Keywords
Intracerebral haemorrhage; Stroke population; Acute neurological symptoms; Neuroimaging; Qatar
Abbreviations
BG: Basal Ganglia; BS: Brain Stem; FFE: Far East; IS: Ischemic Stroke; ICH: Intracerebral Haemorrhage; MENA: Middle East and North African Arabic population; SE: South Indian
Introduction
Intracerebral hemorrhage (ICH) accounts for 10% to 30% of all strokes [1]. However, the clinical outcome is worse than ischemic stroke and 50% mortality rate at 30 days follow up [2,3].
The etiologies of ICH vary based on the age group. The most common risk factors in elderly are HTN, cerebral amyloid angiopathy and anticoagulation related ICH like warfarin [4-6]. Whereas in young, secondary causes need to be ruled out like AVM, cavernoma or cerebral aneurysm or coagulopathy [7,8].
The unique feature of Qatar state is the multi-culture demography of population which might makes the etiology and mechanism of ICH different from the current studies published in the western region. Eighty four percent of the population is male due to a large majority of expatriate blue color laborers and 82% of the population being less than 65 years old for the same reason.
Our group recently reported on the risk factors and clinical characteristics of stroke in Qatar [9]. However, to date there is no report on the prevalence and incidence of ICH in the state of Qatar. We did propose high incidence of ICH in the state of Qatar due to high rate of south east and Far East ethnicity in comparison to the western population.
Out study’s aim is to evaluate the rate of ICH among stroke population in Qatar state for the period from 1st December 2013 to 11th May 2017 and main risk factors and etiology seen based on the age and ethnicity of the population.
Research Methodology
Our stroke data base is based on prospective data collection of patients presented with acute neurological symptoms and classified to have either TIA, mimics, ischemic stroke or ICH from 1st December 2013 to 11th May 2017. Patients with the diagnosis of ICH based on head CT imaging and clinical presentation will be included in our study’s sample. The local ethics committee has approved the stroke data base in our center.
Data collection
The baseline medical history will include age, sex, ethnicity, nationality, marital status, smoking status, alcohol intake, medical comorbidities (including a history of hypertension, diabetes, dyslipidemia, coronary artery disease and chronic kidney disease), and all current prescription and over-thecounter medications. The cerebrovascular event type (stroke vs. TIA; ischemic vs. hemorrhagic) will be documented using the TOAST criteria and the date of hemorrhagic stroke will be recorded. The detailed clinical presentations and neuroimaging findings were recorded. The Etiology of ICH was assumed based on age, risk factors and neuroimaging findings. The location of ICH was classified as the following: lobar, subcortical, basal ganglia, thalamus, brainstem, cerebellum and intraventricular hemorrhage. The etiology of ICH was defined as: HTN, CAA, vascular abnormalities (AVM etc.) other etiology like drug related, vasculitis etc., based on clinical presentation risk factors and neuroimaging, CT/CTA of the neck and brain, MRI/MRA of the brain and neck vessels and cerebral angiogram in selected cases.
Neuroimaging (Head CT, MRI of the brain, CTA and cerebral angiogram) findings were recorded.
Statistical method
Baseline characteristics of ICH populations were calculated using unvaried analysis (χ2 test, ANOVA and student t-test). Then multiple logistic regression analysis was performed to define predictors of ICH. SPSS 23 were used and p value of 0.05 was considered significant.
