Research - (2022) Volume 13, Issue 2
The Prevalence of Vitamin D Deficiency in Migraine Headache Patients & its Response to Vitamin D Replacement in Deficient Patients
Sumirini Puppala1*,
TR Sirohi2 and
Abhijit Acharya3
1Department of Neurology, SOA IMS & SUM Hospital, Bhubaneswar, Odisha, India
2Department of Medicine, Swami Vivekananda Subharti University, Meerut, Uttar Pradesh, India
3Department of Neurosurgery, SOA IMS & SUM Hospital, Bhubaneswar, Odisha, India
*Correspondence:
Sumirini Puppala, Department of Neurology, SOA IMS & SUM Hospital, Bhubaneswar, Odisha,
India,
Tel: +8054871861,
Email:
Received: 19-Jan-2022, Manuscript No. ipjnn-22-12348;
Editor assigned: 21-Jan-2022, Pre QC No. P-12348;
Reviewed: 18-Feb-2022, QC No. Q-12348;
Revised: 22-Feb-2022, Manuscript No. R-12348;
Published:
01-Mar-2022
Abstract
Migraine is a common neurovascular disorder that causes significant morbidity, in terms of quality of life. The migraine syndrome consists of a moderate to severe recurrent, unilateral, throbbing headache lasting hours to days, which is generally accompanied by nausea, photophobia, phonophobia, and is worsened by routine physical exertion. A few studies have shown a positive relationship between vitamin D and migraine headaches. And, it is common to encounter migraine headache and low levels of vitamin D in Indian population suggesting a common link between them. This article is a study of prevalence of vitamin D deficiency in migraine headache patients amongst the north Indian population, to assess & correlate vitamin D levels with the severity of migraine headache, to study the effect of supplementation of vitamin D in patients of migraine with vitamin D deficiency.
Keywords
Headache; Migraine; Vitamin D Deficiency
Introduction
Derived from the Greek word “ημικρανία” (hemikrania), Migraine
means ‘pain on one side of the head’. Migraine is a common
neurovascular disorder with instability in the way the brain
is dealing with the sensory information that is incoming. The
Migraine syndrome consists of a moderate to severe recurrent,
unilateral, throbbing headache lasting hours to days, which is
generally accompanied by nausea, photophobia, phonophobia
and is worsened by routine physical exertion [1]. This sensory
sensitivity is said to be due to dysfunction of monoaminergic
sensory control systems, particularly CGRP, 5-Hydroxytryptamine
and Dopamine. In recent years, many studies have highlighted the
role of vitamin D levels in development of various diseases. Vitamin
D is a steroid which not just has its role in calcium homeostasis
and bone health but possesses apoptotic, anti-inflammatory and
immunomodulatory properties [2]. Vitamin D is also needed in
serotonin synthesis. As increase in serotonin decreases CGRP
levels, it is common to encounter migraine headache and low
levels of vitamin D in Indian population suggesting that there
may be a common link between the two diseases [3]. A study
was conducted by our department in Chhatrapati Shivaji Subharti
Hospital, Meerut to assess the correlation of serum vitamin D
level with the clinical severity & duration for each patient.
Methodology
50 patients diagnosed to be suffering from migraine as per IHS (International Headache Society) guidelines were selected for inclusion in the study. Thus, study population consisted of 100 patients, 50 age and sex matched healthy individuals with similar socio-economic status were taken as controls [4]. Detailed history and examination was carried out in all the patients. Serum vitamin D levels were done in all the cases and controls.
Statistical methods used
Quantitative data was presented as mean ± SD or median and inter-quartile range, as appropriate. Normality of quantitative data was checked by measures of Kolmogorov Smirnov tests of normality. For categorical variables number & percentages were calculated. Frequency of migraine headache was presented as median and interquartile range. For two groups cases & control continuous variables were compared using Mann Whitney U test. Comparisons of continuous variables between three groups of Vitamin D were done by One-Way ANOVA followed by Post- Hoc Multiple comparisons or Kruskal Wallis test. For all patients vitamin D levels were done & prevalence of deficient patients was calculated. Chi-square test or Fisher’s exact test was applied for categorical data. Multinomial regression was carried out to find the independent predictors of headache days (divided into categories). All calculations were two side & performed using SPSS version 17 (Statistical Packages for Social Sciences, Chicago). A P value of <0.05 was considered to indicate statistical significance.
