Keywords
Health care disparities, Cultural competence training, Cross-cultural medicine, Doctor-patient relationship, Junior doctor medical education, Professionalism, Health outcomes
Introduction
In the 21st century, cultural competence training has become a principal means to address health inequalities and improve health outcomes of culturally and linguistically diverse (CALD) populations in English-speaking parts of the world [1]. ‘Health inequalities’ refer to the differences in health status that can be measured and are preventable and unjust: this includes the environment, access to and utilisation of health services, and the quality of care [2]. Continuous demographic changes such as the resettlement of new waves of migrants and refugees, the cultural diversity in rural versus urban populations, and an ageing population, influence health profiles and present challenges to health service delivery. When treating patients from diverse cultural backgrounds, cultural competence training has been shown to heighten clinicians’ cultural awareness and enable them to translate their knowledge into skills thereby decreasing the risk for disparate care and poor health outcomes [3].
‘Competence’ refers to the capacity of functioning within the context of cultural beliefs, behaviours and needs of patients and their families, and carefully considers the impact of ethnicity, culture and language of both parties: each health encounter is a unique cross-cultural encounter [1]. ‘Cultural competence’ is broadly defined as creating a health workforce capable of delivering continuous, high level of care to all patients regardless of any other factors such as culture, ethnicity, gender, age, or language [4]. Clinical outcomes which are compromised by poor adherence to medication, medical errors and lack of follow-up can be significantly improved when limited health literacy and cultural differences are addressed [4]. Culturally competent clinicians promote patient health outcomes when using communication models based on patient participation in health care decision-making: this boosts patient adherence to management plans and attracts higher patient satisfaction ratings during episodes of care [5,3].
A Review of Current Cultural Competence Models in Health Care
While cultural competence training of the clinical workforce has become a professional imperative, the goal of integrating culture into clinical care remains largely elusive [5-7]. Culturally competent care is not visible in everyday practice: a recent Australian study revealed clinical supervisors were unable to define cultural competence and could not apply the concept to teaching junior doctors to become culturally competent in the hospital setting [6,7]. Difficulties include: the fluid use of terminology as new terms are coined and used interchangeably: ‘cultural’ is often followed by awareness, sensitivity, practice, safety, respect, security, diversity and humility, with a more recent emphasis on ‘competence’ [8-10] confirm ‘there is no uniform definition or framework of cultural competence that is accepted across the spectrum of health contexts/settings either within or between countries.’
Although most definitions of cultural competence include an aspect of culture, different terms have diverse meanings, and in its practical application, they vary in focus. For example, cultural awareness training emphasises the positive aspect of cultural diversity and activities focus on drawing attention to a culturally diverse population via cultural artefacts (e.g. food, beliefs, religious practices, dress). However, cultural competence goes further than awareness as it focuses on how multi-disciplinary health professionals can collaborate to ensure the best health outcomes for all patients, regardless of cultural background and language, age and gender, education and income [4,5]. Many models are critiqued because they: i) conflate culture with ethnicity; ii) fail to consider the diversity of individuals within a single culture; iii) exaggerate cultural differences; iv) overlook biomedicine as a cultural system; v) view culture as static; vi) simplify culture as a ‘list of traits’; and vii) examine fragmented and out of context versions of the communication exchange in the clinic [5,6] Lee and Farrell [11] argue while popular models encourage health professionals to act sensitively to cultural differences, they limit culture to a list of characteristics thereby ‘effectively denying the changing, multifarious, integrated and interact[ional] nature of identity’. Epner and Baile [5] remind us that ‘Culture is inseparable from economic, political, religious, psychological and biological conditions.’