Results
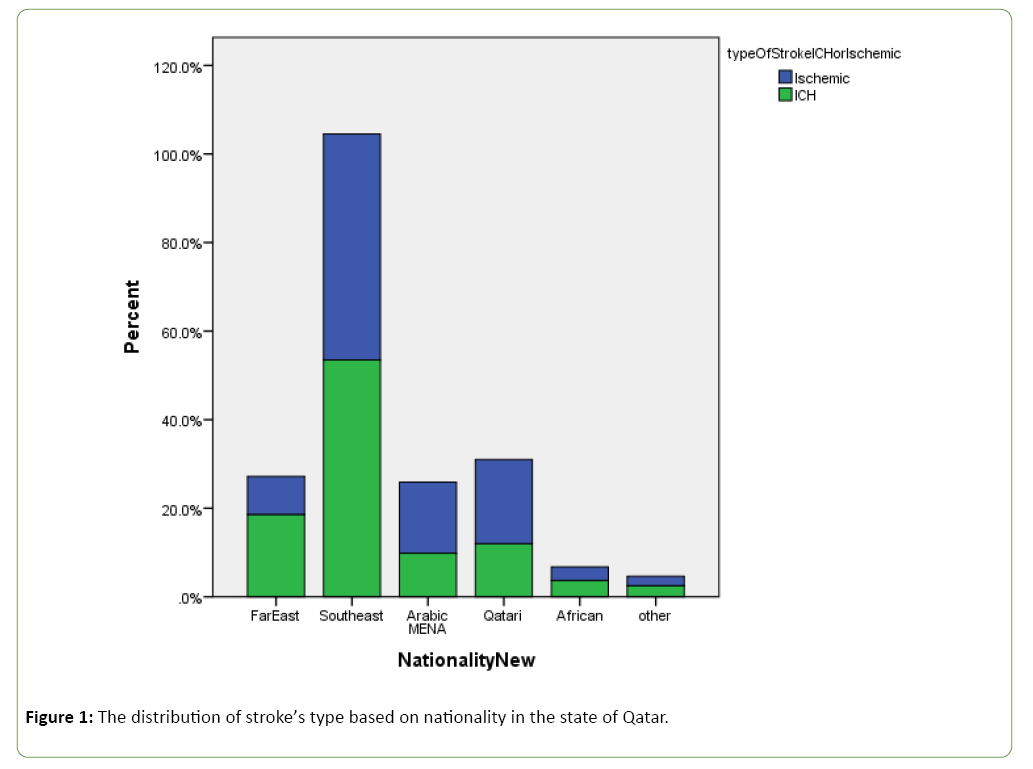
Baseline characteristics were summarized in Table 1. The rate of ICH is 20.5% (518 ICH/25:25 total strokes). In our population, patients with ICH is slightly younger with a mean age of 51.72 ± 13.1 than ones with ischemic stroke 56.12 ± 13.38 (p value 0.68) and more seen in male than female ratio in both ICH and ischemic stroke (IS). (5:1, M=432 (83.3%), F=86 (16.6%). In addition, patient with ICH do worse than ones with IS (3 months mRS >2, 143/302 (47.4%) in ICH versus 678/1896 (35.8%) p<0.001. Based on the population distribution of races, ICH is more common in the South Asian [S.A] 277/518 (53.3)% followed by Filipino and Far East [FFE] 96/513 (18.5%), then Qatari and Arabic population 62/518 (12%) and 51/518 (9.8%), respectively, (p<0.001) (Figure 1). The main risk factor for ICH in our populations is HTN 330/518 (64%) followed by DM 135/518 (26.3%) [10].
