Research Article - (2024) Volume 16, Issue 1
The effect of continuous positive airway pressure on depressive symptoms in obstructive sleep apnea
Sheikh Shoib1,
Javid Ahmed Malik2 and
Ilham Zaidi3*
1Department of Health Services, Srinagar, Kashmir, India
2Department of Pulmonary Medicine, SKIMS Medical College Bemina, Srinagar, India
3International Society for Chronic Illnesses, New Delhi 110001, India
*Correspondence:
Ilham Zaidi,
International Society for Chronic Illnesses, New Delhi 110001,
India,
Tel: 919811629859,
Email:
Received: 22-Jan-2024, Manuscript No. IPAOM-24-14522;
Editor assigned: 25-Jan-2024, Pre QC No. IPAOM-24-14522 (PQ);
Reviewed: 08-Feb-2024, QC No. IPAOM-24-14522;
Revised: 07-Mar-2024, Manuscript No. IPAOM-24-14522 (R);
Published:
14-Mar-2024
Abstract
Objective: Research on the connection between depression and Obstructive Sleep Apnea (OSA) has not been particularly focused. This study looked into possible links between continuous positive airway pressure, or CPAP, and depression in people with OSA.
Methods: Between July 2011 and August 2013, 47 inpatients with OSA who were referred from various specialty clinics underwent polysomnography testing. The patients were assessed using the Mini International Neuropsychiatric Interview (MINI plus). The Montgomery Asberg Depression Rating Scale (MADRS) was employed for follow-up evaluations among patients who had received a diagnosis of depression. In this study, the effect of CPAP on depressive symptoms in individuals with OSA was evaluated at baseline, three months, and six months following the initiation of therapy.
Findings: When comparing pre-CPAP and the conclusion of the CPAP course by 9.1, the 3-month follow-up by 14.4, and the 6-month follow-up by 18.7 (all p < 0.01), there were notable differences in the mean MADRS scores.
Conclusions: Following CPAP treatment, many OSA patients saw a considerable reduction in their MADRS scores. CPAP's ability to lessen depressive symptoms raises the possibility that mood disorders in individuals with OSA are not solely caused by physical symptoms. The amount of evidence demonstrating the connection between depression and OSA is increased by this study.
Keywords
Positive airway pressure; Depression; Obstructive sleep apnea
Highlights
• OSA's public health impact demands attention.
• OSA and depression: Unraveling a complex connection.
• CPAP: Beyond OSA treatment, a potential depression solution.
• CPAP's enduring impact: A 6-month reduction in depressive symptoms.
• Research shift: CPAP emerges as a vital depression intervention.
Introduction
Obstructive Sleep Apnea (OSA) is the most common type of
sleep apnea. It is easily identified by its characteristic snoring and
frequent episodes of partial or total obstruction of the upper airway
during sleep. According to Malik et al. [1] and Prasad et al., [2] these
events interfere with sleep cycles and occasionally cause hypoxia
at night. Because of its high rate of morbidity and death, OSA is
a serious public health concern [3-5]. General population often
ignores OSA, which results in an under diagnosis and, ultimately,
insufficient treatment [6,7].
A significant number of people with OSA are misdiagnosed,
with 93% of females and 82% of males not having an official
diagnosis, per the study [7,8]. Moreover, people with OSA
frequently experience worse health-related quality of life,
cardiovascular problems, reduced neurocognitive function, and
additional metabolic dysfunctions [9-12]. There is now knowledge
that depression and OSA can affect a patient's overall health as well
as the course of their disease, according to recent studies [13-16].
Depression is a prevalent medical illness that is frequently
disregarded and does not receive adequate treatment, according to
Shoib et al. [17]. There is constant debate on the occurrence of
depression in people with OSA, particularly when such people also
have other chronic diseases. There is no clear evidence linking OSA
with depression, despite some study suggesting that a significant
percentage of patients with OSA who also have depression do not
receive therapy (20–63%) [18-20].
Even though the majority of research indicates a link between
depression and OSA, methodological limitations have been
identified. These include small sample sizes and variation in
the evaluation methods, such as questionnaires and ratings for
depressive symptoms. To address the complex relationship between
OSA and depression, longitudinal follow-up studies that track
changes in depression status following OSA treatment are required.
