Research Article - (2022) Volume 16, Issue 3
The Effect of Modified Constraint Induced Movement Therapy on Motor Performance and Daily Functions in Patients One To Nine Months after Stroke
Dr. Sobha Saseendrababu*
Assistant professor College of nursing Northern Border University Arar, Kingdom of Saudi Arabia
*Correspondence:
Dr. Sobha Saseendrababu, Assistant professor College of nursing Northern Border University Arar,
Kingdom of Saudi Arabia,
Email:
Received: 10-Feb-2022, Manuscript No. iphsj-22-12506;
Editor assigned: 12-Feb-2022, Pre QC No. iphsj-22-12506 (PQ);
Reviewed: 25-Mar-2022, QC No. QC No. iphsj-22-12506;
Revised: 31-Mar-2022, Manuscript No. iphsj-22-12506(R);
Published:
08-Apr-2022, DOI: 10.36648/1791-809X.16.4.933
Abstract
Introduction: Stroke is the most common cause of disability in the adult and elderly population and one of the major causes of hospitalization. Impairment of upper limb function is among the most common motor disabilities and it has a great impact on functional and social independence of patients and thus these disabilities represent a major public health problem. Constraint Induced Movement Therapy is an intervention that has been used mainly for the treatment of the upper extremities for stroke patients. When a person’s brain is damaged by a stroke, it often becomes more difficult to move an arm. Therefore, the person tends to use the arm less. This leads to shrinkage of the regions of the brain that control arm movement. Movement of the arm gets even more difficult. Constraint Induced Movement Therapy produces a large rewiring of the brain; that is after treatment, more of the brain works to move the weaker arm than before the therapy. The study was intended to identify the effect of Modified Constraint Induced Movement Therapy on motor performance and daily functions in patients one to nine months after stroke.
Major objectives of the study were,
1. To evaluate changes in motor performance of the upper extremity after Modified constraint Induced Movement therapy.
2. To evaluate changes in fine motor movements of the hand after Modified constraint Induced Movement therapy.
3. To identify changes in daily living functions in patients treated with Modified constraint Induced Movement therapy.
Materials and methods
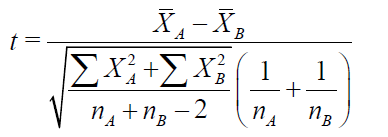
The sample for the study were adult male and female persons one to nine months after stroke with hemiparesis or hemiplegia with age range from 40-80 years who attended the Neurology Department, Medical College, Thiruvananthapuram. After considering the inclusion and exclusion criteria the patients are grouped to two groups by using simple randomization technique. Total 210 patients were selected for the study with 105 in each experimental and control group. Both the groups were assessed by Fugl Meyer Assessment, Action Research Arm Test and the Barthel Index. The experimental group received standard therapy offered in the hospital along with the Modified Constraint Induced Movement Therapy. The control group received the standard therapy offered in the hospital. Follow up assessments were done in the 6th and 10th week by using the same assessment tools. Pre and post assessments were done by the neurologist.
In this study Modified Constraint Induced Movement Therapy means
1. Structured therapy emphasizing affected arm use in the functional task practice for 30 minutes /days for 3 days per weeks for 10 weeks
2. Less affected or unaffected arm restraint 5 days per weeks for 5 hours Structured therapy includes functional practice sessions approached in small steps of progressively increasing difficulty and multiple repetitions of functional task. It is divided into 5 sessions each with 2 weeks duration.
The patient is instructed to wear a constraint sling for 5 hours per day, 5 days a week for 10 weeks. The purpose of the sling was to act as a reminder to refrain from using his less affected or non-affected hand for functional activities. However, the sling allows them to use that arm for gross movement and support for a loss of balance if needed.
The findings of the study showed that the group treated with Modified constraint Induced Movement Therapy had highly significant improvement in the motor performance of the upper extremity as measured by the Fugl Meyer Assessment (p=0.000), fine motor movements of the hand, especially grasp, grip, pinch and gross movement function indicated by the Action Research arm Test score (p=0.000) and improved ability in meeting the activities of daily living as measured by the Barthel Index score (p=0.000).
Conclusion: This study proved that Modified constraint Induced Movement Therapy is more effective in improving the motor performance of the upper extremity, fine motor movements of the hand and thereby increasing the ability to meet activities of daily living in stroke patients.
Keywords
Canned drinks; microorganism; health implications
Introduction
“Nobody can go back and start a new beginning,
But anyone can start today and make a new ending”
(Maria Robinson)
Stroke remains as one of the most devastating of all neurological
diseases, often causing death or gross physical impairment or
disability. As many countries throughout the world undergo the
epidemiological transition of diseases, trends in the prevalence
of stroke have dramatically changed. The global burden of
stroke is high, inclusive of increasing incidence, mortality, DALYs,
and economic impact, particularly in low and middle income
countries. The implementation of better surveillance systems
and prevention programs are needed to help track current trends
as well as to curb the projected exponential increase in stroke
worldwide (Mukherjee D and Patil CG, 2011).Currently there are
more than 6.5 million people living who have had strokes. Of
these who survive, 50% to 70% will be functionally independent
and 15% to 30% will live with permanent disability. Twenty
percent will require long term care after 3 months. Common long
term disabilities include hemi paresis, inability to walk, complete
or partial dependence in activities of daily living, aphasia and
depression. In addition to the physical, cognitive and emotional
impact of the stroke on the survivor, the stroke affects the life
of the caregiver, and family of the stroke victim (Lewis et.al,
2011). An increasing body of scientific evidence suggests that
cortical functional reorganization occurs after central nervous
system damage, and that this reorganization interacts with
environmental influences that may facilitate functional recovery.
In stroke patients, upper limb paresis affects many activities of daily life. Reducing disability is therefore a major aim of
rehabilitation programmes for hemiparesis patients. Constraintinduced
movement therapy (CIMT) is a current approach to
stroke rehabilitation that implies the forced use and the massed
practice of the affected arm by restraining the unaffected
arm. Modified CIMT, as developed by Page and colleagues,
represents a distributed practice pattern in which the mitt is
worn for several hours each day over a 10-week period and this
home-based practice is supplemented with outpatient therapy
several times each week. It is interesting that 27 years after the
original formulation of CIMT, the ability of a patient to initiate
finger extension has been validated as a primary predictor of the
successful application of CIMT [1].
Background of the Study
Stroke is a major public health concern. It is the second leading
cause of mortality worldwide and third most common cause
of death in the industrialized world. Currently there are more
than 6.5 million people living who have had strokes. Of these
who survive, 50% to 70% will be functionally independent and
15% to 30% will live with permanent disability. Twenty percent
will require long term care after 3 months. Common long term
disabilities include hemi paresis, inability to walk, complete
or partial dependence in activities of daily living, aphasia and
depression. In addition to the physical, cognitive and emotional
impact of the stroke on the survivor, the stroke affects the lives of
the caregiver, and family of the stroke victim (Lewis et. al, 2011).
More than 80% of the stroke survivors have paresis of the UL,
and 30%-60% of these patients cannot use the paretic UL (PUL)
which compromises their independence and quality of life [2].
Decreased arm function is common following stroke and impacts
on a person’s ability to perform activities of daily living [3].
Constraint induced movement therapy was developed at the
University of Alabama Birmingham By Edward Taub as Director
for the CI therapy research group. The study by Taub showed
brain activity actually improves with CIMT treatment. “This
finding offers hope to researchers who believe it may be possible
to stimulate or manipulate brain areas to take over lost functions,
a process known as cortical reorganization,” says Dr. Taub.
Constraint induced therapy is intended to help stroke patients
overcome ‘learned nonuse’ of the paretic arm by discouraging
the use of the unaffected or less affected arm in combination
with intensive training of the paretic arm.
CIMT consists of three components
• Massing of repetitive, structured, practice-intensive
therapy in use of the more-affected arm
• Restraint of the less-affected arm
• Transfer program, which includes monitoring arm use
in life situations and problem solving to overcome perceived
barriers to using the extremity [3].
The initial protocol for constraint Induced movement therapy
offers
• Promoting use of the more affected upper extremity for
a target of 90% of waking hours by restraining the less affected
upper extremity for 2-3 weeks’.
• Training of the more affected upper extremity is given
6 hours daily for 10 consecutive week days during that period
(massing of practice or concentrated, repetitive training).
A prospective single blinded, randomized controlled study to
investigate the beneficial effect of Modified Constraint Induced
Movement Therapy in improving the function of hemiplegics
upper extremity in the early sub-acute stroke patients concluded
that significant improvement in hand function could be achieved
with the therapy in sub-acute patients, which was maintained up
to 12 weeks follow up [4].
