Keywords
Snoring, obesity, obstructive sleep apnea
Introduction
Obstructive sleep apnea (OSA) is characterized by repetitive partial or complete closure of the upper airway during sleep. This can happen many times during night in patients with moderate-to-severe [1]. The OSA is characterized by the presence of at least 5 events per hour of sleep, full stop or significantly reducing of the air flow in the upper airways lasting > 10 sec (apnea-hypopnea) accompanied by nightly / or nightly and daytime symptomatology [2]. OSA is part of a spectrum of sleep-related breathing disorders that includes snoring, upper airway resistance syndrome and central sleep apnea. The OSA is the combination of obstructive apneas with tiredness during day or recurrent awakenings [3].
Many studies assessing the prevalence of OSA syndrome have been carried out in young population [4,5]. A first descriptions given for OSA was severe apnea that occurs in middle age obese men [6]. The 33% of OSA patients are women especially in people who are in old age or from Southeast Asia [7,8]. OSA is frequent and it is found in 2% of middle-aged women and 4% of middle-aged men [9]. The therapy of OSA includes weight loss, upper airway surgery, oral appliances, and nasal continuous positive airway pressure [10-13]. The most of those with OSA remain without diagnose. Only the 10% of the population was checked (screening) for the presence of OSA. This is a common disorder with a frequency similar to the bronchial asthma and diabetes in the general population [14].
Snoring is the most symptom of obstructive sleep apnea (OSA) followed by sleepiness, which was reported by a third of the population sample [15]. Also, excessive daytime sleepiness (EDS) is one of the most frequent symptoms in patients with OSA. Moreover, obesity appears in up to 50% of obese male.16 Slim people also can have OSA [17]. Results have shown that 40% of the total obese suffer from sleep apnea while conversely 70% of patients with sleep apnea are obese [18]. The increasing severity of OSA is an important risk factor for the development of hypertension over four years [19]. The effective treatment of OSA in hypertensive patients resulted in significant reduction of blood pressures [20].
In a study of Nena et al., [21] for evaluation of working capacity in patients with OSA without other health problems showed a significant correlation the prices of EWPS and ESS scores (r2 = 0,127, p <0,001). Also, Sjosten [22] showed that patients with OSA had significantly increased number of lost working days. Finally, OSA patients are more likely to have a car accidents [23].
Aim
The aim of the present study was to estimate the prevalence of obstructive sleep apnea syndrome (OSA) in a population of Greek adult students of the Technological Educational Institute of Crete and the correlation with other health parameters.
Material and method
Study Design
The study was conducted in the Technological Educational Institute of Crete over a 3-month period (October - December 2010). We conducted a population-based cross-sectional study on a randomly selected young population aged 18 years or more, who visited doctor’s office for any reason. Collection of data was performed using the Berlin questionnaire. The final selection of 400 students was determined by the principles of convenience sampling. There was voluntary attendance of students.
Study questionnaire
The Berlin Questionnaire consists of three categories (10 questions) designed to illicit information regarding snoring or “3–4 times per week” (category 1), daytime somnolence (category 2) and the presence of obesity and/or hypertension (category 3). In categories 1 and 2, patients answering “almost every day” or “3–4 times per week” were considered to have significant symptoms. Response in categories 1 and 2 was positive if greater than or equal to two items of the category were positive. Response in category 3 was considered positive if the subject had obesity, hypertension, or both. The presence of obesity and/or hypertension in category 3 was considered significant. A patient was considered to have a high likelihood of sleep disordered breathing if significant symptoms exist in 2 out of the 3 categories.
Measurements
Apart from the demographic data were carried out somatometric measurement (height, weight, waist circumference to height, waist and neck circumference) and arterial blood pressure. Also, It was calculated the Body Mass Index (BMI) and were apprised parameters that concern snoring, age, gender, daytime sleepiness, smoking, nasal congestion, heredity, sudden awakenings and respiratory problems. BMI was calculated as the body weight divided by the square of height (expressed in kg/m2). Obesity was defined as BMI 30 or more.
Statistical Analysis
Statistical analysis was performed by using the SPSS 19.0. Reliability was assessed by internal consistency using Cronbach's alpha test. With the x2 test analysis were analyzed the distributions of the descriptive characteristics and the frequency distributions in Berlin questionnaire among students. Based on the correlation coefficient by Spearman were carried out correlations between the descriptive characteristics of somatometric measurements, blood pressure, medical or family history. Finally, the control of the somatometric measurements’ levels and the arterial blood pressure’s levels among students with none, low or high risk was analyzed with the non-parametric Kruskal Wallis test analysis. Also, the non-parametric Mann Whitney test analysis was used between male and female.