Continuous Positive Airway Pressure (CPAP) has been shown to
be the most successful non-pharmacological treatment for Open-Source respiratory disease (OSA) [21,22]. Varied health problems
related to OSA, such as heart disease, stroke, diabetes, metabolic
syndrome, and auto accidents, can be effectively prevented or
treated using CPAP. Moreover, it lessens the psychological and
physical symptoms brought on by OSA [23,24]. Moreover,
research has linked CPAP therapy to enhancements in general quality of life and cognitive function [21]. Continuous positive
pressure breathing has been shown in numerous interventional
investigations to reduce depression levels [20,25,26].
Research on the relationship between depression symptoms
and CPAP therapy for OSA, however, has yielded inconsistent
findings [23,27,28]. Therefore, a large-scale randomised controlled
trial using validated scales to quantify depressive symptomatology
is required to evaluate the efficacy of CPAP treatment for OSA.
Depression symptoms may be significantly reduced by effective
CPAP treatment for OSA, which may have significant clinical
implications. To completely understand how OSA can alleviate
depression, more research is required. Despite a multitude of
epidemiologic and clinical investigations exploring the relationship
between the two disorders, it remains unclear if depression is a
distinct clinical phenomenon associated to OSA or if depression
is a cause of OSA. This could occur if concurrent symptoms are
misconstrued. This study not only looks at how CPAP affects
depressed symptoms in OSA patients, but it also raises a hypothesis
that ought to be looked into in a long-term surveillance research to
clarify how depression and OSA are related.
Materials and Methods
Setting
The investigation was carried out in India's Modern Hospital
Srinagar, a private medical facility called Rajbagh. The professional
staff at this hospital is paid on a salary basis and provides a wide
range of general care and specialty services. Patients are referred to
Modern Hospital from all over the state of Jammu and Kashmir
since it is the only facility in the area that provides routine
polysomnographic testing with a certified laboratory. In terms of
race, the study participants from Modern Hospital are thought to
be representative of the population.
Study design
Forty-seven OSA patients participated in our non-controlled
prospective interventional experiment. Based on inclusion and
exclusion criteria, patients diagnosed with depression and prescribed
CPAP were assessed. The Mini International Neuropsychiatric
Interview (MINI plus) scale was used for the initial assessment
of each patient [29]. Those who scored positively for depression
on the MINI plus scale were subsequently evaluated using the
Montgomery Asberg Depression Rating Scale (MADRS) at three
and six months' follow-ups, as well as before and after the most
recent CPAP cycle [30].
Patient selection
Between July 2011 and August 2013, Polysomnography (PSG)
testing was performed on every patient referred from different
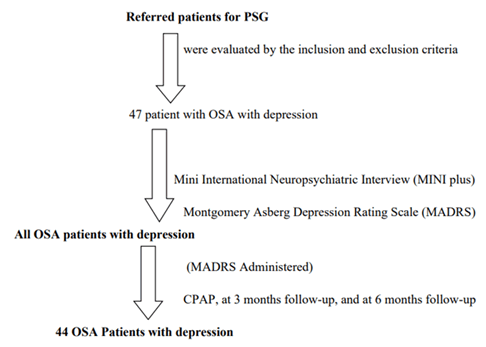
specialist clinics. The participant selection process is depicted in Figure 1.
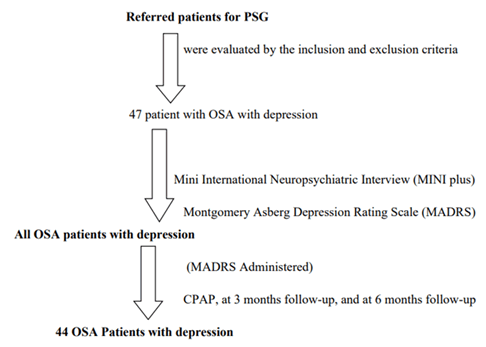
Figure 1: Participants enrollment flowchart.
Prior to the PSG experiment commencing, participants provided
informed consent. An overnight PSG was performed using a
computer-based technique to evaluate sleep-disordered breathing.
On the first visit for presenting problems, sociodemographic
information, general medical history, and clinical data, including
polysomnography results, were recorded. The diagnosis and severity
of OSA were then ascertained using an overnight laboratory PSG.
