Background: An extreme excess of patients exceeding the capacity of emergency departments (EDs) to provide care is an emerging threat to patient safety and health systems worldwide.
Aim: The purpose of this literature review was to investigate the effects of emergency department crowding on patients outcome.
Method and Material: A comprehensive search of the medical literature in Pubmed/ MEDLINE database was performed to identify all original articles that were published or available on-line between January 1, 2003, to January 1, 2013, and related to the concepts of ‘‘emergency department’’ and ‘‘crowding’’ or ‘’overcrowding’’.
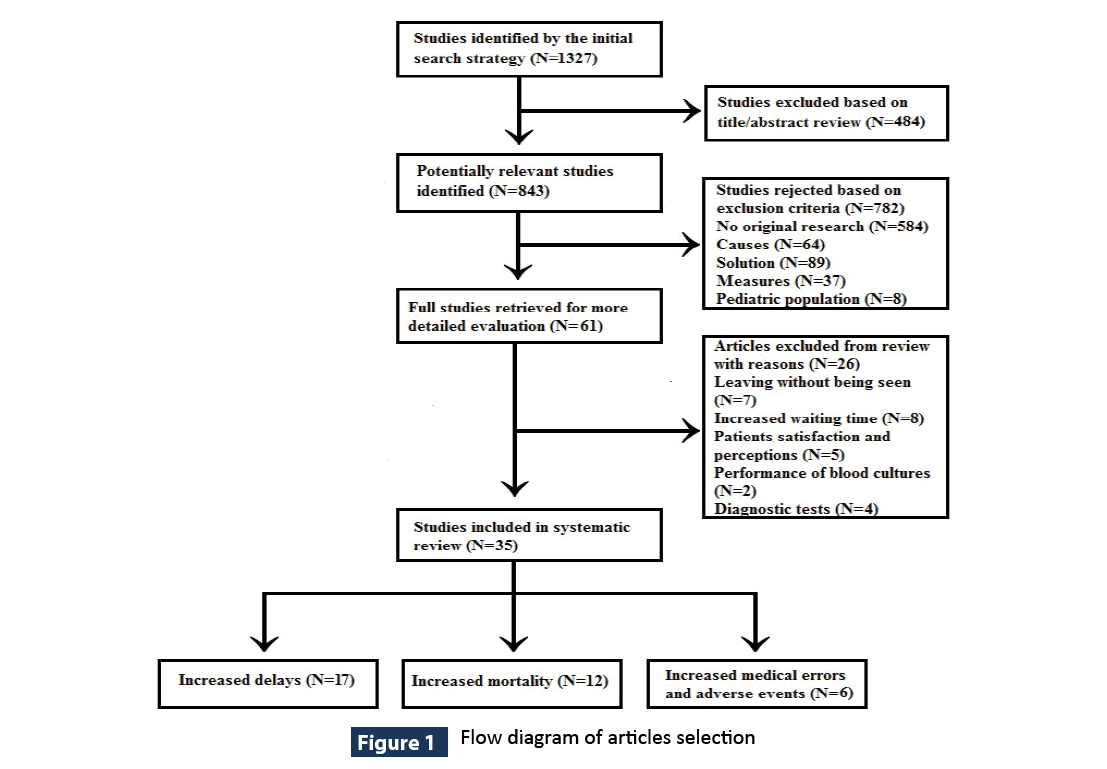
Results: Of the 1327 studies that were initially retrieved, 484 were excluded because they had no relevance to the topic and 843 after checking for eligibility criteria. From remaining 61 articles, a total of 35 studies were finally included in the review. The three main categories that were constructed based on the studies, were delays in treatment interventions, increased medical errors or adverse events and increased mortality.
Conclusions: The body of literature in aggregate strongly suggests that ED crowding is associated with potential of poorer performance and adverse clinical outcomes, including mortality. Further research is needed to fully understand the precise mechanism through which crowding adversely affect patient care. Policies must also be targeted to adapt of emergency care system in the fluctuation of inputs for better care that translates into better outcomes for patients visiting EDs..
