Tanimola Akande1, Adekunle Salaudeen2*, Oluwole Babatunde 3
1MBBS, MSc, FMCPH, Associate Professor, Department of Epidemiology & Community Health, College of Health Sciences, University of Ilorin, Ilorin, Nigeria
2MBBS, FMCPH, FWACP, Lecturer I, Department of Epidemiology & Community Health, College of Health Sciences, University of Ilorin, Ilorin, Nigeria
3MBBS, MPH, Senior Registrar, Department of Epidemiology & Community Health, University of Ilorin Teaching Hospital, Ilorin, Nigeria
- *Corresponding Author:
- Dr. A. G. Salaudeen
Department of Epidemiology and Community Health
University of Ilorin Teaching Hospital
P. O. Box 4465, Ilorin, Nigeria.
E-mail: adekunlesalaudeen@yahoo.com
Tel: +2348036708106
Keywords
Utilization, National, Health, Insurance, Teaching, Hospital, Nigeria
Introduction
The rising cost of health care services as well as the inability of the government health facilities to cope with the people’s demand necessitated the establishment of National Health Insurance Scheme (NHIS). The start of the NHIS dates back to 1962 when the need for health insurance in the provision of health care to Nigerians was first recognized.[1,2] It was fully approved by the Federal Government in 1997, signed to law in 1999 and launched officially on the 6th June 2005. The Scheme is designed to provide comprehensive health care delivery at affordable costs, covering employees of the formal sector, self employed, as well as rural communities, the poor and the vulnerable groups.[1-4]
Prior to the establishment of NHIS, several systems, ranging from free health care purchase, out-of-pocket purchase, retainer ship, in-built health facilities within corporate organizations to private health indemnity insurance have been in vogue. [2] NHIS is a form of managed care that pools regular financial contribution of members and pays a network of providers of health care for defined specific set of health care services, who in turn are accountable for cost containment and improving health outcomes. [2] A contribution entitles the insured person, the spouse and four children under the age of 18 years access to health care. The client will register with NHIS approved Health Maintenance Organization and there after the primary health care provider of his choice from an approved list supplied by Health Maintenance Organization. [1]
The vision of NHIS is to secure universal coverage and access to adequate and affordable health care in order to improve the health status of Nigerians.[3] The role of insurance in health financing is to fold, one, to raise revenue for health care services, and two, to pool these resources so that health risks can be effectively shared among the members of the insurance scheme. [5,6] The main objective of NHIS therefore is to achieve equitable access to health care in Nigeria as an alternative source of funding for a rapidly extending and increasingly costly health care system. [4]
There is dearth of literature on the effect of various health financing options for low and middle income countries. [5,7] More so enrollment in insurance has been found to result in altered behavior, such as utilizing unnecessary medical care, a concept known as ‘moral hazard’. [8] The objective of this study was to compare the pattern of utilization of the services in the Staff Clinic of the University of Ilorin Teaching Hospital two years before and after the commencement of NHIS.
Evidences from countries that have institutionalized national health insurance program indicate positive impact on the health care system. [4,9] In a study in Baltimore USA, health insurance was found to lead to an increase in non urgent utilization of health facilities. [10] Similarly in Taiwan, the utilization of most prenatal and intrapartum care services increased after commencement of NHIS. [11] Also in a related study about public insurance in North Carolina, USA, it was reported that publicly insured children were more likely to have emergency department visit than un-insured children. [12] Same trend was also noticed in Minnesota, USA. [13] Also in Jordan, a middle income country, insurance was found to have a positive effect on the utilization of curative care and significantly increased the number of visits per illness episode. [4]
Generally insurance is found to increase the intensity of utilization and reduce out of pocket spending. [5] However in Nigeria, since the NHIS was established; not much has been carried out to investigate utilization and access to quality health care as a result of the introduction of the Scheme. [14] In Ghana, the utilization of health facilities under insurance cover revealed that Malaria, Respiratory problems and Diarrhea were the commonest illnesses.8 In a survey in Oyo State, Nigeria among health care consumers, 15.8% of respondents were dependants while 84.2% were workers (primary beneficiaries) 4 Pattern of utilization of general practitioners under universal health insurance in Canada indicated that females made more visits than males. [15]
Methodology
This is a cross sectional study using records of four years in University of Ilorin Teaching Hospital Staff Clinic. The University of Ilorin Teaching Hospital Staff Clinic (UITH Staff Clinic) is one of the Federal tertiary institutions in the country and the UITH Staff Clinic is one of the clinics utilized for NHIS in Kwara State. NHIS is currently implemented among federal workers only. NHIS though launched in Nigeria on the 6th June 2005, the full operation in UITH Staff Clinic commenced on the 1st April 2007. Pre-NHIS staff of UITH was refunded for medical expenses.
