Clare Richardson, Gennaya Mattison, James Roring, Adrienne Workman and Subhas Gupta*
Department of Plastic Surgery, Loma Linda University Medical Center, California, USA
*Corresponding Author:
Dr. Subhas Gupta
Department of Plastic Surgery
Loma Linda University 11175 Campus Street
CP 21126, Loma Linda, California, USA
Tel: (909) 558-8085
Fax: (909) 558-4175
E-mail: sgupta@llu.edu
Received Date: February 09, 2015; Accepted Date: February 08, 2016; Published Date: February 19, 2016
Citation: Richardson C, Mattison G, Roring J, et al. The Optimal Duration of Antibiotic Prophylaxis in Plastic Surgery: A Meta-Analysis of 32 Publications Running Head: Optimal Duration of Antibiotics in Plastic Surgery. Health Sci J. 2016, 10:2.
Keywords
Antibiotic prophylaxis; Antibiotic duration; Surgical site infection; Wound infection; Plastic surgery; Meta-analysis
Introduction
Surgical site infections (SSIs) are one of the largest contributors to complications following surgical procedures. In addition, SSIs are the second most common type of nosocomial infections, with reported rates ranging from 1% to 30% depending on the procedure [1,2]. Patients who contract SSIs are estimated to have re-admission rates up to five times that of patients without SSIs and mortality rates up to twice as high [1,3]. SSIs also impact multiple economic factors including length of stay, readmission rates, and use of both hospital and ancillary services, collectively leading to an overall increase in healthcare related costs [4]. In addition to affecting healthcare expenditures, SSIs may also directly affect physician reimbursement. SSIs are designated as a never event by the Center for Medicare and Medicaid Services, meaning that physicians may not be compensated for procedures in which patients subsequently develop post-operative infections [5,6].
Antibiotic prophylaxis to combat surgical site infection was instituted in the 1960’s along with the initiation of a wound classification system by the National Research Council [7]. Since its inauguration, extensive clinical research has been carried out in order to develop standards and guidelines for antibiotic type and duration depending on the procedure being performed. Today, guidelines for the prophylactic use of antibiotics are implemented internationally including within the USA, UK, Canada, Europe, and Australia [8-10]. They exist in multiple surgical fields such as general surgery, colorectal surgery, and obstetrics [2,6,11-13]. Some surgical fields, such as cardiothoracic surgery, do not yet have established guidelines in place for antibiotic prophylaxis, but have multiple studies with suggestions given for evidence-based antibiotic prophylaxis use [14,15]. Additionally, outside of the surgical fields, antibiotic prophylaxis has been a topic of research as well. The American Heart Association produced well-known recommendations for the prevention of endocarditis with dental procedures [16] and guidelines have even been developed for prevention of infections following combat related injuries [17].
Despite these strides, within some subspecialties antibiotic prophylaxis has been less extensively studied and the ideal durations and types are often not specified. A striking example is the field of plastic surgery. Very few studies have been carried out looking at optimal use of antibiotic prophylaxis and practice is largely dependent on physician preference and individual knowledge [7]. The objectives for this study were to seek out and compare studies on the use of antibiotic prophylaxis in the field of plastic surgery. In doing so, we hoped to determine the optimal duration of antibiotic prophylaxis.