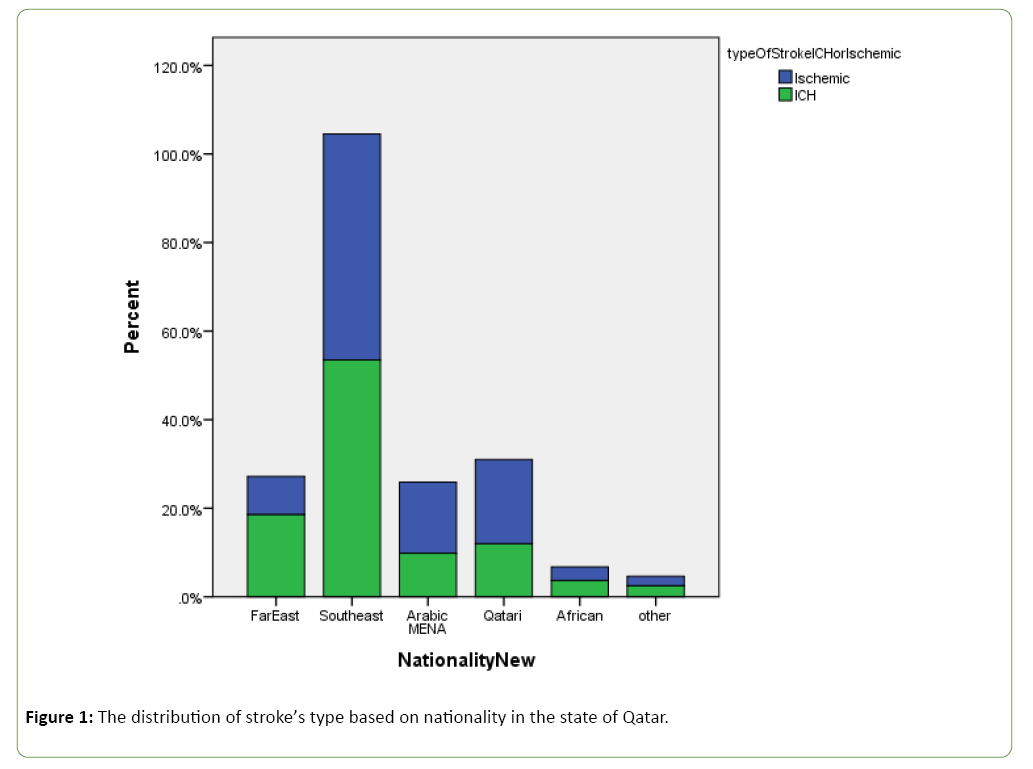
Figure 1: The distribution of stroke’s type based on nationality in the state of Qatar.
Table 1: Demographic data.
| Variables |
ICH (n=518) |
IS(n=2007) |
p-value |
| Age (mean ± SD) |
51.72 ± 13.1 |
56.12 ± 13.38 |
0.688 |
| Sex (Male/Female) |
05:01 |
4.5:1 |
0.478 |
| M=432 (83.3%) |
M=1646 (82%) |
| F=86 (16.6%) |
F=361 (17.9%) |
| Race n (%) |
| Filipino & Far East (FFE) |
96 (18.5%) |
174 (8.7%) |
<0.001 |
| South Asian (S.A.) |
277 (53.5%) |
1024 (51%) |
<0.001 |
| Arab (MENA)* |
51 (9.8%) |
322 (16%) |
<0.001 |
| Qatari |
62 (12%) |
382 (19%) |
<0.001 |
| African |
19 (3.7%) |
62 (3.1%) |
<0.001 |
| Others |
13 (2.5%) |
43 (2.1%) |
<0.001 |
| Risk Factors n (%) |
| DM |
135 (26.3) |
939 (46.8) |
<0.001 |
| HTN |
330 (64) |
1156 (57.9) |
0.14 |
| Tobacco consumption |
72 (17.2) |
432 (22.2) |
0.025 |
| ETOH |
23 (4.4) |
13 (0.6} |
<0.001 |
| SBP (mean ± SD) |
175.78 ± 36.94 |
156.68 ± 30.73 |
<0.001 |
| DBP (mean ± SD) |
100.92 ± 23.56 |
88.05 ± 19.08 |
<0.001 |
| Baseline RBS (mean ±SD) |
8.64 ± 3.78 |
9.84 ± 5.34 |
<0.001 |
| NIHSS (mean ± SD) |
12.09 ± 7.85 |
5.72 ± 5.19 |
<0.001 |
| GCS (mean ± SD) |
11.62 ± 4.49 |
14.56 ± 1.67 |
<0.001 |
| Heart rate (mean ± SD) |
82.6 ± 16.18 |
82.64 ± 15.46 |
0.426 |
| HgA1c (mean ± SD) |
6.42 ± 1.67 |
7.1 ± 2.9 |
<0.001 |
| Poor Long-term outcome (90 days mRS >2) |
143/302 (47.4%) |
678/1896 (35.8 %) |
<0.001 |
| BMI |
27 ± 4.82 |
24.14 ± 8.39 |
<0.001 |
*MENA: Middle East North Africa
In the multiple logistic regression analysis, the main predictors of ICH is the FFE ethnicity (OR: 2.297, CI: 1.77-2.97, p-Value: 0.00), HTN (OR: 1.85 CI: 1.46-2.36, p<0.001, NIHSS (OR: 1.15 CI: 1.13-1.17, p<0.001) and age (OR: 0.9 for each year of age, CI: 0.96-0.98, p<0.001) (Table 2).