Results
Participants’ characteristics
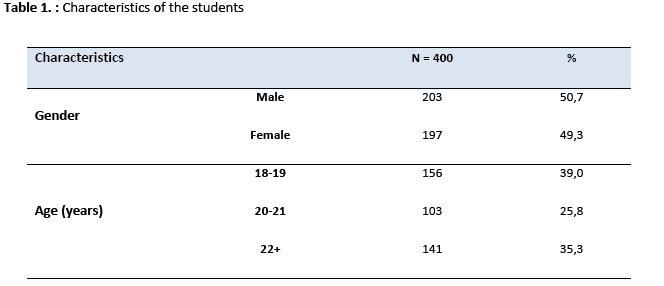
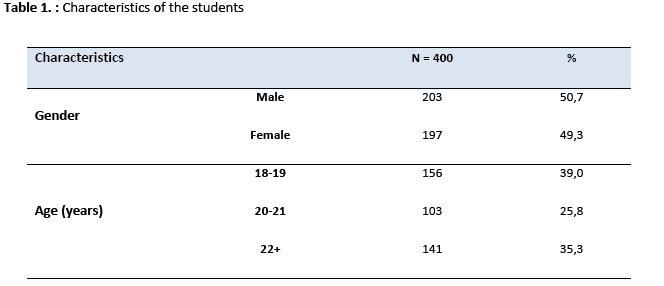
A total of 400 students were enrolled in the study. The table 1 presents the descriptive characteristics of the 400 students: 203 students (50.7%) were male and 197 (49.3%) were female. In regard to age, 39% of the students were between the age 18 and 19, 25.8% were between 20 and 21 years of age and 35.3% were over the age of 22.
Risks for obstructive sleep apnea
Of the 400 respondents, 32 (8%) reported snoring. Of those who snored, 0.3% snore very loud and 1.0% did so every day. 14 (3.5%) snorers reported that their snoring has bothered others. The presence of witnessed pauses was found in only 0.3% of persons in this group. Of those who snored, 11 individuals (2.8%) had hypertension or obesity.
Out of our total population of 400 individuals, 7 (1.8%) reported that they felt sleepy when they woke up in the morning greater than 3–4 times per week and seven (1.8%) almost every day. Seven (1.8%) said that they felt tired during waking time more than 3–4 times and seven (1.8%) almost every day. 4 students (1%) of our study population reported that they had nodded off to sleep while driving at least once in their lifetime.
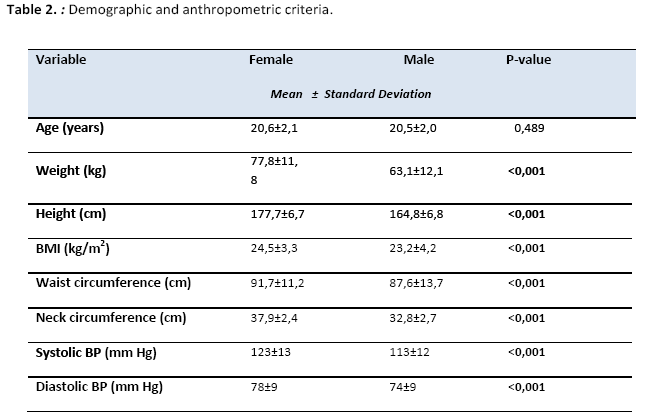
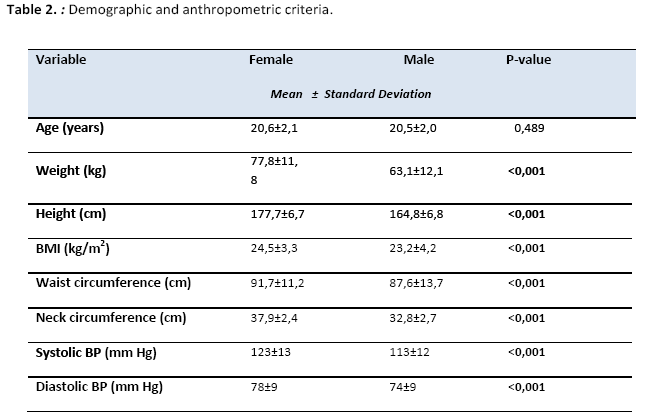
There is a statistically significant difference in somatometric measurements between male and female. The male students significantly have higher average body weight than female (77.8 vs 63.1 kg, p <0.001), BMI (24.5 vs 23.2 kg/m2, p <0.001), neck circumference, (37.9 vs 32.8 cm, p <0.001) except waist circumference to height (0.52 versus 0.53, p > 0.05).