The primary data used for this study was obtained from hospital record of patients seen in UITHSC from 1st April 2005 to 31st March 2009. The data obtained from 1st April 2005 to 31st March 2007 constituted pre-NHIS implementation data; while information generated from 1st April 2007 to 31st March 2009 were post-NHIS implementation data. In this descriptive study, all patients seen in the clinic who presented with complaints were used. Clients, who came for medical test, follow up and those with incomplete records were excluded from the survey.
Data collected from the register were entered into EPI-Info software using a proforma which contained date, day of the week, socio-demographic information, month, follow-up/new case, diagnosis, and classification of diagnosis (communicable/non communicable). Frequency tables, percentages and mean were generated. Cross tabulation of variables was done. Chi-square test was used to determine the relationship between variables. A p-value of less than 0.05 was considered as statistically significant. Only patients who enrolled in the scheme were used for the information after the commencement of NHIS.
Results
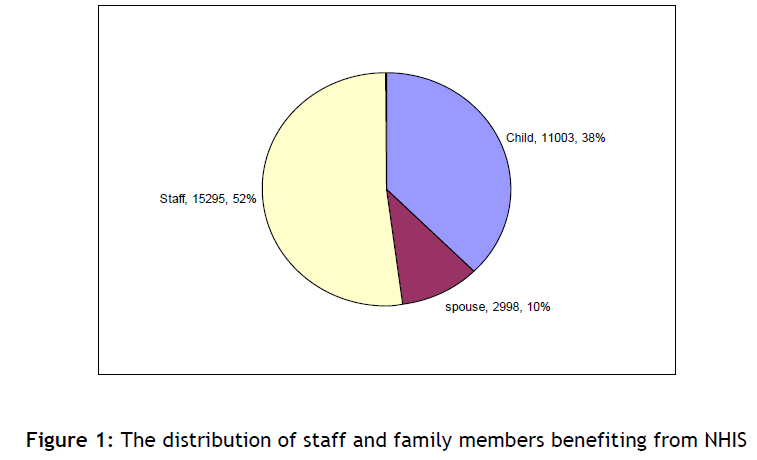
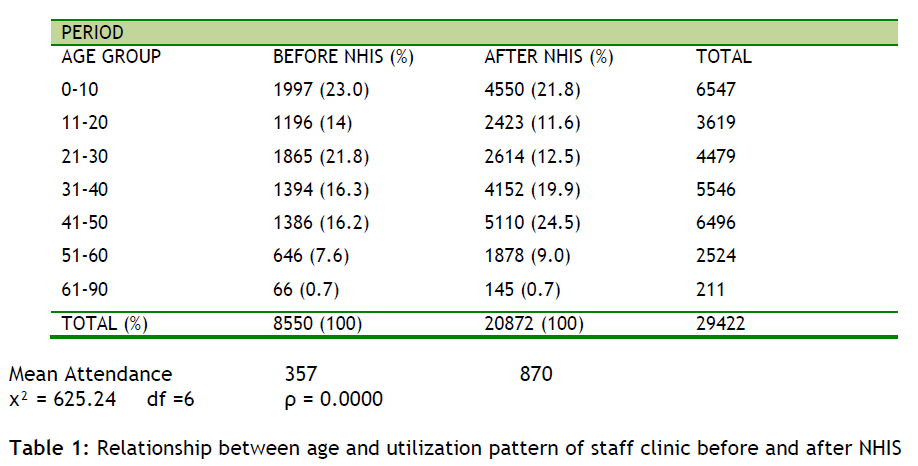
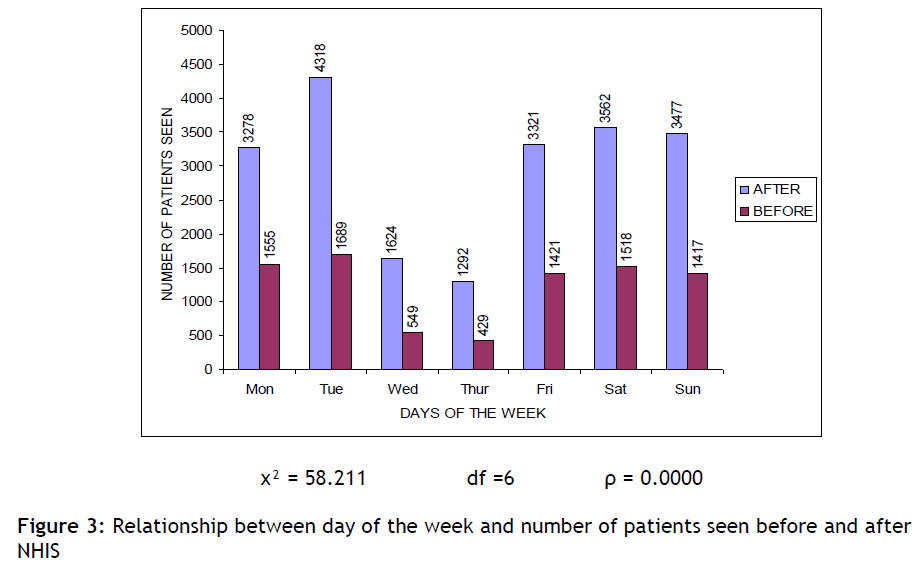
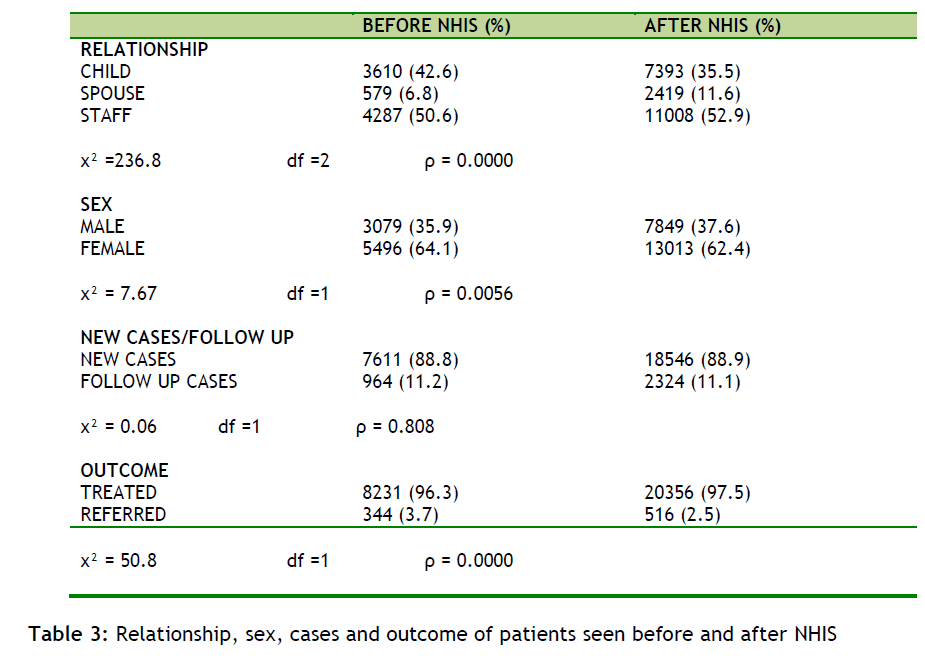
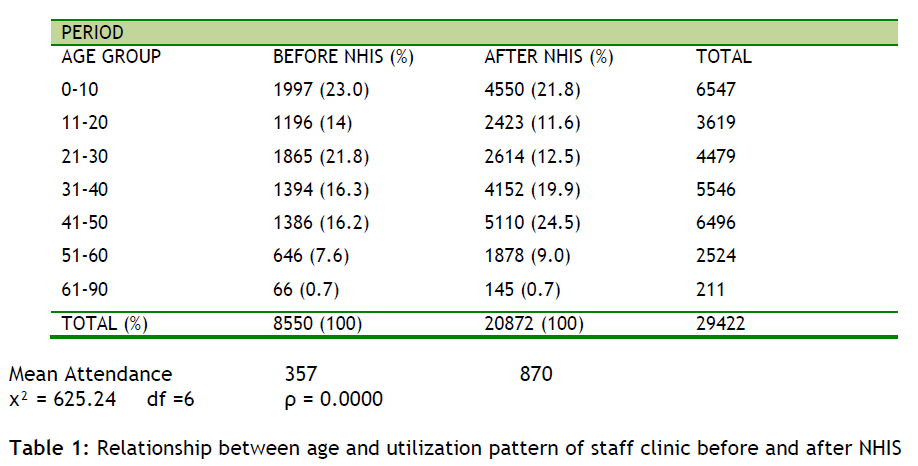
Over the four year period of the study, 29,296 patients utilized the clinic. Of these, 15,295 (52.0%) were staff members while 14,001 (48.0%) were dependants of staff (Figure 1). The dependants consist of