Keywords
Emergency department crowding; Patient safety
Introduction
Emergency department (ED) crowding has been described as the most serious problem that endanger the reliability of health care system worldwide [1]. The American College of Emergency Physicians defines crowding as a situation in which the identified need for emergency services exceeds available resources for patient care in the emergency department, hospital, or both [2]. The conceptual model partitions ED crowding into 3 interdependent components: input, throughput, and output [3].
The commonly studied cause of crowding is demand for ED care. Between 1997 and 2007 the increase in total annual ED visits in USA was almost double [4] and between 2001-2008 was 60% faster than would be expected from population growth [5]. A large proportion of all ED visits were for nonurgent conditions that estimated at 37% (range 8%-62%) [6] and from frequent users who comprised 4.5% to 8% of all ED patients but accounted for 21% to 28% of all visits [7].
One main factor that may cause crowding is inadequate staffing. Half of EDs exceed recommended patient to nurse ratio of 4:1 for routine ED beds [8] and 68% a patient to nurse ratio of 1:1 for critical care beds [9]. The mean nurse: patient ratios at morning shift were 1:15, at afternoon shift 1:7 and at night 1:4 [10].
Hospital bed shortages have been studied as factors that potentially affect crowding. Emergency rooms and trauma centers in U.S.A declined by 3% from period 2003-2007 [11]. Nonavailability of ED beds because they are occupied by admitted patients waiting for transfer from the ED to inpatient units restrict the EDs capacity to accept new arrivals and consume EDs resources [12-14]. A recent study concluded that, if current bed use trends persist and as the numbers of frail older patients rise exponentially, a 62% increase in hospital beds will be required to meet expected demand by 2050, at a cost almost equal to the entire current Australian healthcare budget [15].
ED crowding has resulted in poor performance on waiting time and length of stay (LOS). In US hospitals the odds of being examined by a physician within the time recommended at triage declined by 30% from 1997 to 2006 [16], waiting time increased from 46.5 minutes to 58.1 minutes from period between 2003- 2009 [17] and ED LOS increased from132 minutes in 2001 to 154 minutes in 2005 [18]. There was a larger increase among critically ill patients for whom ED LOS increased from 185 minutes in 2001 to 254 minutes in 2005 [18]. In other study found that an increase from the 20th to the 80th percentile in ED arrivals resulted in increases of 42 minutes in waiting time and 49 minutes in LOS [19].
The obvious operational and logistic problems created by crowding have a variety of undesirable consequences on patients, staff and hospitals [20,21]. The six dimensions of quality including safety, effectiveness, patient-centeredness, efficiency, timeliness, and equity that has been described by The Institute of Medicine, may all be compromised when patients experience long waiting time to see a physician or leaving without being examined, patients remains in the ED after they have been admitted to the hospital, but have not been transferred to an inpatient unit, or ambulances are diverted away from the hospital closest to the patient [22]. Therefore, the objective of this review was to describe the scientific literature that investigates the effect of ED crowding on patients outcomes.
Method
A comprehensive search of the medical literature in Pubmed/ MEDLINE database was performed to identify all scientific articles that were published or were available on-line between January 1, 2003, to January 1, 2013, and related to the concepts of ‘‘emergency department’’ and ‘‘crowding’’ or ‘’overcrowding’’.
The inclusive selection criteria were as follows: To be original article, to use crowding measures, to provide odds ratio (OR), risk ratio (RR) or hazard ratio (HR) estimates with confidence intervals and to be published in English. We excluded commentaries and letters to the editor, original article for causes, solution and measures of emergency department crowding and adverse effects on pediatric patients.
Two reviewers independently evaluated the titles and abstracts for relevance to the topic and subsequently obtained full-text versions of all potentially relevant papers, which were then further discussed among authors for final inclusion.
Results
The initial search yielded a total of 1327 citations, 484 were excluded after title/abstract review and 782 did not fulfill inclusion criteria (94% inter-reviewer agreement). After retrieving the full-text of the remaining 61 articles, another 26 articles, which focus on waiting time, delays for diagnostic test and patients perceptions, related to ED crowding, were excluded from review. Finally, only 35 papers measured the effect of ED crowding on patient outcomes and grouped in three categories: increased delays in treatment, increase medical errors and adverse events and increased mortality. A flowchart of studies included in this review is presented in Figure 1.