Methods
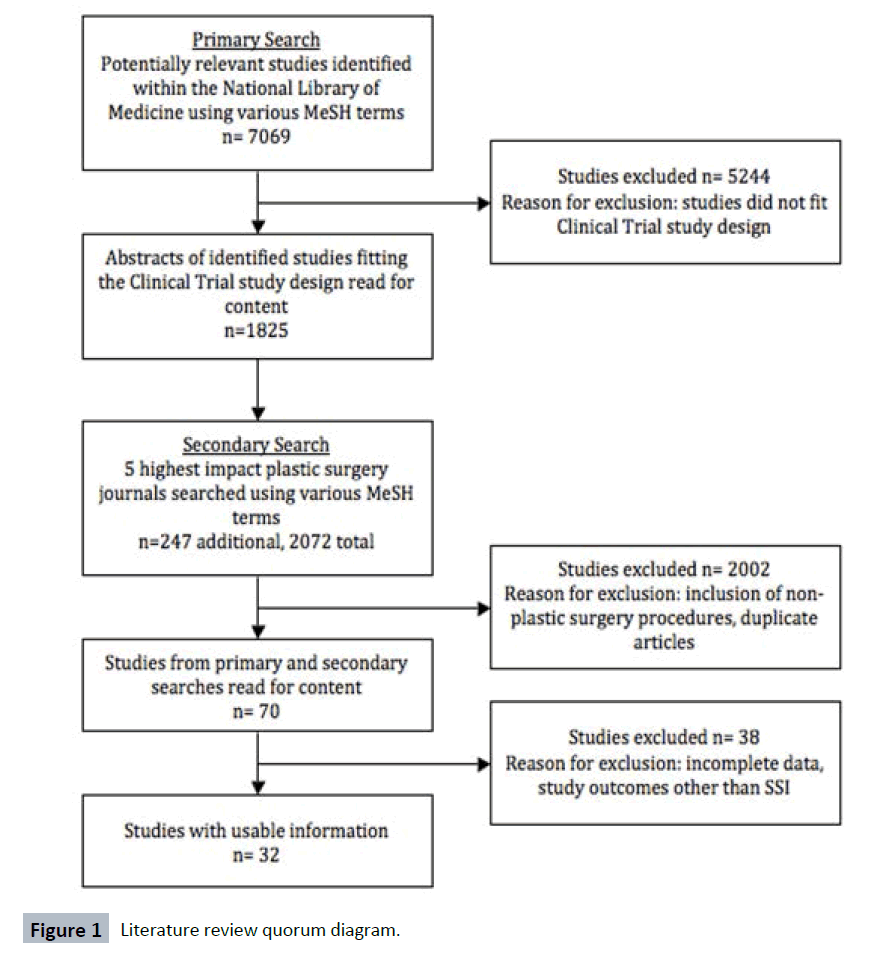
A literature search was performed in the National Library of Medicine using the medical subject headings (MeSH terms) “prophylaxis,” “prophylactic antibiotics,” “pre-operative antibiotics,” “peri-operative antibiotics” and “surgical site infection” combined with various modifiers such as “wound infection,” “postoperative complication,” “timing” and “duration.” To narrow the search field, the article type filter for “clinical trial” was applied. The articles obtained from this search were then reviewed to acquire those that fell within the bounds of our study design. After the initial search, a secondary search was performed using the same terms and modifiers in the top five highest impact plastic surgery journals to ensure the maximum number of studies fitting our criteria had been found. The journals searched included Plastic and Reconstructive Surgery, Journal of Plastic, Reconstructive and Aesthetic Surgery, British Journal of Plastic Surgery, Annals of Plastic Surgery, Aesthetic Plastic Surgery, and Aesthetic Surgery Journal.
Articles dealing specifically with antibiotic prophylaxis in plastic surgery were read for content. Publications were excluded from our study if they included non-plastic surgical procedures, if they did not specify the timing, number, type or duration of antibiotic prophylaxis, if the outcome of surgical site infection was not included, or if the article contained incomplete statistics.
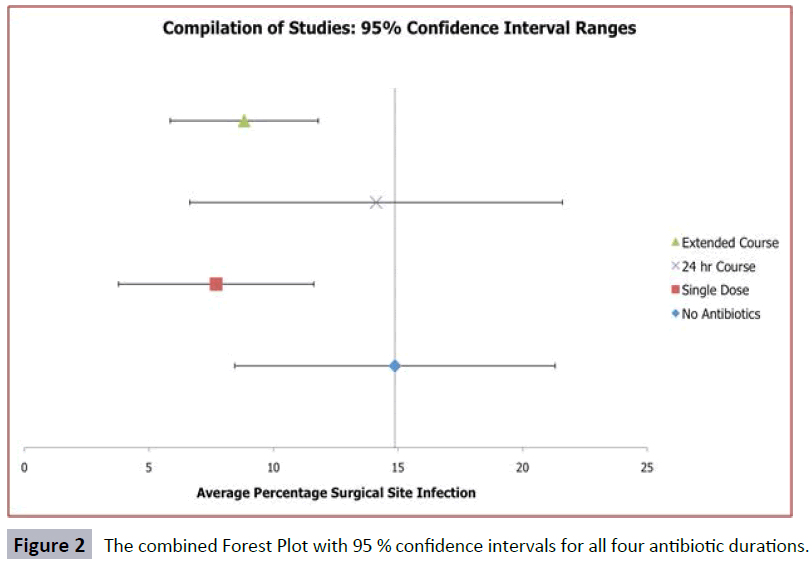
Data was independently extracted from each qualifying study and recorded on a Microsoft Excel spreadsheet. Durations of antibiotic prophylaxis were arbitrarily divided into four groups: no antibiotic prophylaxis, single dose prophylaxis, 24 hour antibiotic course and extended course, which was defined as greater than 24 hours of prophylaxis. Pertinent data points extracted from each study are listed in Table 1. In addition, information about the publication such as authors, study design, field and publication venue were recorded. Analysis of the data was conducted using Microsoft Excel. The random effects statistical model was used to calculate outcomes and a Forest Plot was created of the categories.