The table 2 presents the prevalence of normal weight, overweight and obesity. There is higher percentage of female that were obese than male based on BMI (6.2% vs. 4.4%), while were fewer overweight women (18.8% vs. 27.1 %). But generally the percentage of overweight / obesity was higher among male students compared to female students (25.0% vs. 31.5%). The prevalence of high blood pressure showed statistically significantly higher percentage of male than female students. Male had higher levels of systolic or / systolic and diastolic blood pressure (4.9% vs 0.0%, p <0.002). Also, the prevalence of smoking showed that there is no statistically significant difference between male and female smokers (39.4% vs. 40.6%, p = 0.595).
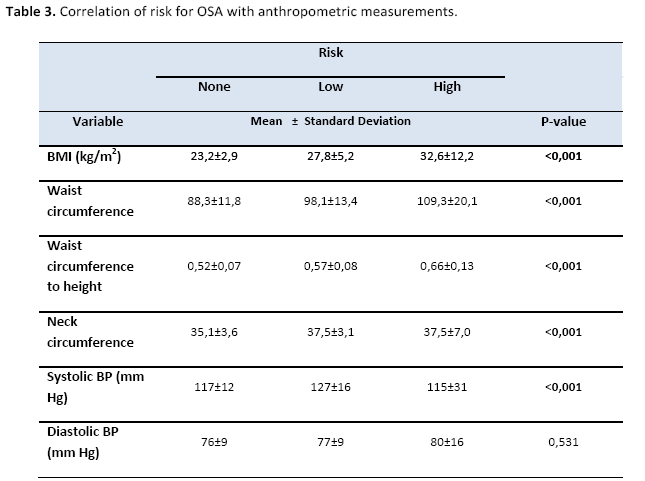
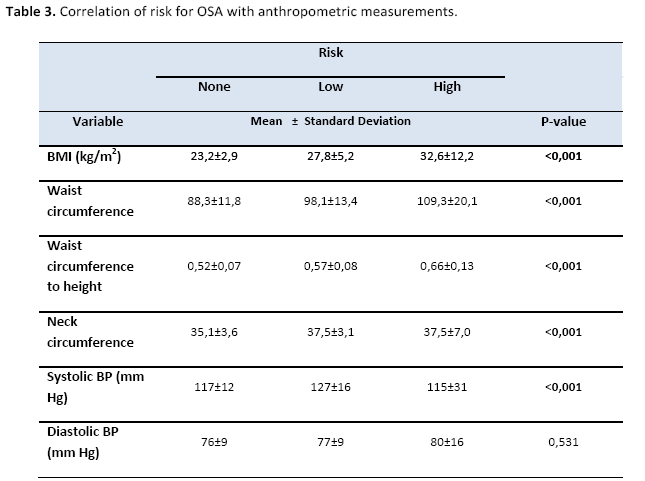
4 students (1%) found to be high risk for OSA, 48 students (12.0%) with low risk and with no risk 348 (87%). Table 3 shows the distribution of somatometriseis and arterial blood pressure of our study population based on OSA risk group. 4 students at high risk compared with those of 48 students with increased risk have statistically significant higher average levels of obesity, such as body mass index (32.6, 27.8 and 23,8 kg/m2, respectively, p <0,001), waist circumference (109.3, 98.1 and 88,3 cm, respectively, p <0,001) or neck circumference (37.1, 37.5 and 35,1 cm, respectively, p <0,001) but only lower systolic blood pressure (115 , 127 and 117 cm, respectively, p <0,001). The distribution of gender of our study population based on OSA risk group. Female was found to be high risk for OSA versus male (1.5% vs. 0.5%, p=0.040) and male was found to be low risk for OSA versus female (15.8% vs. 8.1%). It is interesting to note that in the age subgroup ' 18-19 ' years none of the respondent was found to be high risk for OSA. On the other hand, the highest proportion of high risk individuals 2.1% was found in the age group 22 and over.
Discussion
In this cross-sectional study conducted in the Technological Educational Institute of Crete we have shown that the prevalence of OSA particularly in people at high risk was found at very low frequency while those with low risk were found at very high frequency. Netzer’s study [24] compared results between the United States and Europe found that OSA prevalence in the United States was 35.8% than in Europe 26.3%. Estimates of disease prevalence worldwide are in the range of 3% to 7% in adult men and 2% to 5% in adult women [25]. In the present study, snoring, BMI, hypertension, waist circumference, waist circumference to height and neck circumference had been shown to be predictors of OSA.