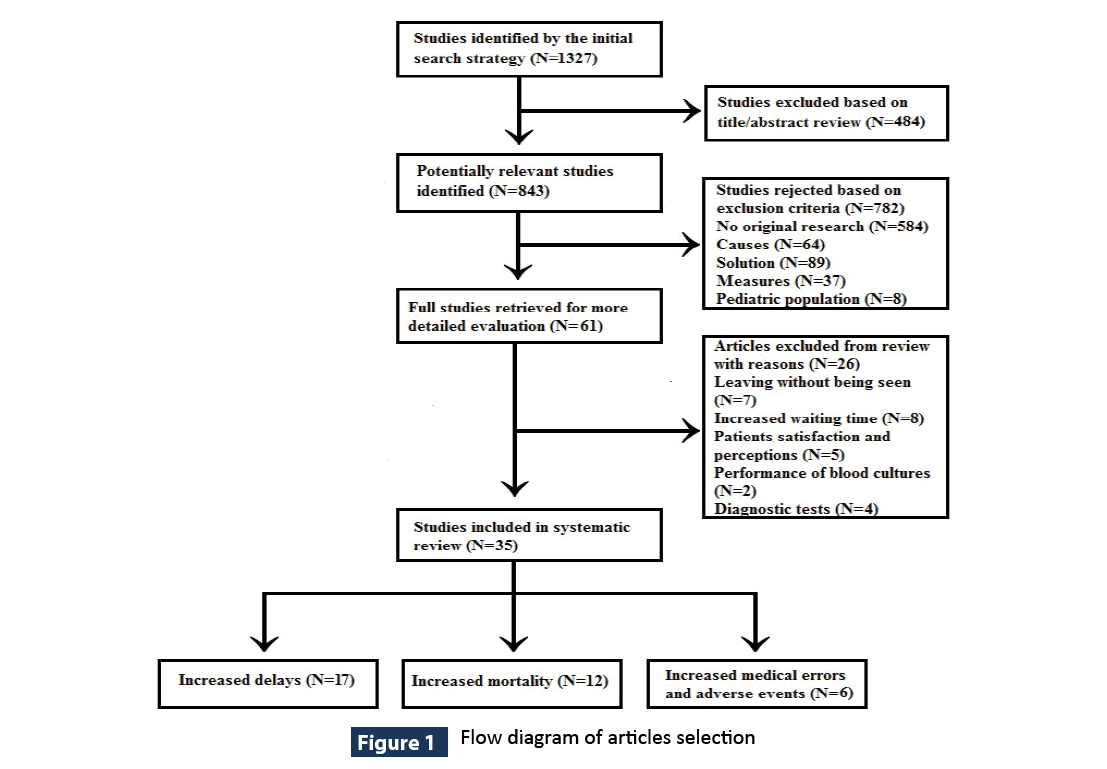
Figure 1: Flow diagram of articles selection
Delay in treatment interventions
Seventeen studies [23-39] examined the relationship between ED crowding and delay in treatment. Regarding pain management, Hwnag et al., found that during periods of greater patient volume, hip fracture patients had less documentation of pain on first assessment and longer times to pain assessment [23]. Patients examined during periods of high patient concentration, took up to 55 minutes longer to have documented pain assessment without differences in likelihood of pain assessment [24]. Administration of analgesia during high levels of ED crowding measures was less likely to patients with severe pain [25] and other painful condition [24] while was not statistically significant in patient with back [26] or abdominal [27] pain and hip fracture [23]. Among those who received treatment, ED crowding measures were associated with a higher likelihood of delay in both time from triage to analgesia and time from room placement to analgesia [25,26]. Likely, no relation between workload and time to analgesia was observed in patients with fractured neck of femur or wrist and renal or billiary colic [28]
Regarding time to antibiotic administration for patients with pneumonia, five studies associated increased level of ED crowding with a decrease in the proportion of community-acquired pneumonia (CAP) patients receiving antibiotics within four hours [29-33]. The time from arrival to order a chest radiograph was prolonged by 14.3 minutes and from ordering of antibiotic to administration by 9.3 minutes for every 10 additional ED patients [30]. The effect of additional patients appears to occur even at volumes below the maximum bed capacity [29].