In addition to improving functional use of the affected arm
and daily functioning Modified Constraint Induced Movement
Therapy improved motor control strategy during goal directed
teaching, a possible mechanism for the improved motor
performance of stroke patients undergoing this therapy. Now the
trials are underway to determine the cost-effective ways to offer
the therapy and totally home based computer assisted constraint
induced movement therapy.
Statement of the Problem
A study to assess the Effect of Modified Constraint Induced
Movement Therapy on motor performance and daily functions in
patients one to nine months after stroke.
Operational Definitions
Effect
In this study, the word effect implies the outcome of Modified Constraint Induced Movement Therapy on motor performance
and daily functions in patients 1-9 months after stroke as
evidenced by increased scores in Fugl Meyer assessment, Action
Research Arm Test and Barthel Index.
Modified Constraint Induced Movement
Therapy
Modified Constraint Induced Movement Therapy encourages
the patient to use the weakened extremity by restricting the
movement of the normal extremity. In this study Modified
constraint Induced Movement Therapy consisting of:
1. Structured therapy emphasizing affected arm use in
functional activities for 30 minutes per days for 3 days per weeks
for 10 weeks.
2. Less affected arm or non-affected arm restraint 5days /
weeks for 5 hours.
Motor Performance
In this study the motor performance means the scores obtained
by assessing the hand function using Fugl Meyer Assessment and
Action Research Arm Test.
Daily Functions
In this study Daily function means the person’s ability to meet
the self care needs such as feeding, bathing, grooming, dressing,
elimination needs and mobility as per the scores obtained by
using The Barthel Index.
Stroke
Stroke is defined as rapidly developed clinical signs of focal (or
global) disturbance of cerebral functions lasting more than 24
hours or leading to death, with no apparent cause other than
a vascular origin. Included are subarachnoid hemorrhage,
intracerebral haemorrhage and ischemic brain infarction, both
embolic and non embolic. Transient ischemic attacks are excluded
according to this definition
Patients
Adult male and female persons 1-9 months after stroke with
hemiparesis or hemiplegia with age range from 40-80 years.
Objectives
General Objectives
To evaluate changes in motor performance of the upper extremity
and daily functions in patients treated with Modified constraint
Induced Movement Therapy as evidenced by increased post test
scores in Fugl Meyer Assessment, Action Research Arm test and
The Barthel Index.
Specific Objectives
1. To evaluate changes in motor performance of the upper
extremity after Modified Constraint Induced Movement Therapy
as measured by pretest and posttest Fugl Meyer Assessment
scores.
2. To evaluate changes in fine motor movements of the
hands evidenced by increased scores in Action research Arm Test
after Modified Constraint Induced Movement Therapy
3. To evaluate changes in daily functions in patients
treated with Modified Constraint Induced Movement Therapy as
evidenced by increased scores in the Barthel Index.
Hypothesis
Null Hypothesis
Modified Constraint Induced Movement Therapy will not
influence motor performance and daily functions in patients 1-9
months after stroke.
Alternate hypothesis
Modified Constraint Induced Movement Therapy will influence
motor performance and daily functions in patients 1-9 months
after stroke.
Methodology
Research Approach
In the present study experimental approach was used to identify
the effect of Modified Constraint Induced Movement Therapy on
motor performance and daily functions in stroke patients.
Research Design
The present study is a randomized controlled trial to assess the
effect of modified constraint induced movement therapy on
motor performance and daily functions in stroke patients. The
researchers study the cause and effect relationship between
Modified Constraint Induced Movement Therapy and motor
performance and daily functions are studied and compared
with the standard therapy used in the hospital. In this study the
independent variable is an example of treatment variable, that
is Modified Constraint Induced Movement Therapy and the
dependent variables are motor performance and daily functions
as evidenced by scores in Fugl Meyer Assessment, action
Research Arm Test and The Barthel Index.
In the present study the investigator tried to reduce or eliminate
all factors that influence the dependent variable other than the
independent variable. This is done by Research manipulation,
use of a control group and randomization. Here the modified
Constraint Induced Movement Therapy is administered to the
experimental group along with the standard therapy offered in
the hospital and the control group received only the standard
therapy offered in the hospital. The pre and post scores were
compared in both groups to identify the effect of therapy.
The use of a control group helps the researcher to generalize
the results in comparison with the control group. The use of
randomization ensures that each subject has an equal chance of
being place in to experimental or control group. The selection
bias is avoided by randomization of samples to experimental
group and control group. The investigator also tried to control
the research situation by maintaining the constancy of condition
and constancy of communication. The investigator prepared
the information giving to the participants ahead of time and delivered the same message to all participants. Also care is taken
in the preparation and adherence to the intervention protocol.
The cause and effect relationship thus measured will truly reflect
the effect of modified Constraint Induced Movement Therapy.
Setting of the Study
The setting of the study was the Out Patient Department,
Department of Neurology, Tertiary Care centre, Medical college
Hospital, Thiruvananthapuram. The Out Patient Department
Days are on Monday, Thursday and Saturday from 9 am to 5 pm.
Population
The patients having stroke who come to the Department of
Neurology, Medical College, Thiruvananthapuram, during the
study period and in the age group of 40-80 years.
Sample Size
Adult male and female persons 1-9 months after stroke with
hemiparesis or hemiplegia age range from 40-80 years were
selected for the study.
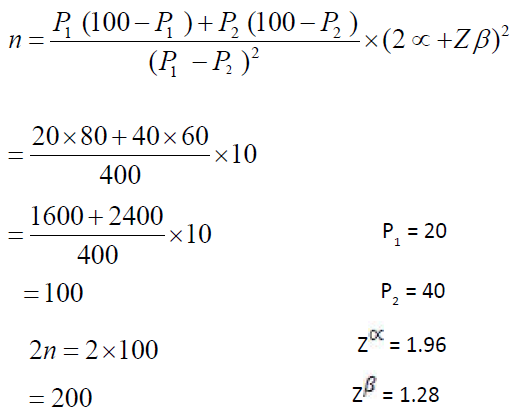
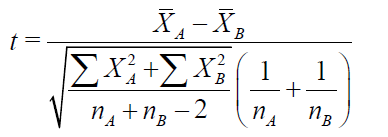
After conducting the pilot study the sample size is calculated by
using the following formula
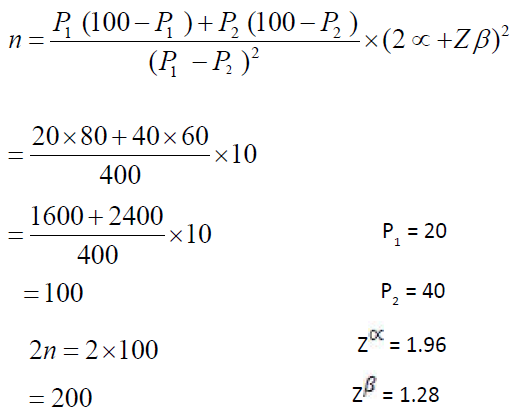
By using the above formula the total patients required for the
study was calculated as 200. 5% extra was added to the total
population and the sample size for the study finalized as 210, 105
each in the experimental and control group.
Sample Size is finalized as,
No. of patients in the Experimental group = 105
No. of patients in the control group = 105
Sampling Technique
The patients having stroke comes to the department of
Neurology, Medical College, and Thiruvananthapuram during the
study period and in the age group of 40-80 years were the target
population for the study. Eligible samples were selected after
considering the inclusion and exclusion criteria based on the
baseline and clinical assessment made by the researcher guided by
the Neurologist. After that, the eligible samples were randomized
in to two groups, experimental group and control group by using
simple randomization technique. Computer generated random digit table was used to facilitate the randomization process.
Duration of the Study
The duration of the study was 3 years 6 months from January
2010 to July 2013.
Inclusion Criteria
1. Adult male and female persons 1-9 months after stroke
with hemiparesis or hemiplegia
2. Patients with first ischemic stroke
3. The persons selected within the age group of 40-80 years
4. Patients with the ability to extend the Meta carp phalangeal
and inter phalangeal joints at least 10 degree and actively
extend the wrist at least 20 degree.
5. Patients with spouse, son or daughter who is willing to give
support and directions in the home as per the advice of the
investigator.
6. The patients who give a signed consent form to participate
in the study.
Exclusion Criteria
1. Comorbidities which may affect the outcome of management
such as Renal failure, Cardiac contraindications and
Neuropathies.
2. Cognitive problems, mentally ill, confused or disoriented
and aphasia
3. Non cooperative patients
4. Patients who are receiving interventions like Sidha , Homeo
and Ayurveda
Tool and Technique
Tool
The tools used in the study were the following
1. Structured Interview Schedule
2. Fugl Meyer Assessment
3. Action Research Arm Test
4. The Barthel Index
Technique
The techniques used for collecting the data were the following
1. Interview
2. observation
3. Measuring fugl Meyer assessment score
4. Assessment of scores in Action Research Arm Test
5. Assessment of scores in the Barthel index
6. Teaching
7. Demonstrations
Tool-1: Structured Interview Schedule
The structured interview schedule consisted of two sections
Section. A: Baseline Data of the participant
The baseline data of the client include age, sex, religion,
education, marital status, dietary habits and personal habits
Section B: Clinical Data of the participant
In this study Clinical Data of the client consisted of co morbid
condition of the client, clinical features, Diagnosis, and routine
blood investigation findings.