Methodology
From our previous study [12] it emerged that junior doctors by and large did not receive cultural competence training from their clinical supervisors. As described above, the literature review provided the foundation for the structure of the new and improved three-tier Continuum Model which was developed and piloted during 2010. From January 2011 onwards until now the model has been adopted for the purpose of cultural competence training of about 255 junior doctors at Darling Downs Hospital and Health Service in Queensland, Australia: this included interns (157), medical residents and registrars (45), and international medical graduates (53). Verbal and written feedback was sought from each participant immediately following the training session by administering a one page evaluation which was divided into three sections. Feedback was sought on the intellectual quality (interactivity, depth of understanding, complexity of concepts), the learning environment (audience engagement, collegial environment, intellectual content), and any other comments. Observations could be made with regard to what was most enjoyable about the workshop and where improvements might prove helpful. Evaluations provided a significant contribution to the quality assurance process and assisted in gauging the uptake and success of this training activity.
The continuum model of cultural competence
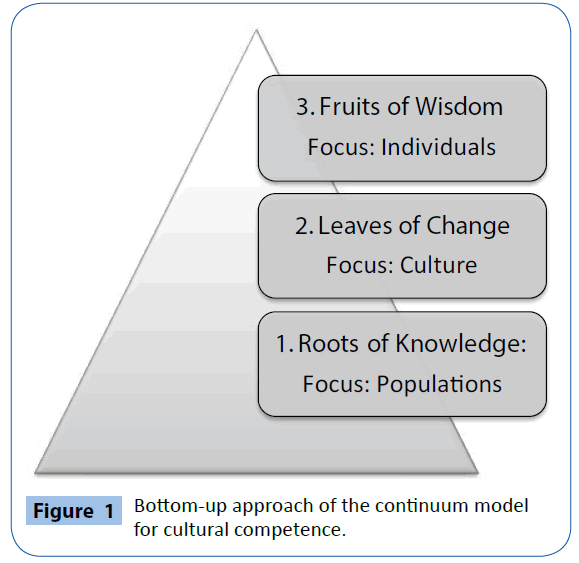
The current international discourse on cultural competence provided the knowledge base for a newly conceptualised Continuum Model; consisting of three distinct workshops and themes (Table 1). The Continuum Model serves as a training guide to address the complexity of cultural competence in clinical care for health professionals, by suggesting educational content and linking it to educational outcomes: thus linking theory to practice. The symbolic nature of a tree with roots (of knowledge), leaves (of change), and fruits (of wisdom) serves as the foundation for this model which divides into these themes using a bottom-up approach (Figure 1). For each theme a half-day workshop is suggested. Alternatively, a blended delivery model which consists of an online course component (2 hours) followed by a face-to-face teaching session/workshop (1 hour) allows for more flexibility and encourages greater participation given health professionals’ clinical commitments. Depending on clinicians’ prior knowledge, each workshop can be shortened or expanded to fit in with variations in training requirements. For example, ‘Roots of Knowledge - Culture and Population Health’ represents an innovative yet essential component not usually included in previous cultural competence training approaches.
| Workshop |
Population Health Profiles |
Core Competencies |
1 Roots of Knowledge:
Culture and Population Health |
•Australian census data on the national, state, regional and local population and cultural diversity
•Epidemiology: current trends in the health of culturally and linguistically diverse (CALD) populations: migrants, refugees, newly emerging and Indigenous communities
•Equity and access to health services
•The social determinants and gradients of health
•The relationship between culture and health: implications for health service delivery |
•Promote knowledge on regional cultural diversity and health profiles
•Explore health inequalities and access to health service are explored
•Examine the socio-cultural context of health inequalities
•Enable more complex, nuanced understanding and analysis of socio-economic and cultural barriers for patients
•Build awareness of social justice issues and how clinicians can use this information to improve health service delivery |
| Workshop |
The Changing Nature of Culture |
Core Competencies |
2 Leaves of Change:
Cultural Concepts in the Context of Change |
•Examination of core concepts central to the understanding of culture and cultural competence
•Culture in context: clinicians and patients navigating the cultural chasm
•The mediating and changing nature of culture