Overcrowding was also associated with increased door-to-balloon and door-to-needle times for the treatment of acute ST-Elevation Myocardial Infarction (STEMI) [34,35]. In contrast, time to achieve emergency percutaneous coronary intervention for acute STEMI did not correlate positively with crowding as measured by the occupancy rate [36] and ED length of stay or left without being examined [33].
Time to acute stroke care however, remained the same in thrombolysis eligible patients regardless of the crowding factor, but not in patients outside of the intravenous thrombolysis window, who experienced delays in a CT-scan order and completion at higher levels of ED crowding [37].
ED crowding as measured by the number of patients visits, was associated with delays in resuscitation efforts and mortality during ED stay. Patients who attended at day with daily visit equal to or greater than 93 (daily ED patient concentration range 57-140) had two-fold increased odds of experiencing delayed resuscitation effort and four-fold increased odds of in-hospital mortality compared with the patients who attended at day with daily visit less than 93 [38].
Medication treatment time in patients with acute asthma wasassociated with highest percentiles of ED occupancy. Time to a nebulizer order was 6 minutes longer (95% CI=1-13 minutes), and time to a steroid order was 16 minutes longer (95% CI =0-38 minutes) during crowded periods [39].
Increased medical errors and adverse events
Six studies [40-45] assessed the effect that ED crowding had on medical errors and adverse events. ED overcrowding is associated with an increased frequency of medication errors measured in real time by the modified EDWIN score [40] or boarding status [41]. Errors included giving medications at incorrect doses, frequencies, durations, or routes and giving contraindicated medications [40]. Patients whose average crowding exposure was in the highest quartile had two-fold increased odds of experiencing a preventable adverse event compared to patients whose average crowding exposure was in the lowest quartile [42]. For every hour spent in the ED, the odds of experiencing an adverse event in-hospital increased by 3% [43].
Among patients with acute coronary syndrome, several crowding measures showed three to five times higher rates of adverse outcomes as cardiac arrest, congestive heart failure, ventricular tachycardia or fibrillation, supraventricular dysrhythmias, symptomatic bradycardia, hypotension or death during the highest levels of crowding [44]. High hospital occupancy was associated with increased incidence of serious complications defined as shock, need for intubation and death within 24 hours for patients admitted, but still treated in the emergency department and managed by emergency department providers. The incidence for serious complications was 13.62 per 1000 patient days when hospital occupancy was ≤90%, and it increased significantly to 17.10 and 22.52 per 1000 patient days for occupancy at 90%-95% and ≥95%, respectively [45].
Increased mortality
Twelve articles [46-57] specifically examined the association between ED crowding and mortality. Occupancy was linked to increased odds of deaths at 10 days for patients who presented to one Australian hospital (OR=1.34, 95% CI=1.04–1.72) [46] Using the same crowding measure, patients with CAP had 9-fold increased odds of 28-day mortality [47] Hospital occupancy ≥100% in combination with access block ≥20% occupancy was associated with an increased 2, 7 and 30-day mortality (HR=1.3, 95% CI=1.1–1.6, 1.3, 95% CI=1.2–1.5 and 1.2, 95% CI=1.1–1.3 respectively) [48].
Mortality increased with increasing boarding time, from 2.5% in patients boarded less than 2 hours, to 4.5% in patients boarding 12 hours or more (p < 0.001) [49]. The in-hospital mortality was 17.4% for critically ill emergency department patients with a >6- hr delay in intensive care unit transfer, versus 12,9% for critically ill patients who were transferred to intensive care unit in <6- hr (p<.001) [50]. The risk of death among high and low acuity patients was 1.79 and 1.71 respectively for mean length of stay of ≥6 hours compared with <1 hour [51]. Prolonged ED boarding stay that exceeded 8 hours was associated with increased mortality in patients with necrotizing fasciitis [52]. The long ED stay was not associated with mortality in patients with non–STEMI but was associated with increased rate of recurrent in-hospital MI [53].