Table 1: Data points extracted from the 32 selected articles.
| Data Type |
| Total number of study participants |
| Number of participants in each prophylaxis group |
| Type of antibiotic |
| Timing of first dose |
| Total number of doses |
| Duration of antibiotic course |
| Cumulative infection rate |
| Infection rate among each prophylaxis group |
| Morbidities other than SSI and mortalities |
Results
A quorum diagram detailing the literature search can be viewed in Figure 1. A total of 32 randomized controlled trials were identified from the initial 7,069 articles as dealing specifically antibiotic prophylaxis in plastic surgery and included 12,641 patients in all [18-49]. Within the various subdivisions of plastic surgery twelve of the studies investigated head and neck procedures, twelve looked at breast and body surgeries, seven focused on hand and extremity surgeries, and one study included multiple types of plastic surgery procedures. The patients from all studies were divided into the four general prophylaxis groups (no prophylaxis, single dose prophylaxis, 24 hour prophylaxis and extended course prophylaxis). Cumulatively, there were 2,425 patients in the group receiving no antibiotic prophylaxis, 5,033 in the group receiving a single dose of antibiotic prophylaxis, 1,052 in the group receiving 24 hours of antibiotic prophylaxis and 4,104 in the group receiving extended course prophylaxis.
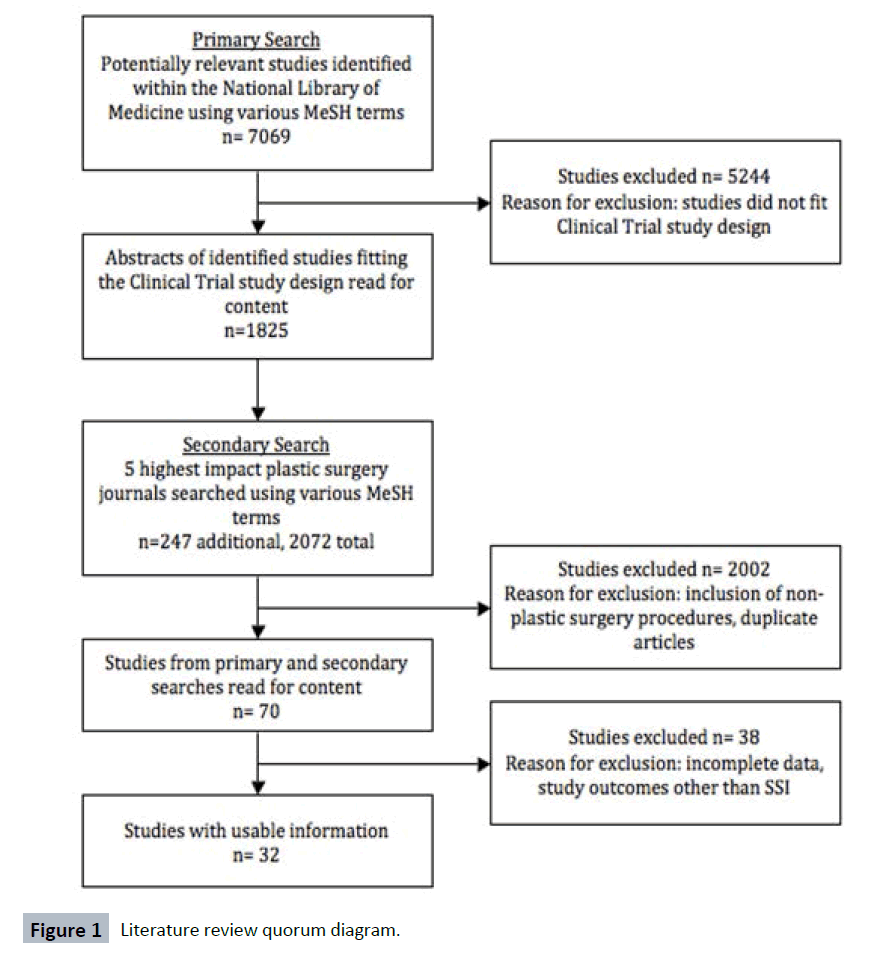
Figure 1: Literature review quorum diagram.
