome of their condition in a qualitative scale (improvement – no change –exacerbation). The 87.3% (48/56) of patients reported an improvement of their symptoms, 10.9 % (6/56) reported no change and only a 1.8 % (1/56) reported an exacerbation of their symptoms (Figure 4).
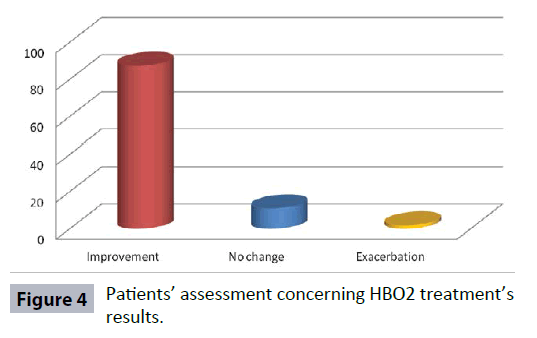
Figure 4: Patients’ assessment concerning HBO2 treatment’s results.
Discussion
The present study assessed the clinical efficacy of HBO2 combined with the standard medication on patients suffering from ISSHL. The main reason for HBO2 therapy was the abrupt hearing loss accompanied with tinnitus and a sense of load as well as of congested ear. Tinnitus appeared to be the main primary symptom in the majority of patients, a fact which was also proved in other studies that had reported its high impact on patients suffering from ISSHL. That symptom occurred to the extent that it hindered the functionality of the ear and caused severe disorder on hearing ability [4,7,19].
As far as it concerns the research data of the patients’ general history, diseases such as hypertension, hyperlipidemia, diabetes mellitus and hypothyroidism did not seem to affect the etiology of the disease. Additionally, the ENT history did not include diseases, which means that difficulty in hearing, allergic rhinitis, and other conditions did not seem to be associated with the main reason for the treatment of patients suffering from ISSHL [20]. These notes converge with the systematic review, in which researchers concluded that sex, age and morbidity do not correlate and do not affect patients suffering from ISSHL. In contrast, in another study, morbidity data is detected more frequently in the group of patients who did not improve their hearing significantly and therefore did not respond positively to HBO2 [21].
In this study, smoking constituted the most common addiction of patients. However this habit did not seem to be related to the effectiveness of the ISSHL in HBO2 because there was a statistically significant improvement to acoustic acuity as well as to tinnitus in both smokers and non-smokers. Similar research findings occurred in a study in which smoking did not seem to affect the prognosis of patients who suffer from ISSHL and are subject to treatment with HBO2. In the same study, it was reported that taking corticosteroids, in conjunction with the use of HBO2, was considered the most important factor influencing the development of ISSHL [20].
The contribution of classical pharmaceutical treatment, which consists of the corticosteroids and the vasodilators, to the treatment of the ISSHL, is acceptable by the scientific otorhinolaryngological community [22-24].
The researchers who deal with HBO2 have conducted appropriate studies into the effects of corticosteroids and of other pharmaceutical products against the application of HBO2. These studies have revealed that ISSHL therapy through the use of HBO2 is considered more effective and leads to better cure results in comparison with that where classical pharmaceutical treatment is only applied [25-29].
In the initial standard therapy of ISSHL, corticosteroids and vasodilators have also been used as part of the treatment. In addition to the conventional treatment, the application of HBO2 therapy, as an adjuvant intervention, may be beneficial [24-26,28- 30]. In the present study, in addition to the application of HBO2 therapy, the majority of the patients were provided corticosteroids and vasodilators. Due to the small number of patients taking part in the above study and the confusing effects of the interventions, the reported data should be interpreted cautiously. Bearing this fact in mind, there was a comparison between patients who had been under corticosteroids vs those who had not, with the use of audiogram. Considering the results, there was no statistically significant improvement in those who were on corticosteroids compared to those who were not. This outcome is in agreement with those ones resulting from other studies due to the fact that HBO2 combined with pharmacological treatment (corticosteroids and vasodilators) leads to a major improvement of hearing acuity, particularly in patients with severe loss of the hearing acuity [24,25,31,32].
The most crucial result deriving from this study is the amelioration in patients’ hearing acuity and it seems that it has been achieved through all the phases of the HBO2 therapy. Additionally, it was detected that patients who obviously had the worst acoustic acuity kept on HBO2 therapy until the completion of its last phase. All this is verified by a large number of studies, the majority of which regardless of the differences in the methodology, suggest that HBO2 constitutes an important treatment option of the ISSHL accomplishing an objective and clear improvement of the mean hearing loss [20,24,25,29,31,32].