Tool -11: Fugl Meyer Assessment of Physical Performance
In the present study, The Fugl Meyer Assessment developed
by Fugl-Meyer et al., (1980) is used to measure the motor
performance of the upper extremity in stroke patients. It is
a performance based measure that provides quantitative
assessment of voluntary movement, balance, sensation, passive
range of motion, and pain. The FM is based on the patterns of
motor recovery delineated by Twitchel (1951). Items in the motor
section were developed from the seven stages of motor recovery
following stroke described by Brunnstorm (1970), and items in
the passive range of motion section were derived based on the
standards of the American Academy of Orthopaedic surgeons.
Test items are rated according to a 3- point ordinal scale from 0
(no function) to 2 (full function), secondary to direct observation
of patient functioning. Scores across the five sessions are summed
for a maximum total score of 226 [5].
The measure has been found to possess adequate inter –rater
and test –retest reliabilities [6]. The total motor score is the
most commonly used subscale of the Fugl Meyer Assessment,
and various investigators have proposed numerical ranges for
categorization of stroke severity [5-7]. In this study, the upper
extremity sub scale of Fugl Meyer Assessment developed by Fugl
Meyer (1980) is used to measure the motor performance of the
upper extremity in stroke patients.
In this study the assessment included testing of 9 areas such as
• Reflexes (Maximum possible score-4)
• Flexor Synergy (Maximum possible score-12)
• Extensor Synergy (Maximum possible score-6)
• Movement combining Synergies (Maximum possible score-6)
• Movement out of Synergy (Maximum possible score-6)
• Normal Reflex Activity (Maximum possible score-2)
• Wrist-Stability, flexion, extension and circumduction
(Maximum possible score-10)
• Hand- finger mass flexion, extension, and grasp (Maximum
possible score-14)
• Coordination, tremor, dysmetria and speed (Maximum
possible score-6)
Total maximum score of upper extremity = 66
Tool- 111: Action Research Arm Test
The Action Research Arm Test is scored on a four level ordinal
scale (0-3) [8], there are four subtests: Grasp, Grip, Pinch, and
Gross Movement. Items in each are ordered so that:
• If the subject passes the first, no more need to be
administered and he scores top marks for that sub test;
• If the subject fails the first and fails the second, he
scores zero, and again no more tests need to be performed in
that subject;
• Otherwise he needs to complete all tasks within the
subtest
• The Action Research Arm Test was scored in the
following way
• 0 = cannot perform any part of the test
• 1 = perform the test partially
• 2 = complete the test, but takes an abnormally long
time, varying from 50- 60 seconds.
• 3 = perform the test normally in less than 5 seconds.
Grasp sub scale consisted of 6 items and the total score ranged
between 0-18
Grip sub scale consisted of 4 items and the total score ranged
between 0 -12
Pinch sub scale consisted of 6 items and the score ranged
between 0-18
Tool-1V: Barthel Index: The Barthel Index developed by
Mahoney& Barthel in 1965 is used in the present study
to assess the daily functions of the patient. It is a 10 item
measure developed to assess functional independence in
personal care and mobility in persons with neuro muscular and
musculoskeletal disorders. Items emphasize various activities
of daily living, including feeding, transferring, personal hygiene,
toileting, bathing, mobility, dressing and controlling bowel and
bladder functions. Each item is assigned a score of 0, 5, 10, or
15, with differential weighting reflecting the relative importance
of each disability with respect to level of assistance required for
performance. Items are summed to obtain a total score ranking
from 0-100, with a score of 100 representing the highest degree
of independence. Excellent internal consistency and reliability
has been demonstrated in persons with stroke undergoing
rehabilitation, with Cronbach’s coefficient alphas of 0.87 at time
of admission and 0.92 at time of discharge (Shah et. al, 1989).
Adequate inter- rater and test-retest reliabilities also have been
shown, with kappa scores of 0.70-0.88 (Loewen and Anderson,
1988) and 0.98 (Wolfe et. al, 1991), respectively.
The Barthel Index has been extensively studied and has had high
construct validation [9]. It has also been shown to have high inter
rater reliability [10].
The scores can be obtained from discussing the questions with
the patient and family.
Pilot Study
After obtaining permission from the Head of the Department,
Neurology and ethical clearance from the Medical College,
Thiruvananthapuram Pilot study was conducted to determine
the feasibility, reliability, validity and practicability of the
designed tool and research methodology. Pilot study was
conducted from 01/02/2010-30/06/2010 in the Out Patient
Department, Department of Neurology, Medical College, and
Thiruvananthapuram.
After satisfying the inclusion and exclusion criteria experimental
group and control group were selected by simple randomization.
Pilot study was conducted in 20 participants after obtaining
individualized consent in local language from the participant
and one relative. Modified Constraint induced movement
therapy was administered along with the standard therapy to
the experimental group. The control group received the standard
therapy offered in the hospital. The Protest and post test scores
of experimental and control groups obtained at the 1st week,
6th week and 10th week were compared and analyzed using
appropriate statistical methods and discussed with the experts.
In order to assess the effectiveness of Modified Constraint
Induced Movement Therapy on motor performance and daily
functions one way repeated measures ANOVA was carried out.
The F value (3802.53) on Fugl meyer assessment, F value (1201)
on The Barthel Index and F value (1923.01) on Action Research
Arm Test shows that the variation in the scores are significant at
0.01 level.
After analysing the pilot study, results were discussed with the
experts. The pilot study helped in testing the feasibility and
practicability of the tool.
Data Collection Process
The investigator obtained prior permission for the conduct of
the study from the Head of the Department, Department of
Neurology, Medical College, and Thiruvananthapuram. Ethical
committee clearance was obtained from The Human Ethical
Committee, Medical College, and Thiruvananthapuram
Total 210 samples were selected after satisfying inclusion and
exclusion criteria and randomized by simple randomization
method using computer generated random digit table. The
investigator met each participant individually; established rapport
with them and the purpose of the study was explained to them.
It was assured to them that all data will be kept confidential and
used only for the study purpose. After that verbal and written
consent of the participants in English/ local language were
obtained for the study.
Initial assessment of all participants was done by the researcher
which included collecting the baseline data and clinical data and
Fugl Meyer Assessment, Action Research Arm Test and Barthel
Index. Based on the randomization interventions were provided.
Experimental Group
After the initial assessment the investigator herself taught about
modified constraint induced movement therapy to the patient
and responsible bystander. On the first day of each session,
the researcher demonstrated how to practice that particular
session of the therapy and 30 minutes practice session was done under the supervision of the researcher. Return demonstration
by the patient and bystander also done to make sure that the
participant can do the home therapy sessions in the proper way.
It was instructed to maintain an activity diary for the participant
and bystander about the sessions in the home. The researcher
herself makes sure that the participant is doing the sessions by
observing the diary and through phone call.
In this study modified constraint induced movement therapy
means
1. Structured therapy emphasizing affected arm use in
functional task practice for 30 minutes/ days for 3 days per weeks
for 10 weeks
2. Less affected or unaffected arm restraint 5 days per
weeks for 5 hours (Figure 1).
Structured therapy includes functional practice sessions
approached in small steps of progressively increasing difficulty
and multiple repetitions of functional task. It is divided in to 5
sessions each with two weeks duration.
The structured therapy consists of 5 sessions in small steps of progressively increasing difficulty .The investigator herself teach
and assist the patient to practice the structured therapy at 1st , 3rd,
5th , 7th , and 9th week. The taught practice has to be repeated by
the patient in the home therapy sessions under the supervision
of caregiver.
The patient is instructed to wear a constraint sling for 5 hours
per day, 5 days a week for 10 weeks. The purpose of the mitt is
to act as reminder to refrain from using his less affected or nonaffected
hand for functional activities. However the mitt allows
them to use that arm for gross movements and support for a loss
of balance if needed.
Structured therapy is divided in to 5 sessions each with two
weeks duration.
1st and 2nd weeks
Sitting with arm on the table. Brief stretch with hand on the table
top. Lifting and lowering an object (glass) held in palm and fingers
over end of table. Lifting glass from table by radial deviation at
wrist, fore arm in mid rotation, placing it to left and right by wrist
flexion and extension. Sliding glass along table top to target by
extending wrist.
Tapping tasks
1. Touch each fingertip to thumb in sequence as rapidly as
possible.
2. Tapping table with single fingers.
3rd and 4th Weeks
1. Reach out and pass the glass by sliding arm on the table
. Slide glass forward in different directions (across the body, out
to the side) to touch targets keeping fore arm in mid rotation.