When analyzed, the varying prophylaxis durations did demonstrate differences in the average number of adverse outcomes (Table 2). However, each category also demonstrated a great deal of variability between studies (Table 3). The results show that are single dose of antibiotics have the lowest incidence at 7.7%, followed closely by the extended course of antibiotic prophylaxis at 8.8%. The 24-hour prophylaxis course demonstrated an average infection rate of 14.1% and the group receiving no prophylaxis predictably demonstrated the highest average rate of infection at 14.9%.
Table 2: Surgical site infection rates for the four durations of antibiotic prophylaxis.
| Prophylaxis Duration |
Average Adverse Events ( %) |
| No antibiotics |
14.8 |
| Single dose |
7.7 |
| 24 hour antibiotics |
14.1 |
| Extended antibiotics |
8.8 |
Table 3: SSI rates among each study broken down by prophylaxis group.
| No Antibiotic Prophylaxis |
Single Dose Antibiotic Prophylaxis |
24 Hour Antibiotic Prophylaxis |
Extended Course Antibiotic Prophylaxis |
| Study |
Outcome |
Study |
Outcome |
Study |
Outcome |
Study |
Outcome |
| Aydin |
3.43 % |
Clayton |
34.33 % |
Liu, 2012 |
19.51 % |
Clayton |
18.10 % |
| Veiga-Filho |
14.00 % |
Mirzabeigi |
2.31 % |
Aydin |
3.13 % |
Liu, 2012 |
15.52 % |
| Sevin |
13.04 % |
Danda |
9.33 % |
Danda |
2.67 % |
Mirzabeigi |
0.00 % |
| Hall |
4.56 % |
Khan |
0.84 % |
Khan |
2.62 % |
Khan |
1.72 % |
| Ahmadi |
29.41 % |
Kang |
10.71 % |
Lovato |
13.33 % |
Veiga-Filho |
2.00 % |
| Whittaker |
14.55 % |
Sevin |
4.35 % |
Liu, 2008 |
30.77 % |
Kang |
7.14 % |
| Kompatscher |
3.68 % |
Hall |
3.22 % |
Andrews |
7.32 % |
Lovato |
10.67 % |
| Stevenson |
4.21 % |
Ahmadi |
17.65 % |
Lindeboom |
8.06 % |
Liu, 2008 |
18.52 % |
| Madsen |
10.15 % |
Lindeboom |
9.68 % |
O'Grady |
18.75 % |
Sevin |
8.70 % |
| Amland |
20.51 % |
Rajan |
0.00 % |
Carroll |
11.43 % |
Andrews |
10.98 % |
| Zubowicz |
46.67 % |
Whittaker |
12.50 % |
Bentley |
60.00 % |
Ahmadi |
25.00 % |
| Platt |
8.14 % |
Kompatscher |
3.92 % |
Hotz |
2.00 % |
O'Grady |
6.60 % |
| Sloan |
30.00 % |
Thomas |
5.55 % |
Mustafa |
13.33 % |
Rajan |
3.00 % |
| Worlock |
5.88 % |
Madsen |
4.90 % |
Sloan |
0.00 % |
Whittaker |
4.35 % |
| |
|
Amland |
5.06 % |
Johnson |
18.87 % |
Carroll |
10.26 % |
| |
|
Hotz |
2.04 % |
|
|
Stevenson |
3.06 % |
| |
|
Platt |
4.47 % |
|
|
Bentley |
6.67 % |
| |
|
|
|
|
|
Mustafa |
10.00 % |
| |
|
|
|
|
|
Madsen |
6.57 % |
| |
|
|
|
|
|
Zubowicz |
0.00 % |
| |
|
|
|
|
|
Sloan |
2.08 % |
| |
|
|
|
|
|
Johnson |
25.00 % |
| |
|
|
|
|
|
Worlock |
7.04 % |
It was curiously observed that the 24-hour prophylaxis group appeared to have significantly higher rates of SSI than either the single dose or extended course groups, closely resembling the group receiving no prophylaxis. Upon analysis of the studies, it was determined that a larger number of hand and extremity surgical procedures were included in the 24 hour group than in either of the other three prophylaxis groups. Many reconstructive hand procedures occur after trauma and can therefore be categorized as contaminated procedures, while elective procedures such as breast reconstruction are categorized as clean or clean-contaminated. It was hypothesized that the larger rate of traumatic events among the hand procedures resulted in higher initial rates of surgical contamination and therefore drove the post-operative rates of SSI up in the 24-hour prophylaxis group.