Table 2: Multiple logistic regression analysis (predictors of ICH).
| Variables |
Adj OR |
CI 95 % |
p-value |
| Far East vs. Rest |
1.85 |
1.36-2.52 |
<0.001 |
| Qatari |
0.571 |
0.400-0.816 |
<0.002 |
| Arabic |
0.595 |
0.414-0.854 |
<0.001 |
| South Indian |
0.914 |
0.728-1.148 |
<0.001 |
| African |
1.267 |
0.696-2.308 |
<0.001 |
| Hypertension |
1.857 |
1.46-2.361 |
<0.001 |
| NIHSS |
1.15 |
1.134-1.17 |
<0.001 |
| Age |
0.9 |
0.966-0.983 |
<0.001 |
Based on ethnicity, the SA and FFE patients with ICH are younger than the Arabic and Qatari ones (S.E.: 49.65 ± 10.7, FFE: 51.79 ± 11.35 versus Arabic: 58.98 ± 15.18 and Qatari: 66.26 ± 14.88 (p<0.001)) Hypertension remains the main risk factor for ICH across all ethnicities followed by DM and smoking.
The basal ganglia (BG) is the most common location of ICH based on ethnicity followed by lobar one then thalamic then cerebellar and brain stem ICH (Table 3). However, in African the BG and lobar ICH are equally distributed.
Table 3: Unvaried analysis based on race.
| Variables |
Qatari (N=62) |
Arabic (N=51) |
S.A.* (N=201) |
Filipino and Far east (N=96) |
African (N=19) |
Other (N=13) |
p value |
| Age (mean ± SD) |
66.26 ± 14.88 |
58.98 ± 15.18 |
49.65 ± 10.7 |
50.76 ± 9.93 |
51.79 ± 11.35 |
48.77 ± 10.37 |
0 |
| Sex (M/F) |
1.6:1 |
2.7:1 |
3.5:1 |
04:01 |
1.3:1 |
03:01 |
0 |
| Risk Factors: n (%) |
| Diabetes |
34 (54.3) |
26 (51%) |
54 (19.7%) |
14 (14.7%) |
6 (31%) |
1 (7.7%) |
0 |
| Hypertension |
52 (83.9%) |
34 (66.7%) |
163 (59.3% |
63 (65.6%) |
10 (52.6%) |
8 (61.5%) |
0 |
| Antiplatelets |
13 (22.4%) |
9 (19%) |
9 (4.2%) |
1 (1.1%) |
3 (18.8%) |
1 14.3%) |
0.007 |
| Statin |
10 (17.2%) |
6 (13%) |
17 (8%) |
4 (4.6%) |
0 (0%) |
0 (0%) |
0 |
| Oral anticoagulant |
7 (12.1%) |
4 (8.5%) |
2 (.9%) |
2 (2.3%) |
0 (0%) |
1 (14.3%) |
0.045 |
| Smoking |
6 (10.3%) |
8 (18.2%) |
45 ( 21.4%) |
10 (11.9%) |
2 (14.3%) |
1 (12.5%) |
0.002 |
| ETOH |
3 (5.2%) |
0 (0%) |
9 (4.3%) |
9 (10.7%) |
1 (7.1%) |
1 (12.5%) |
0.242 |
| SBP (mean +/- SD) |
171 ± 30.53 |
166.26 ± 34.1 |
179.59 ± 39.4 |
178.8 ± 36.73 |
156.47 ± 37.1 |
162.62 ± 38.94 |
0.35 |
| DBP |
88.93 ± 17.98 |
91.98 ± 21.61 |
103.9 ± 23.78 |
105.63 ± 24.7 |
91.24 ± 19.3 |
95.23 ± 21.68 |
0 |
| NIHSS |
12.19 ± 7.25 |
10.92 ± 7.92 |
11.92 ± 8.2 |
12.58 ± 7.85 |
10.37 ± 8.59 |
11.54 ± 7.74 |
0.705 |
| GCS |
11.22 ± 4.5 |
12.48 ± 4.47 |
11.68 ± 4.4 |
11.57 ± 4.75 |
11.16 ± 4.6 |
11.17 ± 4.98 |
0.883 |
| Neuroimaging |
| CMB |
1 (100%) |
