Research Article - (2022) Volume 10, Issue 1
The Survival Of Patients With triple Negative Breast Cancer With Chemotherapy Along With Lifestyle Change Interventions In Survivors
Adiguel Usman*
Department of Internal Medicine, Kermanshah University of Medical Sciences, Kermanshah, Iran
*Correspondence:
Adiguel Usman, Department of Internal Medicine,
Kermanshah University of Medical Sciences, Kermanshah,
Iran,
Tel: 9181313925,
Email:
Received: 18-Feb-2022, Manuscript No. IPACR-22-11447;
, Pre QC No. IPACR-22-11447(PQ);
Reviewed: 07-Mar-2022, QC No. IPACR-22-11447;
Revised: 11-Mar-2022, Manuscript No. IPACR-22-11447(R);
Published:
18-Mar-2022, DOI: 10.36648/2254-6081.22.10.117
Abstract
Background: The present study was conducted to examine
the survival of patients with triple negative breast cancer
subtype undergoing current chemotherapy and along with
implanting weight management, physical activity and diet in
breast cancer survivorship.
Patients and methods: The present study was conducted on
110 patients admitted to the oncology clinics of Talaghani
Hospital of Kermanshah University of Medical science
between October 2009 and July 2018. Patients started 5
chemotherapy cycles, including docetaxel, epirubicin and
cyclophosphamide once every 21 days, and then two cycles
of epirubicin and cyclophosphamide, ending with
fluorouracil. Also recommend patients for physical exercise,
diet and lifestyle change.
Results: The median and mean follow-up was 52.3 and 45.6
months respectively. 8 patients were metastatic and 103
were under adjuvant therapy, 13 of whom had relapses.
Median relapse-free survival and mean overall survival were
44.4 months and 49.2 months, in respective order of the
total of 110 patients, 20 died and 90 still live.
Conclusion: Along with recommendations for physical
exercise, diet and lifestyle change, combination
chemotherapy increases hopes for a better response to
treatment and a reduction in the rate of relapse during the
first three years.
Keywords
Triple negative breast cancer; Current
chemotherapy; Physical exercise; Diet and lifestyle change
Introduction
It is estimated that in 2019 in United State, 268,600 new cases
of breast cancer will occur in women and making it the most
common cancer after skin cancer in women [1]. A number of risk
factors for breast cancer that can be mentioned include: getting
older, genetic mutations, reproductive history, having dense
breasts, family history of breast cancer that these things cannot
be changed. A number of risk factors can be changed, for
example: not being physically active, being overweight or obese
after menopause, taking hormones. However, BRCA and BRCA-1 gene mutations, on chromosomes 17 and 13, account for 5% to
10% of all women with breast cancer [2-3]. Classi ication of
breast cancer based of the histological pro iling into the
following ive distinct subtypes provide insight into therapeutic
strategies: luminal A; IHC and histology this subtype includes
tumors that are estrogen and progesterone receptor positive,
HER-2 negative and have a low-grade histology, luminal B; this
type includes tumors that are estrogen receptor and HER-2
positive, progesterone receptor negative in IHC and higher grade
in histology compared to those with Luminal A, Luminal B are
likely to bene it from chemotherapy and hormone therapy a ter
of end chemotherapy and herceptin therapy, HER-2 positive; this
type includes tumors that based IHC are progesterone receptor
and estrogen receptor negative, but HER-2 positive, Basal-like;
this type, which is also called Triple-Negative Breast Cancer
(TNBC), includes tumors that are ER, PR and HER-2 negative and
accounts for 10-15% of breast cancers [4]. And are associated
with an unfavorable prognosis [5]. It is more common among
younger women, African-American and Hispanic women and
who carry a germ line mutation of the BRCA-1 gene [6]. The
target population of the present study consisted of patients with
triple negative breast cancer subtype undergoing chemotherapy
with conventional drugs including docetaxel, epirubicin,
cyclophosphamide and luorouracil. To reduce the effects of
certain factors with an adverse effect on the prognosis of breast
cancer, patients were given a series of advices. Major factors
involved in breast cancer prognosis include diet (for instance,
food low in vitamin D, prepared at high temperatures, such as
barbecues, high in fat and sugar and low in vegetables), physical
exercise (low levels of it have an adverse effect) and lifestyle
(patients were recommended to change their sedentary lifestyle
into an active one) [7]. The present study aimed to assess
patients' responsiveness to treatments and overall survival and
the effects of Ki67 and P53 on relapse-free survival and overall
survival of patients.