Every patient had PSG recordings for a minimum of seven hours,
starting and stopping in time with their normal home sleep cycles.
Recordings of polysomnography
Polysomnography examinations yielded a wealth of physiological
data. A few of these were the ECG, six EEG channels, bilateral
electrooculograms, chin and tibialis electromyograms, piezo
electrodes to track movements of the wall of the belly and chest,
oronasal thermocouples, and a nasal pressure transducer to
assess airflow. The data was visually evaluated by an experienced
researcher who was blind to the study's findings. The recordings
were visually evaluated at 30-second intervals during REM sleep
and non-REM sleep stages S1 through S4, using predetermined
scoring criteria. Hobson J [31]. Furthermore, microarousals and
respiratory episodes were rated using a set of criteria. Bonnet M
and Lemons W [32].
Hobson JA quotes the definition of sleep provided by
Rechtschaffen and Kales. According to Stammling, a ten-second or
longer breathing stop could be a sign of apnea. A 50% reduction in
thoracic-abdominal motions and a 4% drop in oxygen saturation
were considered indicators of hypopnea. The number of apneas and
hypopneas per hour of total sleep time was used to compute the
apnea/hypopnea index, or AHI. To be diagnosed with obstructive
sleep apnea, a person must have an AHI of five or more apneas
or hypopneas per hour. Daytime weariness was measured using
the Epworth sleepiness scale [33]. A score of nine or above on the
Epworth scale was considered excessive daytime sleepiness. OSAS
is the term used to describe the condition where the sum of the ESS
Score and AHI is greater than 9. The total number of desaturations
of at least 3% for each hour of sleep was used to determine the
oxygen desaturation index, or ODI. Based on commonly accepted
clinical cutoffs, the severity of OSA was categorised into four
groups: No OSA (AHI<5), mild OSA (AHI ≥ 5 but <15), moderate
OSA (AHI ≥ 15 but <30), and severe OSA (AHI ≥ 30).
Psychiatric diagnoses were first made using the Mini International
Neuropsychiatric Interview (MINI plus) scale [29]. Patients with
a diagnosis of depression were evaluated using the Montgomery
Asberg Depression Rating Scale (MADRS) [30]. A consultant
psychiatrist verified the presence of mental health conditions.
Every patient gave their informed consent, which was collected
verbally and in writing. The MADRS was used to assess patients
the day following their last visit, three months later, and six months
later. Preliminary interviews and information sheets made it clear
that providing or withholding consent would not affect the course
of treatment. Every piece of patient data, including demographic
data and generic descriptors, was entered into a semi-structured
case sheet.
Prior to data processing, patient names were substituted with
distinct identification numbers in order to protect participant
identity.
Montgomery Asberg depression rating scale
The severity of different depression symptoms is measured
using the 10-point MADRS scoring system. There are six possible
scores. Suicidal thoughts, anxiety, agitation, tension, appetite,
energy, mood, sleep, and depression are a few of the symptoms.
According to Montgomery and Asberg [30], with seven to nineteen
standing for minor depression, twenty to thirty-four for moderate
depression, and thirty-four or more for severe depression.
None of the trial participants with a diagnosis of depression were
receiving therapy for their illness at the time of CPAP. Below is a list
of the study's inclusion and exclusion criteria.
Inclusion criteria
• Individuals who have been diagnosed with obstructive sleep
apnea.
• Individuals experiencing depression.
• Participants who have provided written consent to engage
in the research and individuals of both genders.
Exclusion criteria
• Patients who have previously undergone upper airway
surgery.
• Patients undergoing oral appliances or positive airway
pressure therapy.
• Patients whose diagnosis is unknown.
• Patients who are already on nocturnal oxygen
supplementation.
• Subjects who did not provide informed agreement to
participate in the trial.
Ethical compliance
The study was authorised by the ethics council of Sher-i-
Kashmir Institute of Medical Sciences (SKIMS Srinagar), located
in Srinagar, India.