children of staff which represented 11,003 (38.0%) and spouses of staff were 2,998 (10.0%). Before NHIS implementation a total of 8,550 patients were seen in the clinic while a total of 20,872 patients were seen after the implementation (Table 1). The mean attendance of patients per month before the implementation of NHIS was 357 patients while after the implementation the mean was 870 patients (Table 1). The age group with the highest frequency of attendance at clinic before the implementation of NHIS was 0-10 years while after the implementation was 41-50 years. The observed difference was statistically significant (p-value = 0.0000).
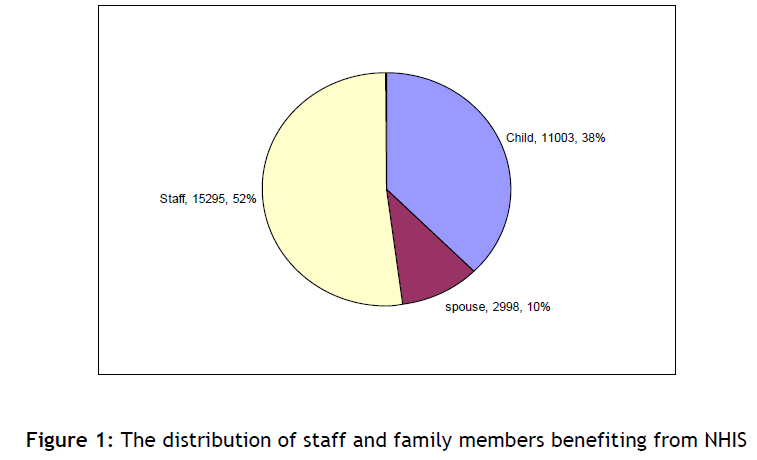
Figure 1: The distribution of staff and family members benefiting from NHIS
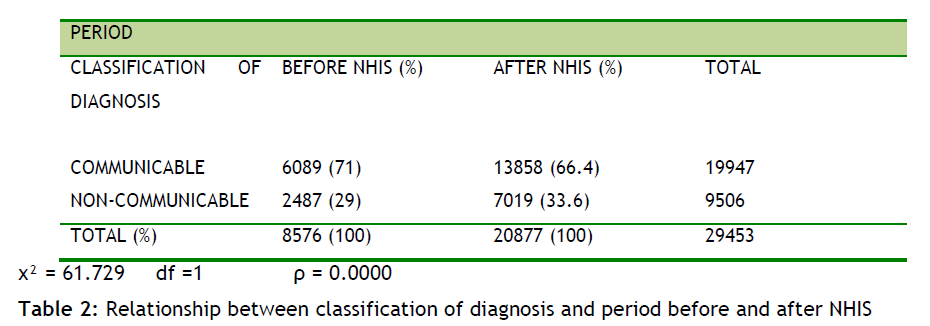
