Key words
Daytime Sleepiness, Snoring, Obesity, Obstructive Sleep Apnea, smoking
Introduction
Normal sleep consists of cycles that return 4 to 6 times its duration. Each cycle consists of four stages of sleep's increasing depth and the phase REM (rapid phase eye movements) considered the phase in which we dream. Insomnia occur in up to 35% of the population. Narcolepsy is a disorder of control of sleep especially a disorder of REM sleep. Also, narcolepsy is an inherited non-progressive disorder that usually occurs in early adolescence and remains throughout life. [1]
Excessive sleepiness is not defined as a illness or disturbance but as symptom of other illness. [2] Excessive sleepiness is a strong desire to sleep at times that the person would like to be awake. Despite its high prevalence and the significant adverse effect on patients' functioning and quality of life, excessive sleepiness often goes unrecognised in the primary care setting. [3] Approximately 15% of the adults in the general population suffer from daytime sleepiness at least once during their lifetime. People who suffer from daytime sleepiness often feel that they have not the energy to function in everyday activities, such as to deal with their family and friends or to carry out their professional duties. [4] Normal effects of daytime sleepiness is fatigue, poor concentration, impaired learning, memory impairment, reduced motivation for activities, laziness, errors in operating machinery, driving accidents, resorting to abuse tobacco caffeine and degradation of quality of life. [5] Furthermore, excessive daytime sleepiness associated with the appearance of narcolepsy, which is characterized by cataplexy (sudden loss of muscle tone caused by strong emotions), rapid eye movements such as sleep paralysis and the hallucinations. [6]
Snoring which is associated with the sleepiness is the most common manifestation of obstructive sleep apnea (OSA) and has been used as a surrogate parameter for OSA in many epidemiological studies. [7] Habitual the snoring was the most common symptom (60%), followed by insomnia, which was reported by a third of the population sample. [8] Excessive daytime sleepiness (EDS) is one of the most common symptoms in patients with OSA. The severity of obesity and disordered breathing (apnea-hypopnoea index) seems to be the most important. Results have shown that 40% of the total obese suffer from sleep apnea while conversely 70% of patients with sleep apnea are obese [9]. The OSA is characterized by the presence of at least 5 events per hour of sleep, full stop or significantly reducing of the air flow in the upper airways lasting> 10sec (apnea-hypopnea) accompanied by nightly / or nightly and daytime symptomatology. The term "syndrome of increased resistance of the upper airways'' describes the situation which occurs continuous loud snoring without apneas, hypopneas or hypoxemia and was recorded much increase of respiratory effort. This syndrome has the same symptomatology and natural history with OSA. [10]
A survey conducted on sleepiness has shown that the driver sleepiness is a causative factor in 1% to 3% of all US motor vehicle crashes. About 96% of sleep-related crashes involve passengers, vehicle drivers and 3% involve drivers of large trucks. [11] A study was realized in 1629 adolescents aged 12 to 19 years in China. The prevalence of sleep disturbances occurring ≥3 days per week in the preceding 3 months were: difficulty falling asleep (5.6%), waking up during the night (7.2%), and waking up too early in the morning (10.4%). [12] Three studies evaluated the gravity of daytime sleepness with Epworth Sleepiness Scale. In Poland, the medium grade of Epworth Sleepiness Scale were 8,5 for the total sample. The excessive daytime sleepiness in passive situation were found in the 22,3% and the excessive daytime sleepness in practicing situation in the 0,7%. A study that was realized in 408 adults in the Big city Campo of Brazil reports that the 8,9% suffers from excessive daytime sleepiness. A Japanese study realized that the 8,9% of the sample of adults had irregular results in Epworth Sleepiness Scale. Responses to the ESS were assessed in 687 patients (52.3% African American) in a sleep clinic. Differences in total ESS score and the scores on individual Epworth questions were compared in African Americans and Whites. [13] In a survey conducted in Taiwan (81 men and 79 women) participated 160 students with average age 20,3 ± 1,9 years. The average rating for ESS was 6.7 (3.2%) in men, 5.9 (3.4%) in women and the total score was 6,3 ± 3,3 (ESS score> 10). [14] A study conducted in Greece participated 1501 people aged 19-90 years Frequent snoring was reported in 45.6%, breathing pauses during sleep in 11.0%, and excessive daytime sleepiness in 6.7% of the sample. Patients with Chronic Obstructive Pulmonary Disease (COPD) were more likely to report frequent snoring (OR=1.34; 95% CI:1.04-1.71), breathing pauses (OR=1.46; 95% CI:1.01-2.10), and excessive daytime sleepiness (OR=2.04; 95% CI:1.33-3.14). [15]
Purpose
The purpose of the present study was to identify the subjective daytime sleepiness among students of Technological Educational Institute of Crete and the correlation with sleep-related symptoms and other physical health parameters, the smoking status, the coexistence of chronic disease, symptoms compatible with apnea syndrome - hypopneas, the connection affinity (inheritance) and the body mass index (BMI).
Material and Method
Statistical analysis
The questionnaire Epworth Sleepiness Scale (ESS) was completed by 407 students. Checking the reliability of the 8 questions of ESS found too low Cronbach's a = 0.152. In the bibliography reported very high (> 0.70) but in the Greek version of Tsara et al (2004) have not been evaluated. After the analysis of the results this seems to be becouse of the very small scale responses (Table 6). The average score of the bibliography is only 0,6 (± 0,8) when in many studies is very high and more than 8 or 10 (the possible limits are 0-24).
Study Design
The study was conducted in the Technological Educational Institute of Crete during an 3-month period (December - February 2011). Collection of data was performed using the Epworth Sleepiness Scale. The study was conducted with the quantify-descriptive method randomly. There was voluntary attendance of students. No exclusion criteria were sampled, except for sex and school. For the survey was used the doctor's office of the School of Health and Welfare Services of the Technological Educational Institute of Crete.