Observation
The mean (± SD) age of study group was 27.7 ± 1.00 years, while in the control group it was 32.52 ± 1.52 years. In the study group, 13 (26%) patients were men and 37 (74%) patients were women, 30 (60%) patients were <30 years of age and 20 (40%) patients were >30 years of age. The control group included 29 women (58%) and 21 men (42%). 20 (40%) controls were <30 years of age and 60 (65.5%) were >30 years of age. The mean duration of headache in our study population was 73.96 ± 1.30 months. For purpose of analysis, study group was further subdivided as per duration of headache into 3 groups. 28 (56%) patients were symptomatic for < 60 months. 16 (32%) were symptomatic for 60-120 months whereas 6 (12%) were symptomatic for > 120 months. Severity of pain was assessed in entire study group as per 0 to 10 numeric pain rating scale. 16 (32 %) patients had pain severity score < 5 while 34 (68 %) patients had pain severity score > 5 (Table 1).
| Parameters |
Value |
| Duration of Headache (mean ± SD) |
73.96 ± 1.30 |
| No. of patients with duration < 60 months |
28 (56%) |
| No. of patients with duration 60-120 months |
16 (32%) |
| No. of patients with duration >120 months |
06 (12%) |
| Mean Duration of Headache |
| No. of patients with headache attack <4 hours |
15 (30%) |
| No. of patients with headache attack 4-72 hours |
34 (68%) |
| No. of patients with headache attack >72 hours |
01 (02%) |
| Location of Headache |
| Holocranial |
18 (36%) |
| Unilateral |
28 (56%) |
| Frontal |
04 (08%) |
| Character of Headache |
| Throbbing |
40 (80%) |
| Pulsatile |
10 (20%) |
| Associated Symptoms |
| Nausea |
39 (78%) |
| Vomiting |
24 (48%) |
| Photophobia |
36 (72%) |
| Phonophobia |
44 (88%) |
| Aura |
07 (14%) |
Table 1 The clinical characteristics of the study population.
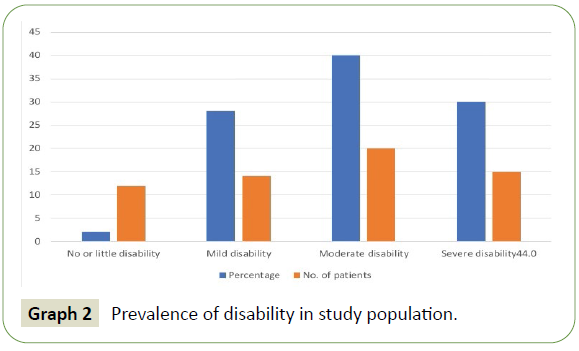
The degree of disability was assessed in study population according to MIDAS questionnaire based on this score into subgroups: Little or no disability, mild, moderate and severe disability. 1 (2%) of patients had little or no disability, 14 (28%) had mild, 20 (40%) had moderate and 15 (30%) patients had severe disability. We carried out vitamin D levels in all the cases and controls. Mean ± SD levels of vitamin D was 16.97 ± 1.03 ng/ ml in study group, while in control group levels were 21.26 ± 1.9 ng/ml . The subjects with vitamin D levels ≤ 20 mg/ml and were classified as ‘deficient’, subjects with vitamin D levels between 20-29 ng/ml were classified as ‘insufficient’ and subjects with vitamin D levels more than 30 ng/ml were named as ‘sufficient’. In the study group, 38 (76%) patients were found to be deficient in vitamin D, 08 (16%) were insufficient and 04 (08%) were found to have sufficient levels of vitamin D. In control group 18 (36%) patients were found to be deficient in vitamin D, 20 (40%) were insufficient and 12 (24%) were found to have sufficient levels of vitamin D.