2 (18.2) |
31 (44%) |
9 (50%) |
2 (33%) |
0 (0%) |
0.263 |
| Ischemic Stroke |
6{66.6%} |
4{36.4%} |
50{66.6%} |
14 (12) |
5{71.4%} |
1{100%} |
0.363 |
| WMD |
2 (100%) |
4 (36.4%) |
29 (43.3%) |
9 (50%) |
3 (50%) |
0 (0%} |
0.41 |
| Pontine rarefication |
0 (0%} |
1 (9.1%) |
11 (16.7%) |
3 (16.7%) |
1 (16.7%) |
0 (0%) |
0.949 |
| IVE |
6 (75%) |
4 (26.7%) |
76 (42%) |
17 (31.5%) |
6 (66.7%) |
4 (40%) |
0.084 |
| Cause of ICH |
| HTN |
80.30% |
80% |
89% |
91% |
83.30% |
77.80% |
0.004 |
| CAA |
6.60% |
0% |
1% |
1.10% |
0% |
11.10% |
0.004 |
| CVT |
0% |
13.30% |
2.60% |
0% |
8.30% |
0% |
0.004 |
| AVM |
4.90% |
0% |
2.90% |
5.40% |
8.30% |
0% |
0.004 |
| Drug related |
8.20% |
0% |
1.60% |
2.20% |
0% |
11.10% |
0.004 |
| Other cause |
0% |
6.70% |
2.20% |
0% |
0& |
0% |
0.004 |
| Location of ICH |
| Lobar |
18 (29%) |
13 (25.5%) |
55 (19.9%) |
13 (13.5%) |
7 (36.8%) |
5 (28.5%) |
0.385 |
| BG |
27 (43.5%) |
24 (47.1%) |
137 (49.5% |
56 (58.3%) |
7 (36.8%) |
6 (46.2%) |
0.385 |
| IVH |
2 (3.2%) |
3 (5.9%) |
8 (2.9%) |
1 (1%) |
0 (0%) |
0 (0%) |
0.385 |
| Cerebellar |
3 (4.8%) |
2 (3.9%) |
16 (5.8%) |
6 (6.3%) |
2 (10.5%) |
0 (0%) |
0.385 |
| BS |
4 (6.5%) |
2 (3.9%) |
28 (10.1%) |
5 (5.2%) |
2 (10.5%) |
0 (0%) |
0.385 |
| Thalamic |
8 (12.9%) |
7 (13.7%) |
33 (11.9%) |
15 (15.6%) |
1 (5.3%) |
2 (15.4%) |
0.385 |
The etiology of ICH based on ethnicity, HTN related remains the main cause of ICH in all ethnic groups (Table 3). Few cases of cerebral amyloid angiopathy (CAA) were reported mainly in the Qatari population as an etiology of ICH (6.6 %).
Discussion
Our study is the first to publish on the rate of ICH in the state of Qatar over period of time. It is quite a bit alarming given the high rate of ICH in some races like the FFE and S.E.A ones mostly related to HTN which is preventable. The other alarming fact is that ICH is quite common in young age in our sample group and this could be explained by the high rate of untreated hypertension.
Several previous studies evaluated the incidence, clinical outcome and mortality rates in different ethnic and age populations [11-15] and reported in a systematic review performed by Van Asch et al. [16] In their systematic review, they assessed the incidence, case fatality, and functional outcome of intracerebral haemorhage in relation to age, sex, ethnic origin, and time period in studies published since 1980, In the meta-analysis, they estimated the incidence of ICH to be 24•6 per 100000 person-years.