2. Hand cupping tasks to train opposition of radial and
ulnar sides of the hand
a, Hold seeds in palm and pour in to a dish
b, scooping coins from table top in to palm of other hand
5th and 6th week
1. Slide glass backwards and fore wards to touch targets by
extending and flexing elbow
2. Pick up different objects between thumb and finger ,
place them on various targets
a. Pick up objects between thumb and 4th and 5th fingers.
b. Pick up small objects from inside a cup with thumb and
several fingers, thumb and fore finger
c. Pick up paper from opposite shoulder
d. Pick up and hold saucer using grip in which hand spans
the whole diameter, thumb extended to the maximum, fingers
stretched wide.
7th and 8th Weeks
1. Reach forwards, sideways or backwards to pick up an
object, transport it to another place (eg. To the floor) pick it up again reach as far in one direction as possible then put it down
2. Pick up larger objects from one side of table and place
to other side; vary weight, distance to be moved
a, Pick up a glass of water and drink
b, Pick up jug of water and pour in to glass; vary amount of water
and size of jug
9th and 10th Weeks
1. a, Point to different parts of a target drawing on sheet
of paper on wall
b, Reaching up to take object from shelf, vary height according
to ability
2. a, turn door handles or knobs
b, turn pages of magazine.
At 12th week the reassessment of the patient was done to assess
the effect of modified constraint induced movement therapy.
The outcome was measured by using Fugl Meyer Assessment,
Action Research Arm Test and barthel Index.
Control Group
After the initial collection of the baseline data, pre assessment
was done by using Fugl Meyer Assessment, action Research Arm
Test and barthel Index. The researcher herself makes sure that
the participant is getting the standard therapy offered in the
medical college hospital. The initial step in the therapy includes
the following.
1. Keep the affected upper extremity in abducted position
at the shoulder, most of the time especially during sleep. This is
to prevent periarthritis shoulder).
2. While in bed keep the affected arm abducted at 900. Flex
the elbow to 900 passively, and then externally rotate till the fore
arm touches the bed. Then internally rotate 1800 again so that
fore arm touches bed. Again externally rotate 1800 so that the
fore arm touches bed. Repeat this passive exercise to prevent
periarthritis shoulder.
3. Hold the upper extremity at the wrist and then passively
rotate at the shoulder. This is to prevent periarthritis shoulder.
4. In sitting position place hand on bed with elbow in
extension and fingers spread out. Tap over the triceps muscle.
This is aimed to increase extensor tone in the upper extremity
and prevent flexor synergy.
5. Patient lie in supine position. Flex at the knee joint 900
with foot placed on the bed. Patient is encouraged to lift the
buttocks up and down actively. This will help to strengthen the
paraspinal muscles.
6. The therapist stands on the side of paralyzed side of the
patient. Patient lies towards the edge of the bed on that side. The
therapist holds the thigh just above the knee joint and with the
other hand holds the foot just above the ankle joint, and flex at
the hip 900 and flex knee to 900. Internally rotate at the hip joint
as far as possible. Extend at the hip joint 5 to 10 degree with knee beyond the edge of the bed, maintaining the 900 flexion at the
knee. Then extend the knee joint. The leg which is beyond the
edge of the bed is returned to the bed. This is aimed to reduce
adductor spasticity.
7. Patient lie in supine position. Flex at the knee joint 900
with foot placed on the bed. Separate the knee joint as far as
possible. This involves external rotation and abduction of the hip
joint. Then return to the apposed position. This is also aimed to
reduce adductor spasticity.
8. At the end of the 12th week the outcome was measured
by using Fugl Meyer Assessment, Action Research Arm Test and
Barthel Index.
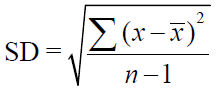
Plans for Data Analysis
The collected data were transformed in to the master sheet and
necessary coding was done and the following statistical tests
were done. Diagrams and charts were also drawn wherever
necessary to give due importance to most salient findings. For all
computations SPSS package was used.
Three kinds of average or statistical measures of central tendency
were used- the mode, median and mean.
Chi square test
Comparison of demographic data of the participants in
experimental and control group was done by using Chi square
test.
The chi square test is a non-parametric procedure used to test
hypothesis about proportions of cases that fall in to different
categories, as when a contingency table has been created.
The Chi square statistics is computed by comparing observed
frequencies and expected frequencies. Expected frequencies
were calculated on the basis of observed total frequencies for
the rows and columns of a contingency table [11].
Need to insert the formula of chi-square test
O=observed frequency
E= Expected frequency
Independent “t” test
The parametric procedure used for testing differences in group
means is called the “t” test.
In this study Independent “t” test was used for testing the
statistical significance of differences between two group means.
One Way Repeated measures ANOVA
In order to assess the effectiveness of Modified Constraint
Induced Movement Therapy and standard treatment on motor performance and daily functions One way Repeated
Measures ANOVA was carried out. In experimental and control
group Fugl Meyer Assessment, Action Research Arm Test and
Barthel index scores were assessed at different stages such
as pre intervention(1st week), 6th week and 10th week of post
intervention. One way repeated measures ANOVA test was used
to find whether the variation at different stages is significant or
not.
Analysis of covariance (ANCOVA)
ANCOVA tests the significance of differences between group
means after first adjusting the scores on the dependent variable
to remove the effect of covariate, so that the results more
precisely reflect the effect of an intervention. The adjustment
uses regression procedures. In essence the first step in ANCOVA
is the same as the first step in hierarchical multiple regression.
Variability in the dependent measure that can be explained by
the covariate is removed from further consideration. ANOVA is
performed on what remains of Y’s variability to see whether,
once the covariate is controlled, significant differences between
groups means exist.
Computation of ANOVA for repeated measures is given below.
First obtain the values N and n.
Analysis of covariance (ANCOVA)
ANCOVA tests the significance of differences between group
means after first adjusting the scores on the dependent variable
to remove the effect of covariate, so that the results more
precisely reflect the effect of an intervention. The adjustment
uses regression procedures. In essence the first step in ANCOVA
is the same as the first step in hierarchical multiple regression.
Variability in the dependent measure that can be explained by
the covariate is removed from further consideration. ANOVA is
performed on what remains of Y’s variability to see whether,
once the covariate is controlled, significant differences between
groups means exist.
Post hoc test
Once the F-ratio indicates statistical significance, additional
hypothesis tests are done to determine which means are
significant and which are not. Post hoc test is used to compare
the mean scores at different time interval taken two at a time
(pair wise) to assess where a significant mean difference exist.
Results Discussion
Effect of Modified Constraint Induced Movement Therapy on Motor Performance of the upper Extremity (Table 1)
| Fugl Meyer assessment |
Mean |
SD |
N |
F# |
Pair |
Mean Diff. |
LS $ |
| Experimental Group |
1st week
(T1) |
32.1 |
4.9 |
105 |
3907.58** |
T1 & T2 |
13.66** |
Significant |
6th week
(T2) |
45.7 |
4.3 |
105 |
T1 & T3 |
29.85** |
Significant |
10th week
(T3) |
61.9 |
2.9 |
105 |
T2 & T3 |
16.19** |
Significant |
Table 1. Fugl Meyer Assessment Score at Different Intervals One way repeated measures ANOVA.
© Under License of Creative Commons Attribution 3.0 License
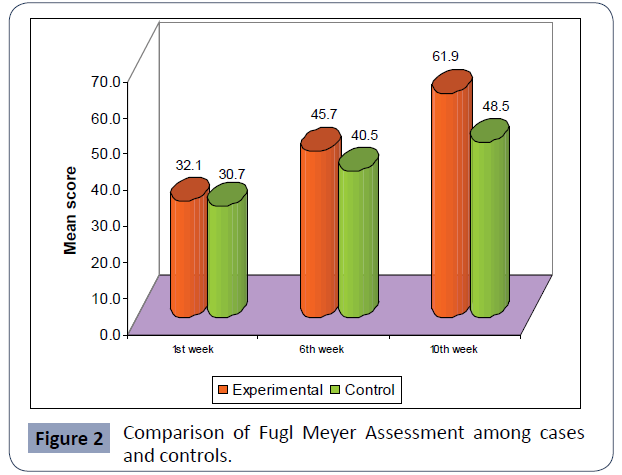
In experimental group, the motor performance of upper extremity, as indicated by the Fugl Meyer Assessment Scores different stages such as preintervention (1st week), 6th week and 10th week post intervention are respectively 32.1, 45.7 and 61.9.The F value, 3907.58 shows that the variation in physical performance of upper extremity at different interval time is significant at 0.01 level.