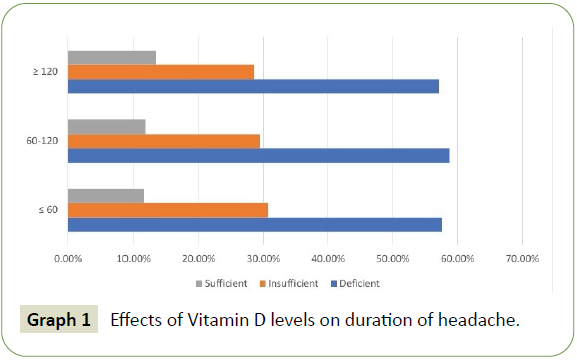
Among the migraine headache patients, 26 (52%) had headache duration of <60 months, out of which 15 (57.6%) had deficient, 08 (30.8%) had insufficient and 3 (11.6 %) had sufficient levels of vitamin D. In group with 60-120 months duration [n=17 (34%)], we had 10 (58.8%) patients with deficient, 05 (29.4%) with insufficient and 02 (11.8%) with sufficient levels of vitamin D. Among the headache patients with duration > 120 months [n= 07 (14%)], 4 (57.1%) had deficient levels, 02 (28.6%) had insufficient levels, and 01 (14.3%) had sufficient levels of vitamin D. Among the patients with migraine attack of <4 hours duration (n=21), 10 (47.6%), 07 (33.3%) and 04 (19.1%) had deficient, insufficient and sufficient vitamin D levels respectively. Among the patients with duration of attack ranging from 4-72 hours (n=28), 16 (57.1%), 8 (28.6%) and 04 (14.3%) had deficient, insufficient and sufficient vitamin D levels, respectively. The only patient with duration of attack >72 hours group had deficient vitamin D levels respectively. Relation between levels of vitamin and associated symptom of migraine was also studied. Out of 50 patients in study group, 39 had nausea, 24 had vomiting, 36 had photophobia, 44 had phonophobia and 07 had aura (Graphs 1 and 2).
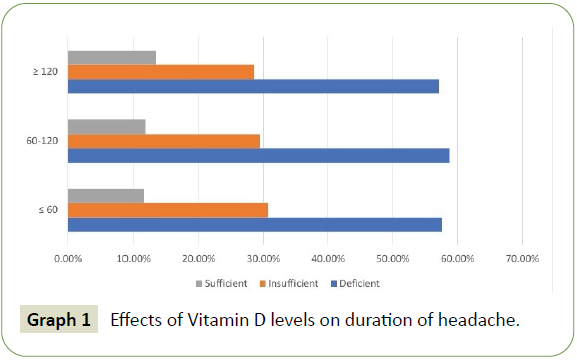
Graph 1: Effects of Vitamin D levels on duration of headache.
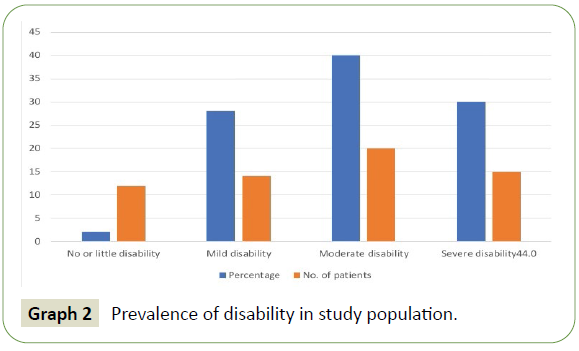
Graph 2: Prevalence of disability in study population.