•Moving away from cultural ‘facts’ and cultural ‘do’s’ and ‘don’ts’
•Valuing diversity and similarity: each health encounter is a unique cross-cultural encounter
•Models of health and illness including biomedicine |
•Perform critical analysis of key concepts - essential for assessment and application
•Engage clinicians in cultural self-assessment at the individual level
•Examine the role of specific knowledge on cultures versus generic knowledge
•Alert clinicians to the over-simplification of culture for addressing bias, racism, prejudice and cultural stereotypes
•Undertake comparative analysis of patients’ and clinician’s health belief frameworks |
| Workshop |
Culturally Competent Care
in the Clinical Setting |
Core Competencies |
| 3 Fruits of Wisdom: In the Clinic: Clinicians and Culturally Competent Care |
•Patient-centred care in context: individualised health interventions
•Culture in the clinical encounter (e.g. health beliefs, religion, diet, physical activity)
•Intercultural and cross-cultural communication styles/power differentials
•The patient’s illness narrative
•CALD and indigenous patients with English as a 2nd, 3rd or 4th language
•Health literacy
•Informed consent
•The social, psychological and economic impact of illness on patients, families, communities
•Empowering patients |
•Adapt health service delivery to match each patient’s needs
•Implement communication strategies: active listening and questioning skills, visual clues, differences in time allocation
•Develop strategies for the provision of health information at the right level
•Apply appropriate interpreter referrals
•Provide patient support, follow-up and collection of confidential patient feedback
•Ensure patient (and family) input in health care decision-making, offering culturally competent solutions
•Teach junior medical staff on how to become culturally competent
•Explore the impact of power/gender differentials between patients and clinicians |
Table 1: Continuum model of cultural competence for clinicians.
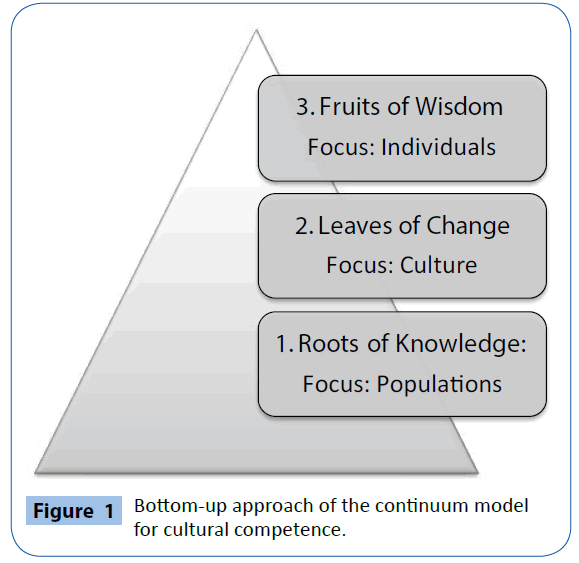
Figure 1: Bottom-up approach of the continuum model for cultural competence.
Theme 1: Roots of Knowledge – Culture and Population Health, explores the health of ethnic and marginalised groups; this approach provides a rich learning experience from which many lessons for clinical practice can be drawn. Discussion topics include the health of refugees, migrants, CALD and Indigenous people by examining recent trends in morbidity and mortality, equitable access to services for various urban and rural population groups by gender, age and education, as well as the predisposition of sub-population groups to high morbidity and premature mortality due to the social determinants of health. Migrant and Indigenous populations from around the world (e.g. United States, Canada, United Kingdom, New Zealand, Australia), have experienced marginalisation and health inequalities with regard to health insurance, access to care, life expectancy, and are affected by high rates of acute and chronic diseases [13-16].
In Australia for example, the incidents of chronic morbidity due to cardiovascular disease, diabetes, infectious diseases as well as health risk factors (e.g. smoking, alcohol use, physical activity, overweight and obesity) for indigenous people are significantly higher than for non-indigenous people [13]. For these vulnerable populations the provision of culturally competent health services is critical: current variable health outcomes are exacerbated by inadequate access to and variable understanding/affordability of medications, their efficacy and side-effects, low health literacy skills and English communication skills, poor instructions on labelling, medical terminology, and complex drug regimens. When medications are not adequately adhered to (and result in hospital re-admissions) then the associated behaviour is referred to as non-compliance. The use of this term is unsuitable as it assigns all responsibility to the patient for not ‘complying’ and masks variable standards of inadequate service provision at the point of care [17,18].