The time of immediate beginning of HBO2 therapy on the first appearance of ISSHL in connection with the satisfactory recovery of hearing is regarded as a parameter of the observations of the research in literature. In this study, the HBO2 was conducted within five days and not later than thirty days from the occurrence of ISSHL (average time of the beginning of HBO2 therapy 17 days) and a clear improvement to the acoustic acuity was recorded in most patients. The findings are consistent with the results of other studies, in which it is indicated that improvement to hearing in patients with ISSHL is achieved, when the beginning of HBO2 therapy occurs two weeks after the onset of the symptoms of the disease [21,24,25,31,33-35].
Regarding the treatment protocol, the improvement of the hearing acuity is accomplished by the attendance of 25 HBO2 sessions, one session per day. This data is consistent with that of Barthelemy, et al. and Dauman et al. which indicates that there is no substantial difference in the hearing improvement if two, instead of one, HBO2 sessions, are conducted per day [33,36].
Additionally, regarding the applied HBO2 pressure, many studies and reviews concerning the treatment of ISSHL are conducted at pressure 2.0-2.8 ATA for 90-120 minutes [20,25,33]. In the present study, the treatments took place at 2.0 ATA for 120 minutes and it is worth mentioning that no side effects were reported from any patient, while at the same time an important/essential improvement in hearing was attained. The choice of pressure and the attainment of safe healing provision of HBO2, was not refuted by the study of Korpinar et al., in which side effects on the patients, who were provided with HBO2 at 2.5 ATA (15 meters therapy depth), were described and reported [20].
The improvement of the tinnitus per therapy phase and the limitation of the problems in patient’s everyday life constitute an important observation factor in this study and point out the efficacy of HBO2. Similar findings are described by Waldemar et al. [37]. Who, using three measurement instruments, along with the visual analogue scale, pointed out, that the HBO2 application combined with medication contributes positively and effectively to the improvement of the patients’ acoustic acuity and reduces tinnitus symptoms, achieving a better life.
In Porubsky et al. [38] study, the HBO2 effect on tinnitus was evaluated in relation to patients’ expectations and it was indicated that subjective elements prevailed on the positive or negative outcome and as a result they had an impact on HBO2 effect. Simultaneously a high rate of relapses of tinnitus was noticed. However, that conclusion doesn’t seem to be in agreement with the results of the present study, according to which the improvement of tinnitus corresponds to a statistically major improvement in the final audiogram. As a result subjectivity does not seem to affect the improvement of tinnitus. It is worth mentioning that an audiogram is considered a reliable implement for measuring acoustic acuity, which was used as a basic indication factor of the auditory function in this particular study. This fact reinforces objectively the interpretation of the outcome and sets the boundaries for the real hearing improvement.
Limitations
The above study was conducted using a prospective framework, No control group existed as it would demand a random assignment of the subjects to an intervention group HBO2 following possibly the traditional medication. However, bearing in mind the flow of patients suffering from ISSHL and the process of implementing the sample protocol, this study would be infeasible as it would demand a large sum of money as well as a long time for gathering a great number of patients. Moreover, the fact that the majority of patients treated at the Diving and Hyperbaric Unit of the general hospital of Athens were outpatients, not even hospitalized in the hospital, was also a reason for the lack of control group. In any case even if the random clinical testing is the chosen kind of research, which is also revealed in bibliography, the present research gives important information which leads to the justification of the effectiveness of HBO2 in ISSHL and tinnitus.
The fact of non – completion of all the treatment phases of the protocol by a great number of patients could be considered a disadvantage of this research. First of all, the high cost of the HBO2 therapy as a treating method, and, secondly, the fact that a large number of insurance companies did not cover it, were more likely the reasons which drove patients to abandoning the above treatment. Consequently, patients who often gradually improved their hearing acuity and the problem of tinnitus per phase, stopped HBO2 therapy. The co-evaluation of the criteria of the patients’ profession and residence reinforce the above - mentioned conclusions. Additionally, it should be pointed out that, according to the results of the statistical analysis, the patients who continued the therapy up to the fifth phase of the treatment protocol were those who had a higher initial audiogram.
Conclusions
The way of handling ISSHL was quite ambiguous. In international bibliography more than 60 protocols exist without any consent and agreement on the way of curing ISSHL. During the 1960s, and for more than 40 years since then, the experts in hyperbaric therapy have been studying and researching the effectiveness of ΙSSHL and it is obvious that they have gained experience in its treatment. A great number of articles have been published and strong evidence can occur only after sample studies in a big number of population. However, after a systematic review by Cochrane Collaboration of the three suggested and effective therapies (corticosteroids, vasodilators, and HBO2), only HBO2 was positively commented.