Materials and Methods
We have entered the study 110 consecutively patients with TNBC from October 2009 until July 2018 at oncology clinics of Kermanshah University of Medical Science (KUMS). These centers are referral centers for patients from Kurdistan, Elam, Lorestan, and Hamadan provinces in IRAN. They were followed from the time of diagnosis to the time of recurrence, then to follow-up to death. The established histomorphological factors patients with TNBC such as pathological tumor size, tumor type, nodal status and hormonal receptor and HER-2 status were identified from the database of the department of Pathology of KUMS and from the documentation in the patients' file. Tumors were classified as IHC stains score 0 if no membrane staining or incomplete faint membrane staining less than ≤ 10% of invasive tumor cells was observed, an IHC score 1+ if an incomplete faint membrane staining was detected in more than 10% of invasive tumor cells, an IHC score 2+ if weak or incomplete circumferential membrane staining was observed in more than 10% of invasive tumor cells and complete and circumferential membrane staining that is intense and within ≤ 10% of invasive tumor cells. For establish patient with score 2 in IHC recommends Fluorescence in Situ Hybridization (FISH). In IHC with score 3+ tumor displays complete, intense circumferential membranous staining in more than 10% of tumors cells. The cells were stained for Ki67 and P53. Patients underwent 5 chemotherapy cycles, including docetaxel 80mg/m2, epirubicin 80 mg/m2 and cy clophosphamide 500 mg /m 2 once every 21 days with G-CSF support, and then two cycles of epirubicin 90 mg/m2 and cyclophosphamide 600 mg/m2 and 5-fluorouracil 600 mg/m 2 with G-CSF support. Over the 21-day period, all patients were monitored for treatment complications, particularly for fever and febrile neutropenia, and were hospitalized if necessary. After completing the 7 chemotherapy cycles, qualified patients were referred for radiotherapy and then checked at regular intervals of 3 months up to a year, and afterwards every 6 months, for potential relapses, and were also reminded of the advices previously given regarding interferences with Lifestyle that could have a potentially negative effect on prognosis and assessed on their compliance with the advices. The following are recommended to patients: Attain and maintain an ideal weight throughout life. Especially for those who are overweight or obese, limit consumption of high calories foods. Participate in in regular physical activity. Be as thin as possible throughout life don't be under ideal weight. Adults should participate in in at least exercise 360 min/weak or vigorous intensity activity at least 4 day/week, or a combination of both during the week. Eat a diet rich in whole grains and high in vegetable. Limit consumption of fast foods, sugar-sweetened drinks, red and processed meat. Avoid smoking and other exposure to tobacco [8].
Results
Patients' mean age was 55.3 years and their median follow-up
was 52.3 months with 95% between 39.1 months and 65.4
months. Their mean follow-up was 45.6 months with 95%
between 45.6 months and 55.3 months.108 patients were
female (98.2%) and 2 (1.8%) were male. In 57 of the patients
(50.4%), the tumor was on the right side, and in 53 (49.6%), on
the left. At the time of diagnosis, 8 patients showed evidence of
metastasis, with 3 cases in the bone, 4 cases in the liver and 1
case in the lung. Out of the 110 patients, 51 met the criteria for
radiotherapy and underwent the procedure. Paget's disease was
observed in 5 patients. Invasive ductal-lobular carcinoma was
observed in only 2 patients. IHC for P53 was performed on 99 out of the 110 patients, but failed for 11 due to technical
problems, and out of the remaining 99 patients, P53 staining
was negative in 53 and positive in 44. IHC staining for Ki67 was
performed on 52 patients only and not on 57 patients because
failed due to technical problems.
Levels above 10% (the cut-off point) were considered
positive. 38 patients (73%) came out positive from the
staining and 14 came out negative. Patients' staging was based
on the ACC system: Stage I: 6 patients (6.9%); stage IIA: 25
patients (22.5%); stage IIB: 35 patients (31.5%); stage IIIA: 31
patients (27.9%); stage IIIB: 2 patients (1.8%); stage IIIC: 3
patients (2.7%); and stage IV: 8 patients (7.2%).