Research has demonstrated that patients with the same illness have very different outcomes [19]. The aim of this workshop is to provide clinicians with an overview of the complexity of health experiences and alert them to health problems within their own practice and geographic region, to examine morbidity and mortality patterns among at risk groups, plus cross-cultural, language and communication factors, so that they can modify their approach to patient-centred care [5,20]
The issue of social justice is at the forefront of discussions, and practical activities focus on the social determinants of health. With increased awareness, clinicians can work more actively on reducing health inequalities and inequities (e.g. improved primary care by offering at risk patients appropriate screening and intervention), recognising the need for clear communication, providing extra health information (oral, written and in multiple languages), increased use of interpreter services, more frequent referral to members of multi-disciplinary health care teams, and ensuring follow-up to reduce hospital re-admissions. Clinicians will also become cognisant that most determinants of health are outside the jurisdiction of the health system (e.g. income, education, private health insurance, transport, housing, the cost and availability of medicines, geographic isolation, accessibility to health services), and therefore recommend more realistic expectations on what can reasonably achieved for inpatients and outpatients.
Theme 2: Leaves of Change - Cultural Concepts in the Context of Change, the dynamic nature of culture and its influence on health is explored. Culture shapes health-related beliefs, behaviours and values, and is relevant in the clinic with regard to diagnosis, treatment and care [21]. A richer, more nuanced conceptualisation of culture within the social context is essential to develop a more structural understanding of this concept; to avoid a simplistic equation of culture with ethnicity. In the health care context, patients belonging to a particular ethnic group may not share many commonly observed characteristics and therefore individual differences should not be dismissed as random, idiosyncratic and meaningless [22]. Cultural labels which prescribe what to do and not to do for a particular group of patients (e.g. Japanese, Arab) in terms of treatment are not very helpful as they mask diversity and focus on similarity. This is demonstrated by Kleinman & Benson [6] in the case of a Mexican HIV positive male patient with a 4 year-old HIV positive son who failed to attend clinics to receive adequate care. Non-clinic attendance was not attributable to cultural differences (health beliefs, being Mexican) but rather to socio-economic factors such as lack of time (the need to work long shifts/hours) and low income from a job as a bus driver. Biomedicine is also a health belief model: every health care encounter is a cross-cultural encounter and clinicians need to become aware of their own beliefs and values (e.g. when patients request a complimentary medicine approach such as herbalism, homeopathy).
Theme 3: Fruits of Wisdom – Clinicians and Culturally Competent Care, offers pathways for clinicians on how to achieve culturally competent health care and optimal health outcomes for culturally diverse patients. Quality in clinical care involves recognising the patient’s problem, diagnosis, management and follow-up. These are especially challenging where culture plays a role: differences in language, education, health literacy and health beliefs can affect communication between clinician and patient, making it more difficult to grasp quickly what the problem is. Lack of problem recognition delays the provision of timely and appropriate care; when incomplete, subsequent diagnosis, management and follow-up will be inadequate [20].
Vulnerable CALD populations experience a greater burden of disease, psychological distress and social problems; have higher risk factors (e.g., poor diet, physical inactivity, smoking); lack knowledge to access services in a timely manner; and are often unaware of health-promoting behaviours and preventive screening practices as these may not be formally practised in their countries of origin (e.g. applying sunscreen on sunny days, Pap smears, bowel cancer screening) [23-26]. Clinicians caring for these patients require additional time to: elicit patients’ expectations and perspectives; complete an examination; give advice on primary health care and behavioural risk factors (e.g. nutrition, alcohol use); confirm patients’ understanding of their condition(s) and health care; address language barriers (e.g. using interpreters and translated health information); establish a rapport; reduce social and cultural distance by building trust and goodwill; coordinate and improve access to care; and encourage greater patient self-efficacy and follow-up visits [20,27]. However, during periods of stress and time-pressure, clinicians are challenged to address the complex needs of patients and are more likely to resort to stereotypical thinking, conforming to preconceived notions and disconfirming data; and fostering miscommunication and misunderstanding. This situation arises due to disagreements about the illness, its treatment and the patient’s role in health care, and may potentially compromise patient-centred care. Clinicians are encouraged to: adapt their health service delivery at the point of care to each patient’s individual needs in terms of their diagnosis, treatment and management; pay attention to their communication style; address any disparities in health literacy; and improve equitable access to services.