The Questionnaire
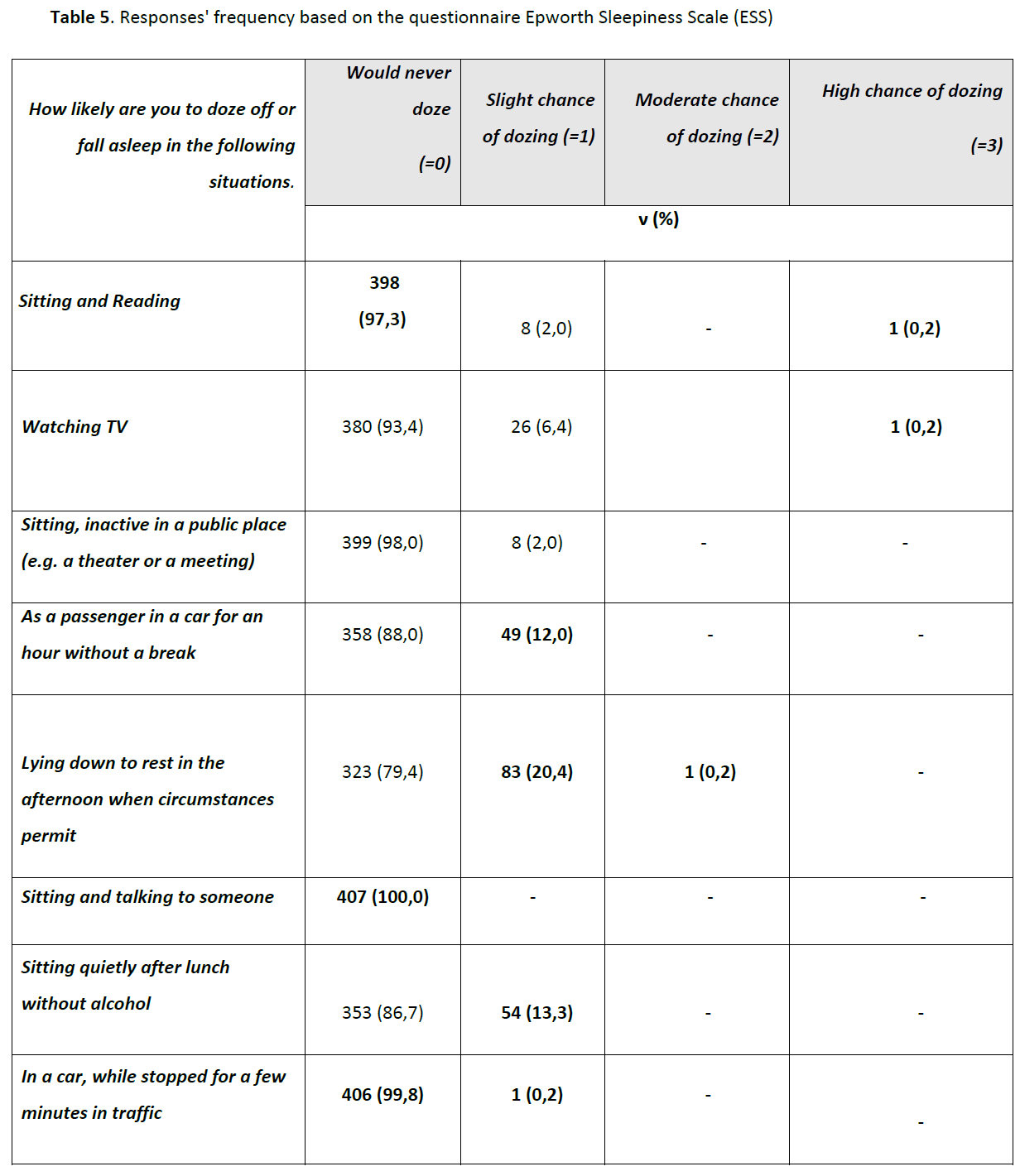
The Epworth Sleepiness Scale (ESS) is a screening tool of measurement of daytime sleepiness which is constituted by 8 questions about the likelihood of dozing in any of 8 situations: sitting and reading, watching TV, sitting, inactive in a public place (e.g., a theater or a meeting), as a passenger in a car for an hour without a break, lying down to rest in the afternoon when circumstances permit, sitting and talking to someone, sitting quietly after a lunch without alcohol, in a car while stopped for a few minutes in the traffic. Response categories include: 0 (would never doze), 1 (slight chance of dozing), 2 (moderate chance of dozing), and 3 (high chance of dozing). Subjects are instructed to respond specifically in relation to dozing off, as opposed to just feeling tired. ESS summary scores range 0–24, its clinical threshold is ≥10, though a threshold of ≥16 has been shown to be more clinically useful. History of genetic predisposition, smoking status, sleep apnea, snoring, insomnia, nasal congestion, sudden awakenings and breathing pauses were included as independent variables. Individual questions (demographic data - age, sex, school, contact information) will be reported in order to serve the goals of the present study.
Measurements
Somatometric measurement (height, weight, neck size, waist and hip circumference) and arterial blood pressure were carried out according to the NHS criteria. Also, It was calculated the Body Mass Index (BMI) and were apprised parameters that concern the heredity and the habit of smoking. BMI was calculated as the body weight divided by the square of height (expressed in kg/m2). Obesity was defined as BMI 30 or more.
Statistical Analysis
With the x2 test analysis were analyzed the descriptive characteristics of students and the distribution of body mass index, the blood pressure, the smoking habit and the grade of the ESS among students. Also, with the non-parametric Mann Whitney test analysis were checked the levels of somatometric measurements and the blood pressure both men and women. Based on the correlation coefficient by Spearman were carried out correlations between the descriptive characteristics of somatometric measurements, smoking, medical history and the grades of questions of the Epworth Sleepiness Scale. Finally, with the one sample Student t test analysis were compared the mean scores of this study with other studies selected from the Greek and international literature. The data analysis was performed using the statistical programme IBM SPSS 19.0.