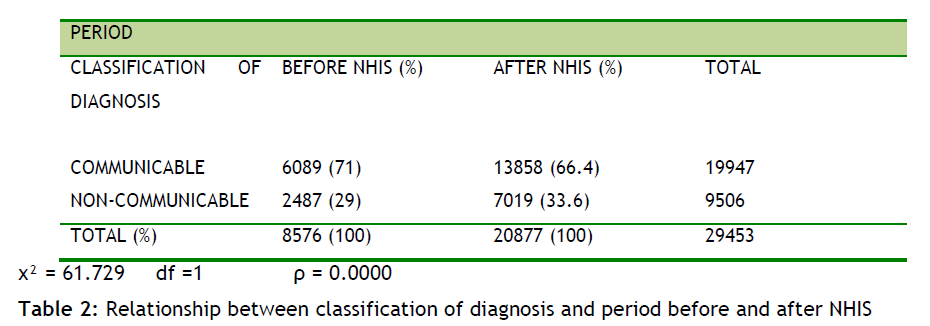
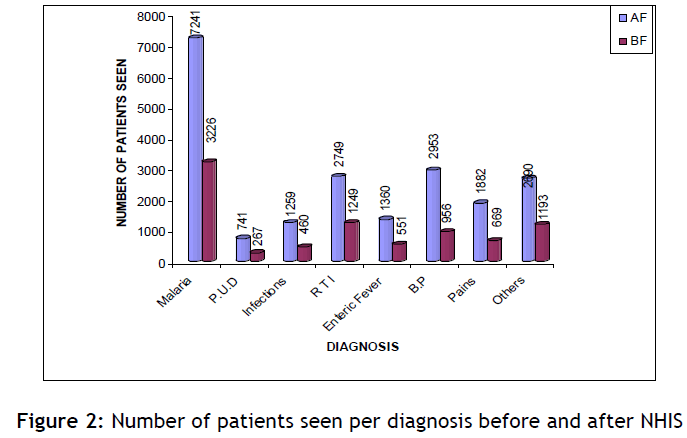
Communicable diseases accounted for 6,089 (71.0%) patients seen before NHIS and 13,858 patients (66.4%) after the commencement of NHIS. Non communicable diseases accounted for 2,487 before and 7,019 cases after the commencement of NHIS. This was statistically significant (p-value = 0.0000). Malaria accounted for the highest number of cases with 7,241 (34.7%) patients after and 3,226 (37.7%) patients before the commencement of NHIS (Figure 2). Highest frequency of patients was seen on Tuesdays both before and after the commencement of NHIS. Before the commencement, a total of 4,318 patients were seen on Tuesday while after the commencement of NHIS, 1,689 patients were seen on Tuesday.