Patients were also grouped based on their age: 22 (20%) in
the 25-35 age group, 41 (37.27%) in the 35-45 age group, 32
(28.8%) in the 46-55 age group and 15 (13.5%) in the over-56
age group. Mean relapse time was 33.3 months (10 months at
minimum and 62 months at maximum). Median relapse time
was 30 months, and in 95% of the patients, relapse occurred
from month 10.3 to month 61.8. During the follow-up of
patients in stages 1,2 and 3 (total of 103 out of 110), relapse
occurred in 13 patients, of which 4 cases had it in the bone, 2 in
the brain, 2 in the lung and 5 in the liver 4 of the 103 patients
(3.6%) experienced local relapse at the site of surgery. Of the
103 patients, 86 (83%) did not experience relapses. Of the 8
patients with metastasis (stage 4), 7 died and one with lung
metastasis is in remission.
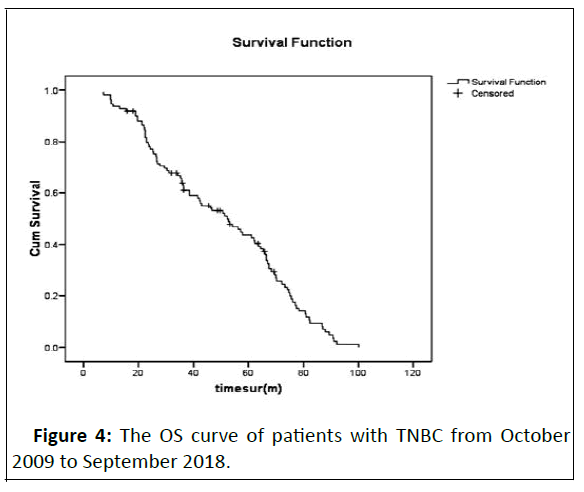
Ultimately, 20 patients died and 90 still live. One relapsed
case of pulmonary metastasis recovered and still lives. At the
end of the statistical analysis phase, one other patient
experienced brain and bone metastases and is currently
receiving treatments and was excluded from the statistical
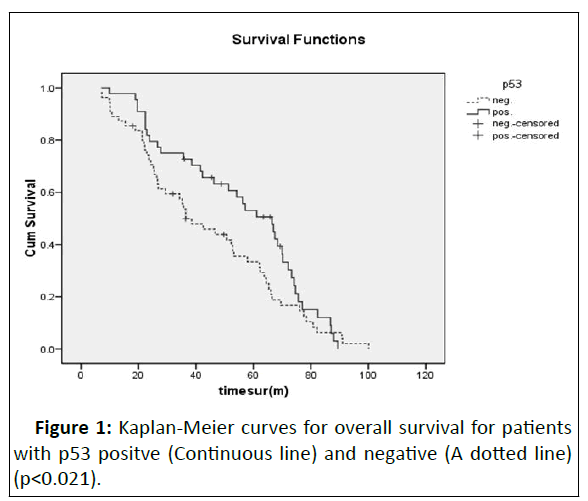
analyses. The relationship between overall survival and P53
was assessed. Overall survival for P53-positive patients was
about 35.3 months (mean OS was 55.72 months and
median OS 66.5 months).