Results
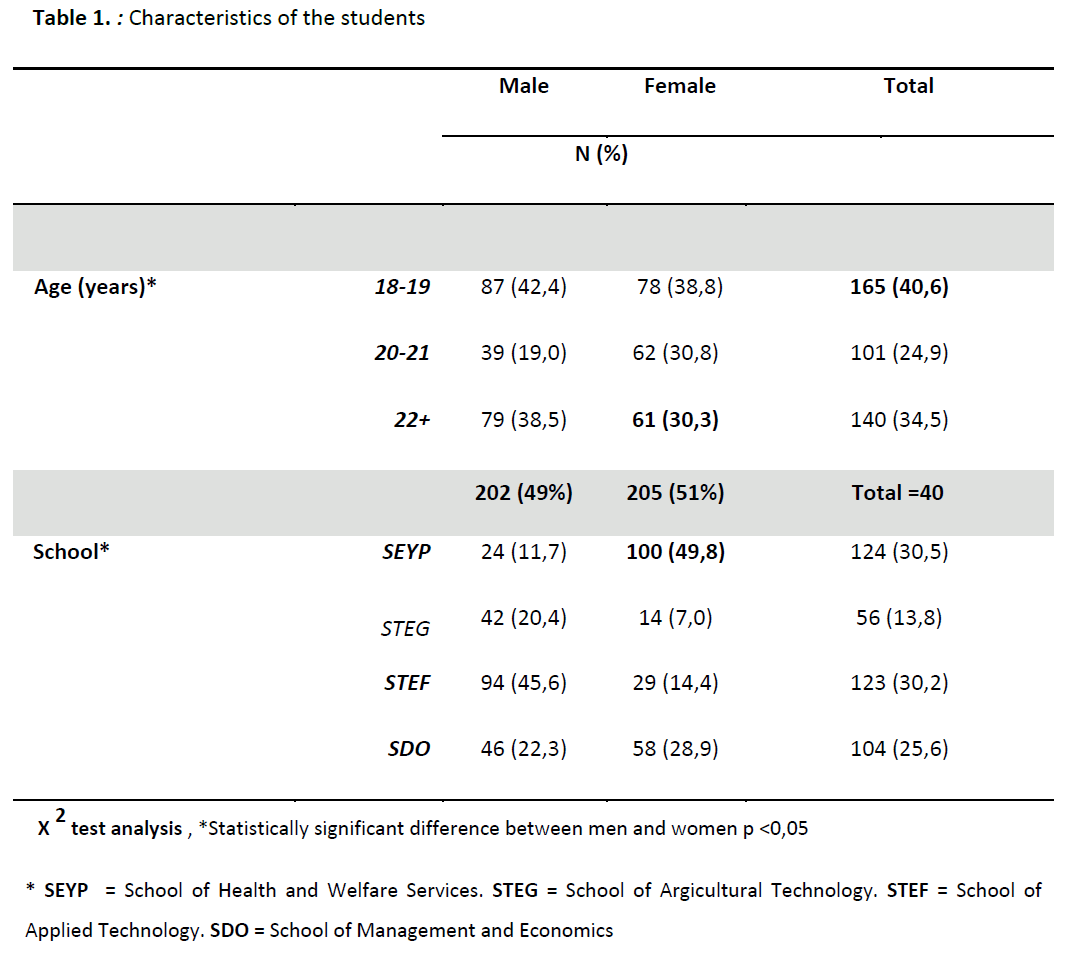
A total of 407 students were enrolled in the study. The table 1 presents the descriptive characteristics of the 407 students: 202 students (49%) were male and 205 (51%) were female. In regard to age, 40,6% of the students were between the age 18 and 19, 24.9% were between 20 and 21 years of age and 34,5% were over the age of 22.
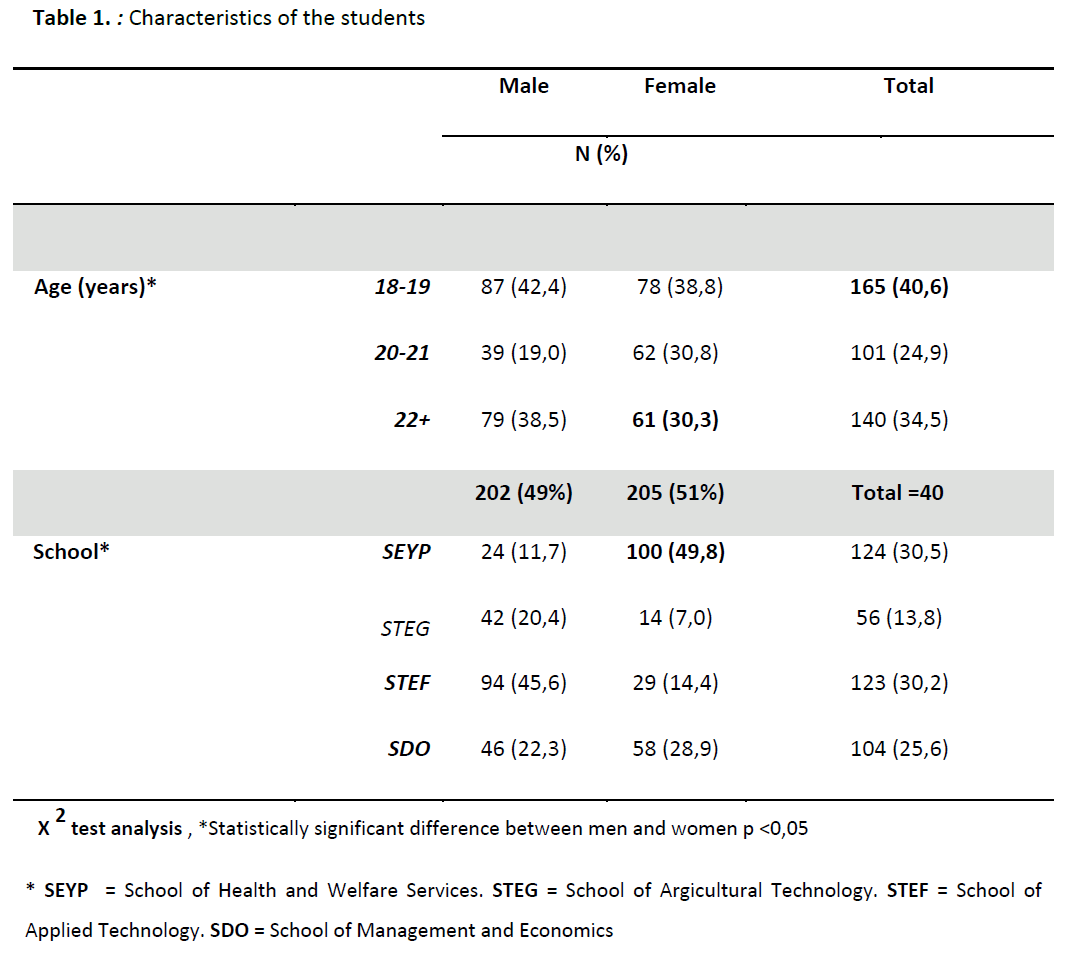
Regarding the school that the students studied, all the students studied in Technological Educational Institute of Crete. From them, 30.5% studied in the School of Health and Welfare Services, 13.8% studied in the School of Agricultural Technology, 30.2% studied in the School of Applied Technology and 25.6% studied in the School of Management and Economics.
With the exception of the middle age, both in Somatometric measurements and in arterial blood pressure there is statistically significant differences between sexes. The male students significantly have higher average body weight (79.4 vs 63,0 kg, p <0,001), BMI (25.0 vs 23,1 kg/m2, p <0,001), neck size, (38.3 vs 32,5 cm, p <0,001) and systolic arterial blood pressure (125 vs 112 mm Hg, p <0,001) than women.