The mean at difference between initial and 6th week assessment is 13.66, the pair wise comparison with Bonferroni correction shows that the difference is statistically significant at 0.01 levels. It means that, through the intervention the score significantly increased at 6th week when compared with 1st week. The increase in score at 10th week in comparison with 1st week (29.85), and in comparison with 6th week (16.19) is also significant at 0.01 levels.
Thus it can be concluded that motor performance of upper extremity significantly increases with the intervention progressing in experimental group and hence the intervention, modified Constraint Induced Movement therapy is effective in increasing the motor performance of upper extremity (Table 2) (Figure 1).
| |
Experimental |
Control |
T |
p |
| Mean |
Std. Error |
N |
Mean |
Std. Error |
N |
| 1st week |
32.09 |
0.48 |
105 |
30.70 |
0.53 |
105 |
1.93 |
0.055 |
| 6th week |
45.74 |
0.42 |
105 |
40.50 |
0.51 |
105 |
7.98** |
0.000 |
| 10th week |
61.93 |
0.28 |
105 |
48.48 |
0.54 |
105 |
22.06** |
0.000 |
Table 2. Comparison of Fugl Meyer Assessment among cases and controls.
Comparison of Motor performance of Upper Extremity between groups by Fugl Meyer Assessment
Figure 1 Symbolic Representation of The Study.
Comparison of Fugl Meyer Assessment scores at 1st week shows no significant variation in the motor performance of the upper extremity among the groups before the intervention. After the intervention, the scores at 6th and 10th week indicates that, the improvement in motor performance of the upper extremity in the experimental group is statistically significant than the control group at 0.01 level (p=0.00).
Effect of Modified Constraint Induced Movement Therapy on daily functions as evidenced by The Barthel Index score
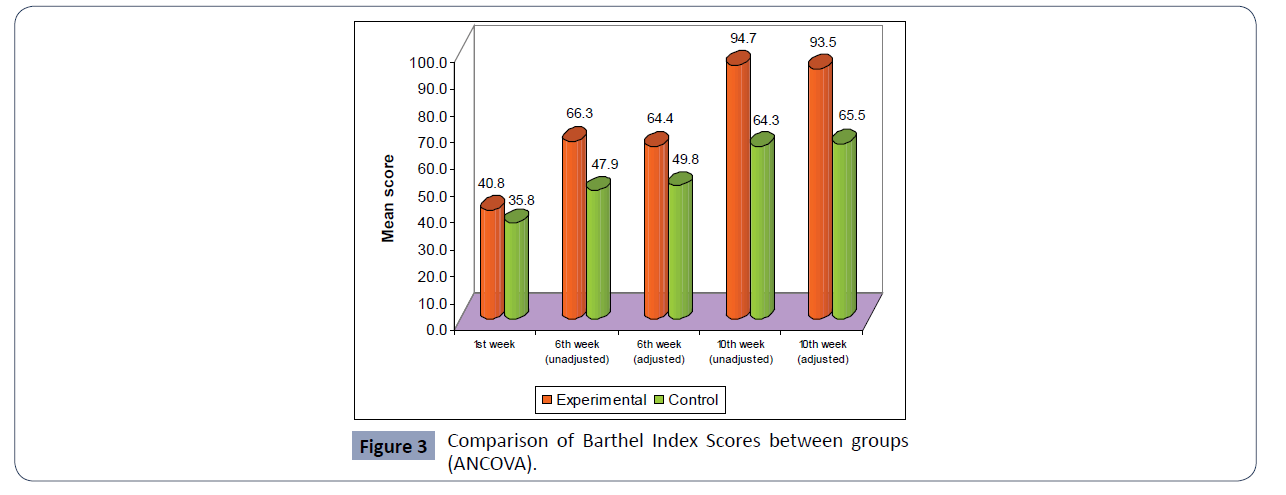
One way repeated measures ANOVA was carried out to assess the effect of Modified Constraint Induced Movement Therapy on Activities of daily living as measured by the Barthel Index score. By using independent “t” test the statistical significance of differences between two group means were identified. As there is significant difference in the mean score of initial assessment between groups, ANCOVA was applied to the Barthel Index scores at 6th and 10th week after correcting for differences in the initial scores (Table 3).
| |
Mean |
SD |
N |
F# |
Pair |
Mean Diff. |
LS $ |
| Experimental |
1st week (T1) |
40.8 |
12.9 |
105 |
1288.38** |
T1 & T2 |
25.45** |
Significant |
| 6th week (T2) |
66.3 |
12.7 |
105 |
T1 & T3 |
53.86** |
Significant |
| 10th week (T3) |
94.7 |
8.0 |
105 |
T2 & T3 |
28.41** |
Significant |
Table 3. Barthel Index Scores at Different Intervals (One way repeated measures ANOVA).
Effect of Modified Constraint Induced Movement Therapy on Daily functions
In experimental group, the ability to meet the activities of daily living as measured by The Barthel Index scores at different stages such as pre intervention (1st week), 6th week and 10th week post intervention are respectively 40.08, 66.3 and 94.7. The F value, 1288.38 shows that the variation in ability to meet activities of daily living at different interval time is significant at 0.01 level.
The mean difference between initial and 6th week assessment is 25.45, the pair wise comparison with Bonferroni correction shows that the difference is statistically significant at 0.01 levels.
It means that, through the intervention the score significantly increased at 6th week when compared with 1st week. The increase in score at 10th week in comparison with 1st week (53.86), and in comparison with 6th week (28.41) is also significant at 0.01 levels (Tables 4 and 5) (Figure 2).
Figure 2 Comparison of Fugl Meyer Assessment among cases and controls.
The above table and figure depict that the mean Barthel Index score indicating the ability to meet activities of daily living increased from 40.81 to 94.67 in the experimental group, when compared to 35.76 to 64.33 in the control group. As there is significant variation of initial scores at the pretest level, Analysis of covariance was applied to 6th and 10th week scores. From the table 4.16 it is clear that the improvement in the ability to meet activities of daily living after the intervention is significantly more in the experimental group than the control group (p=0.000).
| |
Experimental |
Control |
T |
p |
| Mean |
Std. Error |
N |
Mean |
Std. Error |
N |
| 1st week |
40.81 |
1.26 |
105 |
35.76 |
0.88 |
105 |
3.28** |
0.001 |
| 6th week |
66.26 |
1.24 |
105 |
47.90 |
1.14 |
105 |
10.91** |
0.000 |
| 10th week |
94.67 |
0.78 |
105 |
64.33 |
1.23 |
105 |
20.76** |
0.000 |
Table 4. Comparison of The Barthel Index Score between groups.
Comparison of daily functions between groups by Using Barthel Index
Effect of Modified Constraint Induced Movement Therapy On Fine Motor Movements As Evidenced By Action Research Arm Test Score
The fine motor movements of the hand are assessed by using the Action Research arm Test. It is scored on a four level ordinal scale. There are four sub tests for the assessment: Grasp, grip, pinch and gross movement. Analysis of each subtest and the whole score was done to find out the individual and total relationship of modified Constraint Induced Movement Therapy with the fine motor movements of the hand. Here also one way repeated measures ANOVA was carried out to find out the effect of Modified Constraint Induced movement therapy on fine motor movements of the hand. Independent “t” test was used to for testing the statistical significance of differences between two group means. ANCOVA was also used if there was significant differences in the initial mean score was present to determine whether the difference in the scores truly reflect the effect of intervention in the experimental and control groups.
Effect of Modified Constraint Induced Movement Therapy on Grasp (Table 6)
| Stage |
|
Mean ± SD |
df |
F |
P |
| 1st week (pre) |
Experimental |
40.8 ± 12.9 |
(1,208) |
10.79** |
0.001 |
| Control |
35.8 ± 9 |
| 6th week (Post) |
Experimental |
66.3 ± 12.7 |
(1,208) |
119.12** |
0.000 |
| Control |
47.9 ± 11.7 |
| Adjusted 6th week |
Experimental |
64.4 ± 0.9 |
(1,207) |
130.37** |
0.000 |
| Control |
49.8 ± 0.9 |
| Adjusted 10th week |
Experimental |
93.5 ± 0.9 |
(1,207) |
455.94** |
0.000 |
| Control |
65.5 ± 0.9 |
Table 5. Comparison of the Barthel Index Score between Groups (ANCOVA).
| |
Mean |
SD |
N |
F# |
Pair |
Mean Diff. |
LS $ |
Experi
mental |
1st week (T1) |
7.7 |
1.7 |
105 |
2193.92 ** |
T1 & T2 |
4.14** |
Significant |
| 6th week (T2) |
11.8 |
2.0 |
105 |
T1 & T3 |
9.51** |
Significant |
| 10th week (T3) |
17.2 |
0.9 |
105 |
T2 & T3 |
5.37** |
Significant |
Table 6. Grasp score of ARAT at different intervals (one way repeated measure ANOVA).