In the present study, female was found to be high risk for OSA versus male and male was found to be low risk for OSA versus female. Accordingly, data supports that sleep apnea is also more prevalent among men and during sleep in the supine position [26]. Snoring and BMI were the most significantly risk factors for OSA among students. All the students with high risk for OSA have snoring in contrast to those with low risk or no risk. According to Haqqee et al., [27] showed a high prevalence of snoring and frequency of snoring with apnea. Students with high or low risk for OSA have significantly higher levels of obesity. The present study shows that the prevalence of overweight and obesity was higher in male than female students whereas, no significant difference between them. A survey showed that BMI was associated with OSA risk in Asian and Western populations [28]. In Greece, in a sample of 989 students of the Medical Faculty of the University of Crete found that the prevalence of overweight or obesity was 39.5% in male and 23.3% in female. Central obesity levels were significantly higher in men than women. Also, waist circumference, waist circumference to height and neck circumference were significantly risk factors for OSA [29]. In addition, the risk of OSA was higher in patients with large neck circumference and central obesity [30].
The prevalence of high blood pressure differed between male and female students. 1 in 20 students showed high levels of blood pressure while none of the female students of the survey had high blood pressure. A cross-sectional survey was conducted in Jordan. The findings lead to believe that low blood pressure is an additional factor affecting the low incidence of OSA [31].
Finally, the present study showed that the frequency of daytime sleepiness, smoking, the nasal congestion and the inheritance were not associated with low and/or high risk for OSA. Excessive daytime sleepiness is one of the most common symptoms in patients with OSA [32]. Nevertheless; in the present survey the daytime sleepiness is not found to be associated with the occurrence of OSA. A cross-sectional survey of 2201 high school students conducted in Canada shows that most students felt "really sleepy" during day [33]. In the present survey a high percentage of male and female were smokers. Nevertheless, the smoking is not found to be associated with the occurrence of OSA (low and high risk). Smoking is related to sleep apnea in a dose-response relationship [34]. In the present study was not found the inheritance to be associated with risk for OSA. It is not differ significantly the frequency of inheritance with no, low or high risk. The heredity has been suggested as a risk for sleep apnea, given that a number of studies have reported a significantly higher prevalence of sleep-disordered breathing in relatives of OSA patients [35]. Sudden awakenings and the respiratory problems showed to be not associated with the high risk for OSA. 25% of students with high risk for OSA had sudden awakenings and respiratory symptoms. Of those who had nasal congestion, 13.2% was with no risk for OSA, 20.8% was with low risk and 25% had high risk. Accordingly, a number of patients with OSA report waking at night with a choking sensation, which can be quite frightening and presumably reflects an episode of outright wakening during an obstructive apnea.36 However, there is no clear link between obstructive airway diseases and OSA [37].
These findings were observed despite the fact that two potential limitations were emerged. Firstly, our population was younger than most reported series, a finding that can reduce the number of the affected students. A second limitation was that most of the subject information was self-reports that might be affected by misclassification, incomplete information.
Conclusions
The prevalence of OSA particularly in people at high risk was found at very low frequency while those with low risk were found at very high frequency. Our data suggests that snoring and a higher BMI constitutes strong predictors of OSA followed by hypertension and obesity. Although OSA prevalence rates were not alarming, the continuous increase of BMI, central obesity, snoring and hypertension may increase the rates in the next years. Advisory and education are considered important for primary care nurses and general practitioners regarding this common and potentially serious syndrome. Students at high risk for OSA should be referred for further treatment and assessment of respiratory function.
2622
References
- Cheyne J. A case of apoplexy, in which the fleshy part of the heart was converted into fat. Dublin Hospital Rep 1818; 2:216–223.
- Scientific informations of the Greek Medical Society of Obesity. Obesity and apnea-hypopneas Sleep syndrome. Advances in Obesity 2007;15(4):4-5.
- The report of an American Academy of Sleep Medicine Task Force: Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. Sleep 1999; 22: 667–689.
- Amra B. Prevalence of sleep apnea-related symptoms in a Persian population. Sleep Breath 2011; 15(3):425–429.
- Khassawneh B. Symptoms and risk of obstructive sleep apnea in primary care patients in Jordan. Sleep Breath 2009; 13(3):227-32.
- Block A, Boysen P, Wynne J, Hunt L. Sleep apnea, hypopnea and oxygen desaturation in normal subjects: a strong male predominance. N Engl J Med 1979; 300(10):513–517.
- Guilleminault C, Eldridge F, Dement W. Insomnia with sleep apnea: a new syndrome. Science 1973; 181(4102):856–85.