A Forest Plot of the results depicted similar trends (Figure 2). The variability amongst the studied resulted in large, overlapping 95% confidence intervals. The differences in average rate of SSI indicative there is a slight improvement in outcomes in the single dose and extended dose prophylaxis, but the overlapping confidence intervals render the difference as not statistically significant.
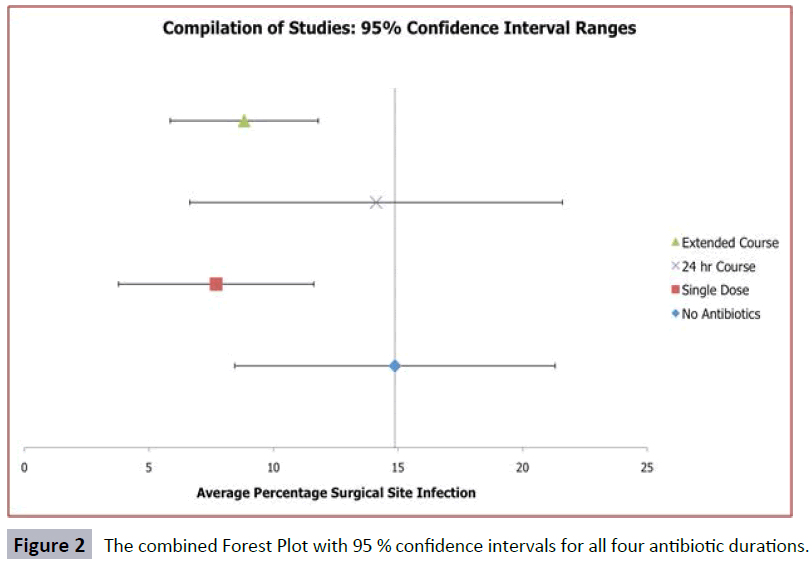
Figure 2: The combined Forest Plot with 95 % confidence intervals for all four antibiotic durations.
Discussion
In surgery, a great deal of focus has been placed on prevention of complications, particularly ones such as SSIs. Antibiotic prophylaxis is one area of developing research considered crucially important, but acknowledged by many to be lacking in evidence in some fields [15]. Within the field of plastic surgery in particular, there is yet to be a prospective trial that establishes a concrete, evidence-based standard of care and antibiotic prophylaxis remains a much discussed and studied topic. When used appropriately, antibiotic prophylaxis has been shown to decrease the incidence of SSIs, resulting in improved outcomes as well as economic benefits [50]. Excessive use of antibiotics, however, is strongly discouraged due to the potential for developing resistance as well as for harmful side effects and consequences to patients, such as C. difficile colitis [50,51].
At this time, wide variations regarding the use of antibiotics prophylactically are present not only in plastic surgery, but in most surgical fields. A recent international survey found differences to exist between European and North American surgeons’ use of antibiotic prophylaxis. Overall, the survey suggested that hesitancy is present for using antibiotics as recommended citing that many surgeons continue the prophylaxis for multiple days over the recommended prophylaxis durations following surgery [52]. This study is not alone in illustrating a need for stronger adherence to guidelines regarding prophylactic antibiotics [53].
Some important limitations to this study should be pointed out. Firstly, we acknowledge the limitation of grouping all surgical procedures, within the various subdivisions of plastic surgery, solely based on four general prophylactic antibiotic groups. The broad inclusion criterion was to allow clinical heterogeneity; however, prophylactic antibiotic treatments should be used on a case-by-case basis. Future investigation may be warranted in further stratifying based on wound type or procedure being performed. Lastly, the possible introduction of selection bias as well as other biases carried over from the studies, in which this meta-analysis examined, should be recognized.