Statistical analysis
The Levene test was used to evaluate variance following
the completion of descriptive statistical analyses pertaining
to the general characteristics of the research participants. The
Kolmogorov-Smirnov test was then used to look at the variable
distribution. When at least one cell had an anticipated count of
less than five, the qualitative variables were evaluated using the χ2 test or the Fisher exact test. When comparing the mean values of
quantitative variables with normal distributions, student t tests
were employed; for variables with non-normal distributions,
Mann Whitney U tests were utilised. Student t-tests were utilised
for continuous data in paired samples, and McNemar tests were
performed for categorical data run. The Pearson correlation
coefficient was utilised to investigate the relationship between the
quantitative variables. At P values <0.05, statistical significance
was acknowledged. The Pearson correlation coefficient was utilised
to investigate the relationship between the quantitative variables.
Utilising SPSS 11.0, the analyses were carried out.
Results
The study participants were 58.6 ± 14.7 years old on average.
There were 27 women (57.4%) and 20 males (42.6%) in the group.
The PSG findings are summarised in Table 1.
| Mean ± SD |
|
| Age (years) |
58.6 ± 14.7 |
| AHI |
26.0 ± 10.5 |
| ESS |
5.7 ± 3.2 |
| Sleep efficiency (percent) |
68.5 ± 9.4 |
| Sleep latency (minutes) |
24.3 ± 10.1 |
| REM sleep latency (minutes) |
78.8 ±14.5 |
| ODI (percent) |
24.8 ± 14.5 |
| Awake SpO2 (percent) |
92.5 ± 4.0 |
| Nocturnal SpO2 (percent) |
84.6 ± 6.4 |
| Gender (number (%)) |
Male |
20 (42.6%) |
| Female |
27 (57.4%) |
| Note: SD: Standard Deviation; AHI: Apnea/Hypopnea Index; ESS: Epworth Sleepiness Scale; REM: Rapid Eye Movement; ODI: Oxygen Desaturation Index |
Tab. 1. Basic characteristics and polysomnography findings of the study population.
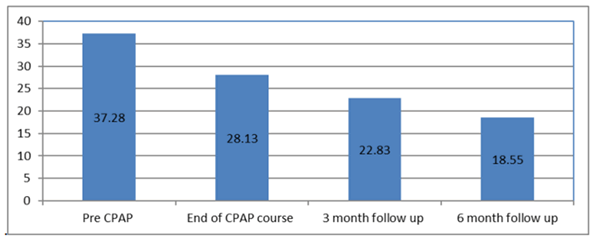
Table 2 displays the mean MADRS scores of patients who
suffer from depression. At the six-month check-in, the MADRS
scores after CPAP were 37.2 ± 9.8 for MADRS1, 28.1 ± 10.7
for MADRS2, 22.8 ± 10.2 for MADRS3, and 18.5 ± 10.9 for
MADRS4. The mean trends from the baseline to the 6-month
follow-up are shown in Figure 2.
| |
Total number of patients |
Mean ± SD |
| Pre-CPAP(MADRSI) |
47 |
37.2 ± 9.8 |
| End of CPAP Course (MADRS2) |
42 |
28.1 ± 10.7 |
| 3-month follow up (MADRS3) |
42 |
22.8 ± 10.2 |
| 6-month follow up (MADRS4) |
42 |
18.5 ± 10.9 |
| Note: CPAP: Continuous Positive Airway Pressure; MADRS: Montgomery Asberg Depression Rating Scale; MADRS1: pre-CPAP MADRS score; MADRS2: MADRS score at the end of the CPAP course; MADRS3: MADRS score at the 3-month follow-up; MADRS4: MADRS score at the 6-month follow-up. |
Tab. 2. Mean MADRS scores of patients with depression.
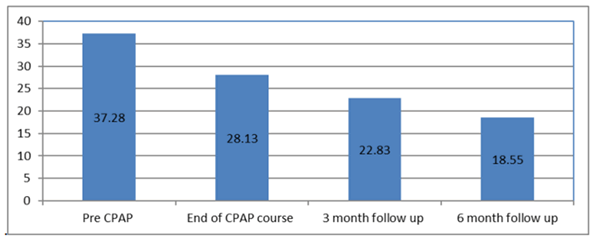
Figure 2: Graph showing mean MADRS
score of patients with depression.