The implementation and evaluation of the continuum model
The Continuum Model’s 3-step approach offers a practical roadmap of continuous learning, explores and reinforces key educational content, and through reflection, assists clinicians in their transition from cultural awareness to cultural competence. After piloting the Continuum Model in 2010, the revised version was administered to junior doctors during cultural competence training from January 2011 onwards. Due to time pressures restricting junior doctors’ protected education time to two hours per week, a blended delivery approach of cultural competence training has been introduced which combines online learning of two hours with a face-to-face workshop of one hour. The online learning management system at our health service (DDLOL is an acronym for Darling Downs Learning Online) is accessible to all doctors including junior doctors and offers a flexible learning platform. A two hour module of pre-reading materials for each of the themes has been uploaded; it is comprised of professional literature, video-recordings of presentations and quizzes. Each online module is then followed by an interactive workshop delivered by a trained facilitator (GB) in which content is linked to medical practice for discussion and reflection.
A brief one page evaluation was administered at the conclusion of each workshop as a means of quality control. Evaluation data has so far been collected from at least 255 junior doctors with a total of 11 questions on three domains: intellectual quality, learning environment and open-ended comments where notes could be made about any aspect of the training. Junior doctors overwhelmingly agreed that the combination of online content and interactive workshop assisted them to reflect on their own practice and increased their understanding of how to deliver patient-centred care to vulnerable, culturally diverse patients. Junior doctors also found the training intellectually engaging because it clarified their understanding of cultural competence and promoted ways in which it could be applied to new clinical situations. The learning environment was described as supportive, amidst an atmosphere of mutual respect and understanding, the interaction was seen as intellectually engaging and taking place within a collegial environment. Comments such as “relaxed and relevant”, “linked to discussions” and “interactive and interesting” were frequently listed. Many doctors also observed that the concept of cultural competence was not clearly understood while they were at medical school while others said that they did not remember studying course content on cultural competence.
By and large junior doctors themselves perceived that they were able to increase their level of cultural competence; and the workshop facilitator (GB) made similar observations. During workshop discussions it became evident that most junior doctors only possessed a vague notion of what it meant to provide culturally competent health care to patients, though there were subtle differences in doctors’ prior levels of understanding. Overall doctors appeared to be aware of the culturally diverse population in the health service district but lacked a guided and specific approach on how to address potential and existing health disparities. After training their understanding was enhanced and they were able to employ a variety of practical and helpful strategies to improve their effectiveness in the clinic thus making progress towards improving health outcomes of their patients.
Conclusion
Cultural competence is defined by complexity: it moves seamlessly between different cultures, worldviews and health belief models, and regards each individual patient and health care encounter as a unique opportunity for clinicians to provide patient-centred care. The key outcomes of the Continuum Model are aligned with the Australian Safety and Quality Framework for Healthcare; including patient-centred care, access and equity to services, safety and quality, and workforce training [28]. For the multidisciplinary health care team, particular areas of action have been identified: increasing health literacy; addressing patient/ family/carer input into healthcare decision-making; providing care which is culturally sensitive and respects cultures; and improving the continuity of care [29]. It will remain a constant challenge for clinicians to incorporate the dynamics of cultural difference in patient-centred care and reduce health inequalities experienced by CALD patients. The Continuum Model focuses on how cultural competence skills can be acquired by clinicians to boost patients’ trust, satisfaction and health outcomes.
6741
References
- Like RC(2011) Educating clinicians about cultural competence and disparities in health and health care.J ContinEduc Health Prof 31: 196-206.
- Carter-Pokras O,Baquet C (2002) What is a "health disparity"?Public Health Rep 117: 426-434.
- Carol M, Julie C, Sandra G, Sheila C, Peter G, et al. (2010) Treating and Precepting with RESPECT: A Relational Model Addressing Race, Ethnicity, and Culture in Medical Training. J Gen Intern Med 25: 146-154.