Overall survival for P53-negative patients was 64.2
months (mean OS was 44.28 months and median OS 36.4
months). 8 patients relapsed in the P53-positive group and 2
relapsed in the P53-negative group. Survival was more
favorable in the negative group (p=0.021) (Figure 1). The
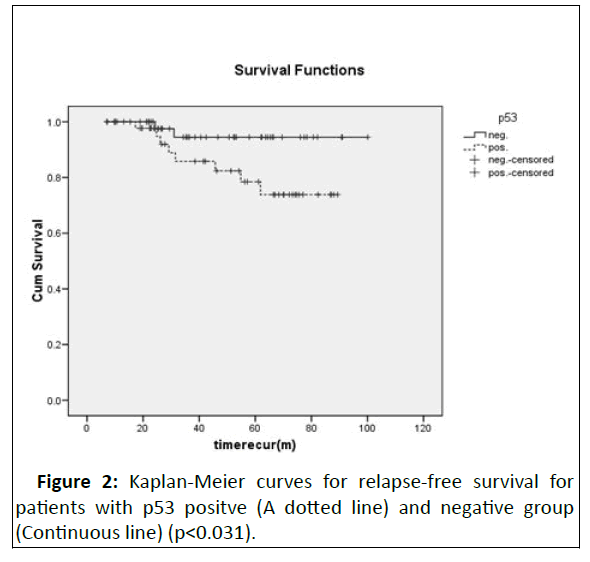
relationship between DFS and P53 was also assessed, and the
mean DFS in the P53-negative group was 96.1% and 76.3% in
the P53-positive group, suggesting a more favorable status in
the P53-negative group (Figure 2).
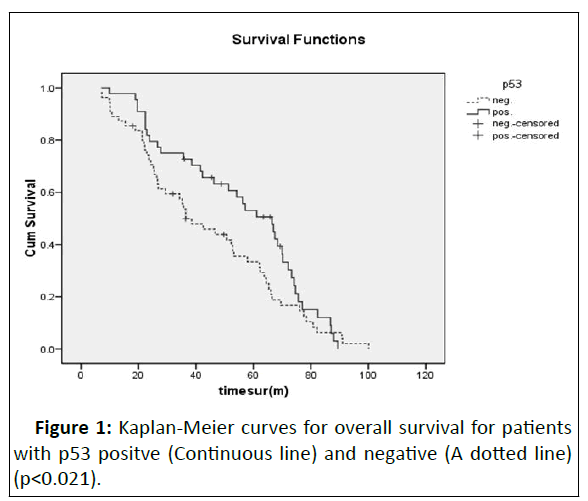
Figure 1: Kaplan-Meier curves for overall survival for patients
with p53 positve (Continuous line) and negative (A dotted line)
(p<0.021).
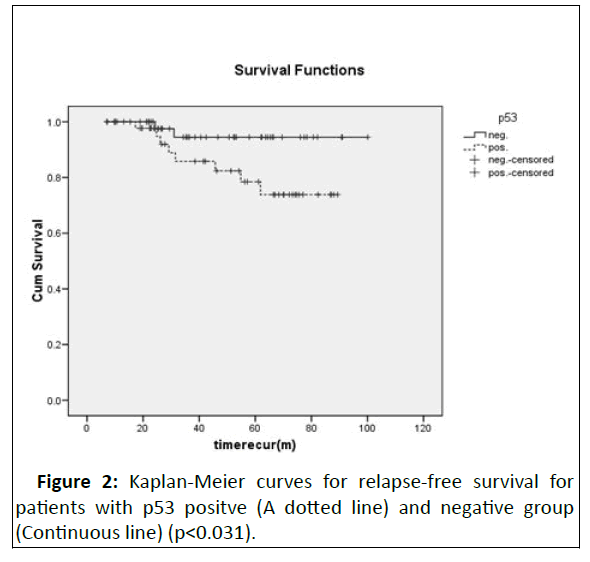
Figure 2: Kaplan-Meier curves for relapse-free survival for
patients with p53 positve (A dotted line) and negative group
(Continuous line) (p<0.031).
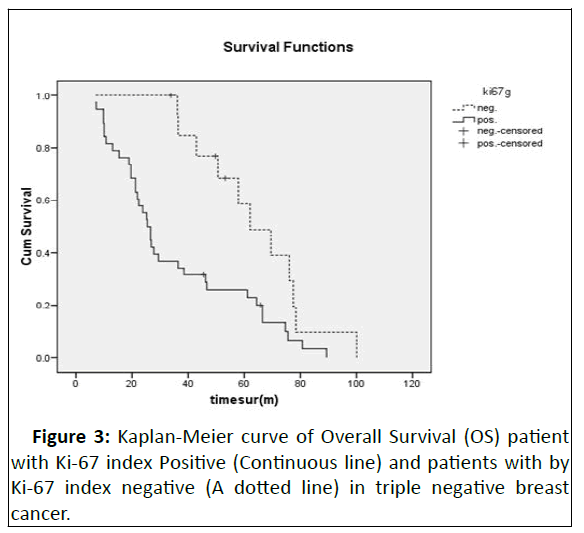
Fifty-two patients were assessed in terms of Ki67, 14 of who
turned out negative and 38 positive. In the Ki-67-positive group,
2 of the total of 38 patients relapsed and ultimately died, and in
the Ki-67-negative group, 3 of the total of 14 patients' relapsed
and ultimately 3 patients of this group died.