ED crowding, as measured by ambulance diversion at 187 hospitals, was associated with increased inpatient death rate occurring in the first 3 days (OR=1.05, 95% CI=1.02–1.08) [54]. Among patients that were admitted for AMI and exposed to 12 or more hours of ambulance diversion, the 30-day, 90-day, 9-month, and 1-year mortality was increased [55]. The mortality for admitted trauma patients on significant diversion days, defined as day when hospitals were on diversion for more than 8 hours, was slightly higher than among those admitted on day when hospitals were on diversion for fewer than 8 hours (3.9% vs. 3.3%), but was statistically significant at the 0.1 level (25% vs 14%) among the most severely ill patients [56]. In contrast, ambulance diversion contributed to 28% reduction in patient mortality at an Australian ED [57]
Discussion
ED crowding is associated with delays in treatment for emergency conditions, thereby increasing the risk of poorer outcomes. Increased crowding levels, according to this review, were associated with the potential of poorer performance regarding pain management standards, such as timely and appropriate assessment or analgesia on which hospitals are judged [23-27]. Delays or not treatment of acute pain has consequences beyond the immediate perception of suffering and can negatively impact patients’ well-being on multiple levels [58].
Emergency departments in crowding conditions were not able to meet The Joint Commission and the Centers for Medicare and Medicaid Services (CMS) performance measures targets for patients with CAP, that are used as an indicator of the quality of care, with a 4- hour benchmark [29-33]. Although current guidelines for treating CAP do not recommend administering antibiotics within a certain time limit, [59] early time to first antibiotic dose should be considered as an important marker of optimal patient care in patients with CAP rather than a factor predicting the outcome [60,61]. Although articles attempted to relate degradations in performance to crowded conditions, their evidence suggests that performance begins to deteriorate long before conditions in the ED begin to be identified as crowded [29].
The impact of ED crowding on time-sensitive processes of care such as reperfusion therapy is controversial. The finding that ED crowding, as measured according to EDWIN score, associated with increased time to balloon inflation during PCI for the treatment of acute STEMI [35] does not confirm by the much more robust, prospective data from the same ED in a study designed to follow up that study’s findings [36]. ED crowding was not associated with care delays in thrombolysis-eligible patients with stroke [37] but for patients with suspected acute myocardial infarction [34]. The established policies that high prioritize diagnostic and treatment algorithm critically ill patients stroke and acute myocardial infarction may not be affected by competing resource demand [36].
ED crowding exacerbates the rate of medical errors adverse affected quality of care [40-42]. Although a medical error does not necessarily imply the occurrence of a medical harm, patients exposed at risk of medical errors potentially increased their risk of adverse events. Critically ill patients exposed to crowding are highly likely to be attributable to adverse events caused by medical errors [44]. The increased likelihood of serious adverse events is a plausible mediator of the relationship between crowding and increased lifethreatening complications [45].
This review is consistent with 4 previous reviews [20-22,62] looking at the effects of emergency department crowding on patients outcomes. Delays in providing needed care and increased risks of mortality are identified in all articles by adding decreased satisfaction [21] and higher probability of leaving the ED against medical advice or without being examined [22]. Another article focuses on adverse moral consequences of ED crowding, as compromised privacy and confidentiality, impaired communication, and diminished access to care [62].
The results of the current review should be interpreted in the context of some limitations. First, our research is limited only to the Pubmed database and we may have missed some studies published in others databases. Second, the retrospective design of the included studies based on existing patient registers or databases cannot exclude the possibility of confounding that may have affected these results. Accuracy and variability in the quality of documentation among different health care personnel it was not feasible to ensure with retrospective audit of databases. The findings show considerable variability in crowding measures, time intervals, patient populations and hospital status, resulting to inability to generalize. Finally, no study determined the exact mechanism responsible for the association between crowding and adverse events, although some inferences can be made.