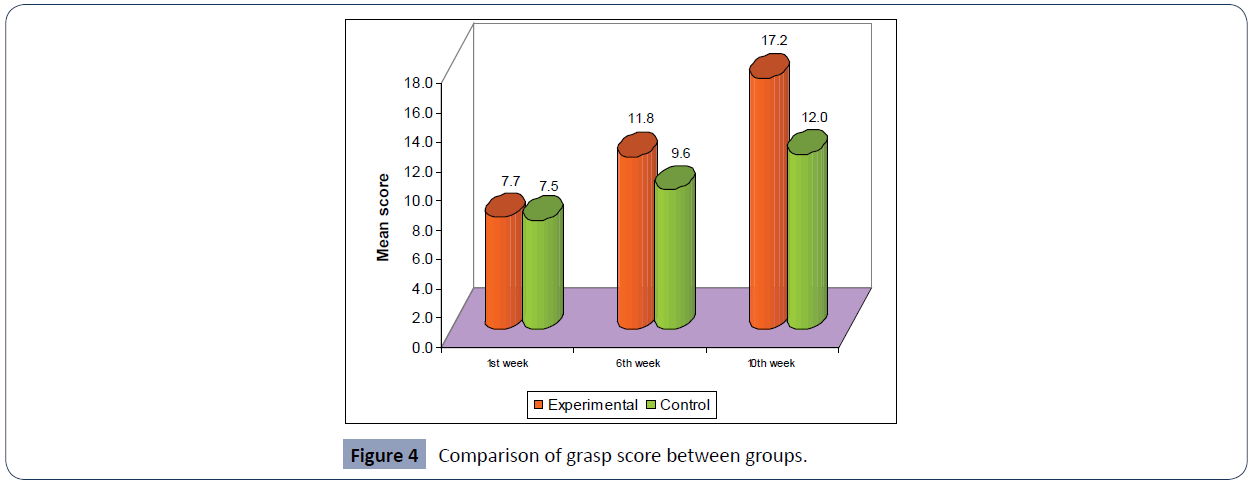
The fine motor movements especially grasp function of the hand in the experimental group at different stages such as pre intervention (1st week), 6th week and 10th week post intervention are 7.7, 11.8 and 17.2 respectively. The F value, 2193.92 shows that after the intervention significant improvement had occurred in the grasp function of the hand [12].
The mean difference between initial and 6th week assessment is 4.14, the pair wise comparison with Bonferroni correction shows that the difference is statistically significant at 0.01 levels. The increases in score at 10th week in comparison with 1st week (9.51), and in comparison with 6th week (5.37) are also significant at 0.01 levels (Table 7) and (Figure 3).
| |
Experimental |
Control |
T |
p |
| Mean |
Std. Error |
N |
Mean |
Std. Error |
N |
| 1st week |
7.66 |
0.16 |
105 |
7.46 |
0.20 |
105 |
0.77 |
0.442 |
| 6th week |
11.80 |
0.20 |
105 |
9.57 |
0.23 |
105 |
7.41** |
0.000 |
| 10th week |
17.17 |
0.09 |
105 |
11.98 |
0.23 |
105 |
21.39** |
0.000 |
Table 7. Comparison of Grasp score between groups.
Comparison of grasp movements of the hands among the groups
Figure 3 Comparison of Barthel Index Scores between groups (ANCOVA).
Comparison of grasp score between groups shows that the mean grasp scores of the experimental group increased from7.66 to11.80 at 6th week and to 17.17 at 10th week. From the result it is clear that increase in the fine motor movements of the hand is significantly more in the experimental group when compared to the control group (p=0.000).
Effect of Modified Constraint Induced Movement Therapy on Grip (Table 8)
| |
Mean |
SD |
N |
F# |
Pair |
Mean Diff. |
LS $ |
Experi
mental
group |
1st week (T1) |
4.9 |
1.3 |
105 |
1821.25 ** |
T1 & T2 |
3.29** |
Significant |
| 6th week (T2) |
8.2 |
1.3 |
105 |
T1 & T3 |
6.44** |
Significant |
| 10th week(T3) |
11.4 |
0.8 |
105 |
T2 & T3 |
3.15** |
Significant |
Table 8. Effect of Modified Constraint Induced Movement Therapy on Grip Score.
© Under License of Creative Commons Attribution 3.0 License
In experimental group, the fine motor movements of the hand as indicated by the grip sub scale scores of the Action Research Arm test, at different stages such as pre intervention (1st week), 6th week and 10th week post intervention are respectively 4.9.8.2 and11.4. The F value, (1821.25) shows that the variation in grip sub scale score at different interval time is significant at 0.01 level [13-15].
The mean difference between initial and 6th week assessment is 3.29, the pair wise comparison with Bonferroni correction shows that the difference is statistically significant at 0.01 levels. It means that, through the intervention the score significantly increased at 6th week when compared with 1st week. The increases in score at 10th week in comparison with 1st week (6.44), and in comparison with 6th week (3.15) are also significant at 0.01 levels. From the above results it is clear that modified constraint induced movement therapy produced significant improvement in the fine motor movements of the hand especially the grip function of the hand (Table 9) (Figure 4).
| |
Experimental |
Control |
t |
p |
| Mean |
Std. Error |
N |
Mean |
Std. Error |
N |
| 1st week |
4.91 |
0.13 |
105 |
4.90 |
0.13 |
105 |
0.05 |
0.958 |
| 6th week |
8.20 |
0.13 |
105 |
6.75 |
0.14 |
105 |
7.8** |
0.000 |
| 10th week |
11.35 |
0.08 |
105 |
8.61 |
0.14 |
105 |
17.29** |
0.000 |
Table 9.Comparison of Grip Score between groups.
Comparison of Grip movements of the hand among the groups
Figure 4 Comparison of grasp score between groups.
Comparison of grip scores between experimental and control groups showed significant improvement of grip function in the experimental group at 6th week (t=7.8) and at 10th week (t=17.29, p=0.000) than the control group.
Effect of Modified Constraint Induced Movement Therapy on Pinch movements of the hand (Table 10)
| |
Mean |
SD |
N |
F# |
Pair |
Mean Diff. |
LS $ |
Experi
mental |
1st week (T1) |
7.6 |
2.0 |
105 |
1277.56 ** |
T1 & T2 |
4.15** |
Significant |
| 6th week (T2) |
11.8 |
1.8 |
105 |
T1 & T3 |
8.96** |
Significant |
| 10th week (T3) |
16.6 |
1.4 |
105 |
T2 & T3 |
4.81** |
Significant |
Table 10. Effect of Modified Constraint Induced Movement Therapy on Pinch.
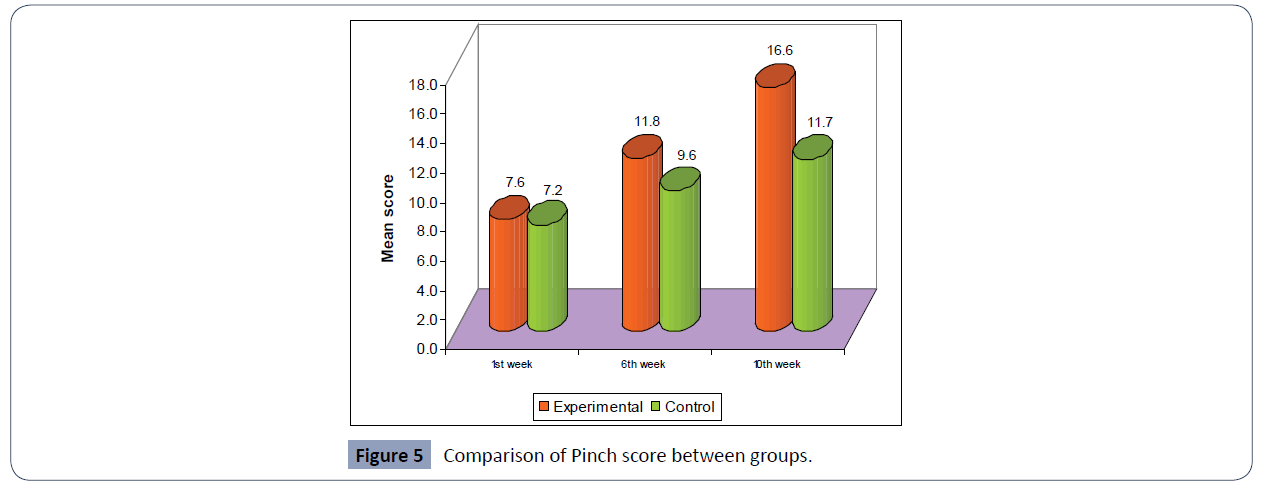
The Pinch sub scale score of Action research Arm Test indicating fine motor movement function of the hand at different stages such as pre intervention (1st week), 6th week and 10th week post intervention are 7.6, 11.8 and16.6 respectively. The F value, 1277.56 shows that the variation in pinch sub scale score at different interval time is significant at 0.01 levels [16].