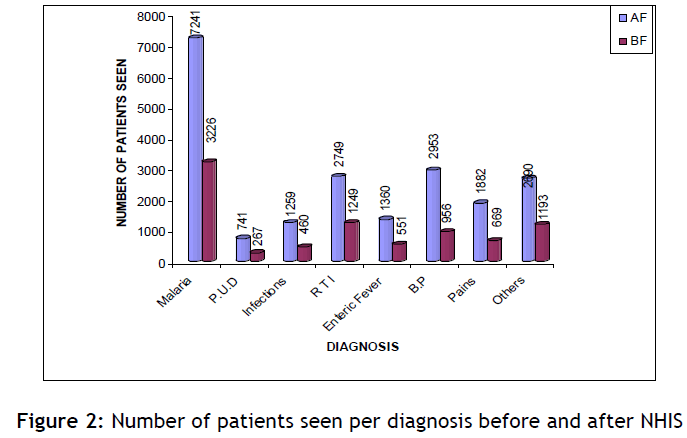
Figure 2: Number of patients seen per diagnosis before and after NHIS
However the lowest frequency of patients was seen on Thursday (Figure 3). Before the commencement of NHIS, the month with the lowest number of patients was April; however after the commencement of NHIS April was the month with the highest frequency of patients (Figure 4).
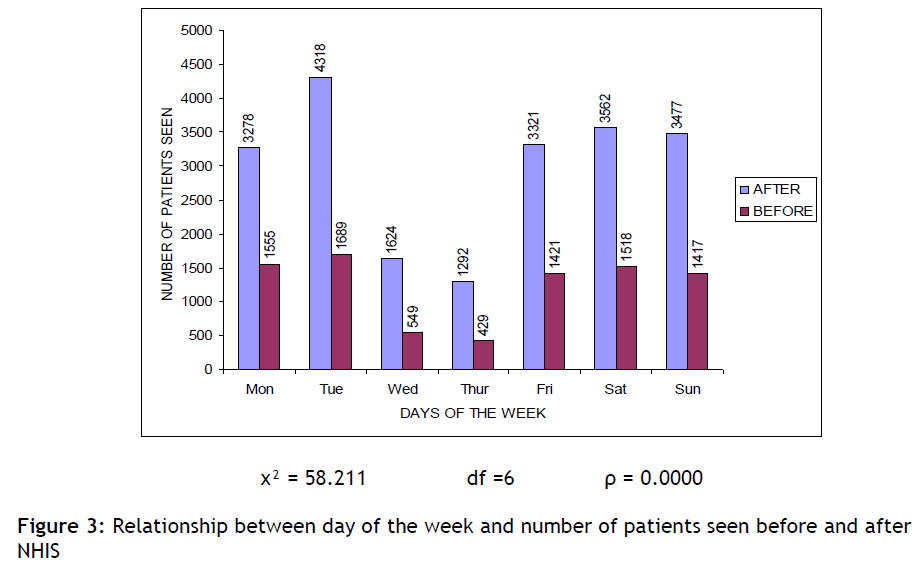
Figure 3: Relationship between day of the week and number of patients seen before and after NHIS

Figure 4: Trend of patients seen per month before and after NHIS
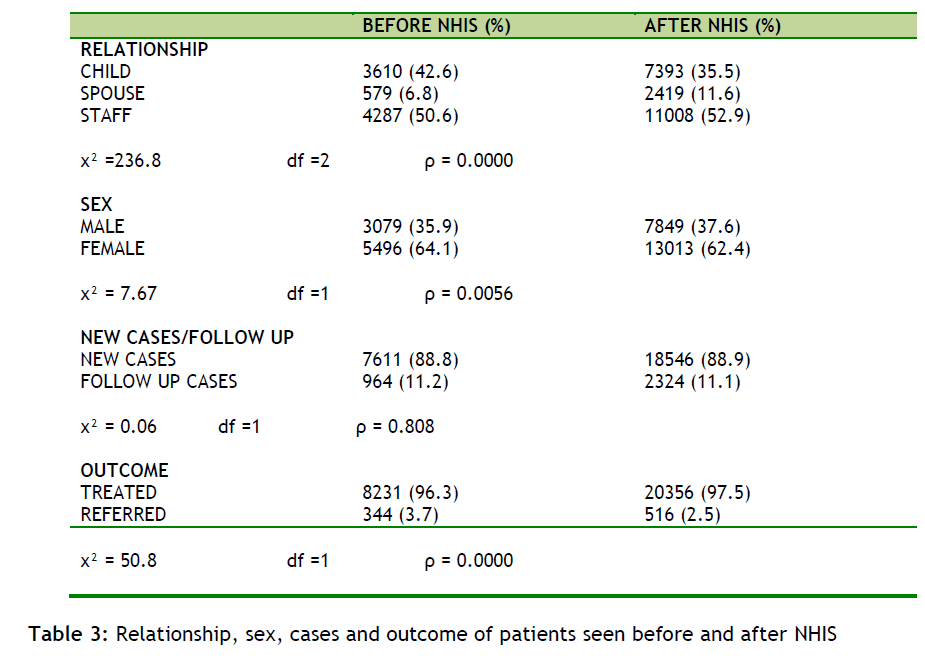
The sex distribution of patients before the NHIS was 3079 males and 5496 females while it was 7849 males and 13013 females after and the difference was statistically significant (p-value 0.0056). There were more new (7611) than follow-up (964) cases before NHIS implementation, similarly 18,546 new cases and 2324 follow-up cases were seen after the commencement (p-value 0.000 Table 3).
Discussion
Primary beneficiaries of the NHIS accounted for 52% while dependants accounted for 48% (spouses-10%, children-38%). This is at variance with the findings from a study done in Oyo State, Nigeria [4] where primary beneficiaries accounted for 84.2% while dependants accounted for 15.8%. The disparity could have been due to the fact that the latter was a field survey while this study was review of past records.
The mean number of attendance before the commencement of NHIS was 357 per month while after the commencement was 870. This is about 144% increase in utilization. This is in line with various studies where utilization of health facilities was found to increase upon the implementation of health insurance. [4,10-13] Specifically in Jordan, [4] it was reported that insurance generally increased the number of visits per illness. However in Ghana, [8] it was reported that enrollment in insurance sometimes results in altered behavior, such as utilizing unnecessary medical care, a concept known as ‘moral hazard’.