Conclusion
The body of literature in aggregate strongly suggests that ED crowding is associated with poorer performance and adverse clinical outcomes, including mortality. Further research is needed to fully understand the precise mechanism through which crowding adversely affect patient care. Policies must also be targeted to adapt of emergency care system in the fluctuation of inputs for better care that translates into better outcomes for patients visiting EDs.
3798
References
- Pines JM, Hilton JA, Weber EJ, Alkemade AJ, Al Shabanah H, et al. (2011) International perspectives on emergency department crowding. Acad Emerg Med 18: 1358-1370.
- American College of Emergency Physicians (2006) Crowding. Ann Emerg Med 47: 585.
- Asplin BR, Magid DJ, Rhodes KV, Solberg LI, Lurie N, et al. (2003) A conceptual model of emergency department crowding. Ann Emerg Med 42: 173-180.
- Tang N, Stein J, Hsia RY, Maselli JH, Gonzales R (2010) Trends and characteristics of US emergency department visits, 1997-2007. JAMA 304: 664-670.
- Pitts SR, Pines JM, Handrigan MT, Kellermann AL (2012) National trends in emergency department occupancy, 2001 to 2008: effect of inpatient admissions versus emergency department practice intensity. Ann Emerg Med 60:679-686
- Uscher-Pines L, Pines J, Kellermann A, Gillen E, Mehrotra A (2013) Emergency department visits for nonurgent conditions: systematic literature review. Am J Manag Care 19: 47-59.
- LaCalle E, Rabin E (2010) Frequent users of emergency departments: the myths, the data, and the policy implications. Ann Emerg Med 56: 42-48.
- Schneider SM, Gallery ME, Schafermeyer R, Zwemer FL (2003) Emergency department crowding: a point in time. Ann Emerg Med 42: 167-172.
- Rose L, Ramagnano S (2013) Emergency nurse responsibilities for mechanical ventilation: a national survey. J Emerg Nurs 39: 226-232.
- Lyneham J, Cloughessy L, Martin V (2008) Workloads in Australian emergency departments a descriptive study. Int Emerg Nurs 16: 200-206.
- Harrison JP, Ferguson ED (2011) The crisis in United States hospital emergency services. Int J Health Care Qual Assur 24: 471-483.
- Cooke MW, Wilson S, Halsall J, Roalfe A (2004) Total time in English accident and emergency departments is related to bed occupancy. Emerg Med J 21: 575-576.
- White BA, Biddinger PD, Chang Y, Grabowski B, Carignan S, et al. (2013) Boarding inpatients in the emergency department increases discharged patient length of stay. J Emerg Med 44: 230-235.
- Crilly J, Keijzers G, Krahn D, Steele M, Green D, et al. (2011) The impact of a temporary medical ward closure on emergency department and hospital service delivery outcomes. Qual Manag Health Care 20: 322-333.
- Scott IA (2010) Public hospital bed crisis: too few or too misused? Aust Health Rev 34: 317-324.
- Horwitz LI, Bradley EH (2009) Percentage of US emergency department patients seen within the recommended triage time: 1997 to 2006. Arch Intern Med 169: 1857-1865.
- Hing E, Bhuiya F (2012) Wait time for treatment in hospital emergency departments: 2009. NCHS Data Brief : 1-8.
- Herring A, Wilper A, Himmelstein DU, Woolhandler S, Espinola JA, et al. (2009) Increasing length of stay among adult visits to U.S. Emergency departments, 2001-2005. Acad Emerg Med 16: 609-616.
- Asaro PV, Lewis LM, Boxerman SB (2007) The impact of input and output factors on emergency department throughput. Acad Emerg Med 14: 235-242.
- Hoot NR, Aronsky D (2008) Systematic review of emergency department crowding: causes, effects, and solutions. Ann Emerg Med 52: 126-136.
- Johnson KD, Winkelman C (2011) The effect of emergency department crowding on patient outcomes: a literature review. Adv Emerg Nurs J 33: 39-54.