The loss of hearing is the most common cause of disability throughout the world and it often causes severe psychological and social problems as well as difficulties in work performance. Moreover the cost of education of these people causes social and economic burden. As a result, the health authorities aim at the effective cure and at the immediate recovery of the patients. Several studies have concluded that the improvement in acoustic acuity is achieved with the immediate application of HBO2 and the simultaneous use of corticosteroids and vasodilators, as HBO2 does not replace but effectively completes the common ways of treatment.
The effectiveness of HBO2 therapy in patients suffering from ISSHL, being either a primary, adjunct or secondary therapy, has not been conclusively established in the literature. This study, similarly to others studies, has shown that for people with acute ISSHL, the application of HBO2 has significantly contributed to the improvement of hearing loss and tinnitus. Therefore, it is considered a reasonable alternative adjuvant treatment along with corticosteroids and vasodilators. In addition, it is indicated that HBO2 does not substitute but completes the usual treatment methods and contributes essentially to the cure of ISSHL [10]. In future this study can be extended to a greater number of patients with the participation of more hyperbaric centers in Greece so that more people can be informed of HBO2 application.
8303
References
- Schreiber BE, Agrup C, Haskard DO, Luxon LM (2010) Sudden sensori neural hearing loss.Lancet 375: 1203-1211.
- Mattox DE, Simmons FB (1977) Natural history of sudden sensorineural hearing loss.Ann Otol Rhinol Laryngol 86: 463-480.
- Sismanis A, Stamm MA, Sobel M (1994) Objective tinnitus in patients with atherosclerotic carotid artery disease. Am J Otol 15: 404-407.
- Sismanis A, Callari RH, Slomka WS, Butts FM (1990) Auditory-evoked responses in benign intracranial hypertension syndrome.Laryngoscope 100: 1152-1155.
- Sismanis A, Butts FM, Hughes GB (1990) Objective tinnitus in benign intracranial hypertension: an update.Laryngoscope 100: 33-36.
- Sismanis A, Butts FM (1994) A practical device for detection and recording of objective tinnitus.Otolaryngol Head Neck Surg 110: 459-462.
- AthanasiadisSismanidis A (2009) Tinnitus: Clinical assessment and treatment. In: AthanasiadisSismanidis A, Otorhinolaryngology. Athens: Publications Parisiano339-349.
- Fetterman BL, Saunders JE, Luxford WM (1996) Prognosis and treatment of sudden sensorineural hearing loss.Am J Otol 17: 529-536.
- Hughes GB, Freedman MA, Haberkamp TJ, Guay ME (1996) Suddensensorineural hearing loss.OtolaryngolClin North Am 29: 393-405.
- Murphy-Lavoie H, Piper S, Moon RE, Legros T (2012) Hyperbaric oxygen therapy for idiopathic sudden sensorineural hearing loss.Undersea Hyperb Med 39: 777-792.
- Moskowitz D, Lee KJ, Smith HW (1984) Steroid use in idiopathic sudden sensorineural hearing loss.Laryngoscope 94: 664-666.
- Wei PCB, Mubiru S, Leary S (2009) Steroids for idiopathic sudden sensorineural hearing loss. Cochrane Ear, Nose and Throat Disorders Group. Cochrane Database Syst Rev.
- Battaglia A, Burchette R, Cueva R (2008) Combination therapy (intratympanic dexamethasone + high-dose prednisone taper) for the treatment of idiopathic sudden sensorineural hearing loss.OtolNeurotol 29: 453-460.
- Cocchiarella L, Anderson GBJ (2001) Guides to the evaluation of permanent impairment. 5th ed.Chicago: AMA Press. 565.
- Folmer RL, Griest SE (2000) Tinnitus and insomnia.Am J Otolaryngol 21: 287-293.
- Folmer RL (2002) Long-term reductions in tinnitus severity.BMC Ear Nose Throat Disord 2: 3.
- Figueiredo RR, Azevedo AA, Oliveira Pde M (2009) Correlation analysis of the visual-analogue scale and the Tinnitus Handicap Inventory in tinnitus patients.Braz J Otorhinolaryngol 75: 76-79.
- Werner JF, Richter B, Laubert A(1995) Some remarks on the classifications of subjective idiopathic tinnitus (SIT)-An essay toward establishing a gross-matched grating system. Int Tinnitus J1: 38-40.
- Mathieu D (2006) Handbook on hyperbaric medicine. Dordrecht, The Netherlands: Springer, France.