In Baltimore USA, [10] the effect of health insurance on utilization pattern of the emergency department was probed into. It was reported that health insurance increased utilization of non-urgent use of the emergency department i.e. patients that are not supposed to be seen at the emergency department increased their utilization of the emergency department as a result of health insurance. In a similar report in Taiwan, [11] the utilization of prenatal and intra-partum care services especially for the more expensive services substantially increased upon implementation of NHIS. For example women who received amniocentesis increased by 246% while women who did German measles test increased by 355%. All these are in line with 144% increase in utilization found in this study. Reports from Carolina USA [12] also revealed that publicly insured children were more likely to have a non urgent emergency department visit than un-insured children.
This study showed that malaria was the commonest diagnosis that was made (35% of all cases before and 38% of all cases after the commencement of NHIS). This was followed by hypertension and respiratory tract infections. This is similar to the finding in Ghana [8] where malaria, respiratory problems and diarrhea were the top three diseases that made respondents seek health care under the NHIS in Ghana.
Day of the week with the highest number of cases seen before and after the NHIS is Tuesday while the month with highest number of cases before and after NHIS was August and April respectively. This is at variance with the temporal variability found in a study on time of the day, day of the week analysis of out-of-hospital cardiac arrest frequency. [17] In this study highest frequency of patients was seen on Saturdays while December accounted for the highest number of patients seen in the year. This variation might be due to the nature of Cardiac arrest compared to outpatients which is the focus of this study. In addition, full clinical work in the hospital is not usually available during the weekend; and Monday is usually used to address some accumulated work in the duty post of hospital workers and as such Tuesday be.