The relationship between DFS and overall survival was
assessed. In the Ki-67-negative group, the mean OS was
64.152 months and the median OS was 62.067 months. In
the Ki-67-positive group, the mean DFS was 35.25 months and
the median DFS 25.43 months; however, the relationship
was not statistically significant (p=0.33)(Figure 3).
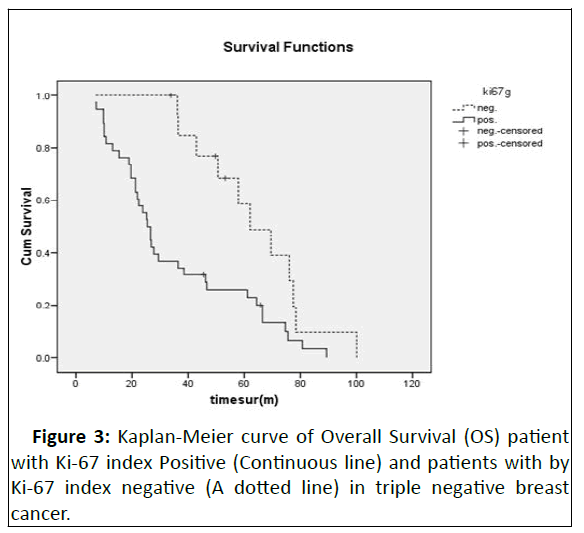
Figure 3: Kaplan-Meier curve of Overall Survival (OS) patient
with Ki-67 index Positive (Continuous line) and patients with by
Ki-67 index negative (A dotted line) in triple negative breast
cancer.
The relationship between Ki-67 and relapse was
assessed. Relapse occurred in 2 patients from the Ki-67-positive
group and 2 from the Ki-67-negative group; however, the
relationship was not significant (p=0.201).
A total of 5 patients died, 2 of whom belonged to the Ki-67-
negative group and 3 to the Ki-67-positive group; however, this
relationship was not significant (p=0.11).
The overall survival total patients are shown in
Survival outcomes in all patients (110 patients) are shown in Figure 4.
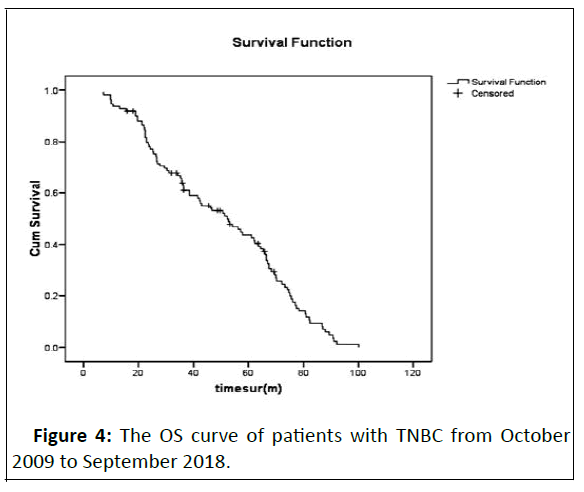
Figure 4: The OS curve of patients with TNBC from October
2009 to September 2018.