In the meta-analysis by Van Asch et al. the incidence rate per 100 000 person-year was ≤ 1.9 in the young group <45 years old. The rate was 136.9 for the age group 75 to 83 years old and 196 for >84 years old. Our study shows the incidence rate in the Qatari population over 70 years age to be 477.3 and 14.9 for the “20 to 49 years”. These very high rates, when compared to reports from elsewhere, may be explained by the high rate of uncontrolled risk factors, especially HT and DM in our population. Rates of ICH are varied between various ethnicities in the meta-analysis. It was 24.2 per 100 000 person-year in Caucasians, 22.9 in Africans, 19.6 in Hispanic, and 51.8 in Asian people in their meta-analysis. They concluded that there was not a substantial decrease in the incidence of ICH between January 1980, and November 2008. The incidence of ICH was higher in men compared with women, especially in Japanese studies; a two times higher rate of ICH in Asian people compared with other ethnic groups; and an increasing incidence of ICH with increasing age. Our study’s finding where ICH is more common in male than female needs to be taken with caution as our study’s sample is squid due to the high number of expatriate males in Qatar population.
Palm et al. and his group reported the incidence of ICH in his population stroke registry in the Ludwigshafen Stroke Study. [10] In his study the crude and age-adjusted incidence rates per 100,000 for first ever primary ICH were 18.7 (95% CI 15.9-21.9) and 11.9 (95% CI 10.2-14.0), respectively, and remained stable over time. The case-fatality rates for first ever primary ICH were 27.0, 34.9 and 44.1% at days 28, 90 and 365, respectively. In his study, the incidence of ICH is in the lower range of those reported from other registries and remained stable over the observation period. He proposes that higher treatment rates for hypertension might partly account for this finding. Our study’s finding revealed higher rate of ICH in our multi-ethnic population than Palm ’ study. This could be explained by the high rate of untreated hypertension in our population. However, our study ’ s sample most likely is a skewed population as it was predominantly young expatriate workers from different ethnicities. The incidence rate of ICH in the SE ethnic population may be higher in India than Qatar since our SE population in Qatar are younger. For that reason, the incidence rate of ICH aside from non-Qatari population in our study’s sample has to be taken with caution. Further study needed in our center to define if the rate of ICH will drop once stringent blood pressure control measurement is taking place in our center. Qiu et al. did study the incidence of recurrent ICHs in multiple ethic south Asian in Singapore and did identify the associated risk factors as well as pattern of ICH recurrence [17].
He did find the average annual incidence rate of primary ICH recurrence in Singapore is 1.1%, and is associated with previous ischemic stroke and lobar location of index ICH. The common pattern of recurrence ICH in his study is ganglionicganglionic (44.1%), followed by lobar-lobar (17.6%). Our study revealed a similar finding where most of the ICH cases in the far east and southeast populations are basal ganglia ICH which is an indicative of being HTN related ICH. However, in our study we could not comment on the recurrence rate due to difficulty in doing follow up and the design of our study of being cross section not prospective one.
Our study’s limitation, first it is retrospective prospectively collecting data so it is prone to selection bias. However, we tried in our analysis to adjust to common confounders. Second, our study sample is from one major tertiary hospital in the state of Qatar. Few cases could be seen and evaluated in another secondary care hospitals which we do not have an access to, But Presumably this is represented of all Qatar since Hamad hospital is the only tertiary hospital in Qatar which treat the majority of patients with ICH. Third, we do not have a follow up outcome in our study due to the difficulty of doing that since some patient ended up leaving the state of Qatar to their home country once they finish rehabilitation.
Conclusion
In conclusion, ICH in the state of Qatar is more seen in young and south Asian population and have worse outcome than ischemic stroke ones. This could be explained by the unique multiple ethnicities ’ population in Qatar. Further prospective studies are needed to understand the mechanism of ICH and its recurrence rate.
26403
References
- Broderick JP, Adams Jr HP, Barsan W, Feinberg W, Feldmann E, et al. (1999) Guidelines for the management of spontaneous intracerebral hemorrhage: a statement for healthcare professionals from a special writing group of the Stroke Council, American Heart Association. Stroke 30: 905-915.