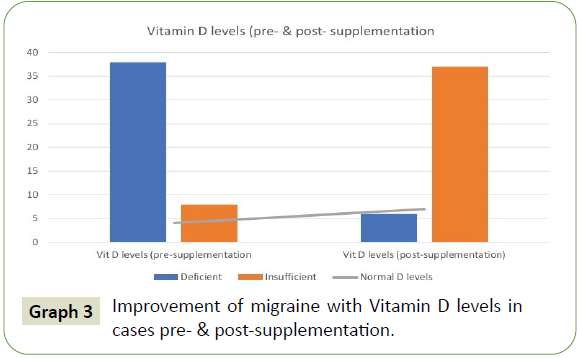
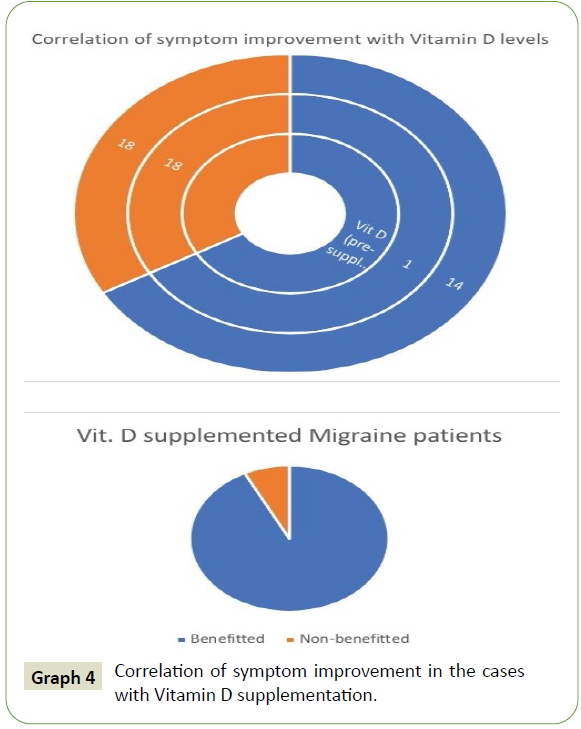
The patients, who were followed up, after Vitamin D supplementation, were included in the study, following compliance ensured verbally. Supplementation was done via injectable as well as oral routes, accordingly. A minimum of 4 weeks and maximum of 8 weeks of supplementation was ensured, before re-sampling of the patient (Graphs 3 and 4).
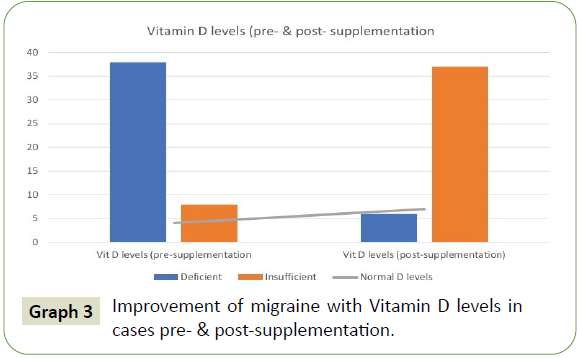
Graph 3: Improvement of migraine with Vitamin D levels in cases pre- & post-supplementation.
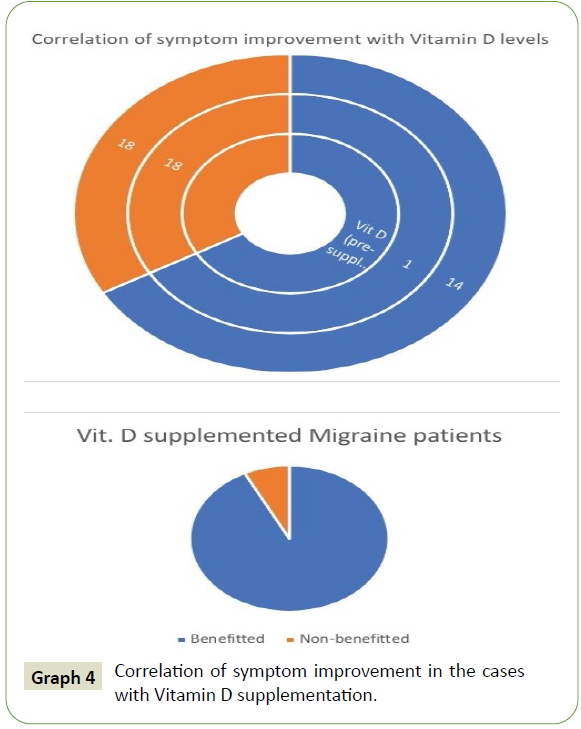
Graph 4: Correlation of symptom improvement in the cases with Vitamin D supplementation.