Discussion
A relative improvement can be noticed in the disease
outcome of patients with Triple Negative Breast Cancer (TNBC)
within the past 20 years [9]. These patients appear to benefit
from chemotherapy and, despite the advances in the treatment
of breast cancer and the emergence of biological and target
therapy techniques, chemotherapy regimens with standard
factors are still the frontline treatment for them. Although
women with TNBC often enter a period of remission in response
to chemotherapy, they often take an aggressive form, and the
likelihood of relapse and death due to the disease is higher in
the first 3 years following diagnosis compared to that in the
other subtypes of breast cancer. After this period, the risk of
relapse is reduced rather significantly compared to the PR and
ER-positive subtypes. Patients with TNBC appear to be different from the other subtypes in terms of the presentation and
expression of certain receptors. For instance, the expression of
Ki-67 and P53 receptors is high at the tumor level, which
comprises poor prognostic factors in breast cancer. Ki-67
overexpression is likely associated with a larger tumor size and
the involvement of axillary lymph nodes [10,11]. Juny Su et al
[10] showed that Ki67 can be an independent prognostic factor
for DFS or OS rates in early-stage breast cancer patients. Breast
cancer with high Ki-67expression responds better to
chemotherapy but visceral recurrence is high during follow-up
[12-13]. In the present study, patients received advice on
increasing their physical exercise and changing their lifestyle
from a sedentary one to an active one. Many epidemiologic
studies show that post-diagnosis exercise may associate with
improved OS among women with TNBC [14]. The American
Cancer Society and the National Comprehensive Cancer Network
has a number of dietary recommendations and weight and
physical activity adjustments in cancer patients along with other
recommendations [15-16]. Many studies suggest that a healthy
lifestyle may reduce the risk of breast cancer and better breast
cancer prognosis [17]. Evidence suggests that physical activity
and weight management has a role in breast cancer prevention
and can improve survival in patient with breast cancer and
vigorous activity can even reduce the risk of relapse in PR and
ER-negative breast cancer patients. Evidence suggests a link
between obesity and breast cancer at the time of diagnosis as
well as recurrence and mortality of patients [18-19]. Also
Evidence has shown that inactivity is a risk factor for breast
cancer and death from the disease [20]. Despite our knowledge
of the above, we have little information on how weight loss and
physical activity can reduce breast cancer risk or in improving
outcomes in individuals diagnosed with breast cancer [21]. Most
recent trials are evaluating impression of interventions such as
diet, weight loss, and physical activity in the relapse and survival
of patients with breast cancer. The results of research success-c
trial were presented at the San Antonio Breast Cancer
Symposium 2018 [22] showed participants who completed the
study had a low relapse rate and mortality. We need
recommendations for patients to lose weight in obese people
and plan for physical activity. Recommendations to patients
about physical activity were either vigorous activity or
household activities or walking [23]. In the present study,
patients were advised to have at least 60 minutes/day walking
for 6 day per week or moderate to intensive physical activity 5
days per week. Early studies have shown that low levels of
vitamin D at the time of diagnosis are associated with a high risk
of relapse; patients are therefore advised to consume food high
in calcium and vitamin D, such as Douq (diluted yoghurt),
yoghurt, fish (twice a week), vegetables (5 days a week) and no
barbecues. Moreover, obese patients are advised to lose weight
[24-27]. Patients with a BMI over 30 are advised to reduce their
BMI by reducing their waistline. Review of literature shows that
a BMI over 25 is associated with a poor prognosis [28-29]. These
patients are therefore advised to use low-fat and low-sugar diets
since high-cholesterol diets may induce vasculogenesis [30]. In
the analysis of patients in the present study, the rates of local
relapse, systemic relapse and mortality were lower in the first
three years compared to other studies. Three unproven
hypotheses were therefore proposed, suggesting different influential factors: First, the stage of disease (a substantial
proportion of patients in the present study were in stages 1,2
and 3); second, the 4 drugs used (epirubicin, taxotere,
cyclophosphamide and 5-E-U); and third, advices about diet,
lifestyle change and physical activity. P53 was found to display
an important role in the prognosis of the disease and the
survival of P53-positive patients was also found to be lower than
the survival of P53-negative patients. In the present study, Ki-67
was not associated with a poor prognosis, which might have
been due to the low number of IHC performed for Ki-67.
Conclusion
Unlike genetic factors affecting prognosis in triple negative
patients that cannot be interfered with, interfering with
environmental and acquired factors might actually improve
patients' prognosis. The high level of visceral metastasis in these
patients necessitates their constant follow-up and surveillance
during the first few years at shorter intervals, especially in the
case of P53-positive patients, because survival rates might
increase with the early diagnosis and aggressive treatment of
relapsed patients. To conclude, TEC is an acceptable treatment
regimen.