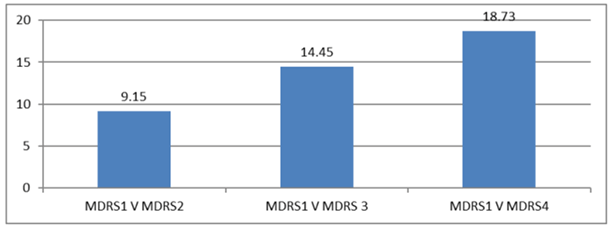
Table 3 compares the mean MADRS scores of patients with
depression throughout time. The MADRS scores revealed variations
of 9.1, 14.4, and 18.7 (MDRS1 vs. MDRS2) between pre-CPAP
and the conclusion of the CPAP treatment and the 3-month
follow-up. Table 4 shows statistical proof of a significant decrease
in MADRS ratings with CPAP therapy over time; all comparisons
had p-values of 0.000 (Figure 3).
| Comparison |
Mean difference |
p-value |
| MADRS1 vs. MADRS2 |
9.15 |
<0.01 |
| MADRS1 vs. MADRS 3 |
14.45 |
| MADRS1 vs. MADRS4 |
18.73 |
| Note: MADRS: Montgomery Asberg Depression Rating Scale; MADRS1: pre-CPAP MADRS score; MADRS2: MADRS score at the end of the CPAP course; MADRS3: MADRS score at the 3-month follow-up; MADRS4: MADRS score at the 6-month follow-up. |
Tab. 3. Comparison of mean MADRS scores of patients with depression.
| Pre-CPAP MADRS (baseline) |
Post CPAP |
| After CPAP |
3-month follow-up |
6-month follow-up |
| 37.28 ± 9.80 |
28.13 ± 10.70 |
22.83 ± 10.28 |
18.55 ± 10.93 |
| Significance between baseline and after CPAP |
P<0.01 |
P<0.01 |
P<0.01 |
| Note: CPAP: Continuous Positive Airway Pressure; MADRS: Montgomery Asberg Depression Rating Scale |
Tab.4. Effect of CPAP on the MADRS scores over time.
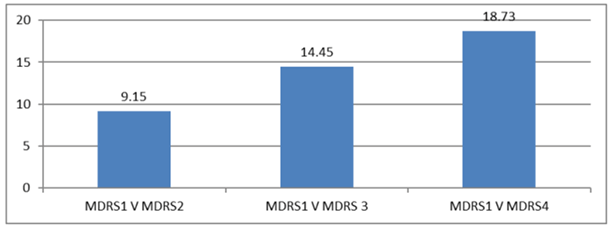
Figure 3: Graph showing mean
comparison madrs score of patients
with depression.
Discussion
For Sleep Apnea (OSA), CPAP is thought to be the most
effective non-pharmacological treatment because it successfully
lowers symptoms. In the current study, 44 out of 47 patients
received CPAP to the end. Between the pre-CPAP and the end
of the CPAP course, the average MADRS score differed by 9.1,
between the pre-CPAP and the 3-month follow-up, and between
the pre-CPAP and the 6-month follow-up, it varied by 14.4. The
fact that this improvement has been observed over time is clinically
significant. Additionally, the study showed that CPAP reduces
depression by demonstrating a decline in MADRS ratings in
depressed individuals.
It was astounding to observe a decrease in depressive symptoms
as soon as one month following the initiation of cognitive
behavioural therapy (CPAP). This is supported by the findings of
earlier trials [26,34] that shown improvements in mood symptoms
at the beginning of treatment. Furthermore, our study showed that
the benefits of Continuous Positive Pressure Breathing (CPAP)
therapy for depression persisted for up to six months after the last
CPAP session. These findings are in line with current studies that
demonstrate that improvements in mood symptoms brought about
by treatment persist for several months [35,36].
In all of the trials, there has been no discernible relationship
found between CPAP therapy and reductions in depression
[37,38]. Our results corroborate earlier studies that found CPAP
lessens depression linked to OSA. These studies looked closely at
the effects of CPAP on patients with OSA who had significant
depression [39-41]. In one of the first studies on this topic,
Habukawa et al. [39] found that CPAP treatment was associated
with a decline in the Epworth Sleepiness Scale (ESS) score as well
as a decline in the Beck Depression Inventory (BDI) and the
Hamilton Depression Rating Scale (HAM-D). El-Sherbini et al.