In the shifting political and financial aspects of healthcare, guidelines and adherence to prophylaxis will likely become even more significant. Due to the changing economics and policies of medicine, as well as to the responsibility of physicians to their patients, it is crucial that the body of evidence-based literature in plastic surgery regarding antibiotic prophylaxis be improved.
Conclusion
This meta-analysis underlines the conflicting reports regarding the efficacy of antibiotics in different plastic surgery procedures and emphasizes the variability among usage currently present in the plastic surgery literature. When the data was compiled and analyzed, large, overlapping confidence intervals were demonstrated on Forest plot. These intervals illustrate the lack of cohesiveness among the current literature and indicate the need for a greater number of subjects in the study populations in order to determine whether or not significant differences exist.
Recent studies indicate that antibiotic prophylaxis use in plastic surgery is increasing, emphasizing a growing demand for concrete scientific evidence and guidelines [54]. The growing use along with the results of this study demonstrates a need for increased (and improved) research regarding the subject of antibiotic prophylaxis in the field of plastic surgery.
Conflicts of Interest and Sources of Funding
None declared.
8771
References
- Bratzler DW, Houck PM, Richards C, Steele L, Dellinger EP, et al. (2005) Use of antimicrobial prophylaxis for major surgery: baseline results from the National Surgical Infection Prevention Project.Arch Surg 140: 174-182.
- Bratzler DW, Houck PM (2005) Antimicrobial prophylaxis for surgery: an advisory statement from the National Surgical Infection Prevention Project. Am J Surg 189: 395-404.
- Eskicioglu C, Gagliardi AR, Fenech DS, Shawn FS, Marg MRNet al. (2012) Surgical site infection prevention: a survey to identify the gap between evidence and practice in University of Toronto teaching hospitals. Can J Surg 55:233-238.
- Dellinger EP, Gross PA, Barrett TL, Krause PJ, Martone WJ,et al. (1994) Quality standard for antimicrobial prophylaxis in surgical procedures. Infectious Diseases Society of America. Clin Infect Dis18:422-427.
- Adetayo OA, Salcedo SE, Biskup NI, Gupta SC (2012) The battle of words and the reality of never events in breast reconstruction: incidence, risk factors predictive of occurrence, and economic cost analysis. PlastReconstr Surg 130:23-29.
- Kao LS, Lew DF, Doyle PD, Carrick MM, Jordan VS, et al. (2010) A tale of 2 hospitals: a staggered cohort study of targeted interventions to improve compliance with antibiotic prophylaxis guidelines.Surgery 148: 255-262.
- Tadiparthi S (2008) Prophylactic antibiotics for clean, non-implant plastic surgery: what is the evidence?J Wound Care 17: 392-394, 396-8.
- Gagliardi AR, Fenech D, Eskicioglu C, Nathens AB, McLeod R (2009) Factors influencing antibiotic prophylaxis for surgical site infection prevention in general surgery: a review of the literature. Can J Surg 52:481-489.
- Commission TJ (2013) Specifications Manual for National Hospital Inpatient Quality Measures v4.2b.
- Young B, Ng TM, Teng C, Ang B, Tai HY, et al. (2011) Nonconcordance with surgical site infection prevention guidelines and rates of surgical site infections for general surgical, neurological, and orthopedic procedures.Antimicrob Agents Chemother 55: 4659-4663.
- Bratzler DW, Dellinger EP, Olsen KM, Perl TM, Auwaerter PG, et al. (2013) Clinical practice guidelines for antimicrobial prophylaxis in surgery. Am J Health Syst Pharm 70:195-283.
- Page CP, Bohnen JM, Fletcher JR, McManus AT, Solomkin JS, et al. (1993) Antimicrobial prophylaxis for surgical wounds. Guidelines for clinical care.Arch Surg 128: 79-88.
- Bratzler DW, Hunt DR (2006) The surgical infection prevention and surgical care improvement projects: national initiatives to improve outcomes for patients having surgery. Clin Infect Dis 43:322-330.
- Chang SH, Krupnick AS (2012) Perioperative antibiotics in thoracic surgery.Thorac Surg Clin 22: 35-45, vi.
- Koch CG, Nowicki ER, Rajeswaran J, Gordon SM, Sabik JF 3rd, et al. (2012) When the timing is right: Antibiotic timing and infection after cardiac surgery.J Thorac Cardiovasc Surg 144: 931-937.
- Leong JW, Kunzel C, Cangialosi TJ (2012) Management of the American Heart Association's guidelines for orthodontic treatment of patients at risk for infective endocarditis. Am J OrthodDentofacialOrthop 142:348-354.