References
- American Cancer Society: Cancer Facts and Figures 2019 Atlanta Ga: American Cancer Society
- Martin J Larsen Mads Thomassen, Anne-Marie Gerdes, Torben A Kruse (2014) Hereditary Breast Cancer: Clinical Pathological and Molecular Characteristics. Breast Cancer (Auckl) 8: 145–155
[Crossref] [Google Scholor] [Pubmed]
- Eunjung Lee, Roberta McKean-Cowdin, Huiyan Ma, Darcy V Spicer, David Van Den Berg, et al. (2011) Characteristics of Triple-Negative Breast Cancer in Patients with a BRCA1 Mutation: Results from a Population-Based Study of Young Women. J Clin Oncol 29:4373–4380
[Crossref] [Google Scholor] [Pubmed]
- Dent R, Trudeau M, Pritchard KI, Hanna WM, Kahn HK, et al. (2007) Triple-negative breast cancer: Clinical features and patterns of recurrence. Clin Cancer Res 13:4429-4434
[Crossref] [Google Scholor] [Pubmed]
- Carey LA, Dees EC, Sawyer L, Gatti L, Moore DT, et al. (2007) The triple negative paradox: Primary tumor chemosensitivity of breast cancer subtypes. Clin Cancer Res 13:2329-2334
[Crossref] [Google Scholor] [Pubmed]
- Boyle P (2012) Triple-negative breast cancer: epidemiological considerations and recommendations. Ann Oncol 23:vi7-vi12
[Crossref] [Google Scholor] [Pubmed]
- Jennifer A Ligibel, Karen Basen-Engquist, Jennifer W Bea (2019) Weight Management and Physical Activity for Breast Cancer Prevention and Control. American Society of Clinical Oncology Book 39:22-33
[Crossref] [Google Scholor] [Pubmed]
- Judith Hugh, John Hanson, Maggie Chon U Cheang, Torsten O Nielsen, Charles M Perou, et al. (2009) Breast cancer subtypes and response to docetaxel in node-positive breast cancer: Use of an immunohistochemical definition in the BCIRG 001 trial. J Clin Oncol 27:1168–1176
[Crossref] [Google Scholor] [Pubmed]
- Katarzyna Pogoda, Anna Niwińska, Magdalena Murawska, Tadeusz Pieńkowski (2013) Analysis of pattern time and risk factors influencing recurrence in triple-negative breast cancer patients. Med Oncol 30:388
[Crossref] [Google Scholor] [Pubmed]
- Jones RL, Salter J, A'Hern R, Nerurkar A, Parton M, et al. (2009) The prognostic significance of Ki67 before and after neoadjuvant chemotherapy in breast cancer. Breast Cancer Res Treat 116:53-68
[Crossref] [Google Scholor] [Pubmed]
- Rakha EA, El-Sayed ME, Green AR, Lee AH, Robertson JF, et al. (2007) Prognostic markers in triple-negative breast cancer. Cancer 109:25-32
[Crossref] [Google Scholor] [pubmed]
- Jung SY, Han W, Lee JW, Ko E, Kim E, et al. (2009) Ki-67 expression gives additional prognostic information on St Gallen 2007 and Adjuvant! Online risk categories in early breast cancer. Ann Surg Oncol 16:1112-1121
[Crossref] [Google Scholor] [Pubmed]
- Bhumsuk Keam, Seock-Ah Im, Kyung-Hun Lee, Sae-Won Han, Do-Youn Oh, et al. (2011) Ki-67 can be used for further classification of triple negative breast cancer into two subtypes with different response and prognosis. Breast Cancer Res 13: R22
[Crossref] [Google Scholor] [Pubmed]
- Ping-Ping Bao, Gen-Ming Zhao, Xiao-Ou Shu, Peng Peng, Hui Cai, et al. (2015) Modifiable lifestyle factors and triple-negative breast cancer survival: a population-based prospective study. Epidemiology 26:909–916
[Crossref] [Google Scholor] [Pubmed]
- Rock CL, Doyle C, Demark-Wahnefried W (2012) Nutrition and physical activity guidelines for cancer survivors. CA Cancer J Clin 62:242-274
[Crossref] [Google Scholor] [Pubmed]