[41] reported that following CPAP treatment, six out of the eleven
patients who had been diagnosed with Major Depressive Disorder
(MDD) using the Structured Clinical Interview for DSM-IV
Disorders showed improvements in their symptoms.
For OSA patients who simultaneously experienced depressive
symptoms, CPAP therapy dramatically lowered MADRS ratings
(Table 4). The reversal of depressed symptoms in obstructive sleep
apnea suggests that the illness has a distinct emotional component
because the physical signs of the disorder are sometimes mistaken
for depressive symptoms. Our results, which show that depression
affected a significant portion of patients (11%-8%), are consistent
with other studies that have connected depression with OSA [42].
Persons with OSA are more likely to experience depression than
persons without OSA, and a sizable fraction of patients (11%-8%)
who experience depression also have undiagnosed OSA. Therefore,
more investigation is required to ascertain how OSA affects the
treatment of depression [43-45]. A comprehensive prospective
study is necessary to address the unresolved topic of whether OSA
is a risk factor for the eventual development of depression on its
own. If future research concentrates on people with OSA who
also have depression, it will be simpler to understand the complex
relationship between depression and OSA. All things considered,
our data suggests that CPAP is a helpful therapy for depression in
individuals with OSA. To prove that CPAP is a successful longterm
treatment for depression, larger prospective trials are needed,
as the current ones lack a control group and have a limited sample
size.
Conclusion
The recent study highlights that the fact that CPAP can reverse
depression symptoms in OSA patients suggests that the illness is more complicated than the physical symptoms that CPAP
addresses.
Ethics Approval
The study was approved by the ethics committee of Sher-i-Kashmir Institute of Medical Sciences (SKIMS Srinagar), Srinagar,
India.
Consent to Participate
A written consent was obtained from all participants.
Consent to Publish
A written informed consent for publication was obtained from
all participants.
Availability of Data and Materials
The datasets used and/or analyzed during the current study are
available from the corresponding author on reasonable request.
Competing Interests
The authors declare that they have no competing interests.
Funding
Financial support was not obtained from any individual,
institutions, agencies, drug industries or organizations.
Acknowledgments
The authors thank all the study participants.
Financial Support
None.
Author Contribution
All authors made substantial contributions to conception and
design; helped in the acquisition of data; analysis and interpretation
of data; took part in drafting the article or revising it critically for
important intellectual content; All authors gave final approval of
the version to be published; and agree to be accountable for all
aspects of the work.
References
- Malik JA, Masoodi SR, Shoib S. Obstructive sleep apnea in Type 2 diabetes and impact of continuous positive airway pressure therapy on glycemic control. Indian J Endo Metab. 2017;21:106-112.
[Crossref] [Google Scholar] [PubMed]
- Prasad B, Steffen AD, Van Dongen HP, et al. Determinants of sleepiness in obstructive sleep apnea. Sleep. 2018;41:199.
[Crossref] [Google Scholar] [PubMed]
- Melanie LM, Bhatt NY, Pack AI, et al. Global burden of sleep-disordered breathing and its implications." Respirology. 2020;25:690-702.
[Crossref] [Google Scholar] [PubMed]
- Morsy NE, Farrag NS, Zaki NF, et al. Obstructive sleep apnea: Personal, societal, public health, and legal implications. Rev Env health. 2019;34:153-69.
[Crossref] [Google Scholar] [PubMed]
- Shoib S, Malik JA, Masoodi SR, et al. Screening for comorbidities in obstructive sleep apnea. J Clin Diagno Res. 2018;12.
[Google Scholar]
- BaHammam AS, Kendzerska T, Gupta R, et al. Comorbid depression in obstructive sleep apnea: An under-recognized association. Sleep breath. 2016;20:447-56.
[Crossref] [Google Scholar] [PubMed]
- Young T, Finn L, Peppard PE, et al. Understanding the Health Burden of Sleep Disordered Breathing (Sdb), A Highly Preva-Lent Condition Of Frequent, Intermittent breathing pauses during Sleep Disordered Breathing and Mortality: Eighteen-Year Follow-up of the Wisconsin Sleep Cohort, Sleep. 2008.
- Shoib S, Malik JA, Masoodi S. Depression as a manifestation of obstructive sleep apnea. J Neuro Rural Pract. 2017;8:346-51.