- Broderick JP, Brott T, Tomsick T, Huster G, Miller R (1992) The risk of subarachnoid and intracerebral hemorrhages in blacks as compared with whites. New England Journal of Medicine 326: 733-736.
- Hansen BM, Nilsson OG, Anderson H, Norrving B, Säveland H, et al. (2013) Long term (13 years) prognosis after primary intracerebral haemorrhage: a prospective population based study of long term mortality, prognostic factors and causes of death. J Neurol Neurosurg Psychiatry 84:1150-1155.
- Woo D, Sauerbeck LR, Kissela BM, Khoury JC, Szaflarski JP, et al. (2002) Genetic and environmental risk factors for intracerebral hemorrhage. Stroke 33: 1190-1196.
- Anderson CS, Chakera TM, Stewart-Wynne EG, Jamrozik KD (1994) Spectrum of primary intracerebral haemorrhage in Perth, Western Australia, 1989-90: incidence and outcome. J Neurol Neurosurg Psychiatry 57: 936-940.
- Itoh Y, Yamada M, Hayakawa M, Otomo E, Miyatake T (1993) Cerebral amyloid angiopathy: a significant cause of cerebellar as well as lobar cerebral hemorrhage in the elderly. J Neurol Sci 116: 135-141.
- Schmidt LB, Goertz S, Wohlfahrt J, Melbye M, Munch TN (2016) Recurrent intracerebral hemorrhage: associations with comorbidities and medicine with antithrombotic effects. PloS one 11: e0166223.
- Rutten-Jacobs LC, Maaijwee NA, Arntz RM, Schoonderwaldt HC, Dorresteijn LD, et al. (2014) Clinical characteristics and outcome of intracerebral hemorrhage in young adults. J Neurol 261: 2143-2149.
- Akhtar N, Kamran S, Singh R, Cameron P, D’Souza A, et al. (2015) Beneficial effects of implementing stroke protocols require establishment of a geographically distinct unit. Stroke 46: 3494-3501.
- Palm F, Henschke N, Wolf J, Zimmer K, Safer A, et al. (2013) Intracerebral haemorrhage in a population-based stroke registry (LuSSt): incidence, aetiology, functional outcome and mortality. J Neurol 260: 2541-2550.
- Islam MS, Anderson CS, Hankey GJ, Hardie K, Carter K, et al. (2008) Trends in incidence and outcome of stroke in Perth, Western Australia during 1989 to 2001: the Perth Community Stroke Study. Stroke 39: 776-782.
- Lovelock CE, Molyneux AJ, Rothwell PM (2007) Change in incidence and aetiology of intracerebral haemorrhage in Oxfordshire, UK, between 1981 and 2006: a population-based study. Lancet Neurol 6: 487-493.
- Marini C, Totaro R, De Santis F, Ciancarelli I, Baldassarre M, et al. (2001) Stroke in young adults in the community-based L’Aquila registry: incidence and prognosis. Stroke 32: 52-56.
- Labovitz DL, Halim A, Boden-Albala B, Hauser WA, Sacco RL (2005) The incidence of deep and lobar intracerebral hemorrhage in whites, blacks, and Hispanics. Neurology 65: 518-522.
- Lavados PM, Sacks C, Prina L, Escobar A, Tossi C, et al. (2005) Incidence, 30-day case-fatality rate, and prognosis of stroke in Iquique, Chile: A 2-year community-based prospective study (PISCIS project). Lancet 365: 2206-2215.
- van Asch CJ, Luitse MJ, Rinkel GJ, Van der Tweel I, Algra A, et al. (2010) Incidence, case fatality, and functional outcome of intracerebral haemorrhage over time, according to age, sex, and ethnic origin: A systematic review and meta-analysis. Lancet Neurol 9: 167-176.
- Qiu L, Upadhyaya T, See AA, Ng YP, King NK (2017) Incidence of recurrent intracerebral hemorrhages in a multiethnic south asian population. J Stroke Cerebrovasc Dis 26: 666-672.