- Tribble DR, Lloyd B, Weintrob A, Ganesan A, Murray CK, et al. (2011) Antimicrobial prescribing practices following publication of guidelines for the prevention of infections associated with combat-related injuries. JTrauma71:299-306.
- Ahmadi AH, Cohen BE, Shayani P (2005) A prospective study of antibiotic efficacy in preventing infection in reduction mammaplasty. PlastReconstr Surg 116:126-131.
- Amland PF, Andenaes K, Samdal F, Lingaas E, Sandsmark M, et al. (1995) A prospective, double-blind, placebo-controlled trial of a single dose of azithromycin on postoperative wound infections in plastic surgery. PlastReconstr Surg 96:1378-1383.
- Andrews PJ, East CA, Jayaraj SM, Badia L, Panagamuwa C, et al. (2006) Prophylactic vs postoperative antibiotic use in complex septorhinoplasty surgery: a prospective, randomized, single-blind trial comparing efficacy. Arch Facial Plast Surg 8:84-87.
- Aydin N, Uraloglu M, YilmazBurhanoglu AD, Sensöz O (2010) A prospective trial on the use of antibiotics in hand surgery.PlastReconstr Surg 126: 1617-1623.
- Bentley KC, Head TW, Aiello GA (1999) Antibiotic prophylaxis in orthognathic surgery: a 1-day versus 5-day regimen. J Oral Maxillofac Surg 57: 226-230.
- Carroll WR, Rosenstiel D, Fix JR, de la Torre J, Solomon JS, et al. (2003) Three-dose vs extended-course clindamycin prophylaxis for free-flap reconstruction of the head and neck.Arch Otolaryngol Head Neck Surg 129: 771-774.
- Clayton JL, Bazakas A, Lee CN, Hultman CS, Halvorson EG (2012) Once is not enough: withholding postoperative prophylactic antibiotics in prosthetic breast reconstruction is associated with an increased risk of infection. PlastReconstr Surg 130:495-502.
- Danda AK, Wahab A, Narayanan V, Siddareddi A (2010) Single-dose versus single-day antibiotic prophylaxis for orthognathic surgery: a prospective, randomized, double-blind clinical study. J Oral Maxillofac Surg 68:344-346.
- Hall JC, Willsher PC, Hall JL (2006) Randomized clinical trial of single-dose antibiotic prophylaxis for non-reconstructive breast surgery.Br J Surg 93: 1342-1346.
- Hotz G, Novotny-Lenhard J, Kinzig M, Soergel F (1994) Single-dose antibiotic prophylaxis in maxillofacial surgery.Chemotherapy 40: 65-69.
- Johnson JT, Schuller DE, Silver F, Gluckman JL, Newman RK, et al. (1986) Antibiotic prophylaxis in high-risk head and neck surgery: one-day vs. five-day therapy.Otolaryngol Head Neck Surg 95: 554-557.
- Kang SH, Yoo JH, Yi CK (2009) The efficacy of postoperative prophylactic antibiotics in orthognathic surgery: a prospective study in Le Fort I osteotomy and bilateral intraoral vertical ramus osteotomy. Yonsei Med J 50:55-59.
- Khan UD (2010) Breast augmentation, antibiotic prophylaxis, and infection: comparative analysis of 1,628 primary augmentation mammoplasties assessing the role and efficacy of antibiotics prophylaxis duration. AesthetPlast Surg 34:42-47.
- Kompatscher P, von Planta A, Spicher I, Seifert B, Vetter S, et al. (2003) Comparison of the incidence and predicted risk of early surgical site infections after breast reduction.Aesthetic Plast Surg 27: 308-314.
- Lindeboom JA, Tuk JG, Kroon FH, van den Akker HP (2005) A randomized prospective controlled trial of antibiotic prophylaxis in intraoral bone grafting procedures: single-dose clindamycin versus 24-hour clindamycin prophylaxis. Mund Kiefer Gesichtschir 9:384-388.
- Liu DZ, Dubbins JA, Louie O, Said HK, Neligan PC, et al. (2012) Duration of antibiotics after microsurgical breast reconstruction does not change surgical infection rate. PlastReconstr Surg 129:362-367.