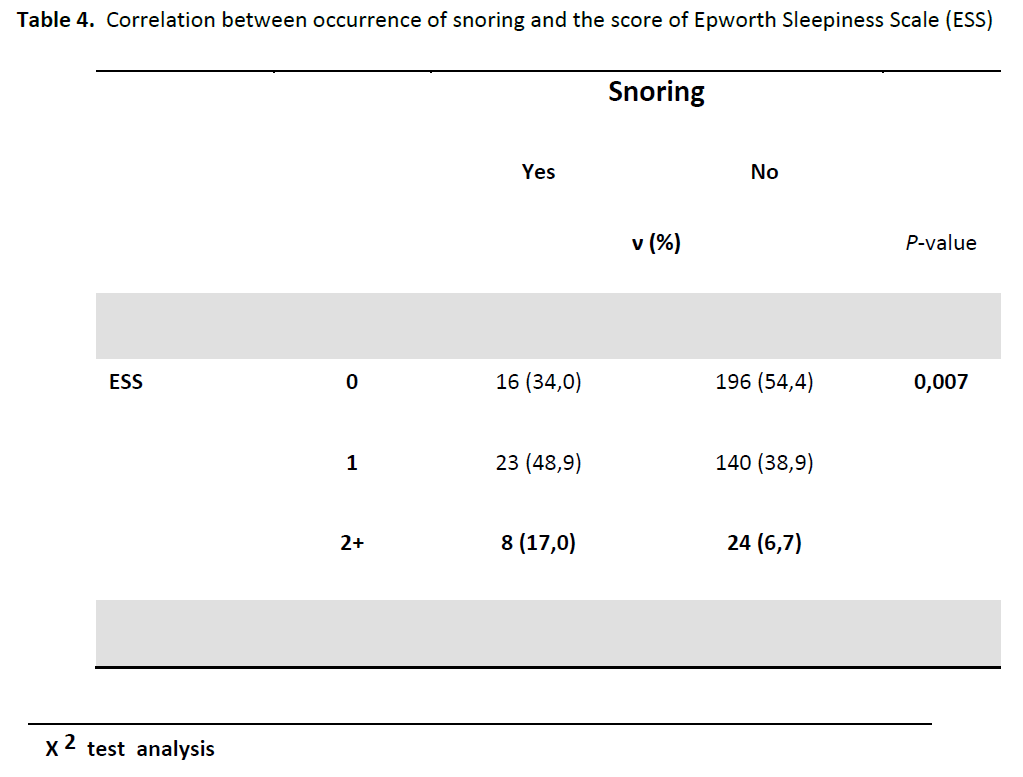
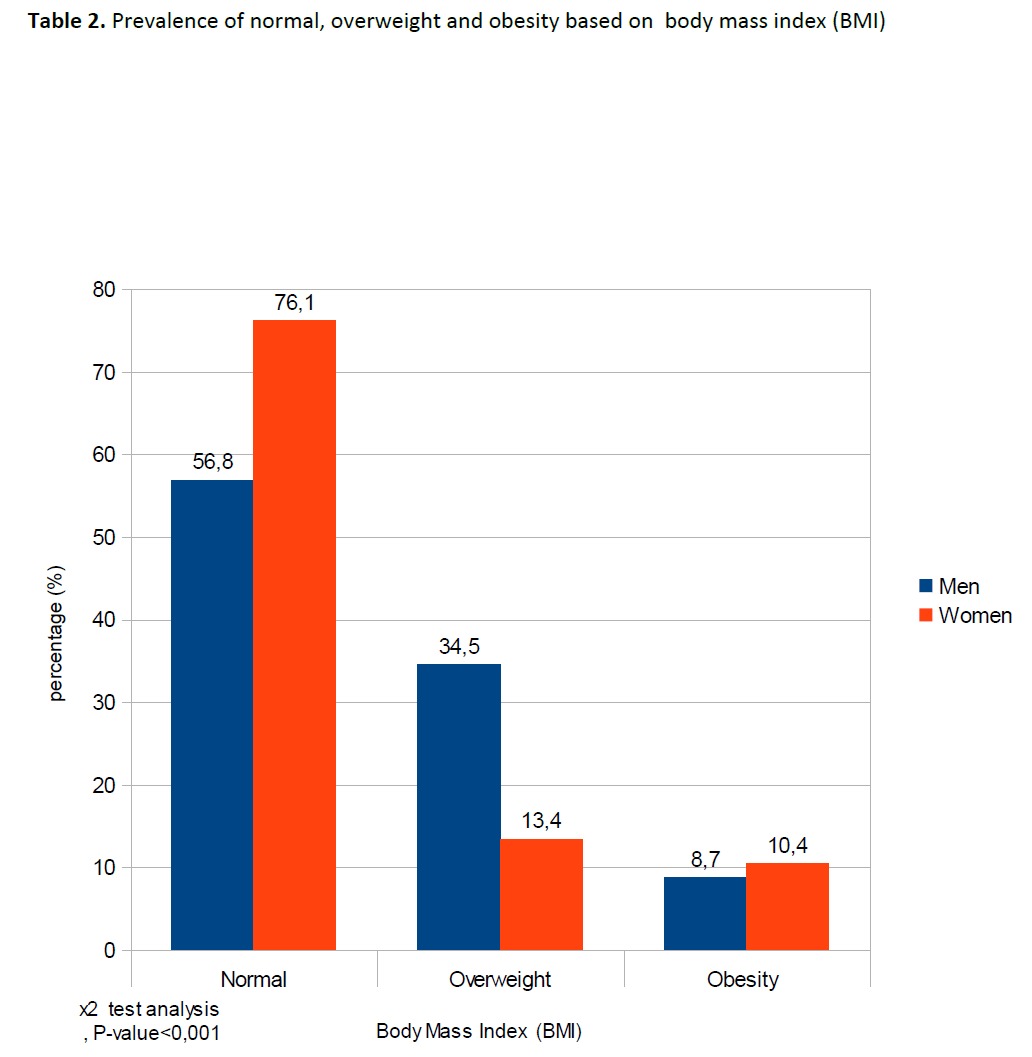
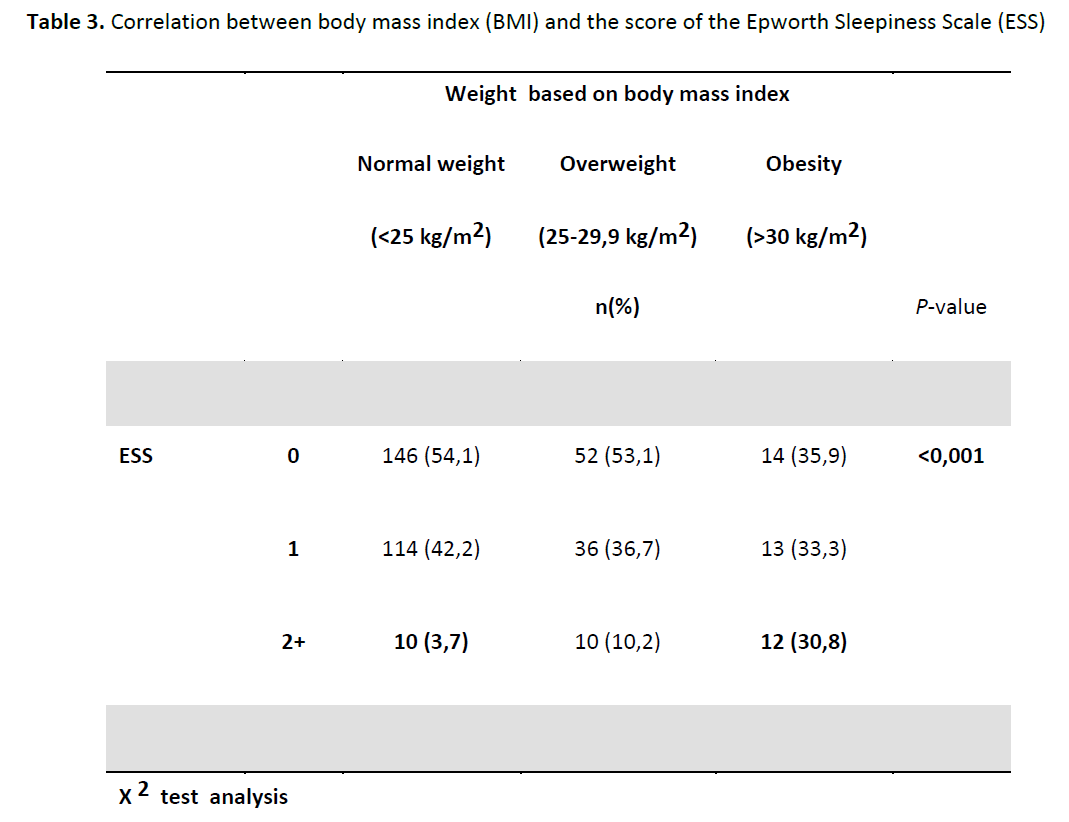
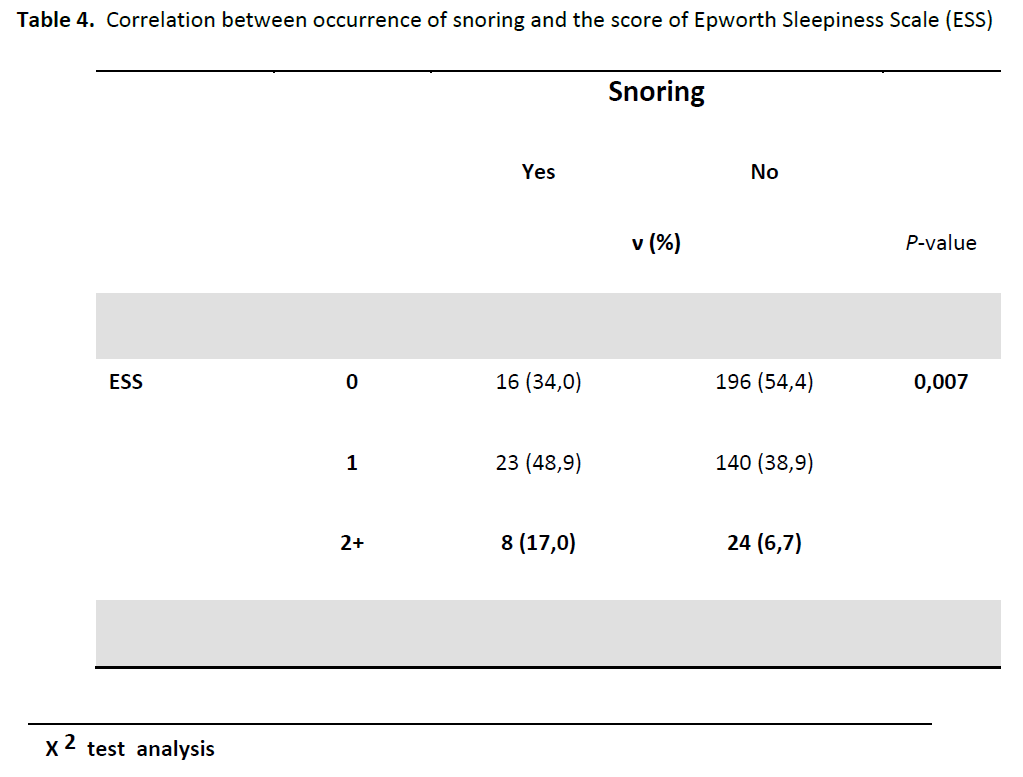
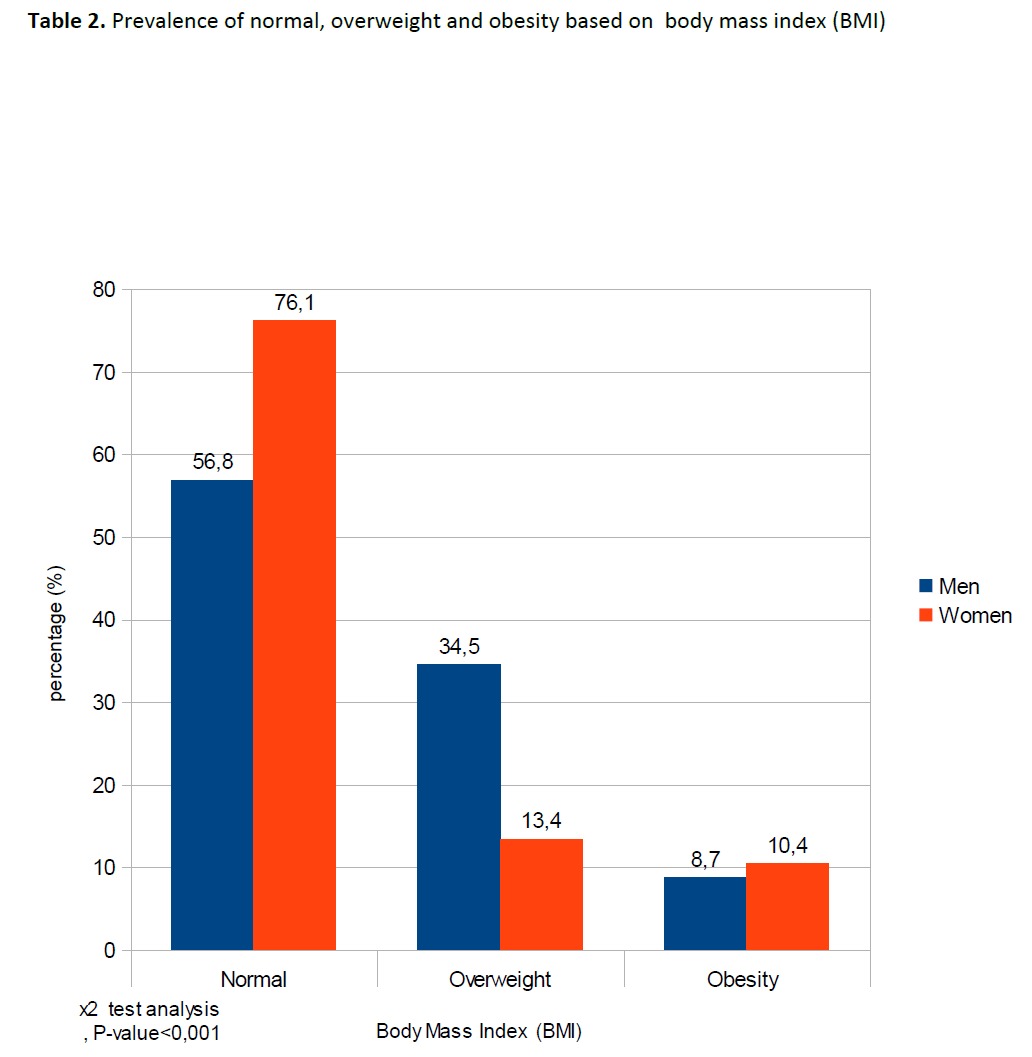
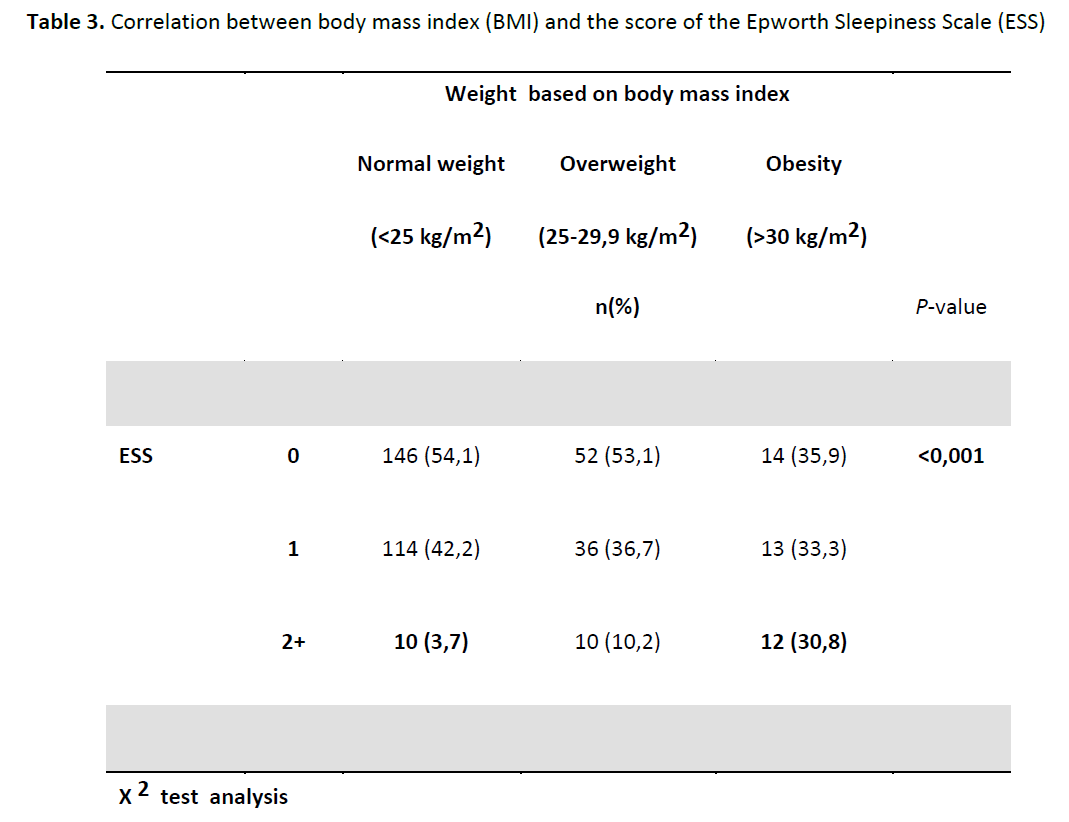
The table 2 presents the prevalence of normal weight, overweight and obesity. There is significantly higher percentage of women students that were obese than men based on BMI (10.4% vs. 8,7%, p <0,001), while significantly were fewer overweight women (13.4% vs. 34.5 %, p <0,001). But generally the percentage of overweight / obesity was higher among male students compared to female students (43.2% vs. 23,8%, p <0,001). The prevalence of high blood pressure showed statistically significantly higher percentage of male than female students. Men had higher levels of systolic or / systolic and diastolic blood pressure (9.7% vs 1,0%, p <0,001). Also, the prevalence of smoking showed that there is no statistically significant difference between men and women smokers (47.1% vs. 37,8%, p = 0,142). The rate of smoking among the student is to 42.5%.In the present study there was significantly higher percentage of students with increased waist circumference (15.3%) compared to normal students (5,5%). Although the ESS score was found at very low levels, significantly there was higher percentage of obese or overweight students with score 2+ versus the students with normal weight (Table 3) (30.8%, 10.2% and 3.7% respectively , p <0,001). The students who snore and had rate 2 + (table 4) are significantly more (17%) compared to those who do not snore (6,7%).
 .
.