The mean difference between initial and 6th week assessment is 4.15, the pair wise comparison with Bonferroni correction shows that the difference is statistically significant at 0.01 levels. It means that, through the intervention the score significantly increased at 6th week when compared with 1st week. The increases in score at 10th week in comparison with 1st week (8.96), and in comparison with 6th week (4.81) are also significant at 0.01 levels [17] (Table 11) (Figure 5).
| |
Experimental |
Control |
t |
p |
| Mean |
Std. Error |
N |
Mean |
Std. Error |
N |
| 1st week |
7.60 |
0.19 |
105 |
7.22 |
0.21 |
105 |
1.35 |
0.178 |
| 6th week |
11.75 |
0.18 |
105 |
9.57 |
0.22 |
105 |
7.7** |
0.000 |
| 10th week |
16.56 |
0.13 |
105 |
11.70 |
0.20 |
105 |
20.52** |
0.000 |
Table 11. Comparison of Pinch score between groups.
Comparison of Pinch Movements of the hand between the groups
Figure 5 Comparison of Pinch score between groups.
The maximum possible score for the pinch subscale of ARAT is 18. The pinch score of the experimental group increased from 7.60 to11.75 at 6th week (t=7.7) and to16.56at 10th week (t=20.52) [18]. It depicts that the improvement in the pinch function of the hand in the experimental group is significant at 0.01 level (p=0.000).
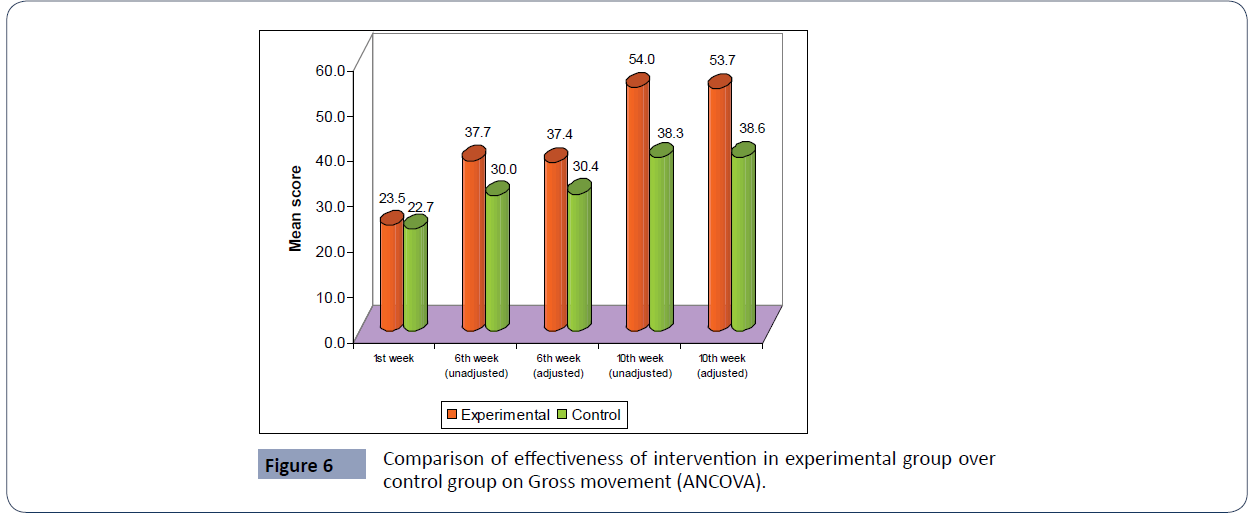
Effect of Modified Constraint Induced Movement Therapy on Gross movement (Table 12)
| |
Mean |
SD |
N |
F# |
Pair |
Mean Diff. |
LS $ |
| Experimental |
1st week (T1) |
3.4 |
1.0 |
105 |
1950.44** |
T1 & T2 |
2.64** |
Significant |
| 6th week (T2) |
6.0 |
0.6 |
105 |
T1 & T3 |
5.5** |
Significant |
| 10th week(T3) |
8.9 |
0.6 |
105 |
T2 & T3 |
2.87** |
Significant |
Table 12. Effect of Modified Constraint Induced Movement Therapy on Gross movement.
The gross movement function of the hand in experimental group, at different stages such as pre intervention (1st week), 6th week and 10th week post intervention are respectively 3.4, 6.0 and 8.9. The F value, 1950.44 indicates that that the variations in gross movement function of the hand at different interval time is significant at 0.01 level [19-22].
The mean difference between initial and 6th week assessment is 2.64, the pair wise comparison with Bonferroni correction shows that the difference is statistically significant at 0.01 levels. It means that, though the intervention the score significantly increased at 6th week when compared with 1st week. The increases in score at 10th week in comparison with 1st week (5.5), and in comparison with 6th week (2.87) are also significant at 0.01 levels. (Table 13, and 14), (Figure 6).
| |
Experimental |
Control |
T |
p |
| Mean |
Std. Error |
N |
Mean |
Std. Error |
N |
| 1st week |
3.36 |
0.09 |
105 |
3.12 |
0.06 |
105 |
2.17* |
0.031 |
| 6th week |
6.00 |
0.06 |
105 |
4.18 |
0.13 |
105 |
12.66** |
0.000 |
| 10th week |
8.87 |
0.06 |
105 |
5.90 |
0.11 |
105 |
23.39** |
0.000 |
Table 13. Comparison of Gross movement between groups.
Comparison of Gross Movements of the hands between groups
| Stage |
|
Mean ± SD |
df |
F |
p |
| 1st week (pre) |
Experimental |
3.4 ± 1 |
(1,208) |
4.70* |
0.031 |
| Control |
3.1 ± 0.6 |
| 6th week (Post) |
Experimental |
6 ± 0.6 |
(1,208) |
160.19** |
0.000 |
| Control |
4.2 ± 1.4 |
| Adjusted 6th week |
Experimental |
6 ± 0.1 |
(1,207) |
153.41** |
0.000 |
| Control |
4.2 ± 0.1 |
| Adjusted 10th week |
Experimental |
8.8 ± 0.1 |
(1,207) |
534.77** |
0.000 |
| Control |
5.9 ± 0.1 |
Table 14. Comparison of effectiveness of intervention in experimental group over control group on Gross movement (ANCOVA).
Figure 6 Comparison of effectiveness of intervention in experimental group over control group on Gross movement (ANCOVA).
The above table and figure depict that the mean gross movement score increased from 3.36to 8.87 in the experimental group, when compared to 3.12 to 5.90 in the control group. As there is significant variation in the initial pretest scores between the groups, Analysis of covariance (ANCOVA) was applied to 6th and 10th week scores. From the table 4.25 it is clear that the improvement in gross movement function after the intervention is significantly more in the experimental group (p=0.000) [23-25].
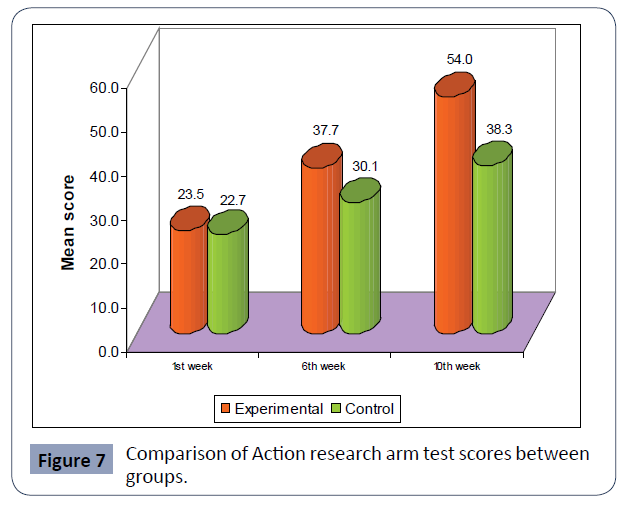
Effect of Modified Constraint Induced Movement Therapy on Fine motor Movements of the hand (Table 15)
| |
Mean |
SD |
N |
F# |
Pair |
Mean Diff. |
LS $ |
| Experimental |
1st week
(T1) |
23.5 |
4.6 |
105 |
4662.31 ** |
T1 & T2 |
14.21** |
Significant |
6th week
(T2) |
37.7 |
4.1 |
105 |
T1 & T3 |
30.44** |
Significant |
| 10th week (T3) |
54.0 |
2.4 |
105 |
T2 & T3 |
16.23** |
Significant |
Table 15. Effect of Modified Constraint Induced Movement Therapy on Action research arm test score.
In experimental group, the fine motor movements of the hand as indicated by the Action Research Arm test Assessment Scores at different stages such as pre intervention (1st week), 6th week and 10th week post intervention are respectively 23.5, 37.7and 54.The F value, (4662.31) shows that the variation in fine motor movements of the hand at different interval time is significant at 0.01 level.