- Denlinger CS, Ligibel JA, Are M (2016) NCCN Guidelines insights: survivorship, version 1. J Natl Compr Canc Netw 14:715-724
[Crossref] [Google Scholor] [Pubmed]
- Blanchard CM, Courneya KS, Stein K (2008) American Cancer Society’s SCS-II Cancer survivors’ adherence to lifestyle behavior recommendations and associations with health-related quality of life: results from the American Cancer Society’s SCS-II. J Clin Oncol 26:2198-2204
[Crossref] [Google Scholor] [Pubmed]
- Chan DS, Vieira AR, Aune D (2014) Body mass index and survival in women with breast cancer-systematic literature review and meta-analysis of 82 follow-up studies. Ann Oncol 25:1901-1914
[Crossref] [Google Scholor] [Pubmed]
- Protani M, Coory M, Martin JH (2010) Effect of obesity on survival of women with breast cancer: systematic review and meta-analysis. Breast Cancer Res Treat 123:627-635
[Crossref] [Google Scholor] [Pubmed]
- Kushi LH, Doyle C, McCullough M, Rock CL, Demark-Wahnefried W, et al. (2012) American Cancer Society Guidelines on nutrition and physical activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity. CA Cancer J Clin 62:30-67
[Crossref] [Google Scholor] [Pubmed]
- Chlebowski RT, Luo J, Anderson GL (2019) Weight loss and breast cancer incidence in postmenopausal women. Cancer 125:205-212
[Crossref] [Google Scholor] [Pubmed]
- W Janni, BK Rack, TW Friedl, V Müller, R Lorenz, et al. (2019) Lifestyle intervention and effect on disease-free survival in early breast cancer pts: interim analysis from the randomized SUCCESS C study. Cancer Res 79
[Crossref] [Google Scholor]
- Hildebrand JS, Gapstur SM, Campbell PT, Gaudet MM, Patel AV, et al. (2013) Recreational physical activity and leisure-time sitting in relation to postmenopausal breast cancer risk. Cancer Epidemiol Biomarkers Prev 22:1906-1912
[Crossref] [Google Scholor] [Pubmed]
- Chlebowski RT, Aiello E, McTiernan A (2002) Weight loss in breast cancer patient management. J Clin Oncol 20:1128-1143
[Crossref] [Google Scholor] [Pubmed]
- Kroenke CH, Chen WY, Rosner B, Holmes MD (2005) Weight,weight gain, and survival after breast cancer diagnosis. J Clin Oncol 23:1370-8
[Crossref] [Google Scholor] [Pubmed]
- Loi S, Milne RL, Friedlander ML, McCredie MR, Giles GG, et al. (2005) Obesity and out-comes in premenopausal and postmenopausal breast cancer. Cancer Epidemiol Biomarkers Prev 14:1686-1691
[Crossref] [Google Scholor] [Pubmed]
- Cleveland RJ, Eng SM, Abrahamson PE, Britton JA, Teitelbaum SL (2007) Weight gain prior to diagnosis and survival from breast cancer. Cancer Epidemiol Biomarkers Prev 16:1803-1811
[Crossref] [Google Scholor] [Pubmed]
- Shaheenah Dawood, Kristine Broglio, Ana M Gonzalez-Angulo, Shu-Wan Kau, Rabiul Islam (2008) Prognostic value of body mass index in locally advanced breast cancer. Clin Cancer Res 14:1718-1725
[Crossref] [Google Scholor] [Pubmed]
- Rose DP, Vona-Davis L (2009) Influence of obesity on breast cancer receptor status and prognosis. Expert Rev Anticancer Ther 9:1091-1101
[Crossref] [Google Scholor] [Pubmed]
- Ebba Bråkenhielm, Renhai Cao, Bihu Gao, Bo Angelin, Barbara Cannon (2004) Angiogenesis Inhibitor, TNP-470, Prevents Diet-Induced and Genetic Obesity in Mice. Circulation Research 25
[Crossref] [Google Scholor] [Pubmed]
Citation: Usman A (2022) The Survival of Patients with Triple Negative Breast Cancer with Chemotherapy Along with Lifestyle Change
Interventions in Survivors. Arch Can Res Vol:10 No:1