- Bernstein SL, Aronsky D, Duseja R, Epstein S, Handel D, et al. (2009) Society for Academic Emergency Medicine, Emergency Department Crowding Task Force. The effect of emergency department crowding on clinically oriented outcomes. Acad Emerg Med 16:1-10
- Hwang U, Richardson LD, Sonuyi TO, Morrison RS (2006) The effect of emergency department crowding on the management of pain in older adults with hip fracture. J Am Geriatr Soc 54: 270-275.
- Hwang U, Richardson L, Livote E, Harris B, Spencer N, et al. (2008) Emergency department crowding and decreased quality of pain care. Acad Emerg Med 15: 1248-1255.
- Pines JM, Hollander JE (2008) Emergency department crowding is associated with poor care for patients with severe pain. Ann Emerg Med 51: 1-5.
- Pines JM, Shofer FS, Isserman JA, Abbuhl SB, Mills AM (2010) The effect of emergency department crowding on analgesia in patients with back pain in two hospitals. Acad Emerg Med 17: 276-283.
- Mills AM, Shofer FS, Chen EH, Hollander JE, Pines JM (2009) The association between emergency department crowding and analgesia administration in acute abdominal pain patients. Acad Emerg Med 16: 603-608.
- Mitchell R, Kelly AM, Kerr D (2009) Does emergency department workload adversely influence timely analgesia? Emerg Med Australas 21: 52-58.
- Fee C, Weber EJ, Maak CA, Bacchetti P (2007) Effect of emergency department crowding on time to antibiotics in patients admitted with community-acquired pneumonia. Ann Emerg Med 50: 501-509, 509.
- Fee C, Weber EJ, Bacchetti P, Maak CA (2011) Effect of emergency department crowding on pneumonia admission care components. Am J Manag Care 17: 269-278.
- Sikka R, Mehta S, Kaucky C, Kulstad EB (2010) ED crowding is associated with an increased time to pneumonia treatment. Am J Emerg Med 28: 809-812.
- Pines JM, Localio AR, Hollander JE, Baxt WG, Lee H, et al. (2007) The impact of emergency department crowding measures on time to antibiotics for patients with community-acquired pneumonia. Ann Emerg Med 50: 510-516.
- Pines JM, Hollander JE, Localio AR, Metlay JP (2006) The association between emergency department crowding and hospital performance on antibiotic timing for pneumonia and percutaneous intervention for myocardial infarction. Acad Emerg Med 13:873-878
- Schull MJ, Vermeulen M, Slaughter G, Morrison L, Daly P (2004) Emergency department crowding and thrombolysis delays in acute myocardial infarction. Ann Emerg Med 44: 577-585.
- Kulstad EB, Kelley KM (2009) Overcrowding is associated with delays in percutaneous coronary intervention for acute myocardial infarction. Int J Emerg Med 2: 149-154.
- Harris B, Bai JC, Kulstad EB (2012) Crowding does not adversely affect time to percutaneous coronary intervention for acute myocardial infarction in a community emergency department. Ann Emerg Med 59: 13-17.
- Chatterjee P, Cucchiara BL, Lazarciuc N, Shofer FS, Pines JM (2011) Emergency department crowding and time to care in patients with acute stroke. Stroke 42: 1074-1080.
- Hong KJ, Shin SD, Song KJ, Cha WC, Cho JS (2013) Association between ED crowding and delay in resuscitation effort. Am J Emerg Med 31: 509-515.
- Pines JM, Prabhu A, Hilton JA, Hollander JE, Datner EM (2010) The effect of emergency department crowding on length of stay and medication treatment times in discharged patients with acute asthma. Acad Emerg Med 17:834-839
- Kulstad EB, Sikka R, Sweis RT, Kelley KM, Rzechula KH (2010) ED overcrowding is associated with an increased frequency of medication errors. Am J Emerg Med 28: 304-309.
- Patanwala AE, Warholak TL, Sanders AB, Erstad BL (2010) A prospective observational study of medication errors in a tertiary care emergency department. Ann Emerg Med 55: 522-526.
- Epstein SK, Huckins DS, Liu SW, Pallin DJ, Sullivan AF, et al. (2012) Emergency department crowding and risk of preventable medical errors. Intern Emerg Med 7: 173-180.