[Crossref] [Google Scholar] [PubMed]
- Abbasi A, Gupta SS, Sabharwal N, et al. A comprehensive review of obstructive sleep apnea. Sleep Sci. 2021;14:142.
[Crossref] [Google Scholar] [PubMed]
- Almeneessier AS, Alasousi N, Sharif MM, et al. Prevalence and predictors of arrhythmia in patients with obstructive sleep apnea. Sleep Sci. 2017;10:142-46. [Crossref]
[Google Scholar] [PubMed]
- Banno K, Kryger MH. Sleep apnea: Clinical investigations in humans. Sleep Med. 2007;8:400-26.
[Crossref] [Google Scholar] [PubMed]
- Ohayon MM. The effects of breathing-related sleep disorders on mood disturbances in the general population. J Clin Psy. 2003;64:1195-1200.
[Crossref] [Google Scholar] [PubMed]
- Jehan S, Auguste E, Pandi-Perumal SR, et al. Depression, obstructive sleep apnea and psychosocial health. Sleep Med Dis Int J. 2017;1.
[Google Scholar] [PubMed]
- Flemons WW, Tsai W. Quality of life consequences of sleep-disordered breathing. J Alle Clin Immunol. 1997;99:750-56.
[Crossref] [Google Scholar] [PubMed]
- Pochat MD, Ferber C, Lemoine P. Symptomatologie depressive et syndrome d'apnees du sommeil. L'Encephale (Paris). 1993;19: 601-07.
[Google Scholar]
- Shoib S, Das S. Factors predicting the presence of depression in obstructive sleep apnea. Ind Psychiatry J. 2020;29:29-32.
[Crossref] [Google Scholar] [PubMed]
- Shoib S, Mushtaq R, Tasleem A, et al. Depression and diabetes: Common link and challenges of developing epidemic. J Psychiatry. 2015;18:14-64.
[Google Scholar]
- Aikens JE, Caruana-Montaldo B, Vanable PA, et al. Depression and general psychopathology in obstructive sleep apnea. Sleep. 1998;21:71.
- Millman RP, Fogel BS, McNamara ME, et al. Depression as a manifestation of obstructive sleep apnea: Reversal with nasal continuous positive airway pressure. J Clin Psychiatry. 1989;50:348-51. [Crossref]
[Google Scholar] [PubMed]
- Mosko S, Zetin M, Glen S, et al. Self-reported depressive symptomatology, mood ratings, and treatment outcome in sleep disorders patients. J Clin Psychology. 1989;45:51-60.
[Crossref] [Google Scholar] [PubMed]
- Rotenberg BW, Murariu D, Pang KP. Trends in CPAP adherence over twenty years of data collection: A flattened curve. J Otolaryngol-Head Neck Surg. 2016;45:43.
[Crossref] [Google Scholar] [PubMed]
- Sullivan C, Berthon-Jones M, Issa F, et al. Reversal of obstructive sleep apnoea by continuous positive airway pressure applied through the nares.Lancet. 1981;317:862-65.
[Crossref][Google Scholar] [PubMed]
- Doherty LS, Kiely JL, Swan V, et al. Long-term effects of nasal continuous positive airway pressure therapy on cardiovascular outcomes in sleep apnea syndrome. Chest. 2005;127:2076-84.
[Crossref][Google Scholar] [PubMed]
- Zheng D, Xu Y, You S, et al. Effects of continuous positive airway pressure on depression and anxiety symptoms in patients with obstructive sleep apnoea: Results from the sleep apnoea cardiovascular Endpoint randomised trial and meta-analysis. E Clin Med. 2019;11:89-96.
[Crossref] [Google Scholar]
- Derderian LC, Bridenbaugh CR, Rajagopal LC. Neuropsychologic symptoms in obstructive sleep apnea improve after treatment with nasal continuous positive airway pressure. Chest. 1988;94:1023-27.
[Crossref] [Google Scholar] [PubMed]
- Charboneau M, Tousignant P, Lamping DL, et al. The effects of Nasal Continuous Positive Airway Pressure (nCPAP) on sleepiness and psychological functioning in Obstructive Sleep Apnea (OSA). Am Rev Respir Dis. 1992;145:A168.