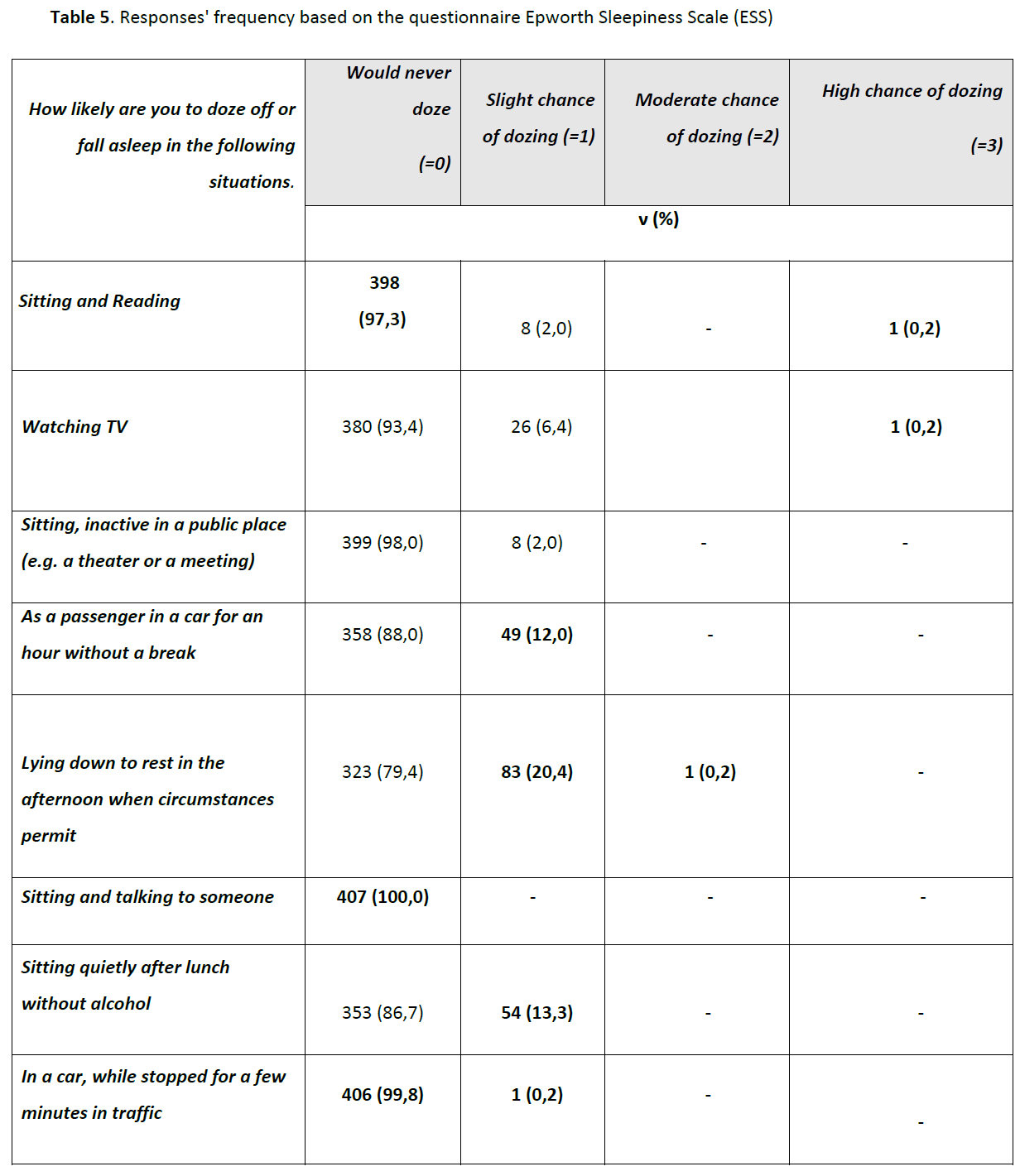
The table 5 presents the frequency of responses that concern the questionnaire Epworth Sleepiness Scale (ESS). Among other things, no chance to fall asleep when "sitting and reading" says the 97.3% of the students , 100% when "Sitting and talking to someone" or 99.8% when "In a car, while stopped for a few minutes in traffic". However, low probability to fall asleep says the 12.0% of the students when "as a passenger in a car for an hour without a break" 20.4% "lying down to rest in the afternoon when circumstances permit" or 13.3% when "Sitting quietly after a lunch without alcohol". There are still some students who say moderate or more likely to fall asleep when "read sitting", "watching TV" or "lying down to rest in the afternoon when circumstances permit". From the scores' estimate of students resulting from the questionnaire ESS (table 6) for the syndrome of daytime sleepiness, 52.1% collects score zero (no chance), 40% collects score equal to one, 7.6% collects score 2 and only 0.2% collects score equal to three or more. In summary, 406 students or 99.8% have scored from 0 to 6 or they have no impact on their sleep. There is no person with score 7-9 or person with moderate sleep and finally one person have score >10 or prevalence 0.2%. Score >10 evaluated as an excessive daytime sleepiness. This indicates that this person has high likelihood to suffer from Obstructive Sleep Apnea.

Discussion
Our results shown that the total score of the ESS has a positive significant correlation with BMI (r = 0,121, p <0,05), the waist circumference (r = 0,115, p <0,05 ) and the snoring (r = 0,148, p <0,05) while not significantly correlated with the parameters such as the arterial blood pressure or smoking the habit. Moreover, the obese students and those students who snore have statistically significantly higher score of the ESS (p <0,05).
From the present study was found only one student suffering from daytime sleepiness. Moreover, the student suffers from obesity, snoring, nasal congestion, respiratory disorders, smoking and has heredity. The brief bibliography review in order to compare the results of the present study with other bibliography showed that ESS scores of the students is statistically significantly less than all of the studies found.
Furthermore, in the present study the prevalence of subjective assessment of daytime sleepiness in the students of Technological Educational Institute of Crete was very low despite the impressive and disappointing rates of obesity and smoking habit. The most powerful factors that seem to be relative with the rating of subjective assessment of daytime sleepiness are the BMI or the waist circumference and the snoring. Other indicators such as heredity, blood pressure or smoking does not seem to be important determinants related with daytime sleepiness because of the students' young age.
In the meanwhile, in the present study the presentation of the ESS score showed very low subjective assessment of daytime sleepiness than other studies. However, generally according to Tsara [16] and colleagues in a sample of 130 Greeks working in hospitals the prevalence of daytime sleepiness with the same measurement tool was found in 8.4%. Another study [17] in adult nurses with chronic sleepiness found 31% with estimated score ESS > 10 or sleepy, but not confirmed by the supposed causal relationship.
Worldwide the prevalence of daytime sleepiness is formed from a variety of different estimates and vary the limits between 0.5% and 14%. These global estimates are generally higher than the estimate of the present research. But it should be noted that diversity exists even in the measurement of the daytime sleepiness with the different criteria even for the same diagnostic tool. The traffic accidents due to daytime sleepiness estimated at 1-3% in the U.S., 10% in France and a very high percentage of 33% in Australia. [18] Nena’s study [19] in their effort to evaluate the productivity of labor in patients with obstructive sleep apnea that the daytime sleepiness has negative effects on productivity. Pilot study investigate sleep problems in Greek nurses found that those who work 11-20 years had more sleep-related symptoms. [20]
Symptoms of daytime sleepiness are a lot and different. Great relation has the daytime sleepiness with the sleep apnea syndrome. There is OSA when a episodes of apnea accompanied by daytime sleepiness. In this case obesity is a key factor and reduce the size of the airways and increases the appearance of OSA. [21] Results of Greek study shown a person with chronic sleep deprivation. This person was young and obese. [22] A person with the same symptoms diagnosed in the present study but without drinking alcohol, smoking, drug use, tranquilizers or other substances and with normal clinical picture. These figures give an important information on diagnosis. Moreover, apnea significantly associated with increased the chance of daytime sleepiness when people "Sitting quietly after lunch without alcohol” (r = 0,113, p <0,05). Also, the daytime sleepiness have correlation with snoring when people "Watch TV” (r = 0,183, p <0,05) or "a passenger in a car for an hour without a break Sitting” (r = 0,150, p <0,05), and the nasal congestion with increased chance to fall asleep when people "As, inactive in a public place (e.g. a theater or a meeting)” (r = 0,105, p <0,05). Also, the total score of the ESS has a positive significant correlation with BMI (r = 0,121, p <0,05), the waist circumference (r = 0,115, p <0,05) or the snoring (r = 0,148, p <0,05)..From the present study the arterial blood pressure and smoking didn't have significantly correlation with ESS.