- Ackroyd-Stolarz S, Read GJ, Mackinnon NJ, Kovacs G (2011) The association between a prolonged stay in the emergency department and adverse events in older patients admitted to hospital: a retrospective cohort study. BMJ Qual Saf 20:564-569
- Pines JM, Pollack CV Jr, Diercks DB, Chang AM, Shofer FS (2009) The association between emergency department crowding and adverse cardiovascular outcomes in patients with chest pain. Acad Emerg Med 16:617-625
- Zhou JC, Pan KH, Zhou DY, Zheng SW, Zhu JQ, et al. (2012) High hospital occupancy is associated with increased risk for patients boarding in the emergency department. Am J Med 125: 416.
- Richardson DB (2006) Increase in patient mortality at 10 days associated with emergency department overcrowding. Med J Aust 184: 213-216.
- Jo 1, Kim K, Lee JH, Rhee JE, Kim YJ, et al. (2012) Emergency department crowding is associated with 28-day mortality in community-acquired pneumonia patients. J Infect 64: 268-275.
- Sprivulis PC, Da Silva JA, Jacobs IG, Frazer AR, Jelinek GA (2006) The association between hospital overcrowding and mortality among patients admitted via Western Australian emergency departments. Med J Aust 184:208-212
- Singer AJ, Thode HC Jr, Viccellio P, Pines JM (2011) The association between length of emergency department boarding and mortality. Acad Emerg Med 18: 1324-1329.
- Chalfin DB, Trzeciak S, Likourezos A, Baumann BM, Dellinger RP; DELAY-ED study group (2007) Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med 35: 1477-1483.
- Guttmann A, Schull MJ, Vermeulen MJ, Stukel TA (2011) Association between waiting times and short term mortality and hospital admission after departure from emergency department: population based cohort study from Ontario, Canada. BMJ 342:d2983
- Hong YC, Chou MH, Liu EH, Hsiao CT, Kuan JT, et al. (2009) The effect of prolonged ED stay on outcome in patients with necrotizing fasciitis. Am J Emerg Med 27: 385-390.
- Diercks DB, Roe MT, Chen AY, Peacock WF, Kirk JD, et al. (2007) Prolonged emergency department stays of non-ST-segment-elevation myocardial infarction patients are associated with worse adherence to the American College of Cardiology/American Heart Association guidelines for management and increased adverse events. Ann Emerg Med 50:489-496
- Sun BC, Hsia RY, Weiss RE, Zingmond D, Liang LJ, et al. (2013) Effect of emergency department crowding on outcomes of admitted patients. Ann Emerg Med 61: 605-611.
- Shen YC, Hsia RY (2011) Association between ambulance diversion and survival among patients with acute myocardial infarction. JAMA 305: 2440-2447.
- Begley CE, Chang Y, Wood RC, Weltge A (2004) Emergency department diversion and trauma mortality: evidence from houston, Texas. J Trauma 57: 1260-1265.
- Fatovich DM (2005) Effect of ambulance diversion on patient mortality: how access block can save your life. Med J Aust 183: 672-673.
- Sinatra R (2010) Causes and consequences of inadequate management of acute pain. Pain Med 11: 1859-1871.
- Yahav D, Leibovici L, Goldberg E, Bishara J, Paul M (2013) Time to first antibiotic dose for patients hospitalised with community-acquired pneumonia. Int J Antimicrob Agents 41: 410-413.
- Bordon J, Aliberti S, Duvvuri P, Wiemken T, Peyrani P, et al. (2013) Early administration of the first antimicrobials should be considered a marker of optimal care of patients with community-acquired pneumonia rather than a predictor of outcomes. Int J Infect Dis 17: e293-298.
- Yu KT, Wyer PC (2008) Evidence-based emergency medicine/critically appraised topic. Evidence behind the 4-hour rule for initiation of antibiotic therapy in community-acquired pneumonia. Ann Emerg Med 51:651-662
- Moskop JC, Sklar DP, Geiderman JM, Schears RM, Bookman KJ (2009) Emergency department crowding, part 1--concept, causes, and moral consequences. Ann Emerg Med 53: 605-611.