- Engleman HM, Martin SE, Kingshott RN, et al. Randomised placebo controlled trial of daytime function after Continuous Positive Airway Pressure (CPAP) therapy for the sleep apnoea/hypopnoea syndrome. Thorax. 1998;53:341-45.
[Crossref] [Google Scholar] [PubMed]
- Borak J, Cieslicki J, Szelenberger W, et al. Psychopathological characteristics of the consequences of obstructive sleep apnea prior to and three months after CPAP. Psy Polska. 1994.
[Google Scholar] [PubMed]
- Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59:22-33. [Crossref]
[Google Scholar] [PubMed]
- Montgomery SA, Asberg MA. A new depression scale designed to be sensitive to change. British J Psychiatry. 1979;134:382-89.
[Crossref] [Google Scholar] [PubMed]
- Hobson JA. A manual of standardized terminology, techniques and scoring system for sleep stages of human subjects. Clin Neuro. [Crossref]
[Google Scholar]
- Flemons W. Sleep-related breathing disorders in adults: Recommendations for syndrome definition and measurement techniques in clinical research. Sleep. 1999;22:667-89.
[Google Scholar]
- Johns MW. Reliability and factor analysis of the Epworth Sleepiness Scale. Sleep. 1992;15:376-81.
[Crossref] [Google Scholar] [PubMed]
- Engleman HM, Martin SE, Douglas NJ, et al. Effect of continuous positive airway pressure treatment on daytime function in sleep apnoea/hypopnoea syndrome. Lancet. 1994; 343: 572-575.
[Crossref] [Google Scholar] [PubMed]
- Kingshott RN, Vennelle M, Hoy CJ, et al. Predictors of improvements in daytime function outcomes with CPAP therapy. Amer J Res Crit Care Med. 2000;161:866-71.
[Crossref] [Google Scholar] [PubMed]
- Platón MJ, Sierra JE. Changes in psychopathological symptoms in sleep apnea patients after treatment with nasal continuous positive airway pressure. Int J Neuro. 1991; 62: 173-195.
[Crossref] [Google Scholar] [PubMed]
- Borak J, Cieslicki J, Koziej M, et al. Effects of CPAP treatment on psychological status in patients with severe obstructive sleep apnoea. J Sleep Res. 1996; 5: 123-127.
[Crossref] [Google Scholar] [PubMed]
- Munoz A, Mayoralas LR, Barbe F, et al. Long-term effects of CPAP on daytime functioning in patients with sleep apnoea syndrome. Euro Res J. 2000;15:676-81.
[Crossref] [Google Scholar] [PubMed]
- Habukawa M, Uchimura N, Kakuma T, et al. Effect of CPAP treatment on residual depressive symptoms in patients with major depression and coexisting sleep apnea: contribution of daytime sleepiness to residual depressive symptoms. Sleep Med. 2010;11:552-57.
[Crossref] [Google Scholar] [PubMed]
- Mackinger HF, Svaldi JJ. Autobiographical memory predicts cognitive but not somatic change in sleep apnea patients vulnerable for affective disorder. J Affect Dis. 2004;81:17-22.
[Crossref] [Google Scholar] [PubMed]
- Makram El-Sherbini A, Bediwy AS, El-Mitwalli A. Neuropsychiatric Disease and Treatment Dovepress Association between Obstructive Sleep Apnea (OSA) and depression and the effect of continuous positive airway pressure (CPAP) treatment. 2011.
- Young T, Evans L, Finn L, et al. Estimation of the clinically diagnosed proportion of sleep apnea syndrome in middle-aged men and women. Sleep. 1997;20:705-6.
[Crossref] [Google Scholar] [PubMed]
- Harris M, Glozier N, Ratnavadivel R, et al. Obstructive sleep apnea and depression. Sleep Med Rev. 2009;13:437-44.
[Crossref] [Google Scholar] [PubMed]
- Scoring EA. EEG arousals: Scoring rules and examples: a preliminary report from the sleep disorders atlas task force of the american sleep disorders association. Sleep. 1992;15:174-84.
[Crossref] [Google Scholar] [PubMed]
- Stradling JR, Davies RJ. Obstructive sleep apnoea/hypopnoea syndrome: Definitions, epidemiology, and natural history. Thorax. 2004;59: 73-8.
[Crossref] [Google Scholar] [PubMed]