- Betancourt JR, Green AR (2010) Commentary: linking cultural competence training to improved health outcomes: perspectives from the field.Acad Med 85: 583-585.
- Epner D E, Baile WF (2012) Patient-centered care: the key to cultural competence. Ann Oncol 3:33-42.
- Kleinman A, Benson P (2006) Anthropology in the clinic: the problem of cultural competency and how to fix it.PLoS Med 3: e294.
- Teal CR, Street RL (2009) Critical elements of culturally competent communication in the medical encounter: a review and model.SocSci Med 68: 533-543.
- Grant J, Parry Y, Guerin P (2013) An investigation of culturally competent terminology in healthcare policy finds ambiguity and lack of definition.Aust N Z J Public Health 37: 250-256.
- Thackrah RD, Thompson SC (2013) Refining the concept of culturalcompetence: building on decades of progress.Med J Aust 199: 35-38.
- Truong M,Paradies Y, Priest N (2014) Interventions to improve cultural competency in healthcare: a systematic review of reviews.BMC Health Serv Res 14: 99.
- Lee SA, Farrell M (2006)Is cultural competency a backdoor to racism. Anthropology News 47: 9-10.
- Berger G, Conroy S, Peerson A, Brazil V (2014) Clinical supervisors and cultural competence.Clin Teach 11: 370-374.
- Australian Bureau of Statistics (2013) Australian Aboriginal and Torres Strait Islander Health Survey: First Results, Australia, Canberra, ACT, Australia.
- Kagawa-Singer M,Kassim-Lakha S (2003) A strategy to reduce cross-cultural miscommunication and increase the likelihood of improving health outcomes.Acad Med 78: 577-587.
- Mortensen A(2010) Cultural safety: does the theory work in practice for culturally and linguistically diverse groups?NursPrax N Z 26: 6-16.
- Reading J,Nowgesic E (2002) Improving the health of future generations: the Canadian Institutes of Health Research Institute of Aboriginal Peoples' Health.Am J Public Health 92: 1396-1400.
- Davidson PM, Abbott P, Davison J, Digiacomo M (2010) Improving medication uptake in aboriginal and Torres Strait islander peoples.Heart Lung Circ 19: 372-377.
- Hamrosi K, Taylor SJ, Aslani P (2006) Issues with prescribed medications in Aboriginal communities: Aboriginal health workers' perspectives.Rural Remote Health 6: 557.
- Friel S, Marmot MG (2011) Action on the social determinants of health and health inequities goes global.Annu Rev Public Health 32: 225-236.
- Fiscella K, Epstein RM (2008) So much to do, so little time: care for the socially disadvantaged and the 15-minute visit.Arch Intern Med 168: 1843-1852.
- Kleinman A, Eisenberg L, Good B (1978) Culture, illness, and care: clinical lessons from anthropologic and cross-cultural research.Ann Intern Med 88: 251-258.
- Lo MC, Stacey CL (2008) Beyond cultural competency: Bourdieu, patients and clinical encounters.Sociol Health Illn 30: 741-755.
- Australian Institute of Health and Welfare 2014 (2014) Australia's Health 2014 Australia's Health Series No 14. Cat.no. AUS 178. Canberra: AIHW, Australia.
- Dart J (2008) Australia's disturbing health disparities set Aboriginals apart.Bull World Health Organ 86: 245-247.
- Harris M, McDonald J (2009) Health care reform - Facing inequities.AustFam Physician 38: 911-912.
- National Preventative Health Taskforce(2008) Australia: The Healthiest Country by 2020: A Discussion Paper. Canberra: Commonwealth of Australia,Australia.
- Starfield B,Gérvas J, Mangin D (2012) Clinical care and health disparities.Annu Rev Public Health 33: 89-106.
- Australian Commission on Safety and Quality in Health Care (2010) Australian Safety and Quality Framework for Health Care, Australia.
- Australian Commission on Safety and Quality in Health Care (2010) Putting the Framework into Action: Getting Started - Activities for the Healthcare Team, Australia.