- Liu SA, Tung KC, Shiao JY, Chiu YT (2008) Preliminary report of associated factors in wound infection after major head and neck neoplasm operations--does the duration of prophylactic antibiotic matter? J LaryngolOtol 122:403-408.
- Lovato C, Wagner JD (2009) Infection rates following perioperative prophylactic antibiotics versus postoperative extended regimen prophylactic antibiotics in surgical management of mandibular fractures. J Oral Maxillofac Surg 67:827-832.
- Madsen MS, Neumann L, Andersen JA (1996) Penicillin prophylaxis in complicated wounds of hands and feet: a randomized, double-blind trial.Injury 27: 275-278.
- Mirzabeigi MN, Mericli AF, Ortlip T, Tuma GA, Copit SE, et al. (2012) Evaluating the role of postoperative prophylactic antibiotics in primary and secondary breast augmentation: a retrospective review. Aesthet Surg J 32:61-68.
- Mustafa E, Tahsin A (1993) Cefotaxime prophylaxis in major non-contaminated head and neck surgery: one-day vs. seven-day therapy.J LaryngolOtol 107: 30-32.
- O'Grady KF, Thoma A, Dal Cin A (2005) A comparison of complication rates in large and small inferior pedicle reduction mammaplasty.PlastReconstr Surg 115: 736-742.
- Platt R, Zaleznik DF, Hopkins CC, Dellinger EP, Karchmer AW, et al. (1990) Perioperative antibiotic prophylaxis for herniorrhaphy and breast surgery.N Engl J Med 322: 153-160.
- Rajan GP, Fergie N, Fischer U, Romer M, Radivojevic V, et al. (2005) Antibiotic prophylaxis in septorhinoplasty? A prospective, randomized study.PlastReconstr Surg 116: 1995-1998.
- Sevin A, Senen D, Sevin K, Erdogan B, Orhan E (2007) Antibiotic use in abdominoplasty: prospective analysis of 207 cases. J PlastReconstrAesthet Surg 60:379-382.
- Sloan JP, Dove AF, Maheson M, Cope AN, Welsh KR (1987) Antibiotics in open fractures of the distal phalanx?J Hand Surg Br 12: 123-124.
- Stevenson J, McNaughton G, Riley J (2003)The use of prophylactic flucloxacillin in treatment of open fractures of the distal phalanx within an accident and emergency department: a double-blind randomized placebo-controlled trial. J Hand Surg Br28:388-394.
- Thomas R, Alvino P, Cortino GR, Accardo R, Rinaldo M, et al. (1999) Long-acting versus short-acting cephalosporins for preoperative prophylaxis in breast surgery: A randomized double-blind trial involving 1,766 patients. Chemotherapy 45:217-223.
- Veiga-Filho J, Veiga DF, Sabino-Neto M, Amorim MC, Novo NF, et al. (2010) The role of antibiotics in reduction mammaplasty.Ann Plast Surg 65: 144-146.
- Whittaker JP, Nancarrow JD, Sterne GD (2005)The role of antibiotic prophylaxis in clean incised hand injuries: a prospective randomized placebo controlled double blind trial. J Hand Surg Br 30:162-167.
- Worlock P, Boland P, Darrell J, Hughes S (1980) The role of prophylactic antibodies following hand injuries.Br J Clin Pract 34: 290-292.
- Zubowicz VN, Gravier M (1991) Management of early human bites of the hand: a prospective randomized study.PlastReconstr Surg 88: 111-114.
- Rangel SJ, Fung M, Graham DA, Ma L, Nelson CP, et al. (2011) Recent trends in the use of antibiotic prophylaxis in pediatric surgery.J Pediatr Surg 46: 366-371.
- Schwartz B, Bell DM, Hughes JM (1997) Preventing the emergence of antimicrobial resistance. A call for action by clinicians, public health officials, and patients. JAMA 278:944-945.
- Alexiou VG, Ierodiakonou V, Peppas G, Falagas ME (2010) Antimicrobial prophylaxis in surgery: an international survey.Surg Infect (Larchmt) 11: 343-348.
- Tourmousoglou CE, YiannakopoulouECh, Kalapothaki V, Bramis J, St Papadopoulos J (2008) Adherence to guidelines for antibiotic prophylaxis in general surgery: a critical appraisal.J AntimicrobChemother 61: 214-218.
- Hauck RM, Nogan S (2013) The use of prophylactic antibiotics in plastic surgery: update in 2010.Ann Plast Surg 70: 91-97.