Summarizing, Korean survey (participated 4405 subjects) reported that the daytime sleepiness has association with snoring. Those who snore were found to have 92% higher risk of daytime sleepiness than those who do not snore. [23] The only incident of our survey said that snoring occurs during sleep. Generally found a positive significant correlation with the total score of the ESS. Moreover, results from another Korean adolescents, have shown a similar relationship of snoring and ESS. Those who snore had a significantly higher score. [24] In the present snoring was found to be associated with both high BMI and the smoking habit.
Our data suggest that an invitation strategy for obese adolescents in primary care settings may identify a large proportion of young people with asymptomatic OSA. Therefore, contributing to the early ignore of OSA. The fact that supports the need for screening and health promotion programs in primary care for preventing obesity in the early age.
Conclusions
Despite the statistical limitation, this study may considered a “pilot”. In accordance with our results, students seems to be healthy from the daytime sleepiness. Obesity is a major demographic problem in Greece. Obesity is connected with many diseases and the daytime sleepiness which is one of the characteristic symptom in OSA Syndrome. Additionally, the lack of the primary care in Greece and inadequate conduct screening programs in the young population for a number of risk factors increase the chances of syndromes and diseases appearance at older ages.
3070
References
- Velentzas J. Insomnia: What lies behind it [website]. Iatronet 2007 - [ recieved on 13 May 2011] - Available on the Internet: https://www.iatronet.gr/article.asp?art_id=1342 (14/5/2011).
- Ohayon MM. From wakefulness to excessive sleepiness: what we know and still need to know. Sleep Med Rev 2009; 12(2): 129-141.
- Schwartz J RL. Modafinil in the treatment of excessive sleepiness. Drug Des Devel Ther. 2008; 2: 71–85.
- Neta S. Insomnia: The heat disturbs our sleep [website]. Iatronet June 2007 - [ recieved on 13 May 2011] - Available on the Internet : < https://www.iatronet.gr/newsarticle.asp?art_id=2255 >
- McWhirter D, Bae C, Budur K. The Assessment, Diagnosis, and Treatment of Excessive Sleepiness: Practical Considerations for the Psychiatrist. Psychiatry (Edgmont) 2007;4(9): 26–35.
- Khatami R et al. Insufficient Non-REM Sleep Intensity in Narcolepsy-Cataplexy. Sleep 2007; 30(8): 980–989.
- Nakano H, Furukawa T, Nishima S. Relationship Between Snoring Sound Intensity and Sleepiness in Patients with Obstructive Sleep Apnea. J Clin Sleep Med 2008;4(6): 551–556.
- Bouscoulet LT et al. Prevalence of Sleep Related Symptoms in Four Latin American Cities. J Clin Sleep Med 2008; 4(6): 579–585.
- Koehler U et al. Daytime sleepiness in patients with Obstructive Sleep Apnoea (OSA) - pathogenetic factors. Pneumologie 2010; 65(3):137-42.
- Scientific informations of the Greek Medical Society of Obesity. Obesity and apnea-hypopneas Sleep syndrome. Advances in Obesity April. – July. 2007;15(4):1, 4-5.
- Lyznicki JM, Doege TC, Davis RM, Williams MA. Sleepiness, Driving, and Motor Vehicle Crashes, for the Council on Scientific Affairs, American Medical Association. JAMA 1998; 279 (23):1908-1913.
- Chung KF, Cheung MM. Sleep-Wake Patterns and Sleep Disturbance among Hong Kong Chinese Adolescents. Sleep 2008; 31(2): 185–194.
- Ohayon MM. From wakefulness to excessive sleepiness: what we know and still need to know. Sleep Med Rev 2009; 12(2): 129-141.
- Kang JH, Chen SC. Effects of an irregular bedtime schedule on sleep quality, daytime sleepiness, and fatigue among university students in Taiwan. BMC Public Health 2009; 9: 248.
- Karachaliou F, Kostikas K, Pastaka C, Bagiatis V, Gourgoulianis KI. Prevalence of sleep-related symptoms in primary care population- their relation to asthma and COPD. Primary Care Respiratory Journal 2007; 16(4): 222-228.
- Tsara V, Serasli E, Amfilochiou A, Constantinidis T, Christaki P. Greek version of the Epworth Sleepiness Scale. Sleep Breath 2004; 8(2): 91-5.
- Canani SF, John AB, Raymundi MG, Schönwald S, Menna Barreto SS. Prevalence of sleepiness in a group of Brazilian lorry drivers. Public Health 2005; 119(10): 925-929.
- Nena E Steiropoulos T, Perantoni E, Serasli E Correlation of apnea syndrome and low productivity at work [website]. - [ recieved on 24 May 2011] - Available on the Internet: < https://www.elinyaecongress2010.gr/01.anartimenes/aa037.pdf >
- Rupee Z, Rekleiti T, Kyloudis P, Bagiatis B, C. Wozniacki. Investigation of sleep problems in Greek nurses: a pilot study 2010 [website]. - [ recieved on 14 Aprli 2011] - Available on the Internet : < https://www.cyna.org/17thm/030.pdf >
- Michailidou M. Clinical expression and recognition of OSA. Info Respiratory January - March 2005; 33:34.
- Grigoriadis D, Tsara B. A case of chronic sleep deprivation. Greek General Hospital Psychiatry 2006; 4 (1): 30-31.
- Joo S, Baik I, Yi H, Jung K, Kim J, Shin C. Prevalence of excessive daytime sleepiness and associated factors in the adult population of Korea. Sleep Med 2009; 10(2): 182-188.
- Shin C, Joo S, Kim J, Kim T. Prevalence and correlates of habitual snoring in high school students. Chest 2003; 124(5): 1709-15.






 .
.