NHIS led to 144% increase in the utilization of health service at staff clinic of the University of Teaching Hospital. More studies need to be done to probe into factors responsible for this increase and to rule out possible of this scheme.
3425
References
- Akande TM, Bello O. National Health Insurance Scheme in Nigeria. MedilorJounal 2002; 7(1): 21-26.
- Katibi IA, Akande AA, Akande TM. Awareness and Attitude of Medical practitioners in Ilorin towards National Health Insurance Scheme. Nigerian Medical Practitioner 2003; 43(2): 33-35.
- Ministry of Health, Federal Republic of Nigeria. National Health Insurance Scheme Handbook. Operational Guidelines on National Health Insurance Scheme 2006.
- Sanusi RA, Awe AT. An Assessment of awareness level of National Health Insurance Scheme among Health Care Consumers in Oyo State, Nigeria. The Social Science 2009; 4(2): 143-148.
- Ekman B. The impact of health insurance on outpatient utilization and expenditure: evidence from one middle-income country using national household survey data. Health Research Policy Systems 2007; 5: 6.
- Folland S, Goodman AC, Stano M. The economics of health and health care. Upper Saddle River, NJ, Pearson Preventive Hall 2004.
- Mills A, Rasheed F, Tollman S. Strengthening Health Systems, Chapter 3. In Disease Priorities In Developing Countries, 2nd Ed by : Jamison DT, Breman JG, Measham AR, Alleyne G, Clacson M, Evans DB et al. Washington DC, Oxford University Press and The World Bank; 2006.
- Sulzbach S, Garshong B, Owusu-Banahene G. Evaluating the effect of the National Health Insurance Act in Ghana : Baseline Report : United States Agency For International Development 2005.
- Collins SR, White C, Kriss JL. Whither employer based health insurance? The current and future role of United States Companies in the provision and financing of health insurance. The Commonwealth Fund Publication Number 1059. 2007. Available at www.commonwealthfund.org.
- Speck SK, Peyrot M, Hsaw CW. Insurance coverage and health care consumers? use of emergency departments: has managed care made a difference? J Hosp Mark Public Relations 2003; 15(1) : 3-18.
- Li-Mei C, Shi WW, Chung-Yi L. The impact of National Health Insurance on the Utilization of National Health Insurance on the utilization of health care services by pregnant women: The Case in Taiwan. Maternal And Child Health Journal 2001; 5(1) :35-42.
- Luo X, Liu G, Frush K, Hey LA. Children?s health insurance status and emergency department utilization in the United States. Paediatrics2003 ; 112(2) : 314-9.
- Kane RL, Keckhafer G, Flood S, Bershadsky B, Siadaty MS. The effect of Evercare on Hospital use. J Am GeriatrSoc 2002; 51(10) : 1427-34.
- Ibiwoye A, Adeleke IA. Does Nationaln Health Insurance Promote Access to Quality Health Care? Evidence from Nigeria. The Geneva Papers 2008;33(2) : 219-233.
- Segovia J, Edwards AC, Li N, Batlett RF. Patterns of utilization of general practitioners under Universal Health Insurance. Abstr Book Assoc Health Serv Res Meet. 1999 ; 223.
- National Population Commission, Federal Republic of Nigeria. Federal Republic of Nigeria official Gazette of the 2006 National Population and Housing Census. The Federal Government Printer Lagos, Nigeria FGP 71/5200712, 500(OL24) 2007; 94(24) : 175-198.
- Coptermedic. Time of the day, day of the week analysis of out-of-hospital arrest (OCHA) frequency and viability. Coptermedic 2009. Available at http:/acutecareinc.wordpress.com. Last accessed 13th January 2010.