- Körpinar S, Alkan Z, Yigit O, Gör AP, Toklu AS, et al. (2011) Factors influencing the outcome of idiopathic sudden sensorineural hearing loss tre ated with hyperbaric oxygen therapy.Eur Arch Otorhinolaryngol 268: 41-47.
- Subbotina N, Jacobino R, Roitman D (2010) HBO and Idiopathic Sudden Sensorineural Hearing Loss and Tinnitus, UHMS Annual Scientific Meeting, USA.
- Gianoli GJ, Li JC (2001) Transtympanic steroids for treatment of sudden hearing loss.Otolaryngol Head Neck Surg 125: 142-146.
- Silverstein H, Choo D, Rosenberg SI, Kuhn J, Seidman M, et al. (1996) Intratympanic steroid treatment of inner ear disease and tinnitus (preliminary report).Ear Nose Throat J 75: 468-471, 474, 476 passim.
- Fujimura T, Suzuki H, Shiomori T, Udaka T, Mori T (2007) Hyperbaric oxygen and steroid therapy for idiopathic sudden sensor ineural hearing loss.Eur Arch Otorhinolaryngol 264: 861-866.
- Racic G, Maslovara S, Roje Z, Dogas Z, Tafra R (2003) Hyperbaric oxygen in the treatment of sudden hearing loss.ORL J Otorhinolaryngol Relat Spec 65: 317-320.
- Cavallazzi G, Pignataro L, Capaccio P (1996) Italian experience in hyperbaric oxygen therapy for idiopathic sudden sensorineural hearing loss. In: Marroni A, Oriani G, WattelF, Proceedings of International Joint Meeting on Hyperbaric and Underwater Medicine, Milano, Italy.
- Chen CY, Halpin C, Rauch SD (2003) Oral steroid treatment of sudden sensorineural hearing loss: a ten year retrospective analysis.Otol Neurotol 24: 728-733.
- Fattori B, Berrettini S, Casani A, Nacci A, De Vito A, et al. (2001) Sudden hypoacusis treated with hyperbaric oxygen therapy: a controlled study.Ear Nose Throat J 80: 655-660.
- Topuz E, Yigit O, Cinar U, Seven H (2004) Should hyperbaric oxygen be added to treatment in idiopathic sudden sensorineural hearing loss?Eur Arch Otorhinolaryngol 261: 393-396.
- Stachler RJ, Chandrasekhar SS, Archer SM, Rosenfeld RM, Schwartz SR, et al. (2012) Clinical practice guideline: sudden hearing loss.Otolaryngol Head Neck Surg 146: S1-35.
- Alimoglu Y, Inci E, Edizer DT, Ozdilek A, Aslan M (2011) Efficacy comparison of oral steroid, intatympanic steroid, hyperbaric oxygen and oral steroid + hyperbaric oxygen treatment in idiopathic sudden sensorineural hearing loss cases. Loss. Eur Arch Otorhinolaryngol 268:1735-1741.
- Domachevsky L, Keynan Y, Shupak A, Adir Y (2007) Hyperbaric oxygen in the treatment of sudden deafness.Eur Arch Otorhinolaryngol 264: 951-953.
- Barthelemy A, Bergmann E, Sainty JM (2002)Oxygenotherapie hyperbare et surdites brutales de perception. Bull Medsubhyp Sup 12:153-157.
- Lamm K, Lamm H, W. Arnold W (1998) Effect of hyperbaric oxygen therapy in comparison to conventional or placebo therapy or no treatment in idiopathic sudden hearing loss, acoustic trauma, noise-induced hearing loss and tinnitus. A literature survey. Adv Otorhinolaryngol 54:86-89.
- Aslan I,Oysu C, Veyseller B, Baserer N (2002)Does the addition of hyperbaric oxygen therapy to the conventional treatment modalities influence the outcome of sudden deafness? Otolaryngol Head Neck Surg 126:121-126.
- Dauman R, Poisot D, Cros AM, Zennaro O, Bertrand B, et al. (1993) Surditesbrusques: etude comparative randomisee de deux modes d’administration de l’oxygeno therapie hyperbareassociee au Naftidofuryl. Rev Laryngol Otol Rhinol (Bord) 114:53-58.
- Waldemar N, Zdzslaw S, Jerzy K, Czeslaw, Tomasz P (2003) Usefulness of hyperbaric oxygen therapy in patients with sensorineural acute and chronic tinnitus. Int Congr Ser 1240: 277-286.
- Porubsky C, Stiegler P, Matzi V, Lipp C, Kontaxis A, et al. (2007) Hyperbaric oxygen in tinnitus: influence of psychological factors on treatment results?ORL J Otorhinolaryngol Relat Spec 69: 107-112.