Results
Females formed a majority in our study, and most of the patients
were in the age group of less than 30 years of age. More than
half the patients had migraine for less than past 60 months of
duration, and very low members had the headache for more
than 120 months. Majority of the patients had the pain lasting
between 4-72 hours. More than half the patients complained
of headache unilaterally. Almost all the patients complained of
throbbing headache, with vast majority having accompanying
nausea, vomiting, phonophobia followed by photophobia in
more than half the patients. Very few patients complained of
aura. Majority of patients having headache had <30 headache
days in the past 3 months. Vast majority of patients had a pain
severity score of more than 5. Majority of patients had headache
leading to moderate to severe disability. Majority of patients
in the study group are vitamin D deficient or insufficient, but a lesser majority of the same in the control group. Females were
found to be more deficient in Vitamin D, in both study and control
groups. In patients whose history of headache were less than 60
months or between 60 to 120 months or more than 120 months
– in all the cases, majority of patients were found to be vitamin
D deficient. In patients studied having duration of headache
less than 4 hours, half the patients were vitamin D deficient. In
patients having headache of duration between 4-72 hours or
more, majority had vitamin D deficiency and insufficiency.
Most of the patients who were followed up, had improved Vitamin D levels. Follow up of Vitamin D deficient migraine patients was
done minimum after 4 weeks of supplementation. More than
three-quarters of the patients with improved Vitamin D levels,
had significant improvement in migraine symptoms, as qualified
by MIDAS questionnaire, following supplementation. Hence, in
our study, the correlation of deficient serum vitamin D level was
positively significant with the prevalence & severity of migraine.
Conclusion
In our study, the correlation of serum vitamin D level was
significant with prevalence of migraine. We found that there
is a positive correlation between lower serum vitamin D levels
and severity & duration of migraine. Lower vitamin D levels
were found in more severe migraine. Vitamin D deficient and
insufficient patients, were more prone to develop migraine.
So, serum vitamin D levels can be used to assess the proneness,
severity and duration of migraine & can also be an important
predicator of clinical outcome in migraine. Patients with improved
Vitamin D levels, had significant improvement in migraine
symptoms, as qualified by MIDAS questionnaire, following
supplementation. Hence, the vitamin D levels correlated well with
the incidence of migraine during the hospital visit, suggesting
that the serum vitamin D levels was an indicator of the clinical
outcome of the patients during their hospital visit.
REFERENCES
- Rasmussen BK, Olesen J (1992) Migraine with aura and migraine without aura: an epidemiological study. Cephalalgia 12: 221-228.
Google Scholar, Crossref, Indexed at
- Olesen J (1993) Migraine with aura and its subforms. In the Headaches. Olesen J. Hansen P. Welch KMA (editors), New York. Raven Press; pp: 263-275.
- Tovner LJ, Hagen K, Jensen R, Katsarava Z, Lipton R, et al. (2007) The global burden of headache: a documentation of headache prevalence and disability worldwide. Cephalalgia 27: 193-210.
Google Scholar, Crossref, Indexed at
- Wang SJ (2003) Epidemiology of migraine and other types of headache in Asia. Curr Neural Neurosci Rep 3: 104-108.
Google Scholar, Crossref
Citation: Puppala S, Sirohi TR, Acharya A (2022) The Prevalence of Vitamin D Deficiency in Migraine Headache Patients & its Response to Vitamin D Replacement in Deficient Patients. J Neurol Neurosci Vol.13 No.2:410.