The mean difference between initial and 6th week assessment is 14.21, the pair wise comparison with Bonferroni correction shows that the difference is statistically significant at 0.01 levels.
It means that, through the intervention the score significantly increased at 6th week when compared with 1st week. The increases in score at 10th week in comparison with 1st week (30.44), and in comparison with 6th week (16.23) are also significant at 0.01 levels [26].
Thus it can be concluded fine motor movements of the hand significantly increases with the intervention progressing in experimental group and hence the intervention, modified Constraint Induced Movement therapy is effective in increasing the fine motor movements of the hand (Figure 7) (Table 16).
| |
Experimental |
Control |
T |
p |
| Mean |
Std. Error |
N |
Mean |
Std. Error |
N |
| 1st week |
23.52 |
0.45 |
105 |
22.74 |
0.52 |
105 |
1.14 |
0.255 |
| 6th week |
37.73 |
0.40 |
105 |
30.05 |
0.59 |
105 |
10.85** |
0.000 |
| 10th week |
53.96 |
0.24 |
105 |
38.31 |
0.57 |
105 |
25.42** |
0.000 |
Table 16.Comparison of action research arm test score between groups.
Comparison of Fine motor movements between the groups
Figure 7 Comparison of Action research arm test scores between groups.
In experimental group the Action Research Arm test score increased from 23.52 to 37.73 at 6th week and to 53.96 at the 10th week. From the result it is clear that fine motor movements of the hand increased significantly in the experimental group (p=0.000) [27, 28].
From all the results it can be concluded that even though both the treatment increases motor performance and daily functions of the stroke patients, Modified Constraint Induced Movement Therapy is significantly more effective than the standard therapy offered in the hospital.
Conclusion
From the study it was found that Modified Constraint Induced
Movement Therapy was very effective in improving the motor
performance of the upper extremity, fine motor movements of
the hand such as grasp, grip, pinch and gross movement and daily
functions in stroke patients. Both basic and clinical researches are
critical in improving rehabilitation of stroke patients. Evidence
based practice throughout the path of health care delivery
system offers a new and challenging way for the health care
delivery persons.
REFERENCES
- Albert SJ, Kesselring Neurorehabilitation of Stroke. J Neurol 1-16.
Google Scholar, Crossref
- Amanda C, Fuzaro Carlos T, Guerreiro, Fernanda C, Galetti Renata B V M (2012) Modified constraint-induced movement therapy and modified forced-use therapy for stroke patients are both effective to promote balance and gait improvements Araujo Brazilian. J Phys Ther 16:2 .
Indexed at, Google Scholar, Crossref
- American (2010) Heart Association Heart and Stroke Statistical Update.
Google Scholar, Crossref
- Askim T, Indredavik B, Vangberg T, Håberg A (2009) Motor network changes associated with successful motor skill relearning after acute ischemic stroke: a longitudinal functional magnetic resonance imaging study. Neuro Neur Rep 23:295-304.
Indexed at, Google Scholar, Crossref
- Chan DY, Chan CC, Au DK (2006) Motor relearning programme for stroke patients: a randomized controlled trial. Clin Rehabil 20:191-200.
Indexed at, Google Scholar, Crossref
- Ching-yi Wu, Hsish-ching Chen, I-Husan Chen (2007) Effects of modified constraint induced movement therapy on movement kinematics and daily functions in patients with stroke. Clin Rehab 21:1075-1086.
Indexed at, Google Scholar, Crossref
- Ching-yi Wu ScD, Chia-ling Chen, Wen-chung Tsai, Keh-chung Lin (2007) A Randomized Controlled Trial of Modified Constraint-Induced Movement Therapy for Elderly Stroke Survivors: Changes in Motor Impairment, Daily Functioning, and Quality of Life. Arch Phys Med Rehab 88:273.
Indexed at, Google Scholar, Crossref
- Secondandary Stroke Prevention Continuum (2011). Minneapolis Minn 17:1213-32.
Indexed at, Google Scholar
- Fritz SL, Light KE, Patterson TS (2005) Active finger extension predicts outcomes after constraint-induced movement therapy for individuals with hemiparesis after stroke. 36:1172-1177.
Indexed at, Google Scholar, Crossref
- Grotta J C, Noser E A, Ro T, Boake C, Levin H et al. (2004) Constraint-induced movement therapy. Stroke 35:2699-2701.
Indexed at, Google Scholar, Crossref
- Grotta J (2004) Constraint-induced movement therapy. Stroke 35:2699-2701.
Indexed at, Crossref
- Haynes MP, Phillips D (2012) Modified Constraint Induced Movement Therapy enhanced by a Neuro-Development Treatment-based therapeutic handling protocol: Two case studies. J Pediatr Rehabil Med 5:117-24.
Indexed at, Google Scholar, Crossref
- Kim DG, Cho YW, Hong JH, Song JC, Chung HA (2008) Effect of constraint-induced movement therapy with modified opposition restriction orthosis in chronic hemiparetic patients with stroke 23:239-44.
Indexed at, Google Scholar
- Kim Y, Park J, Ko M, Jang S, Lee, P (2004) Plastic changes of motor network after constraint induced movement therapy. Yonsei Med J 54:241-246.
Indexed at, Google Scholar, Crossref
- Kitago T, Liang J, Huang VS, Hayes S, Simon P et al. (2012) Improvement After Constraint-Induced Movement Therapy: Recovery of Normal Motor Control or Task-Specific Compensation? Neurorehabil Neural Repair 23.
Indexed at, Google Scholar, Crossref
- Kunkel A, Kopp B, Muller G, Villringer K, Villringer A et al. (1999) Constraint-induced movement therapy for motor recovery in chronic stroke patients. Am J Phys Med Rehabil 80:624-628.
Indexed at, Google Scholar, Crossref
- Liepert J, Miltner W H R, Bauder H, Sommer M, Dettmers C et al.(1998) Motor cortex plasticity during constraint-induced movement therapy in stroke patients. Neurosci Lett 250:5-8.
Indexed at, Google Scholar, Crossref
- Lin KC, Wu CY, Wei TH, Grung C, Lee CY, Liu JS (2007) Effects of modified constraint induced movement therapy on reach to grasp movements and functional performance after chronic stroke. A randomized controlled study. Clin Rehabil: 21:1075-1086.
Indexed at, Google Scholar, Crossref
- Mark VW, Taub E, Morris DM (2006) Neuroplasticity and constraint-induced movement therapy. Eura Medicophys 42:269-84.
Indexed at, Google Scholar
- Morris (2006) Constraint-induced movement therapy: characterising the intervention protocol. Eura medicophys 42:257-68.
Indexed at, Google Scholar
- Nijland R, Kwakkel G, Bakers J, van Wegen E (2011) Constraint-induced movement therapy for the upper paretic limb in acute or sub-acute stroke: a systematic review. Int J Stroke 6:425-33.
Indexed at, Google Scholar, Crossref
- Page S (2008) Modified constrain-induced therapy in chronic stroke: results of a single-blinded randomized controlled trial. PT 88:333-340.
Indexed at, Google Scholar, Crossref
- Page S, Sisto S, Levine P, McGrath R (2004) Efficacy of modified constraint induced movement therapy in chronic stroke: A single-blinded randomized controlled trial. Arch Phys Med Rehabil 85:14-18.
Indexed at, Google scholar , Crossref
- Siebers A, Oberg U, Skargren E (2010) The effect of modified constraint-induced movement therapy on spasticity and motor function of the affected arm in patients with chronic stroke. Physiother Can Fall 62:388-396.
Indexed at, Google scholar, Crossref
- , Sirtori V, Corbetta D, Moja L, Gatti R (2009) Constraint-induced movement therapy for upper extremities in stroke patients.Cochrane Database Syst Rev: CD004433.
Indexed at, Google Scholar, Crossref
- Taub E, Crago JE, Uswatte G (1998) Constraint-induced movement therapy: a new approach to treatment in physical medicine. Rehabil Psychol 43:152–170.
Indexed at, Google Scholar, Crossref
- Treger I, Aidinof L, Lehrer H, Kalichman L (2012). Modified constraint-induced movement therapy improved upper limb function in subacute post stroke patients: a small-scale clinical trial. Top Stroke Rehabil 19:287-93.
Indexed at , Google Scholar, Crossref
- Winstein CJ, Miller JP, Blanton S (2003) Methods for a multisite randomized trial to investigate the effect of constraint-induced movement therapy in improving upper extremity function among adults recovering from a cerebrovascular stroke. Neuro Neural Repai 17:137-152.
Indexed at, Google Scholar, Crossref
Citation: Saseendrababu S (2022) The Effect of Modified Constraint Induced Movement Therapy on Motor Performance and Daily Functions in Patients One To Nine Months after Stroke. Health Sci J. Vol. 16 No. 3: 933.