- Ip M, Lam B, Tang L, Lauder I, Lauder I, Ip T. A community study of sleep-disordered breathing in middle-aged Chinese men in Hong Kong.Chest 2001; 119(1):62–69.
- Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badur S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 1993; 328(17):1230-5.
- Smith P. Weight loss in mildly to moderately obese patients with obstructive sleep apnea. Ann Intern Med 1985; 103(6)part 1:850-5.
- Fujita S, Conway W, Zorick J. Evaluation of the effectiveness of uvulopalato-pharyngoplasty. Laryngoscope 1985; 95(1):70-4.
- O'Sullivan R, Hillman D, Pantin R, Finucane K. Mandibular advancement splint: an appliance to treat snoring and obstructive sleep apnea. Am J Respir Crit Care Med 1995; 151(1):194-8.
- Sullivan C, Issa F, Berthon-Jones M, Eves L. Reversal of obstructive sleep apnea by continuous positive airway pressure applied through the nares. Lancet 1981; 18:1(8225):862-5.
- Alkhalil M, Schulman E, Getsy J. Obstructive Sleep Apnea Syndrome and Asthma. J Clin Sleep Med 2009; 5(1):71–78.
- Young T, Evans L, Finn L, Palta M. Estimation of the clinically diagnosed proportion of sleep apnea syndrome in middle-aged men and women. Sleep 1997; 20(9):705–6.
- Nakano H, Furukawa T, Nishima S. Relationship between Snoring Sound Intensity and Sleepiness in Patients with Obstructive Sleep Apnea. J Clin Sleep Med 2008; 4(6): 551–556.
- Bouscoulet L, Vázquez-García J, Muiño A, Márquez M, López M, Montes de Oca M. Prevalence of Sleep Related Symptoms in Four Latin American Cities. J Clin Sleep Med 2008; 4(6):579–585.
- Koehler U. Daytime sleepiness in patients with Obstructive Sleep Apnoea (OSA) - pathogenetic factors. Pneumologie 2010; 65(3):137-42.
- Peppard P, Young T, Palta M, Sktarud J. Prospective study of the association between sleep-disordered breathing and hypertension 2000. N Engl J Med, 2000; 342(19):1378–1384.
- Pepperell J. Ambulatory blood pressure after therapeutic and subtherapeutic nasal continuous positive airway pressure for obstructive sleep apnoea: a randomized parallel trial. Lancet 2002; 359(9302):204–210.
- Nena E, Steiropoulos, P, Tsara V. The sleep apnea syndrome as a risk factor for traffic accidents. Archives of Greek Medicine 2010; 27(1):18-130.
- Sjösten N, Kivimäki M, Oksanen T. Obstructive sleep apnoea syndrome as a predictor of work disability. Respir Med 2009; 103(7):1047-1055.
- Tregear S, Reston J, Schoelles K, Phillips B. Continuous positive airway pressure reduces risk of motor vehicle crash among drivers with obstructive sleep apnea. SLEEP 2010; 33(10):1373-1380.
- Netzer C, Hoegel J, Loube D, Netzer M, Hay B, Alvarez-Sala R. Sleep in Primary Care International Study Group. Prevalence of symptoms and risk of sleep apnea in primary care. Chest 2003; 124(4):1406-14.
- Punjabi N. Obstructive Sleep Apnea:The Epidemiology of Adult Obstructive Sleep Apnea Proc Am Thorac Soc 2008; 5(2):136-143.
- Shelton K, Woodson H, Gay S, Suratt P. Pharyngeal fat in obstructive sleep apnea. Am Rev Respir Dis 1993; 148(2):462-6.
- Haqqee R, Hussain S, Mujib M, Ahmad H. A hospital based preliminary report on sleep disordered breathing in Pakistani population. J Ayub Med Coll Abbottabad 2002; 14(3):2-4.
- Ip M. A community study of sleep-disordered breathing in middle-aged Chinese women in Hong Kong: prevalence and gender differences. Chest 2004; 125(1):127–134.
- Bertsias G, Mammas I, Linardakis M, Kafatos A. Overweight and obesity in relation to cardiovascular disease risk factors among medical students in Crete, Greece. BMC Public Health 2003; 3:3.
- Bouscoulet L, Vázquez-García J, Muiño A, Márquez M, López M, Montes de Oca M. Prevalence of Sleep Related Symptoms in Four Latin American Cities. J Clin Sleep Med 2008; 4(6):579–585.
- Khassawneh B. Symptoms and risk of obstructive sleep apnea in primary care patients in Jordan. Sleep Breath 2009; 13(3):227-32.